

Parent Proxy Report and Pre-adolescent Self-report
of Pain and Trauma: A Cross-sectional
Observational Study in SwedenThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Clinical Chiropractic Pediatrics 2019 (May); 18 (2): 1596–1590 ~ FULL TEXT
OPEN ACCESS Sue A. Weber DC, MSc, FEAC, FRCC
Private practitioner in Stockholm, Sweden
EAC Chairperson of special interest group (SIG) within Pediatrics
Educator internationally in chiropractic pediatrics

Background: The prevalence of musculoskeletal pain changes significantly between pre-adolescence and adolescence. It is unclear whether parent proxy reports and child report of pain and trauma are concordant. This study investigated the respective agreement between pre-adolescents and their parents in reporting head and/or neck trauma and recurrent neck pain and/or headache.
Methods: This cross-sectional observational study formed part of a study carried out to ascertain the prevalence of non-specific neck pain and/or headache in 131 Swedish pre-adolescents. Information was gathered from a questionnaire completed in school, and an informed consent with additional questions for the parents.
Results: All of the students (n = 131) who were approached to participate in the study agreed to complete the questionnaire. Of these, 40% (n = 52) reported that they experienced neck pain and/or headaches with 31% (n = 41) reporting the frequency was “often.” The parental report differed with 6% (n = 8) of parents acknowledging that their child often had neck pain and/or headache. Similarly, 61% (n = 80) of children reported trauma to the head/neck while 20% (n = 26) of the parents reported that their child had experienced trauma to the head and/or neck region.
Conclusion: Neck pain and/or headache in this group of Swedish pre-adolescents were common, as was previous trauma to the head or neck. Most of the parents were unaware that their child often had neck pain and/or headache or had suffered head or neck trauma. This discordance should be further explored to better understand the change in reporting pain from pre-adolescence to adolescence.
From the Full-Text Article:
Introduction
Pain is the most common reason why people seek healthcare. [1] The decision to seek care for the pre-adolescent in pain involves both the parent and the child. The clinical encounter involves both their perspectives of the problem including exposure to trauma, assessment of pain and the impact on daily living. Studies comparing parent proxy and child report of pain show discrepancies [2, 3] and few explore musculoskeletal pain in the pre-adolescent. [4, 5] Studies of parent proxy reports of trauma in the pre-adolescent age group have not been performed, but Sundblad et al. 2006 study of older children reported that parent-child agreement occurred consistently only in cases of severe trauma. [6] Because pain in childhood is a predictor of pain in adulthood, [7] gathering an understanding of the complexity of the problem from the child perspective is warranted and considered the gold-standard. [8, 9] It has been accepted that assessing pain in children is different from assessing pain in adults. [10]
A parent’s perception that their child is experiencing pain is the main motivating factor when arranging a visit to a caregiver. Parents, particularly mothers, are relied upon by health care practitioners to provide information about their child. [11] Many things influence the parent’s and the child’s verbal response to the doctor’s questions.
Some of the factors which influence how the child responds are:(1) if the rating has positive or negative consequences associated with it;
(2) if the response is verbal or written; and among other things
(3) if the child’s previous experience with health care has been positive or negative. [12]The parental response is influenced by their own health, the relationship they have with the child, and their expectations of the child. [1] It is consistently noted in children and adolescents with chronic pain syndromes, as in low back pain and headaches that parents underestimate the amount of pain their child is experiencing. [13–17]
Von Baeyer et al in 2017 [18] implied that some children from four years old are able to relay information in an age appropriate tool about how much pain or “hurt” they have, although authors agree that children under seven years may have difficulty using scales appropriately to relay accurate information about pain. [18–20] By the age of eight years, most children have the skills of numeracy to use a numbered scale to rate their pain. [21–23]
Although the gold standard for assessing health related parameters is self-report, when measuring pain retrospectively, there is a tendency for children to inflate their pain, reporting higher numbers than if they had recorded pain daily. [24] This is particularly true for children who have experienced significant pain or anxiety associated with the painful event. [25]
The aim of this study was to compare the agreement of answers from pre-adolescent middle school students with answers given by their parents on questions addressing prevalence and frequency of neck pain and headache and the occurrence of head and /or neck trauma.
Methods

Table 1 This was a cross-sectional observational study included as a sub-set of a larger study carried out to ascertain the prevalence of non-specific neck pain and/or headache in Swedish pre-adolescent children. This was a group of middle school students in the 4th, 5th and 6th grades, who were 9-10 years, 11-12 years and 12-13 years old. Participants were selected from a convenience sample of students at a municipal school in a middle-class suburb outside Stockholm, Sweden. An informed consent form with additional questions for the parents (the parents were asked if the child experienced neck pain and /or headache, and how often; experienced trauma to the head or neck; and if the child had a systemic disease) was sent home in a sealed envelope. Information was gathered from students via a questionnaire which was completed in school with an informed teacher present. The inclusion criteria are listed in Table 1.
The questionnaire was adapted from questionnaires found in the literature investigating characteristics of headaches and neck pain. [26–29] The questionnaire was pilot tested on a group of 10 year olds (n = 10) to ensure that the youngest students had no problems understanding the questions and the alternatives provided. The questions concerned the duration and the frequency of pain, among other questions. None of the pilot participants were included in the final study.
Categorization
The neck pain/headache group was defined as those students who answered “I have neck pain” or “I have headaches” when asked on the questionnaire if they experienced neck pain or headaches. The no-pain group consisted of students who answered “I never have neck pain or headaches, or “I only have neck pain or headaches when I am sick” when answering the same question.
Ethical Consideration
The procedures were performed with the approval of the Anglo-European University College Research Ethics SubCommittee for postgraduate research in accordance with the Declaration of Helsinki. Ethics approval was required in Sweden and was granted by the Stockholm regional Medical Ethics Committee
Results
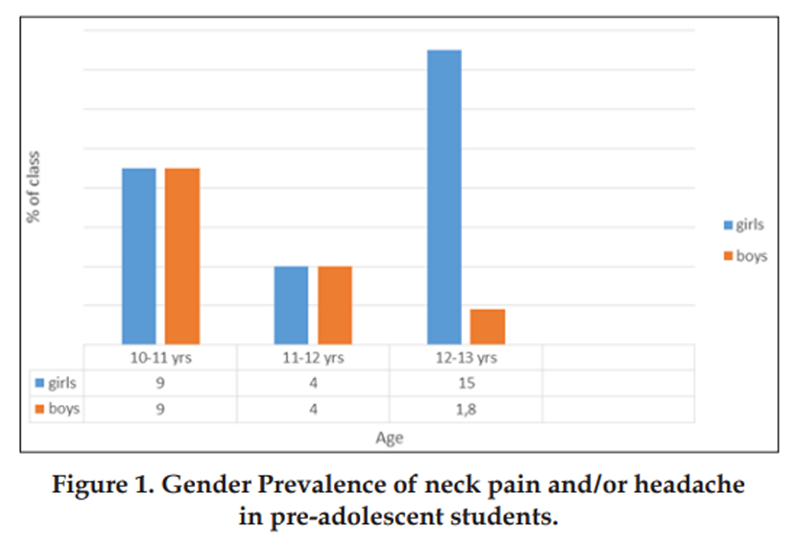
Figure 1
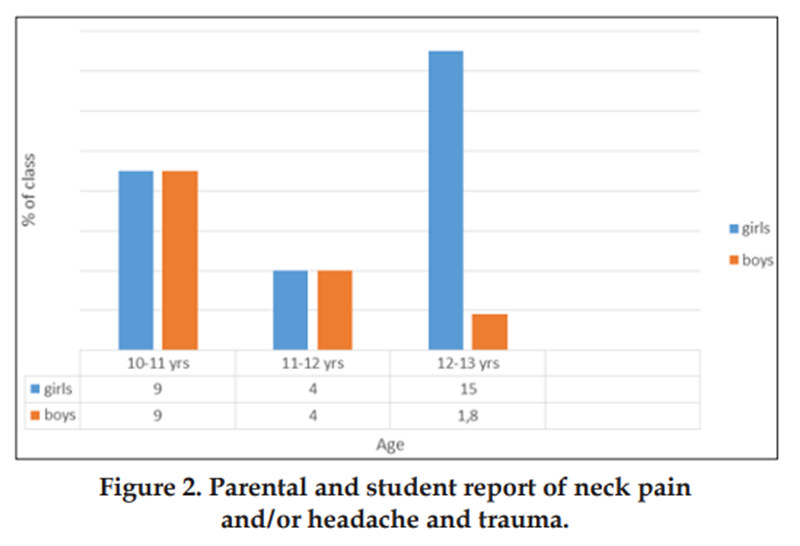
Figure 2 The questionnaire was completed by 131 students between 10 and 13 years of age. These accounted for 100% of the students who were asked to participate. Of these, 40% (n = 52) reported that they experienced neck pain and/or headache. In the fourth grade (10-11 years) there were as many boys as girls who described having neck pain and/or headaches and this was also true for the fifth graders (11-12 years). In the sixth grade (12-13 years) there were more girls than boys reporting neck pain and/or headache (Figure 1).
In all, 31% (n = 41) of the children reported in the questionnaire that they “often” had neck pain and/or headaches, while 6% (n = 8) of the parents wrote that their child had neck pain and/or headaches “often.” In total 61% (n = 80) of children reported trauma to the head/neck, whereas 20% of parents reported that their child had experienced trauma to the head and/or neck region (Figure 2). There was no significant association found between the occurrence of trauma and the incidence of neck pain and/or headaches in the students examined when analyzed with the Chi square test (P = .102)
Discussion
The goal of this study was to compare and contrast a preadolescent child’s perception of pain with that of their parents. As such, there was a clear difference in the report of the students versus the report of their respective parents. Pre-adolescent students were selected to better understand the changes which occur in neck pain and/or headache prevalence and gender distribution between pre-adolescence and adolescence. It is first in adolescence that neck pain and/or headache take on more adult-like characteristics with an increase in overall prevalence and a shift in gender distribution with a female preponderance. [30, 31] It was difficult to compare the results from this study with others because prevalence rates of neck pain and/or headaches in children vary considerably depending primarily on the criteria used and how the study has been designed. Parents reported approximately five times less frequent head and neck pain than their child. These discrepancies may reflect the weakness of the questionnaires in assessing pain in pre-adolescents and highlight the need for gathering data prospectively with daily recording of symptoms as well as through interviews with parents and children. Other possible reasons for discrepancies may be lack of communication and/or the child feelings of awkwardness about their own physical state. The results otherwise support the findings of Lundqvist et al [6] which indicated that parents not uncommonly underestimate headaches in their children.
There was also a discrepancy between parental report and child self-report in regard to the incidence of trauma to the head or neck. Despite the fact that so many students reported trauma, there was no statistical relationship between trauma and neck pain and/or headache in these students. It is feasible that children did not always tell their parents that they have hurt themselves. It is also possible that their memory of having experienced trauma is better than what their parents remember.
There was an even gender distribution among the students who reported having neck pain and/or headaches who were between 10 and 12 years of age. This is similar to other reported data for this age group. [4, 32] Students between 12 and 13 years of age must be considered peri-adolescent and interestingly, in this group, there was an increase in prevalence of neck pain and/or headaches among both boys and girls, along with a clear shift in gender distribution with female preponderance. The increase in the prevalence of neck pain and/or headache with a female gender shift in adolescence has been noted previously in the literature. [31, 33]
The fact that trauma was not significantly related to neck pain and/or headaches in this study may be that injuries occurring in childhood may become symptomatic first in adolescence with cumulative strain associated with increase in demands of studying and screen time. To explore this theory, it would be appropriate to conduct a prospective study following students to see if those who experienced trauma early in childhood more commonly suffered neck pain and/ or headaches once they reach adolescence.
Limitations
This was a pragmatic study of students in their own school setting. A pragmatic study is useful for its real world implications, but also has some weaknesses. Despite a high participation rate, the study sample was small so only trends may be observed. The study sample, a convenience sample, represents students from one school only which may introduce bias. The study sample was intended to be pre-adolescent but included a class of peri-adolescents. Further studies should clearly subgroup children into pre-adolescent, peri-adolescent and adolescent groups to investigate how neck pain and headaches evolve in this transitional period.
Conclusion
Forty percent of the pre-adolescents in this middle school setting reported recurring neck pain and/or headaches. Four out of five parents reported headaches, neck pain and trauma experienced by the child significantly less frequently than the child. This is important not only because recurrent musculoskeletal pain in this age group can have a significant impact on quality of life, but the discordance in reporting may be a factor in why report of pain changes significantly between pre-adolescence and adolescence. Because musculoskeletal pain in adolescence is a predictor for pain in adulthood, early attention in pre-adolescence could serve as a preventive measure for the long-term.
References:
Vetter T, Bridgewater C, McGwin G.
An observational study of patient versus parental perceptions of health-related
quality of life in children and adolescents with a chronic pain condition:
who should the clinician believe?
Health and Quality of Life Outcomes 2012;10:85.
http://www.hqlo.com/content/10/1/85Chiwaridzo M and Naidoo N.
Are parents and adolescents in agreement on reporting of recurrent
non-specific low back pain in adolescents?
A cross-sectional descriptive study.
BMC Pediatr 2015;8;15:203.
doi: 10.1186/s12887-015-0518-1.Vetter TR, Bridgewater CL, Ascherman LI, Madan-Swain A, McGwin GL.
Patient versus parental perceptions about pain and disability
in children and adolescents with a variety of chronic pain conditions.
Pain Res Manag 2014;19(1)7-14 No 1.Ståhl M, Kautiainen H, El-Metwally A, Håkkinen A, Salminen JJ, Mikkelsson M.
Non-specific neck pain in schoolchildren: prognosis and risk factors
for occurrence and persistence. A 4-year follow-up study.
Pain 2008;15;137(2):316-22.El-Metwally A, Salminen JJ, Auvenin A, Kautiainen H, Mikkelsson M.
Prognosis of non-specific musculoskeletal pain in preadolescents:
a prospective 4-year follow-up study till adolescence.
Pain 2004;110(3)550-9.Sundblad G, Saartok T, Engström L.
Child-parent agreement on reports of disease, injury and pain.
BMC Public Health 2006;6:276.Hestbaek L, Leboeuf-Yde C, Kyvik KO, Manniche C:
The Course of Low Back Pain from Adolescence to Adulthood:
Eight-year Follow-up of 9600 Twins
Spine (Phila Pa 1976) 2006 (Feb 15); 31 (4): 468–472McGrath PA, Speechley KN, Seifert CE, Biehn JT, Cairney AEL, Gorodzinsky FP.
A survey of children’s acute, recurrent, and chronic pain:
validation of the Pain Experience Interview.
Pain 2000;87:59-73.Goodman JE, McGrath PJ.
The epidemiology of pain in children and adolescents: a review.
Pain 1991;46:247-264.Stinson JN, Kavanagh T, Yamada J, Gill N, Stevens B.
Systematic review of the psychometric properties, interpretability
and feasibility of selfreport pain intensity measures for use
in clinical trials in children and adolescents.
Pain 2006;125:143–57.Laurell K. Larsson B, Eeg-Olofsson O.
Headache in school children: Association with other pain,
family history and psychosocial factors.
Pain 2005;119:150-8.Lifland B, Mangione-Smith R, Palermo T, Rabbitts J.
Agreement between Parent Proxy- and Child Self-Report of Pain
Intensity and HealthRelated Quality of Life after Surgery.
Acad Pediatr 2018;18(4): 376–383.
doi:10.1016/j.acap.2017.12.001Chambers CT, Reid GJ, Craig KD, McGrath PJ, Finley GA.
Agreement between child and parent reports of pain.
Clin J Pain 1998;14:336-42.Kelly A-M, Powell CV, Williams A.
Parent visual analogue scale ratings of children’s pain
do not reliably reflect pain reported by child.
Pediatric Emergency Care 2002;18:159-162.Manne SL, Jacobsen PB, Redd WH.
Assessment of acute pediatric pain: do self-report, parent ratings,
and nurse ratings measure the same phenomenon?
Pain 1992;48:45-52.Waters E, Doyle J, Wolfe R, Wright M, Wake M, Salmon L.
Influence of parental gender and self-reported health
and illness on parent-reported child health.
Pediatrics 2000;6:1422-1428.Lundqvist C, Clench-Aas J, Hofoss D, Bartonova A.
Self-reported headache in school children parents
underestimate their children’s headaches.
Acta Paediatr 2006;95:940-6.von Baeyer CL, Jaaniste T, VoHLT T, Brunsdon G, Lao HC, Champion GD.
Systematic Review of Self-Report Measures of Pain Intensity in 3-
and 4-Year-Old Children: Bridging a Period of Rapid Cognitive Development.
J Pain 2017;18(9):1017-1026.
doi: 10.1016/j.jpain.2017.03.005.Tsze DS, von Baeyer CL, Bulloch B, Dayan PS.
Validation of self-report pain scales in children.
Pediatrics 2013;132(4):e971-9.
doi: 10.1542/ peds.2013-1509.Tomlinson D, von Baeyer CL, Stinson JN, Sung L.
A systematic review of faces scales for the
self-report of pain intensity in children.
Pediatrics 2010;126(5):e1168-98.
doi: 10.1542/peds.2010-1609.Andersen RD, Langius-Eklöf A, Nakstad B, Bernklev T, Jylli L.
The measurement properties of pediatric observational
pain scales: A systematic review of reviews.
Int J Nurs Stud 2017;73:93-101.
doi: 10.1016/j.ijnurstu.2017.05.010.de Tovar C, von Baeyer CL, Wood C, Alibeu JP, Houfani M, Arvieux C.
Postoperative self-report of pain in children: interscale agreement,
response to analgesic, and preference for a faces scale
and a visual analogue scale.
Pain Res Management 2010;15(3)163-8.Palerma T, Valenzuela D, Stork P.
A randomized trial of electronic versus paper pain diaries in children:
impact on compliance, accuracy, and acceptability.
Pain 2004;107:213-9.Van de Brink M, Bandell-Hoelstra E, Abu-Saad H.
The occurrence of recall bias in pediatric headache:
a comparison of questionnaire and diary data.
Headache 2001;41:11-20.Thrane S, Wanless S, Cohen S, Danford C.
The assessment and non-pharmacologic treatment of procedural pain
from infancy to school age through a developmental lens:
A synthesis of evidence with recommendations.
J Pediatr Nurs 2016;31(1): e23–e32.
doi:10.1016/j.pedn.2015.09.002.Bruni O, Fabrizi P, Ottabianno S, Cortesi F, Giannotti F, Guidetti V.
Prevalence of sleep disorders in childhood and adolescence
with headache: a case control.
Cephalalgia 1997;17:492-8.Özge A, Bugdayci R, Sasmaz T, Kurt Ö, Karakelle A.
The sensitivity and specificity of the case definition criteria of headache:
a school-based epidemiological study of 5562 children in Mersin.
Cephalgia 2002;22:791-8.Espositio SB and Gherpelli JL.
Chronic daily headaches in children and adolescents:
a study of clinical characteristics.
Cephalalgia 2004;24:476- 82.Galli F, Patron PM, Bruni O, Strambi LF, Guidetti V.
Chronic daily headache in childhood and adolescence:
clinical aspects and a 4 year followup.
Cephalalgia 2004;24:850-8.Auvinen J, Tammelin T, Taimela S, Zitting P, Karppinen J.
Neck and shoulder pains in relation to physical activity and sedentary activities in adolescence.
Spine 2007;200:32(9)1038-44.Laimi K, VahlbergT, Salminen J, Metsähonkala L, Mikkelsson M.
Characteristics of neck pain associated with adolescent headache.
Cephalalgia 2007;27:1244-54.Kröner-Herwig B, Heinrich M, Morris L.
Headache in German children and adolescents:
a population–based epidemiological study.
Cephalalgia 2007;27:27:519-27.Anttila P.
Tension-type headache in childhood and adolescence.
Neurology 2006;5:268-74
Return to PEDIATRICS
Since 2-16-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |