

Improving Posture to Reduce the Symptoms of Parkinson's:
A CBP® Case Report with a 21 Month Follow-up
This section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Physical Therapy Science 2019 (Feb); 31 (2): 153–158 ~ FULL TEXT
OPEN ACCESS Justin M Anderson, DC • Paul A Oakley, MSc, DC • Deed E Harrison, DC
Paul A Oakley, MSc, DC
2) Private Practice: 11A-1100 Gorham Street,
Newmarket, Ontario L3Y8Y8, Canada
HEREPurpose: To demonstrate the reduction of symptoms related to Parkinson's disease by improvement in posture.
Participant and Methods: A 59–year-old male patient presented with a prior diagnosis of Parkinson's. Symptoms included a resting right hand tremor, intermittent 'freezing episodes' with gait, mild ataxia with shuffling on toes and bradykinesia assisted with a cane, as well as low back pain and right knee pain. Radiography revealed gross postural and spine deformity. The patient received Chiropractic BioPhysics care including mirror image exercises, spinal traction, spinal adjustments as well as gait rehabilitation.
Results: After 38 treatments over 5 months, the patient had significant improvements in posture alignment as well as gait, balance, hand tremors, low back and knee pains and SF-36 values. A 21 month follow-up revealed the patient had remained essentially well and the initial postural improvements were maintained.
Conclusion: This case demonstrates improvement of various symptoms in a patient with Parkinson's disease. Since poor posture is a long known clinical manifestation of this disorder, it is proposed that the improvement of posture in these patients may lead to improved outcomes. X-ray use in the diagnosis and management in those with spine deformity is safe and not carcinogenic.
Keywords: Adult spinal deformity; Parkinson’s disease; Posture rehabilitation. Keywords:
From the FULL TEXT Article:
INTRODUCTION
Parkinson’s disease (PD) is a slow progressive neurodegenerative disorder causing impaired motor function including slow movements, tremor, as well as gait and balance disturbances. [1] For 50 years, the main pharmaceutical treatment for PD has been Levodopa (L-dopa) [2], an amino acid and precursor to dopamine, a neurotransmitter that is found to be lower in the brains of PD patients.
PD treatment by L-dopa therapy has resulted in improved activities of daily living, enhanced quality of life and improved mortality rates. [2] Long-term use of L-dopa, however, is associated with side effects of development of motor fluctuations and dyskinesia and has little or no effect on some motor functions such as gait and balance, as well as little or no effect on some non-motor functions such as autonomic dysfunction, pain syndromes, sleep disorders, mood disturbances and dementia. [2]
Until recently, the relationship between PD and posture has been unclear. Mikami et al. [3], however, have recently determined a relationship between standing posture and quality of life in PD patients. Since the study was a retrospective analysis of patient files, it remains undetermined what effect correcting posture may have on the symptoms and activities of daily living (ADL) in PD patients. We present the successful reduction in symptoms of PD in a 59 year old by improving posture by use of the Chiropractic BioPhysics (CBP®) multimodal posture rehabilitation program.
PARTICIPANT AND METHODS
On May 2, 2016, a 59–year-old male presented with a chief complaint of Parkinson’s disease that was diagnosed by his medical doctor in 2014. The patient also complained of low back pain and right knee pain, both rated as a 6/10 on a numeric pain rating scale (NPRS: 0=no pain; 10=worst pain ever), as well as great difficulty with gait and balance.

Table 1 Of note, the patient had suffered previously from bacterial spinal meningitis (1975) and lumbar spine discitis resulting in fusion of L1/L2 (2015). He was currently taking carbidopa-Levodopa (dopamine) and mirapex (dopamine agonist) for his Parkinson’s symptoms. The SF-36 [4] scores were collected and are shown in Table 1.
Physical assessment revealed pain and muscle spasm upon palpation throughout the paraspinal areas C0–T5 and L4–L5 bilaterally. All ranges of motion (ROM) in the cervical, thoracic, and lumbar spine were reduced with lumbar extension and right lumbar lateral flexion eliciting pain.
The patient demonstrated a resting tremor in his right hand as well as ‘freezing episodes’ during gait, mild ataxia with shuffling on the toes and bradykinesia assisted with a cane. He also reported difficulties with odour perception. The patient scored a 36% on the Oswestry chronic low back pain disability questionnaire (ODI). [5]

Figure 1
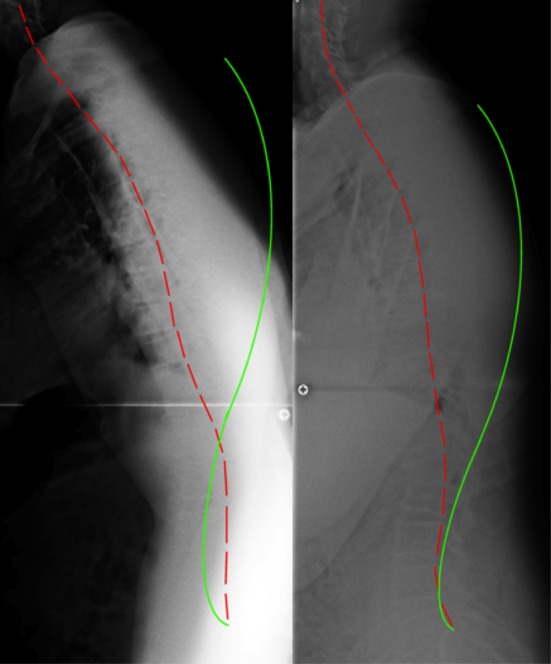
Figure 2
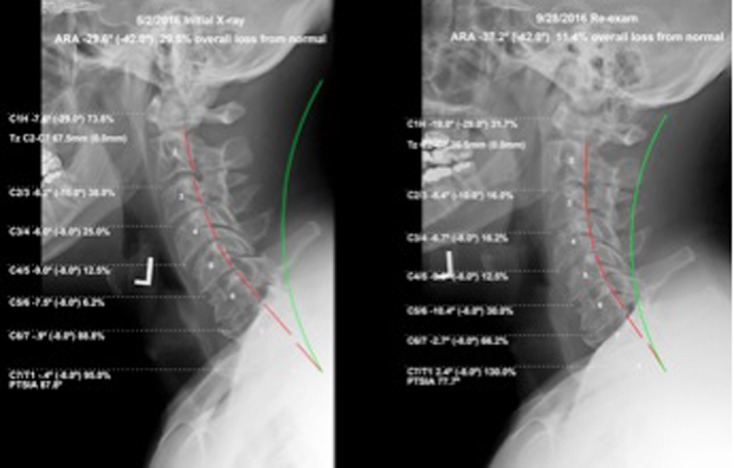
Figure 3
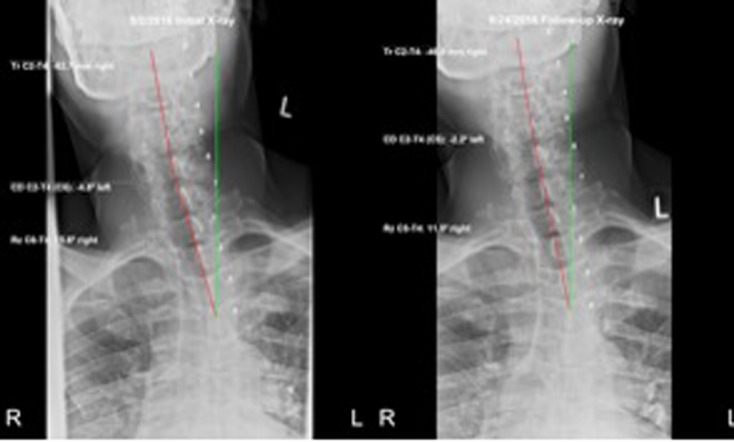
Figure 4
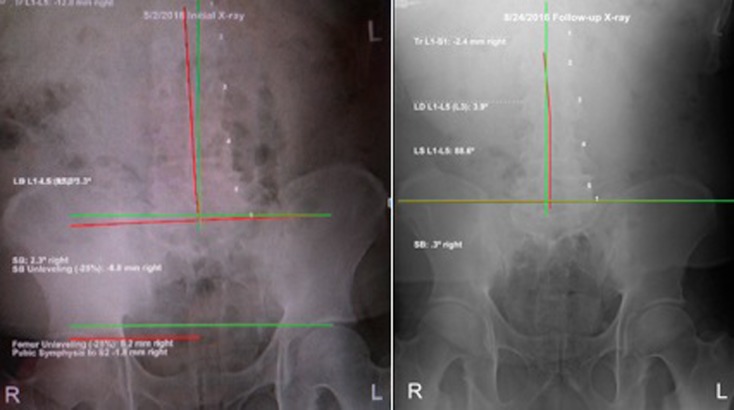
Figure 5
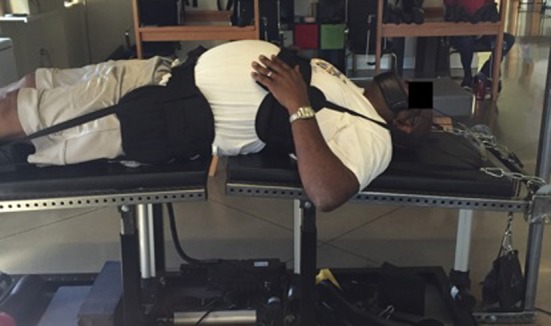
Figure 6

Figure 7 Posture analysis (Figure 1) as outlined by Harrison [6] revealed a forward head position, a prominent right head translation, a forward translated thorax, a right translated thorax, and a right laterally tilted pelvis.
Full spine radiographic assessment was performed (by JMA) including an antero-posterior (AP) cervical, thoracic, and lumbar views as well as a lateral full-spine and lateral cervical specific views. All radiographs were digitized and analyzed using the PostureRay system (Trinity, FL, USA). This system uses the Harrison posterior tangent (HPT) method for lateral spine images [7, 8] and the modified Riser-Ferguson method for AP spine images. [8] These mensuration methods are repeatable and reliable. [7–9] The HPT method measures rotation between adjacent vertebra or global regions (Absolute Rotation Angle: ARA, i.e. C2–C7) by placing lines along the posterior vertebral bodies.
The lateral full-spine radiograph (Figure 2) demonstrated a significant forward lean, as the measurement from the horizontal distance from the posterior-superior vertebral body corner of T1 to the posterior inferior body corner of S1 measured 192.3 mm (ideal=0 mm. [10] The lateral cervical specific image (Figure 3) demonstrated a forward head position of 67.5 mm (normal=0–15 mm [11]), an ARA from C2–C7 of –29.6° (normal= –31° to 42° [11–13]), and an atlas plane angle of –7.6° (normal= –29° [11, 12]). The AP cervico-thoracic view (Figure 4) showed a large right head translation (62.7 mm; normal=0 mm [10]), with a cervico-dorsal angle of –4.8° (normal=0° [10]) and an Rz angle of 15.6° (normal=0° [10]). The AP lumbar view (Figure 5) showed a right thoracic translation (–12.6 mm; normal=0 mm [10]), with unleveling of the pelvis lower on the right.
The patient was treated with CBP protocol [14–17] at a frequency of up to three times a week over a 5-month time period. CBP is a multimodal treatment approach that includes ‘mirror image’ exercises, spinal adjustments, and traction techniques for the correction of posture and spine alignment. CBP was developed by Don Harrison in 1980, and originated from ideas related to the application of linear algebra concepts applied to human posture. [14] Essentially, the spine and posture is stressed in an exact opposite (mirror image) position via exercises, traction, and drop-table adjustments to obtain its correction. Many clinical controlled trials have been conducted and prove its efficacy. [18–25]
Chiropractic treatment included both mirror image drop-table and instrument adjustments; this involves the patient to be placed in an opposite postural position and external forces via vibration of a table piece dropping to a stopped position, or stimulation of paraspinal muscles by hand-held adjusting instrument which simply taps or stimulates the muscles and soft tissues around the spine. Exercises included both left head translation and posterior head translation exercises; both were prescribed at 15 repetitions and held for 15 seconds per repetition. The patient was recommended to do the same two exercises at home daily at a frequency of 50–75 repetitions per day. Traction included two set-ups on the Robo-Trac traction table (Middletown, NY, USA): Sagittal traction with the patient supine with a superior-posterior pull on the head and torso to provide both a distraction and extension force to the head, neck and upper thoracic spine (Figure 6) and was done for 20 minutes each visit; Coronal traction had the patient on their left side with the pelvis elevated so the thorax is translated to the left and the head is also translated to the left (Figure 7) and was performed for 10 minutes each visit.
Gait rehabilitation was also prescribed utilizing the PowerPlate (Northbrook, IL, USA). The patient would lay on the PowerPlate in the prone position for two minutes while laying on the forearms to force an extension into the torso; the vibration platform adds intensity to the stretch. [26]
He was also taken outside the clinic and instructed to walk in an exaggerated fashion concentrating on lifting his legs and emphasizing all parts of the gait cycle including heel strike and toe-off. The patient consented to the publication of this case including all x-rays and pictures.
RESULTS
The patient was diligently monitored throughout treatment and a comprehensive re-assessment was performed, after the patient had received 38 treatments, on Sep. 28, 2016 that included follow-up radiographs, posture pictures, questionnaires and orthopedics tests.
At this time the patient reported that their LBP and right knee pain was a 2/10, and scored a 34% on the ODI. The SF-36 indicated there was improvement in 5/8 health categories (Table 1). The patient’s balance and coordination had noticeably improved, ROM improved in all directions and there was no report of pain in any direction. The patient was now walking without a cane and the ‘freezing’ episodes were significantly reduced, the patient was even able to jog.
The patient’s posture as seen visually (Figure 1) improved dramatically. Follow-up radiographic assessment confirmed and quantified the significant improvements in the patient’s posture (Figures. 3–6).The total body forward shift from T1-S1 reduced (132 mm vs. 192 mm),
forward head posture reduced (36.5 mm vs. 67.5mm),
there was an increased cervical lordosis (–37.2° vs. –29.6°),
an increased atlas plane angle (–19.8° vs. –7.6°),
a reduced lateral head translation (–46 mm vs. –62.7 mm) and
a reduced lateral thoracic translation (–2.4 mm vs. –12.8 mm).
The pelvis was also leveled out by the prescription of a 12 mm heel lift for the right leg.On Jun. 28, 2018, a 21 month follow-up consultation was performed over the phone. The patient reported to be well other than extreme rigidity and tightness of the right leg and knee. Overall the patient felt better postured since the initial treatments and much improved functionally.
DISCUSSION
This report documents the successful outcome in a 59-year-old suffering from Parkinson’s who had significant health improvements corresponding with the improvement in posture.
It is known that the area of the substantia nigra is affected in patients with PD. [27] However, it is also known that extra tension exerted onto the spinal cord and brainstem through poor spine and posture position may stretch and strain the cord and subtentorial brain. [28] This ‘pathologic tension’ may impede both blood flow as well as neuron conduction. [29–32]
It is proposed that those with well established nervous system disorders such as those with PD or multiple sclerosis (MS) may be more affected by substantially poor posture, as for example, neurosurgeon Alf Breig provided significant neurologic symptom relief to MS patients by his ‘cervicolordodesis’ surgical procedure that restored the cervical lordosis. [33]
Breig states that the restoration of neurologic function in his recovered patients were due to the restoration of normal slack into the pons-cord tissue tract and the relief of the so-called pathologic tensions exerted onto the cord and brain matter by the flexed cervical posture. [31] We suggest this explanation may be applicable to other neurologic disorders such as PD as the substantia nigra is located in the midbrain and can be biomechanically stressed/strained through tension onto the cord as in poorly hunched postures.
Abnormal posture has long been recognized as a clinical manifestation of PD [34, 35], however, the treatment of abnormal posture in PD is difficult because it is thought to be comprised of multiple background pathologies such as proprioceptive dysfunction, dystonia and rigidity for example. [35] Since postural deformity is directly related with the quality of life in patients with PD [3] it is only logical to assume that a postural rehabilitation program should, if successfully improving posture, bring about improvements to the quality of life in PD patients as what occurred with the patient reported here. We recommend postural rehabilitation as a key treatment for patients with PD.
Radiographic imaging is the most accurate method to reliably measure spine alignment and displacement in adults having spine deformity as other methods are indirect and not accurate. [36] X-rays and its radiation exposures are thought to be risky for the patient as it is assumed to be carcinogenic. This long-held belief is erroneous. Recent evidence has emerged that substantiates the fact that the amount of radiation from spinal x-rays (2–3 mGy) are only about 6% of the amount it would take to reach the threshold (500 mSv) changing from zero risk to possibly carcinogenic for leukemia. [36] In fact, based on this evidence, patients could get a few dozen (500 mGy threshold/3 mGy=167 sets of X-rays) full-spine x-rays for spinal assessment and monitoring of treatment (i.e. for scoliosis) and it would still be safe and not carcinogenic. [36–38]
Limitations to this report are that this is a single case only. The patient was treated with multiple treatments blurring which component of the treatment may have been most essential in the correction of posture. It should be noted that exercise [39] has not been proven to routinely correct structural spine alignment; therefore, it is assumed that the traction portion is most likely responsible for the spine alignment correction as has been demonstrated recently by Moustafa et al. [18–23]
Our case demonstrates that the correction of posture in this patient suffering from all the cardinal symptoms of PD resulted in dramatic improvement in symptoms. More research is needed to evaluate the role of correcting posture in those with PD.
Conflict of interest
Dr. Paul Oakley (PAO) is paid by CBP NonProfit, Inc. for writing the manuscript; Dr. Deed Harrison (DEH) teaches chiropractic rehabilitation methods and sells products to physicians for patient care used in this manuscript.
References:
Sveinbjornsdottir S:
The clinical symptoms of Parkinson’s disease.
J Neurochem, 2016, 139: 318–324.Sethi K: Levodopa unresponsive symptoms in Parkinson disease.
Mov Disord, 2008, 23: S521–S533.Mikami K, Shiraishi M, Kamo T:
Effect of abnormal posture on quality of life in patients
with Parkinson’s disease.
Adv Parkinson’s Dis, 2016, 5: 7–14.McHorney CA, Ware JE, Jr., Raczek AE:
The MOS 36-Item Short-Form Health Survey (SF-36): II.
Psychometric and clinical tests of validity in
measuring physical and mental health constructs.
Med Care, 1993, 31: 247–263Deyo RA:
Measuring the functional status of patients with low back pain.
Arch Phys Med Rehabil, 1988, 69: 1044–1053.Harrison DD:
Abnormal postural permutations calculated as rotations and
translations from an ideal normal upright static posture.
In Sweere, JJ: Chiropractic Family Practice,
Gaithersburg: Aspen Publishers, 1992, chap 6–1, pp 1–22.Harrison DE, Harrison DD, Cailliet R, et al.:
Cobb method or Harrison posterior tangent method:
which to choose for lateral cervical radiographic analysis.
Spine, 2000, 25: 2072–2078.Harrison DE, Holland B, Harrison DD, et al.:
Further reliability analysis of the Harrison radiographic
line-drawing methods: crossed ICCs for lateral posterior
tangents and modified Risser-Ferguson method on AP views.
J Manipulative Physiol Ther, 2002, 25: 93–98Harrison DE, Harrison DD, Colloca CJ, et al.:
Repeatability over time of posture, radiograph positioning, and
radiograph line drawing: an analysis of six control groups.
J Manipulative Physiol Ther, 2003, 26: 87–98.Harrison DE, Harrison DD, Haas JW, et al.:
Spinal biomechanics for clinicians.
Evanston, WY: Harrison CBP® Seminars, Inc., 2003. p 42Harrison DD, Janik TJ, Troyanovich SJ, et al.:
Comparisons of lordotic cervical spine curvatures to a
theoretical ideal model of the static
sagittal cervical spine.
Spine, 1996, 21: 667–675.Harrison DD, Harrison DE, Janik TJ, et al.:
Modeling of the sagittal cervical spine as a method to
discriminate hypolordosis: results of elliptical
and circular modeling in 72 asymptomatic subjects,
52 acute neck pain subjects, and 70 chronic
neck pain subjects.
Spine, 2004, 29: 2485–2492.McAviney J, Schulz D, Bock R, et al.:
Determining the relationship between cervical lordosis
and neck complaints.
J Manipulative Physiol Ther, 2005, 28: 187–193.Harrison DD, Janik TJ, Harrison GR, et al.:
Chiropractic biophysics technique: a linear algebra approach
to posture in chiropractic.
J Manipulative Physiol Ther, 1996, 19: 525–535.Oakley PA, Harrison DD, Harrison DE, et al.:
Evidence-based protocol for structural rehabilitation of
the spine and posture: review of clinical biomechanics
of posture (CBP) publications.
J Can Chiropr Assoc, 2005, 49: 270–296.Harrison DE, Harrison DD, Haas JW:
Structural rehabilitation of the cervical spine.
Evanston, WY: Harrison CBP® Seminars, Inc., 2002.Harrison DE, Betz JW, Harrison DD, et al.:
CBP structural rehabilitation of the lumbar spine:
Harrison Chiropractic Biophysics Seminars, Inc. 2007.Moustafa IM, Diab AA, Taha S, et al.:
Addition of a sagittal cervical posture corrective
orthotic device to a multimodal rehabilitation
program improves short- and long-term outcomes
in patients with discogenic cervical radiculopathy.
Arch Phys Med Rehabil, 2016, 97: 2034–2044.Moustafa IM, Diab AA, Harrison DE:
The effect of normalizing the sagittal cervical
configuration on dizziness, neck pain, and
cervicocephalic kinesthetic sensibility:
a 1-year randomized controlled study.
Eur J Phys Rehabil Med, 2017, 53: 57–71.Moustafa IM, Diab AA, Hegazy FA, et al.:
Does rehabilitation of cervical lordosis influence sagittal
cervical spine flexion extension kinematics in cervical
spondylotic radiculopathy subjects?
J Back Musculoskeletal Rehabil, 2017, 30: 937–941Diab AA, Moustafa IM:
Lumbar lordosis rehabilitation for pain and lumbar
segmental motion in chronic mechanical low back pain:
a randomized trial.
J Manipulative Physiol Ther, 2012, 35: 246–253Moustafa IM, Diab AA:
Extension traction treatment for patients with discogenic
lumbosacral radiculopathy: a randomized controlled trial.
Clin Rehabil, 2013, 27: 51–62Diab AA, Moustafa IM:
The efficacy of lumbar extension traction for sagittal
alignment in mechanical low back pain: a randomized trial.
J Back Musculoskeletal Rehabil, 2013, 26: 213–220Harrison DE, Cailliet R, Betz J, et al.:
Conservative methods for reducing lateral translation
postures of the head: a nonrandomized clinical control trial.
J Rehabil Res Dev, 2004, 41: 631–639Harrison DE, Cailliet R, Betz JW, et al.:
A non-randomized clinical control trial of Harrison mirror
image methods for correcting trunk list (lateral
translations of the thoracic cage) in patients
with chronic low back pain.
Eur Spine J, 2005, 14: 155–162Lee DY:
Analysis of muscle activation in each body segment in
response to the stimulation intensity of whole-body vibration.
J Phys Ther Sci, 2017, 29: 270–273Kalia LV, Lang AE:
Parkinson’s disease.
Lancet, 2015, 386: 896–912Breig A:
Biomechanics of the central nervous system.
Stockholm: Almquist & Wicksell, 1960Breig A:
Adverse mechanical tension in the central nervous system.
Stockholm: Almquist & Wicksell, 1978Panjabi M, White A, 3rd: VBiomechanics of nonacute cervical spinal cord trauma.
Spine, 1988, 13: 838–842Breig A, Turnbull I, Hassler O:
Effects of mechanical stresses on the spinal cord in
cervical spondylosis. A study on fresh cadaver material.
J Neurosurg, 1966, 25: 45–56Dohrmann GJ:
Experimental spinal cord trauma. A historical review.
Arch Neurol, 1972, 27: 468–473Breig A:
Skull traction and cervical cord injury.
A new approach to improved rehabilitation.
New York: Springer-Verlag, 1989Parkinson J:
An essay on the shaking palsy.
J Neuropsychiatry Clin Neurosci, 2002, 14: 223–236,
discussion 222Doherty KM, van de Warrenburg BP, Peralta MC, et al.:
Postural deformities in Parkinson’s disease.
Lancet Neurol, 2011, 10: 538–549Oakley PA, Cuttler JM, Harrison DE:
X-ray imaging is essential for contemporary chiropractic
and manual therapy spinal rehabilitation: radiography
increases benefits and reduces risks.
Dose Response, 2018, 16: 1559325818781437Oakley PA, Harrison DE:
Radiophobia: 7 reasons why radiography used in spine
and posture rehabilitation should not
be feared or avoided.
Dose Response, 2018, 16: 1559325818781445Oakley PA, Harrison DE:
Radiogenic cancer risks from chiropractic x-rays are
zero: 10 reasons to take routine radiographs in
clinical practice.
Ann Vert Sublux Res, 2018, March 10: 48–56Hrysomallis C, Goodman C:
A review of resistance exercise and posture realignment.
J Strength Cond Res, 2001, 15: 385–390.
Return to PARKINSON'S DISEASE
Return to CASE STUDIES
Since 2-01-2026


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |