

Chiropractic Care of a 6-year-old Girl with Neck Pain;
Headaches; Hand, Leg, and Foot Pain;
and other Nonmusculoskeletal SymptomsThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Chiropractic Medicine 2009 (Sep); 8 (3): 131–136 ~ FULL TEXT
OPEN ACCESS Jan Roberts, DC, Tristy Wolfe, MA
HealthQuest Chiropractic,
Farmington, ME 04938.OBJECTIVE: The purpose of this case report is to describe the response to chiropractic care of a pediatric patient with complaints of neck pain; headaches; and hand, leg, and foot pain after head trauma and the reports of changes in the patient's history of chronic fatigue, vomiting, and coughing.
CLINICAL FEATURES: A 6-year-old girl was pushed into a playground slide, hitting her head and resulting in acute complaints of her "neck and brain hurting" and hand, foot, and occasional leg pain. In addition, the patient had a several-year history of unexplained fatigue, vomiting, and coughing spells. She had a neck pain disability index of 17.8%; left lateral and rotational head tilt; cervical antalgic lean; loss of cervical range of motion; anterior cervical translation; and spasm, tenderness, trigger points, and edema along the cervical and thoracic spine.
INTERVENTION AND OUTCOME: The patient was cared for using Activator Methods protocol. After the fifth treatment, all the patient's symptoms dissipated, with a complete return to normal activity and spinal stability after 9 treatments. At 19 weeks, her spine continued to be asymptomatic; and her neck disability index was 0%.
CONCLUSION: This case demonstrated that the Activator Method of chiropractic care had a beneficial effect for this pediatric patient.
Key indexing terms: Child, Chiropractic, Neck pain, Headache
From the FULL TEXT Article
Introduction
Pediatric chiropractic care is becoming more common as parents are seeking a more natural approach to health care for their children. In a study by Lee et al, [1] 420,000 pediatric patients saw chiropractors in just the metropolitan Boston area in 1998. The study further concluded that 30 million pediatric visits to chiropractors were made in 1997. Even subtle trauma throughout childhood may affect the future development of the spine, leading to impaired nervous system function.
One of the most common reasons parents seek care for their child is due to trauma from an injury. Injury remains the leading health problem for children. [2] Data collected from the National Hospital Ambulatory Medical Care Survey from 1992 to 1997 showed 920,551 visits to the emergency department by children and adolescents attributable to falls from playground equipment. Of those visits, children aged 5 to 9 years had the highest number of playground falls. [3] Fuhr [4] describes 3 biological principles including neuromechanical, biomechanical, and mechanochemical that could describe the sustained physiologic effects of chiropractic care. In addition, results from chiropractic care are often seen in symptoms other than musculoskeletal complaints. For example, Leboedeuf-Yde et al [5] collected data on nonmusculoskeletal responses (N-MSRs) after chiropractic care, with results of approximately 1 in 4 patients reporting at least 1 improved N-MSR.
Much of the literature on acute posttraumatic neck pain in children is reported as whiplash injury, cervical dystonia, or atlantoaxial subluxation. This particular case does not fall in any of these categories and points to the need for further studies on posttraumatic neck pain in children. A survey by Haneline [6] with 94 study participants showed that, of those with neck pain, 82% of the patients reported secondary conditions, with one of those conditions being headaches. Pediatric headache occurrence of 70% by age 15 years was reported in one Swedish study of 9000 children. [7] In addition, an Australian study of 900 children aged 10 to 18 years showed that only 36.8% had never experienced a headache. [8]
The Activator Method suggests that faulty biomechanical behavior of articulations is reflected in changes in leg length, such that [4] “The assessment protocol consists of a series of prone leg length observations and provocative tests designed to evaluate the function of the joints from the feet progressively upward throughout the axial skeleton.” Furthermore, [4] “Neurological chains of information isolated within a malfunctioning biomechanical unit will feed back through the nervous system, creating an error in muscular activation; this can be visualized as a change in leg length.” These areas may be manipulated using the Activator Adjusting Instrument, which allows for a mechanically assisted high-speed, low-amplitude thrust to specific vertebrae. [4, 9] This technique is also referred to as a form of Activator-assisted spinal manipulative therapy. [10]
Given the limited amount of research on pediatric chiropractic care for posttraumatic acute neck and headache pain and the desire of parents for more natural approach to care, we report the chiropractic care of a pediatric patient with these complaints. As well, this case reports the result of chiropractic care on chronic nonmusculoskeletal (N-MS) preinjury complaints of fatigue, coughing, and vomiting.
Case report
A 6-year–old girl with complaints of posttraumatic neck pain; headaches; and hand, foot, and occasional leg pain presented for the Activator Method of chiropractic care. The patient sustained an injury on the schoolyard after being pushed into a slide and hitting her head. A couple of days after the injury, she complained to her mother that her “neck and brain hurt.” She was waking every 2 hours with complaints of pain. In addition, the patient had a history of chronic complaints of fatigue, vomiting, and coughing.
The patient's history included prior complaints of unexplained fatigue for 7 months, numerous upper respiratory tract infections since three and a half years of age, and complaints of intermittent coughing and vomiting spells since the age of 4 years. The vomiting was often secondary to coughing. Three months before the accident, fatigue was noted on the patient's school physical; and the mother reports she would fall asleep for the night by 5:00 pm. A medical doctor ordered blood work, and a diagnosis of chronic allergic rhinitis was given. These test results were brought to her new pediatric primary care provider after relocating residences. She had a family history of paternal juvenile diabetes. There was no other significant history for trauma, surgeries, or diseases.
A recorded history by the mother after the incident includes visits to a physician, an emergency department visit, and 2 appointments with a manual manipulation chiropractor before activator care. A couple of days after the incident, the patient was complaining of neck pain; so she saw a medical doctor who could not find any apparent signs of injury and sent the patient home with instructions to ice and rest. Two days later, the patient was crying and complaining of hand and foot pain with tingling and was frequently waking and crying throughout the night. At this point, she was brought to the emergency department where she had blood work to rule out Lyme disease and was sent home with normal test results.
After the emergency department visit, the patient followed up with the original medical doctor. This doctor ordered referrals to check lead levels, endocrinology for family history, and a pediatric gastrointestinal doctor to review a high liver function test from 2 months earlier. The patient's symptoms remained unchanged with complaints of neck pain, headaches, and hand and foot pain 2 weeks postinjury; so the parent sought out a doctor of chiropractic. The chiropractor examined the patient, took cervical radiographs, and completed a manual manipulation to the cervical spine at the first visit and 2 days later to T5 and L4/L5. The parent noted that the child was hesitant and would not lay down for the treatment, so the treatments were completed with the child sitting. Her pain was a 6/10 on a visual analog scale (VAS) at the first visit and 5/10 VAS at the second visit, with a diagnosis of a cervical sprain/strain and a C2 flexion malposition. The patient's condition remained relatively unchanged, and the family relocated. The parent chose to follow up with a pediatrician and a chiropractor at their new location.
After relocating, approximately one and a half months post-injury, she saw the new pediatrician who noted that the patient was complaining of occasional foot pain and that the high LFT was normal. The patient presented to the new chiropractor three and a half months postinjury. At the time, her complaints of neck pain, intermittent headaches, hand and foot pain with occasional leg pain, vomiting, and coughing were unresolved. Bending aggravated her neck pain. Ice and ibuprofen had been used at home for palliative care without sustaining results.
At the time of examination, she appeared coherent and alert but nervous and moderately distressed. She was 47 in tall, weighed 52 lb, and presented with a seated blood pressure of 96/60 mm Hg. Visual examination revealed a left head tilt, right high ear, right high shoulder, anterior cervical translation, left lateral flexion and rotation of the cervical spine, and a cervical antalgic lean. On examination, the patient had edema on the left from C1 through C7, spasm on the left from the occiput through T6, and trigger points from C4 through T6. Trigger points are described as taut bands of muscle that when pressed illicit a jump response in that muscle and refer pain to different areas of the body.11 On palpation, tenderness was noted on the left at a 2/4 at the occiput, C6 through C7, and T3 through T6; and in addition, she had more tenderness 3/4 on the left from C1 through C3 and T1 through T2.
The cervical range of motion was 40°/50° cervical flexion, 40°/60° cervical extension, 60°/80° left cervical rotation, and 70°/80° right cervical rotation, all completed without pain. Cervical lateral flexion was not completed because of the discomfort of the patient, and further orthopedic cervical tests were omitted at the time because of her age and the elevated level of apprehension during her first appointment. The patient was able to perform neurologic testing including accurately bringing finger to nose and complete heel and toe walking. Her neck pain disability index was 17.8%. Her diagnosis was an unresolved sprain/strain to the cervical spine and cervical and thoracic chiropractic subluxations.
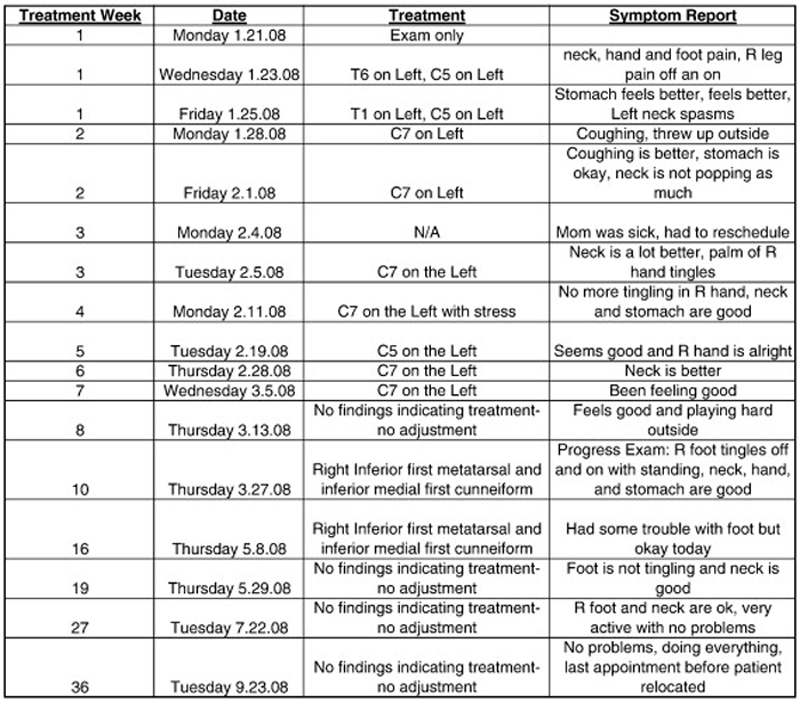
Figure 1 The treatment goal was to repair and give relief to the postinjury complaints of neck pain; intermittent headaches; hand, foot, and occasional leg pain; and preinjury conditions. The patient was prescribed a treatment plan of Activator protocol twice a week with home instructions to rest from activity for 2 weeks. This treatment plan was changed according to the patient's progress. Adjustments were indicated and performed at C5, C7, T1, and T6 throughout her treatment as per the Activator Method protocol (Figure 1). After her third adjustment, her coughing and vomiting showed improvement with decreased intensity and frequency; the patient stated that her neck pain was a lot better after her fourth adjustment; and her hand pain started feeling better by her fifth adjustment. By the 11th appointment and after 9 adjustments, she reported that she was feeling well with no complaints of pain and was playing hard. At this time, the patient was evaluated; and no further adjustments were needed.
At her progress evaluation 10 weeks into treatment, the patient was coherent, relaxed, and alert. All of the patient's complaints of pain were resolved; and she reported that she no longer had problems with fatigue, coughing, and vomiting. She reported intermittent complaints of tingling in her right foot. Her posture was erect, and she had normal ambulation. There was no edema, spasm, or trigger points in her spine. Her examination revealed cervical range of motion as 60°/50° of flexion, 60°/60° of extension, 45°/45° of left lateral flexion, 45°/45° of right lateral flexion, 60°/80° of left rotation, and 50°/80° of right rotation without relating pain. Her neck pain disability index score was 8.9%. Nineteen weeks into management, her neck disability index was 0%. At 19 weeks after initiation of treatment and approximately 33 weeks postinjury, the patient had no complaints and had a pain score of 0/10 VAS.
Discussion
As reported by Haneline, [12] millions of chiropractic manipulations for neck pain are performed each year; yet there is little information available in the medical or chiropractic literature about chiropractic manipulation and acute neck pain. In a review of the literature, fewer than 10 articles even peripherally dealt with the treatment of acute neck pain with cervical manipulation. Narrowing this search even further to pediatric neck pain and chiropractic care proved to be more difficult, although the American Chiropractic Association reported in 2000 that 12% of chiropractic patients are 16 years and younger. [9]
At present, there is no published study of postinjury neck pain treated with chiropractic care in a pediatric patient not diagnosed as cervical dystonia, whiplash, congenital torticollis, or atlantoaxial subluxation. Of the research that has been conducted, we can draw some conclusions about the effectiveness of chiropractic care for symptoms of headache and neck pain. McMorland and Suter [13] showed a reduction in neck pain on average of 53.8% and reduction in disability on average of 48.4% after an average of 12 chiropractic treatments over a 4-week period. Further reductions in disability were reported in 94 patients with acute neck pain from 84% to 25%.8 In this case report, we saw a 17.9% reduction from 17.9% to 0% in the neck pain disability index.
One study involving a pediatric patient with both severe headache and neck pain for 5 days showed resolution of both symptoms after 4 chiropractic treatments over a 2-week period. [8] In addition, a case series of 5 children with varying types of headaches were resolved after chiropractic care in a study by Anderson-Peacock. [14] Although the cause of the symptoms in these studies differs from this case report, it indicates that research is needed because there appears to be a correlation between chiropractic care and resolution of headache and neck pain.
Other studies have addressed issues with similar symptoms experienced chronically by the patient in this case study. One such case study of a 9-year–old boy who have had asthma and upper respiratory tract infections since infancy, headaches since age 6 years, and neck pain since age 8 years showed resolution of all symptoms after 6 weeks of chiropractic care. [15] In this case, we saw an overall improvement of the patient's health and well-being and resolution of various chronic complaints including N-MSRs. In the study by Leboefu-Yde et al, [5] of the patients who experienced N-MSRs with chiropractic care, respiratory and digestive system responses were the most commonly reported. The concept of musculoskeletal dysfunction or nerve interference inducing organic disorders or symptoms is questioned by whether or not removing spinal dysfunction removes symptoms and signs that mimic disease or disorders. [5] Results in this case would point to the need for more research in the area of chiropractic care improving overall health and resolving symptoms unrelated to the chief complaint.
In this case, the Activator Method may have been a good method of treatment for this patient because she appeared apprehensive. The Activator adjustment is a high-speed, low-force adjustment that may be less intimidating than a manual adjustment for children. Further studies in this treatment method with the younger population would be beneficial.
The chiropractic treatment of neck pain is important because neck pain is second only to low back pain in its frequency in the general population and because it has been estimated that 25% of primary complaints among chiropractic patients involve neck pain. [16] In addition, it is estimated that approximately 30% of patients with neck pain will develop chronic symptoms. [13] It is highly recommended that more research be done in the area of chiropractic care of posttraumatic acute neck pain and headaches for pediatric patients as well as resolution of nonmusculoskeletal symptoms in this special population with the Activator Method. This case report is important in 2 ways: first, the resolution of the patient's acute traumatic onset of her chief complaints and, secondly, the prior preinjury chronic nonmusculoskeletal symptoms that resolved during subluxation correction. The possible cost and public health benefits from chiropractic care are also worth further exploration.
Limitations of this report include the complex history, age, and apprehension of the patient. It is possible that the resolution of symptoms was spontaneous or that symptoms could have resolved during the natural course of the disorder. It is also possible that the patient's chronic symptoms were caused by an environmental allergy or other environmental factors that resolved after she moved. However, the patient had been in her new location for almost 3 months without resolution before reporting for chiropractic care. This case study report could have been enhanced by including follow-up laboratory work to show any change in her condition in relationship to her blood work as well as collecting more objective measurements of the various complaints throughout her treatments.
Conclusion
We report the successful resolution of a 6-year–old patient with complaints of posttraumatic neck pain; headaches; hand, leg, and foot pain; and chronic N-MS complaints of fatigue, coughing, and vomiting using the Activator Method protocol. The positive results in this case study and limited current research warrant further studies.
Funding sources and conflicts of interest:
No funding sources were reported for this study. Dr Roberts serves as a member of the Activator Methods Clinical Advisory Board and as an instructor of Activator Methods International.
References:
Lee A.C.C., Li D.H., Kemper K.J.
Chiropractic care for children
Arch Pediatr Adolesc Med 2000 (Apr); 154 (4): 401–407Sanchez J.I., Paidas C.N.
Childhood trauma: now and in the new millennium.
Surg Clin North Am. 1999;79:1503–1535Phelan K.J., Khoury J., Kalkwarf H.J., Lanphear B.P.
Trends and patterns of playground injuries in United States children and adolescents.
Ambul Pediatr. 2001;1:227–233Fuhr A.W.
2nd ed. Mosby; St. Louis: 2009.
Activator Method.Leboeuf-Yde C., Axen I., Ahlefeldt G., Lidefelt P., Rosenbaum A., Thurnherr T.
The types and frequencies of improved nonmuskuloskeletal symptoms reported after chiropractic spinal manipulative therapy.
J Manipulative Physiol Ther. 1999;22(9):559–564Haneline M.T.
Symptomatic Outcomes and Perceived Satisfaction Levels of Chiropractic Patients
with a Primary Diagnosis Involving Acute Neck Pain
J Manipulative Physiol Ther 2006 (May); 29 (4): 288–296Hewitt E.G.
Chiropractic care of a 13-year–old with headache and neck pain: a case report.
J Can Chiro Assoc. 1994;38(3):160–162.King N.J., Sharpley C.F.
Headache activity in children and adolescents.
J Paedtr Child Health. 1990;26:50–54Fuhr A.W., Menke J.M.
Status of activator methods in chiropractic technique, theory, and practice.
J Manipulative Physiol Ther. 2003;28:135.e1–135.e2Song, XJ, Gan, Q, Cao, J-L, Wang, Z-B, and Rupert, RL.
Spinal Manipulation Reduces Pain and Hyperalgesia After
Lumbar Intervertebral Foramen Inflammation in the Rat
J Manipulative Physiol Ther. 2006 (Jan); 29 (1): 5–13Moore M.K.
Upper Crossed Syndrome and Its Relationship to Cervicogenic Headache
J Manipulative Physiol Ther 2004 (Jul); 27 (6): 414—420Haneline M.T.
Chiropractic manipulation and acute neck pain: a review of the evidence.
J Manipulative Physiol Ther. 2005;28:521McMorland G., Suter E.
Chiropractic management of mechanical neck and low-back pain: a retrospective, outcome-based analysis.
J Manipulative Physiol Ther. 2000;23:307–310Anderson-Peacock E.S.
Chiropractic care of children with headaches: five case reports.
J Clin Chiropr Pediatr. 1996;1:18–27.Elster E.
Upper cervical chiropractic care for a nine-year–old male with Tourette syndrome, attention deficit hyperactivity disorder, depression, asthma, insomnia, and headaches: a case report.
J Vertebral Subluxation Res. 2003;1:1–11.Vernon H.T., Humphreys K., Hagino C.A.
A systemic review of conservative treatments for acute neck pain not due to whiplash.
J Manipulative Physiol Ther. 2005;28:443
Return to PEDIATRICS
Since 3–29–2017


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |