

Resolution of Conductive Hearing Loss Due to
Otitis Media after Chiropractic TreatmentThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Clinical Chiropractic Pediatrics 2011 (Dec); 12 (2): 903–909 ~ FULL TEXT
OPEN ACCESS Peri Dwyer, DC, DICCP and James Boysen, DC
Private practice,
Tallahassee, Florida, USAObjective: To describe the chiropractic management of a patient with otitis media and conductive hearing loss.
Clinical Features: Parents of a 6-year-old male sought chiropractic care for the child’s measured conductive hearing loss on puretone audiometry, fluid in both ears and repeated bouts of otitis media. Prior treatment included several rounds of antibiotics starting at 14 months and myringotomy at age 3.
Intervention And Outcome: Treatment consisted of cervical, thoracic and pelvic manual manipulative therapy along with cranial manipulation. After 6 chiropractic adjustments, the child was asymptomatic, and remained free of otitis media symptoms on long-term follow-up. Nineteen months after commencement of treatment, a repeat audiogram was performed, showing normal hearing in both ears.
Conclusion: A 6-year-old male with recurring otitis media and conductive hearing loss was successfully managed using chiropractic adjustments. This may suggest a role for chiropractic care the management of otitis media with conductive hearing loss. Further research is necessary to examine this in more detail.
Key Words: Otitis media, audiology, chiropractic, therapy, child, manipulation
From the Full-Text Article:
Introduction
Ten million office visits in the United States are associated with otitis media (OM). [1] The economic burden in the US is estimated at $108 to $1,300 per episode. [2] Total cost of otitis-associated disease in the US is $3.8 billion annually: $1.8 billion in medical costs; and $2.0 billion in parental time costs. [3] Mean time-off hours lost of caregivers in 7 European countries ranged from 17.3 to 35.1 while mean productivity lost ranged from 6.7 to 22.7 hours. [4]
According to O’Reilly, risk factors include: young age, functional immaturity of the Eustachian tube, group child care, season of the year, lack of breastfeeding, the presence of adenoid tissue, environmental smoke exposure, pacifier use, allergy, sibling order, craniofacial abnormalities, genetic predisposition, and ethnicity. [5] Exposure to dioxin-like compounds and air pollution, as well as preterm birth, socioeconomic status and overweight status are also associated with OM. [2, 6-9] OM in its broadest sense is simply inflammation of the middle ear. In common usage, the word is used as synonymous with “ear infection,” even by many physicians, but the condition which most chiropractors confront in pediatric patients, persistent middle ear effusion (MEE) involves no culturable pathogenic bacteria in 75% of patients. [10]
There are 3 major categories of otitis media:Acute otitis media (AOM): Oski’s Principles and Practice of Pediatrics (1994, JB Lippincott, Philadelphia) defines this as “suppurative middle ear infection of relatively sudden clinical onset.” Otoscopy is the diagnostic hallmark, and the condition is defined by a “hyperemic, opaque tympanic membrane with distorted or absent light reflex and indistinct landmarks”. Of children with a red or yellow tympanic membrane and distention and absence of visible landmarks on otoscopy, 91% will have a bacterial infection of the middle ear. [11] Many studies have demonstrated that the majority of these infections resolve well without treatment, and that comparing antibiotic treatment to placebo reveals a very slight difference, or no difference, in the recovery rate from the acute, symptomatic episode. [10]
Otitis media with effusion (OME): This is the pediatric condition most often evaluated by audiology. The presence of effusion is generally believed to be due to a pressure gradient formed by the microvascular resorption of nitrogen from the middle ear in the absence of a patent Eustachian tube. This results in decreased pressure (and often a retracted tympanic membrane), causing extracellular fluid to exude into the middle ear cavity. [11] However, the presence of OME cannot be diagnosed by inspection of the tympanic membrane alone. Pneumatic otoscopy and/or tympanometry is necessary to assess the mobility of the tympanic membrane. [12] The prevalence of OME accounts for 25% to 35% of all otitis media. [13] Williamson stated that by 4 years of age, 80% of children have been affected by OME and the prevalence declines after age 6.
Middle ear effusion (MEE): Finally, there may exist a condition in which the patient is asymptomatic and afebrile, but has continued presence of fluid and evidence of a non-functional Eustachian tube. The criteria for a diagnosis of MEE are either:
- Two of the 3 findings:
a. membrane opacity;
b. color change/fullness; and
c. impaired mobility; or- Direct visualization of an air-fluid level. [10]
Up to 60% of children who have AOM will have persistent MEE 14 days after the bacteria have been eradicated. [14]
AOM is the most frequently diagnosed condition in children and the most common reason for antibiotic therapy. [15] Eighty percent of AOM resolves in 3 days without treatment and watchful waiting has been advised by the American Academy of Pediatrics and the American Academy of Family Physicians (AAP-AAFP) as a viable approach for children 2-12 years old with non-sever, uncomplicated AOM. The AAP-AAFP recommends antibiotic therapy for younger children or those with recurrent AOM. [16] Antibiotic use may include adverse events such as GI upset, destruction of the gut’s natural flora (which may lead to thrush), allergic reactions, increased microbial resistance to antibiotics and cost. [17]
Complications of Otitis Media
Complications of OM may include: tympanic membrane perforation, tympanosclerosis, otorrhea, or cholesteatoma. [13] Sequelae of OM may include: hearing loss (most commonly conductive); developmental delays in language, behavior, and education; mastoiditis; facial nerve paralysis; vestibular, balance and motor dysfunction; and meningitis. [18] In older children increased aggressiveness and rule-breaking behavior have been reported. [19] Tinnitus in adults is associated with a history of childhood OM. [20]
Treatment Options
Treatment of OM includes antibiotics, prophylactic antibiotics, vaccination, myringotomy with/without insertion of tympanostomy tube, and/or adenoidectomy with or without tonsillectomy. [18]
Surgical treatment with tympanostomy tubes is widespread yet controversial. A Cochrane review concluded tympanostomy tubes for hearing loss associated with otitis media with effusion were mainly beneficial in the first 6 months after insertion, although the benefits were small and diminished over time. [21] This study did not find any benefit to speech, language, learning or developmental problems, but no study has been performed on children who have established deficits in these areas.
Williamson concluded that “Oral antibiotics, antihistamines plus oral decongestants, or mucolytics may be of no benefit in OME and can cause adverse effects”, “Ventilation tubes may improve short-term outcomes, but the clinical effect size is small” and “Ventilation tubes improve hearing for the first two years, but have no longer-term benefit, and may not improve cognition of language.” [13] Tympanostomytube insertion is the most frequently performed operation in children in the US. [3]
Audiometry
The great concern when a child has recurrent OME or chronic MEE is that the child’s language development may be compromised due to hearing loss. [22] In children 5 years of age or older, the most reliable method of determining hearing loss is by pure-tone audiology. When the hearing is below the depicted normal range in one or more frequencies, it is given the following grade:-10dB to 25dB = Normal range
26dB to 40 dB = Mild hearing loss
41 dB to 55 dB = Moderate hearing loss
56 dB to 70 dB = Moderately Severe hearing loss
71 dB to 90 dB = Severe hearing loss
over 90 dB = Profound hearing loss.
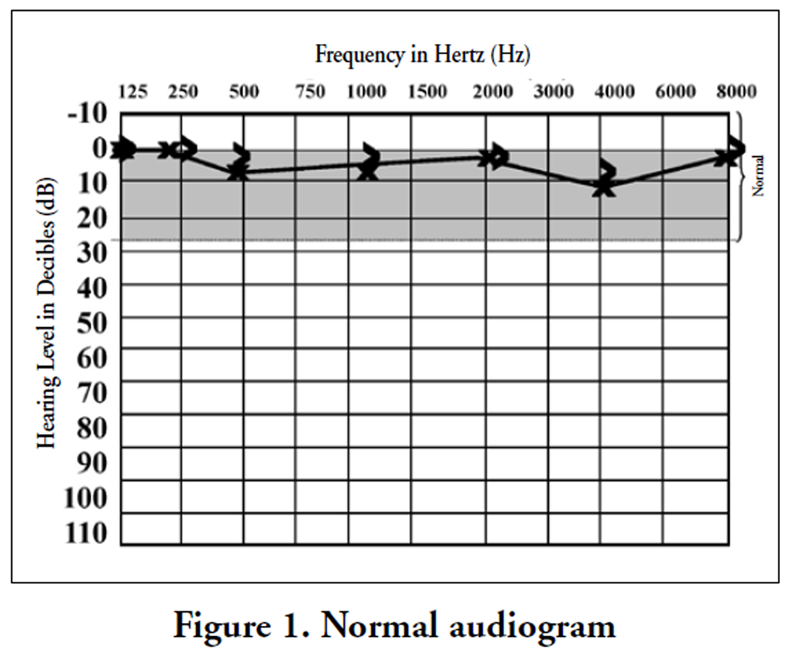
Figure 1
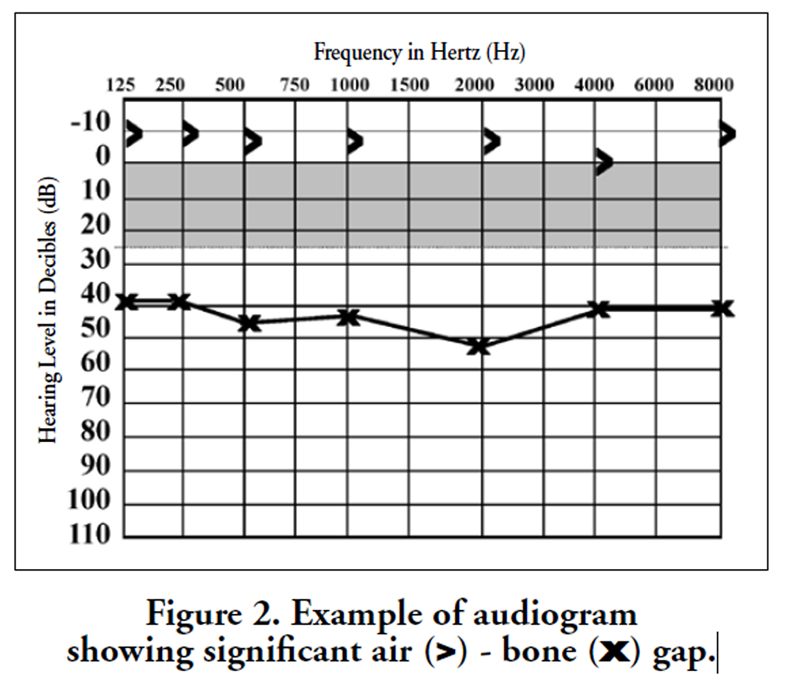
Figure 2 If the hearing loss is less than normal, it becomes necessary to determine if the hearing loss is sensorineural (due to loss of function in the cochlea, 8th cranial nerve, or brain), or conductive (due to interruption of sound in its travel from the external ear canal, through the malleus, incus, and stapes of the middle ear, and into the cochlea). This is done by comparing bone conduction to air conduction. A loss only in air conduction would be diagnostic of conductive hearing loss, while combined bone and air conduction loss would be diagnostic of sensorineural hearing loss (Figure 1).
When an air-bone gap (conductive hearing loss) is present, MEE is present 86-100% of the time. [23] When the pressure is artificially equalized between the middle ear and the nasopharynx or between the middle ear and the outside world, this air-bone gap reduces immediately but temporarily in over 90% of cases (Figure 2). [24, 25]
Case Report
Parents of a 6-year-old male sought care for fluid in both ears for “quite a while”. They also reported concern about hearing loss as measured by audiometry ordered by an ENT specialist. History revealed recurrent ear infections beginning at the age of 14 months. He was initially treated with repeated courses of antibiotics, and then by insertion of myringotomy tubes at age 3. These tubes extruded spontaneously at about age 5. Prior to seeking chiropractic care, he had recently completed a course of antibiotics for an episode of AOM. When the condition did not appear to resolve, his ENT recommended repeat tube insertion. History included several risk factors for otitis media, including short duration of breastfeeding, parental smoking, and early day care.
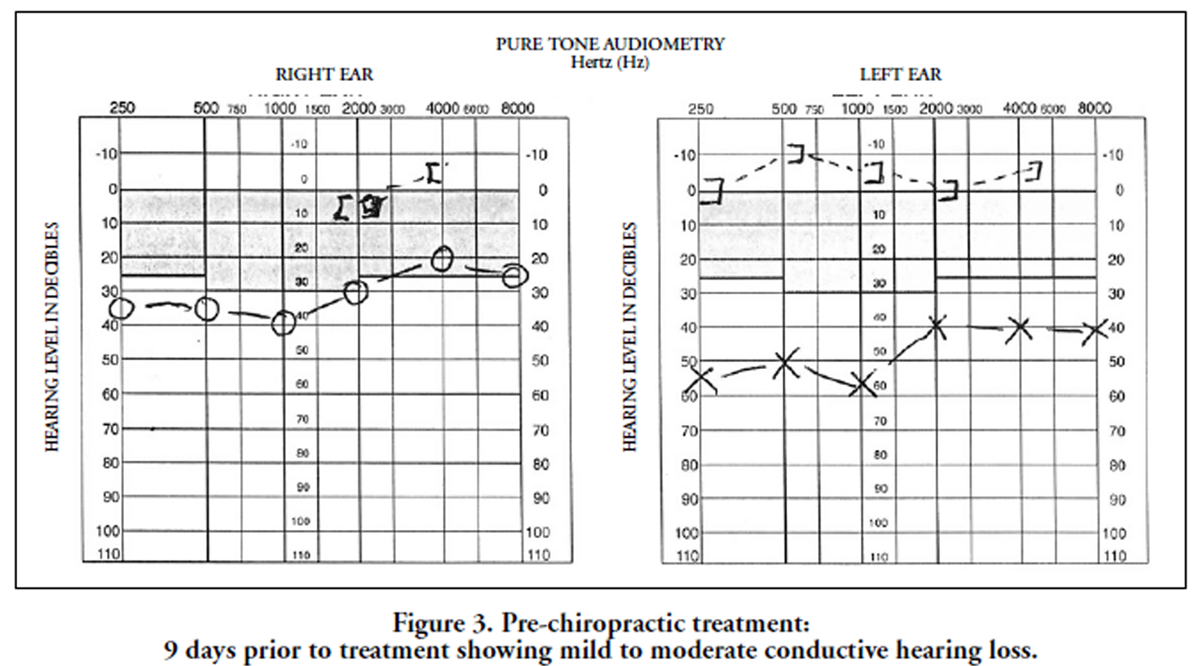
Figure 3 His initial audiogram was performed at a separate facility 9 days before starting chiropractic treatment, at the age of 6 years, 7 months (Figure 3). The test showed an obvious air-bone gap, with conductive hearing loss greater on the left than on the right. Examination of this well-nourished white male child showed postural distortion in the form of a right head tilt, restricted cervical ranges of motion and spinal subluxations/fixations of multiple segments. Multiple enlarged cervical and submandibular lymph nodes were palpable.
Treatment consisted of 6 chiropractic manipulations utilizing Gonstead and Diversified high-velocity low amplitude techniques modified to use fingertip contacts and lower force for pediatric application. Segments adjusted were based on static and motion palpation of the entire spine, and no attempt was made to correlate the segments adjusted with the segmental innervation of the middle ear or Eustachian tubes. No dietary changes were advised, and the risk factor of household smoking was not changed. The treatments were applied on a gradually tapering basis over the course of 22 days.
A brief summary of the notes from clinical encounters and treatment follows:
Day 1: See the initial history and exam findings above. Chiropractic manipulative therapy (CMT) consisted of the following: C1 right supine rotatory; C6 left supine rotatory; T4 and T10 prone double-contact diversified; right sacroiliac side posture.
Day 6: Patient reported that he heard things “louder” immediately after last visit. Right tympanic membrane (TM) showed fluid and was immobile on insufflation, but was glossy. The left TM showed no fluid and was mobile but had some dullness. Lymph node enlargement was more pronounced on the right. CMT consisted of C1 right supine rotatory; C5 right supine rotatory; T7 prone double-contact diversified; and Sacro-Occipital Technique craniopathy.
Day 9: “Hearing better” as reported by the patient’s father. The right TM was mobile with no fluid and some dullness; the left TM was dull with increased fluid but was mobile. CMT was C1 right supine rotatory, C5 left supine rotatory, T7 prone double-contact diversified, and Applied Kinesiology cranial.
Day 14: Hearing continues intermittently better per patient and per informal observations by father. TMs both were observed as dull/opaque/fluid-filled and nonmobile. Head and body posture improved. Assessment was: fair-poor results with tympanic problem and good results with subluxations/mechanical derangement. CMT was C1 right supine rotatory and T8 double contact diversified.
Day 22: Left TM mobile with no fluid; right TM mobile with fluid seen. CMT was C3 or C4 (the note is ambiguous) right supine rotatory only.
Day 27: Hearing “up and down” per father. TM’s bilaterally had no fluid and were mobile on insufflation. There was slight erythema of the left middle ear visible through the tympanic membrane. The patient’s cervical spine was free of palpable chiropractic subluxations. CMT was T9 prone diversified, left sacroiliac side-posture.
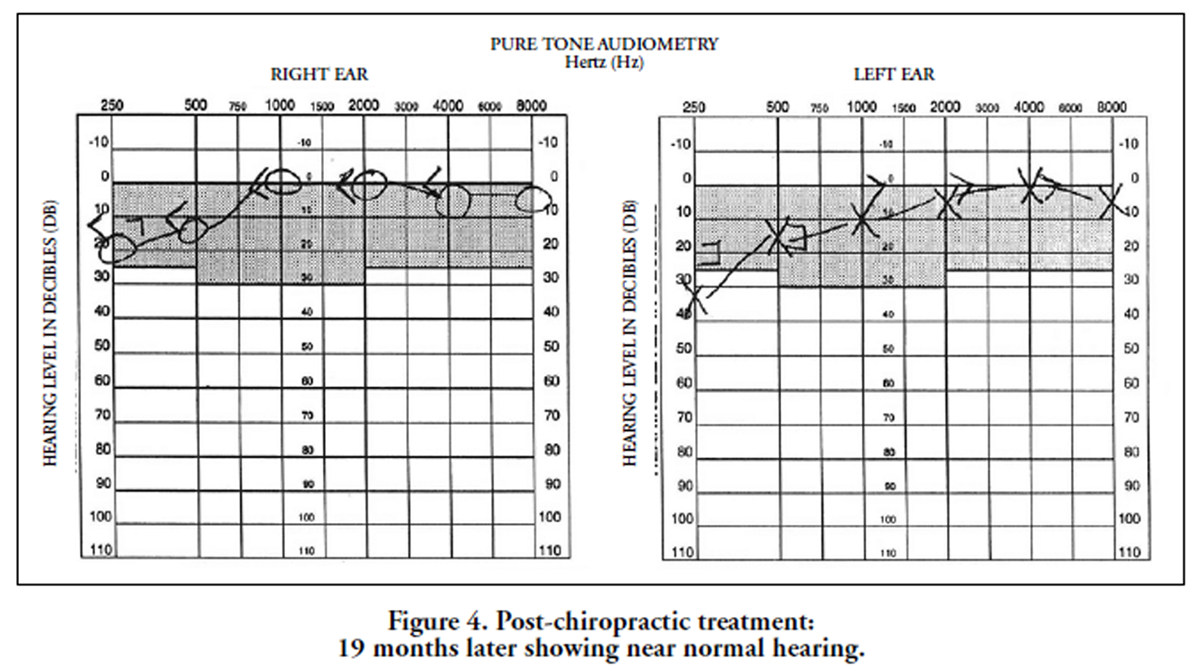
Figure 4 The patient had no ear pain or drainage and his hearing subjectively seemed improved at the end of the treatment, and the parents chose to cancel the surgery. The child remained asymptomatic with no further chiropractic or medical treatment. When the child was age 8 years, 2 months, a repeat audiogram was performed at the same separate audiology facility (19 months after his initial audiogram and 18 months after completing chiropractic treatment). Results showed the patient’s air-bone gap had closed completely, and the hearing in both ears was within normal limits (Figure 4).
Discussion
Chiropractic non-manipulative interventions
Treatment or prevention available to the chiropractor may include: xylitol as a preventative; precautions against reflux by avoiding chocolate, acidic or fruit juices, tomatoes, and fatty or greasy food, and not eating before bedtime. [9, 26] Hand washing reduces URTI which may also decrease OM. [22] Zinc supplements for preventing otitis media found no convincing evidence in a Cochrane review. [27]
Manipulation’s effects on OM
Manipulation evidence for OM has been mixed. A review of the effectiveness of manual therapies on otitis media found the evidence to be inconclusive. [28] Another review found that there is little current evidence to support chiropractic care for improvement of AOM. [29] However, Hawk’s et al. systematic review of chiropractic for nonmusculoskeletal conditions found 1 random controlled trial (RCT), 3 case series, 3 case reports and 1 pilot study for evidence of chiropractic care for otitis media. The RCT was found to be of “high” quality and found significantly fewer surgical procedures compared to usual medical care. [30] Since Hawk’s 2007 review, two additional case studies on otitis media with hearing loss have been reported in children. [31, 32]
The prevalence for otitis media decreases after 6 years of age, which is the approximate age of cranial vault maturity [18] (Although the subject of this paper had persistent symptoms after reaching the age of 6). This, along with craniofacial abnormality as a risk factor and the fact that myringotomy with tympanostomy tube insertion affords symptomatic relief, suggests that a dysfunctional eustachian tube plays a large role in OM. The adult eustachian tube is larger, contains more elastin and traverses 45 degrees from the temporal bone to the nasopharynx, compared to the child’s smaller eustachian tube with less elastin that traverses 10 degrees. [18]
The mechanism of theorized effects of manipulation on OM are unknown. Interference from swollen lymphatic tissues and/or muscle spasm may mechanically distort the eustachian tube or distort the small nerve fibers and blood vessels which serve the middle ear. Manipulation may relax muscle spasm and allow normal lymph, nerve and blood to flow. Also, Froehle states “Eustachian tube function depends upon appropriate contraction of the tensor veli palatine muscle, which in turn depends upon proper function of the mandibular branch of cranial nerve V, which in turn is dependent upon proper alignment and movement of the occiput and upper cervical vertebrae as the nucleus of the spinal trigeminal tract extends down to the level of the upper cervical segments”. [17] These mechanisms suggest a mechanical and nerve dysfunction as a potential cause of OM for which manipulative therapy may be beneficial. Therefore, this case report has potentially two different mechanisms of success: establishing the cranial nerve V flow at the level of the upper cervical vertebra and improvement of the child’s lymphatic drainage. The possibility of spontaneous remission of OM cannot be ruled out.
The likelihood of spontaneous remission of conductive hearing loss in a case like this one is small. This is implied by a controlled trial of ear tubes (grommets), involving 55 children between 4 and 10 years of age, which found that within 6 months after insertion, the grommet ear and the control ear had the same average degree of hearing loss: 16 decibels. This hearing loss persisted for the entire five-year period of the study. [33] This suggests that complete spontaneous resolution of hearing loss over a period of eighteen months is unlikely.
While this represents only a single case, the suggestion it brings of normalization of auditory physiology by chiropractic manipulation is tantalizing. Additionally, it may represent a new method for monitoring the results of CMT in children with MEE or recurrent OME. A 1999 feasibility pilot study for clinical trials has suggested that performing consistent tympanometry and/or pneumatic toscopy in the chiropractic clinic setting may be impractical. [34] Most young children are uncooperative with repeated pneumatic otoscopy examinations. Attempting such examinations makes the performance of spinal manipulation more difficult due to vocalization and active resistance on the part of the patient. The availability of independent, non-medical practitioners in the audiology profession may present an opportunity to obtain reliable, objective criteria, on a pre- and post-treatment basis, for treatment effectiveness. An added advantage to this method would be that the patients would not come to associate the setting of the chiropractic clinic with an aversive stimulus (i.e.: an uncomfortable examination procedure). The major limitation of this measurement technique is that the minimum age for an accurate audiogram is approximately 5 years, so such studies of younger children would not be feasible
Conclusion
Conservative therapy such as chiropractic care with referral for audiology monitoring may offer children with otitis media and hearing loss a possible benefit of recovery from their condition without the concern of antibiotic side effects, antibiotic resistance, or risks of surgery and associated anesthesia.
Consent
Written informed consent was obtained from the patient for publication of this Case report and any accompanying images.
References:
Laufer AS, Metlay JP, Gent JF et al.
Microbial communities of the upper respiratory tract and otitis media in children.
MBio 2011;2(1):e00245-10Zemek R, Szyszkowicz M, Rowe BH.
Air pollution and emergency department visits for otitis media: a case-crossover study in Edmonton, Canada.
Environ Health Perspect 2010;118(11):1631-1636O’Brien MA, Prosser LA, Paradise JL et al.
New vaccines against otitis media: projected benefits and cost-effectiveness.
Pediatrics 2009;123(6):1452-1463Wolleswinkel-van den Bosch JH, Stolk EA, Francois M et al.
The health care burden and societal impact of acute otitis media in seven European countries: results of an Internet survey.
Vaccine 2010;28 Suppl 6:G39-G52O'Reilly RC, He Z, Bloedon E et al.
The role of extraesophageal reflux in otitis media in infants and children.
Laryngoscope 2008;118(7 Part 2 Suppl 116):1-9Miyashita C, Sasaki S, Saijo Y et al.
Effects of prenatal exposure to dioxin-like compounds on allergies and infections during infancy.
Environ Res 2011;111(4):551-558Bentdal YE, Haberg SE, Karevold G et al.
Birth characteristics and acute otitis media in early life.
Int J Pediatr Otorhinolaryngol 2010;74(2):168-172Post JC.
Genetics of otitis media.
Adv Otorhinolaryngol 2011;70:135-140Nelson HM, Daly KA, Davey CS et al.
Otitis media and associations with overweight status in toddlers.
Physiol Behav 2011;102(5):511-517Bonadio WA.
The evaluation and management of acute otitis media in children.
Am J Emerg Med 1994;12(2):193-206Daly KA, Hunter LL, Giebink GS.
Chronic otitis media with effusion.
Pediatr Rev 1999;20(3):85-93Kaleida PH; Rireman P,
Diagnostic assessment of otitis media.
Clinical Allergy and Immunology 2000; 15:260Williamson I.
Otitis media with effusion in children.
Clin Evid (Online ) 2011;2011Carlin S, Marchant D, Shurin P, et al:
Host factors and early therapeutic response in acute otitis media: Does symptomatic response correlate with bacterial outcome?
J Pediatri 1991, 118; 178-183Hoberman A, Paradise JL, Rockette HE et al.
Treatment of acute otitis media in children under 2 years of age.
N Engl J Med 2011;364(2):105-115Bliner L, Devereaux T.
Watchful waiting. A viable approach to acute otitis media.
Adv Nurse Pract 2009;17(10):39-40Froehle R.M.
Ear Infection: A Retrospective Study Examining Improvement From Chiropractic Care and Analyzing Influencing Factors
J Manipulative Physiol Ther 1996 (Mar); 19 (3): 169–177Degenhardt BF, Kuchera ML.
Osteopathic evaluation and manipulative treatment in reducing the morbidity of otitis media: a pilot study.
J Am Osteopath Assoc 2006;106(6):327-334Gouma P, Mallis A, Daniilidis V et al.
Behavioral trends in young children with conductive hearing loss: a case-control study.
Eur Arch Otorhinolaryngol 2011;268(1):63-66Dawes PJ, Welch D.
Childhood hearing and its relationship with tinnitus at thirty-two years of age.
Ann Otol Rhinol Laryngol 2010;119(10):672-676Browning GG , Rovers MM, Williamson I et al.
Grommets (ventilation tubes) for hearing loss associated with otitis media with effusion in children.
Cochrane Database Syst Rev 2010;(10):CD001801Teele D, Klein J, Pelton S, et al:
Effects of persistent middle ear effusion on development of speech and language.
Pediatr Res 1981; 68:869Ben-David J; Pdoshin L; Fradis M,
Tympanometry and audiometry in diagnosis of middle-ear effusion.
Ear Nose Throat J 1981 Mar; 60(3): 120-123Eliachar I; Jachims HSZ; Goldsher M; et al,
Assessment of longterm middle ear ventilation.
Acta Otolaryngo 1983 Jul-Aug; 96 (1-2): 105-12Harbert F; Young IM; Menduke H,
Audiologic findings in serous otitis media.
Eye Ear Nose Throat Mon 1970 Sep; 49(9): 409-11McCoul ED, Goldstein NA, Koliskor B et al.
A prospective study of the effect of gastroesophageal reflux disease treatment on children with otitis media.
Arch Otolaryngol Head Neck Surg 2011;137(1):35-41Abba K, Gulani A, Sachdev HS.
Zinc supplements for preventing otitis media.
Cochrane Database Syst Rev 2010;(2):CD006639Bronfort G, Haas M, Evans R, Leiniger B, Triano J.
Effectiveness of Manual Therapies: The UK Evidence Report
Chiropractic & Osteopathy 2010 (Feb 25); 18 (1): 3Ferrance, RJ and Miller, J.
Chiropractic Diagnosis and Management of Non-musculoskeletal
Conditions in Children and Adolescents
Chiropractic & Osteopathy 2010 (Jun 2); 18: 14Hawk C, Knorsa R, Lisi A, Ferrance RJ, Evans MW.
Chiropractic Care for Nonmusculoskeletal Conditions: A Systematic Review
With Implications For Whole Systems Research
J Altern Complement Med. 2007 (Jun); 13 (5): 491–512Pilsner R, Richardson M.
Improvements in hearing, speech, development and behavior following chiropractic in a 4 year old male.
Journal of Pediatric, Maternal and Family Health Chiropractic 2011;2011(1):14-22Brown CDB.
Improved hearing and resolution of otitis media with effusion following chiropractic care to reduce vertebral subluxation.
Journal of Pediatric, Maternal and Family Health Chiropractic 2009;2009(1):1-7)Brown MJ, Richards SH, Ambegaokar AG.
Grommets and glue ear: a five-year follow up of a controlled trial.
J R Soc Med 1978;71(5):353-356Sawyer CE, Evans RL, Boline PD et al.
A Feasibility Study of Chiropractic Spinal Manipulation Versus Sham Spinal Manipulation for Chronic Otitis Media with Effusion in Children
J Manipulative Physiol Ther 1999 (Jun); 22 (5): 292–298
Return to OTITIS MEDIA
Since 12-08-2015


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |