

Criteria to Screen for Traumatic Cervical Spine Instability:
A Consensus of Chiropractic RadiologistsThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Manipulative Physiol Ther. 2018 (Feb); 41 (2): 156–163 ~ FULL TEXT
Sarah Dion, DC, Maja Stupar, DC, PhD, Pierre Côté, DC, PhD,
Julie-Marthe Grenier, DC, PhD, John A. Taylor, DC
Institut Franco-Européen de Chiropraxie,
Toulouse, France.
Sarah.dion89@gmail.comOBJECTIVE: The purpose of this study was to establish consensus on a radiographic definition for cervical instability for routine use in chiropractic patients who sustain trauma to the cervical spine.
METHOD: We conducted a modified Delphi study with a panel of chiropractic radiologists. Panelists were asked to rate potential screening criteria for traumatic cervical spine instability when assessing cervical spine radiographs. Items rated as important for inclusion by at least 60% of participants in round 1 were submitted for a second round of voting in round 2. Items rated for inclusion by at least 75% of the participants in round 2 were used to create the consensus-based list of screening criteria. Participants were asked to vote and reach agreement on the final screening criteria list in round 3.
RESULTS: Twenty-nine chiropractic radiologists participated in round 1. After 3 rounds of survey, 85% of participants approved the final consensus-based list of criteria for traumatic cervical spine instability screening, including 6 clinical signs and symptoms and 5 radiographic criteria. Participants agreed that the presence of 1 or more of these clinical signs and symptoms and/or 1 or more of the 5 radiographic criteria on routine static radiographic studies suggests cervical instability.
CONCLUSION: The consensus-based radiographic definition of traumatic cervical spine instability includes 6 clinical signs and symptoms and 5 radiographic criteria that doctors of chiropractic should apply to their patients who sustain trauma to the cervical spine.
KEYWORDS: Joint Instability; Radiography; Spine
From the FULL TEXT Article:
Introduction
Each year, emergency departments in the United States and Canada manage more than 13 million trauma patients at risk of cervical spine injury. [1, 2] In the United States, an estimated 11,000 cervical spinal cord injury cases are diagnosed annually and approximately 800,000 cervical spine radiographs are ordered to screen for cervical spine injury. [3–5] Adults with blunt trauma have an annual incidence of cervical spine injury of 2% to 6%, and 0.2% to 0.6% are purely ligamentous injuries. [6]
The evaluation of cervical spine radiographs can be challenging because no standardized definition of traumatic cervical spine instability (TCSI) is available to clinicians. Although several clinical and radiological definitions are available, [7–13] there is a lack of consensus among experts about their validity. [14] For example, little is known about the screening and diagnostic accuracy of the commonly used definition proposed by White and Panjabi [11, 12]: “Clinical instability [as] the loss of the ability of the spine under physiologic loads to maintain its pattern of displacement so that there is no initial or additional neurological deficit, no other major deformity, and no incapacitating pain.” The absence of information on the reliability and validity of these definitions limit their clinical utility.
Validated prediction tools, such as the Canadian C-Spine Rule and the National Emergency X-Radiography in the Emergency Room Utilization Study (NEXUS) low-risk criteria, are available to clinically screen patients who sustained blunt trauma. [1] The purpose of these tools is to inform whether radiographs or computed tomography (CT) scans should be ordered in the emergency room for patients with acute cervical spine trauma. However, these tools do not provide criteria to evaluate cervical spine radiographs.
Although most radiographs reveal no signs of traumatic lesions, any delay in recognizing a cervical fracture/dislocation and segmental instability can lead to catastrophic damage [15, 16] including sensory impairment (monoparesia, hemiparesia), motor deficit (tetraplegia), microfractures, and dislocations (“subluxations”) >3 mm. [17] Although screening guidelines for imaging are available, no consensus or standardized criteria exist to diagnose TCSI on radiographs. In fact, it is estimated that 4% to 23% of patients experience a delay in their diagnosis because of inadequate radiographic evaluation, misinterpretation, or misdiagnosis. [3] Therefore, a standardized TCSI definition is needed to improve agreement among chiropractic clinicians and radiologists. The objective of this study was to develop a consensus-based radiographic definition of cervical instability for routine use in patients who sustain trauma to the cervical spine.
Methods
Study Design, Participants, and Data Collection
We conducted a modified Delphi study. The Delphi method is useful to collect expert opinions and create consensus. [18–26] We recruited a panel of North American chiropractic radiologists certified by the American Chiropractic Board of Radiology. All potential participants attended the annual American Chiropractic College of Radiology conference in September 2014 and our workshop on TCSI.
To be eligible, participants had to(1) have an active radiology practice;
(2) be in practice for at least 5 years;
(3) routinely interpret cervical spine series;
(4) have screened or diagnosed TCSI;
(5) write their radiological reports in English; and
(6) have written communication skills and computer literacy.All participants gave consent to participate in this study, which was approved by the Research Ethics Board of the Canadian Memorial Chiropractic College (No. 1408X02).
Potential participants attended a 1–hour workshop on TCSI, which was led by the principal investigator (S.D.). At the workshop, potential study participants were asked to complete a survey, which was used to collect baseline data and confirm eligibility (the inclusion criteria were collected on the survey). Data collected in the baseline survey included age, sex, year of certification as a chiropractic radiologist (ie, having Diplomate, American Chiropractic Board of Radiology [DACBR] certification), current practice location, full-time or part-time practice, type of practice (private practice, chiropractic college, retired), number of cervical spine radiographs interpreted per week, and number of traumatic cervical spine imaging cases interpreted per year.
Questionnaire Development
The baseline questionnaire included 62 clinical symptoms and radiographic findings commonly used to assess and define TCSI based on information taken from various authors. [1, 7–13, 27] The feasibility of administering the baseline questionnaire to chiropractic radiologists was pilot-tested in a sample of 3 experienced chiropractic radiologists (who did not participate in the main study). Pilot testing was done to ensure that the questionnaire was clear and easy to complete. Minor edits and modifications were made afterward based on feedback from the pilot test. For example, a “positive stretch test” was removed as a possible item for inclusion because that test is no longer clinically used.
Modified Delphi Methodology
The baseline questionnaire for the first round was distributed to participants at the workshop. Participants were asked to rate the importance of including items as criteria used to define TCSI when assessing cervical spine radiographs. Response options were based on a Likert scale and ranged from 1, indicating that it was the least important, to 5, indicating that it was the most important option. Items had to be rated as “important” or “most important” (4/5 or 5/5) by the majority of participants to be included in the consensus list of criteria. [28, 29] Participants were also asked to suggest additional items that should be included in the definition; these additional items were included in the next round for voting.
Items that were rated as important for inclusion in the list of criteria by at least 60% of the participants in round 1, as well as new items suggested by participants, were submitted for a second round of voting in round 2. The items rated as important for inclusion by at least 75% of the participants in round 2 were used to create the consensus-based list of screening criteria for round 3. During the last phase of the study (round 3), we asked participants to vote on whether they approved the list of consensus screening criteria. We also asked participants to indicate whether or not flexion and extension radiographs should be obtained in patients with chronic neck pain who may have TCSI (this question was asked because some radiologists and clinicians still routinely order flexion and extension radiographs). We performed a sensitivity analysis to assess the lack of clarity related to inclusion criteria with overlapping response options for 1 of our participants (ie, the 0–5 response category overlapped with the 5–10 response category for the number of cervical spine radiographs interpreted per week and the number of traumatic cervical spine imaging cases interpreted per year). [30, 31] The overlap in response options was due to a typographical error when preparing our baseline questionnaire. We assessed if our results changed when the lower of the overlapping response categories were excluded (ie, results were compared with and without voting responses of participants in the 0–5 response category).
Results
Participants
In 2014, the total number of chiropractic radiologist active members with the American Chiropractic Board of Radiologists was 200. Ninety-five chiropractic radiologists and residents attended the workshop and were invited to participate in the study. Forty-six percent of attendees (44/95) were interested in participating, and 29 of those met the inclusion criteria. Reasons for exclusions were not being a DACBR (1/15); being in practice less than 5 years (6/15); not routinely interpreting cervical spine series (8/15); not having evaluated TCSI (7/15); and not being in clinical practice (2/15). Some participants had more than 1 reason for exclusion.

Table 1 Seventy-six percent of round 1 participants (22/29) participated in round 2, and 69% (20/29) participated in round 3. The mean age of participants was 54.1 years (range: 35–65), and most participants were male (Table 1). Participants practiced in 3 countries and were in practice for an average of 19.9 years (range: 5–38).
Round 1

Table 2 In round 1, 75% of the panel agreed that 8 of 45 clinical history, 3 of 12 radiographic, and 1 of 5 measurement method items should be included in the consensus-based TCSI screening list of criteria (Table 2). Of patients with acute symptoms (1–14 days) and suspicion of TCSI, 89% rated flexion/extension radiographs as important. Similarly, 82% of participants rated magnetic resonance imaging (MRI) as important in evaluating patients with acute symptoms (1–14 days) who are suspected of having TCSI. In patients suspected of having TCSI with chronic symptoms (>3 months), 100% of the panel recommended that flexion/extension radiographs be used in the assessment.

Table 3 In round 1, 6 of 45 clinical history items, 3 of 12 radiographic criteria, 1 of 5 measurement criteria, and 2 of 8 diagnostic imaging modalities in a chronic context of suspected TCSI achieved more than 60% agreement among the panel (Table 3).
Participants recommended 3 new items/symptoms in round 1 for voting:
Assessment of the shape of the curve (C-curve or reserved, S-shaped, straight, lordotic).
Prevertebral soft tissues: The soft tissue in front of the vertebral bodies and behind the air shadow of the pharynx, larynx, and trachea is measured. The body landmarks are the anterior arch of the atlas; the inferior corners of the axis and C3; the superior corner of C4; and the inferior corners of C5, C6, and C7. [32]
Anterior-posterior open mouth lateral bending.
Round 2

Table 4 In round 2, 75% of the panel rated 7 of 14 clinical history items, 5 of 6 radiographic criteria, and 2 measurement methods (horizontal displacement and interspinous widening) as important to include in the consensus-based criteria for TCSI (Table 4). The panel recommended using flexion/extension radiographs (90.5%) only when assessing chronic stages of TCSI. No new items were suggested for voting in round 2.
Based on the voting results from round 2, the consensus-based list of criteria included the following items:
Signs and symptoms: Spinal cord symptoms with neck movement; a dangerous mechanism of injury; feeling of instability/shakiness or lack or control; incapacitating pain; a history of Ehler-Danlos, Marfan, or Down syndrome; neck get stuck or locks with movement and myelopathy.
Radiographic criteria: Horizontal translation of 1 segment over the other on neural lateral cervical spine radiographs of ≥3.5 mm, angular deformity on neutral lateral cervical spine radiograph of ≥11°, abnormal movement or alignment on flexion/extension radiographs, interspinous widening, and a kyphotic deformation of ≥11°.
Round 3
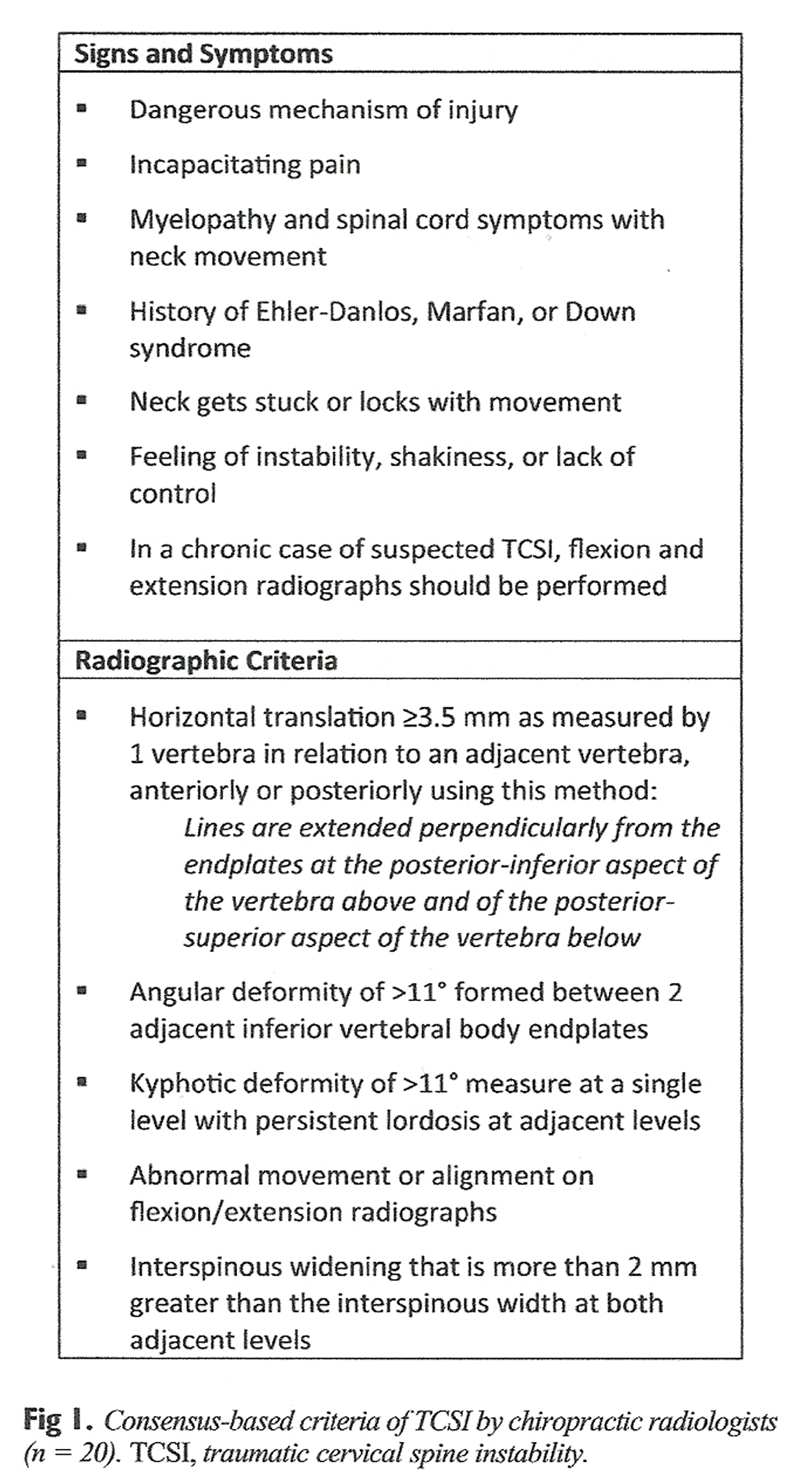
Figure 1 Eighty-five percent of the participants approved the final consensus-based list of criteria (Fig 1). This represents 10% of all the certified DACBRs in 2014 (20/200). The final consensus-based criteria for TCSI include 6 clinical signs and symptoms and 5 radiographic criteria. If 1 or more of the signs and symptoms are present in the history or if 1 or more of the radiographic criteria are present on the radiographic study, chiropractors and chiropractic radiologists should suspect TCSI.
Participants who disagreed with the final consensus-based list of criteria gave the following reasons for disagreement:(1) Dangerous mechanism of injury and incapacitating pain were not defined in Round 1;
(2) patients often exaggerate symptoms for a variety of reasons;
(3) a history of a connective tissue disease or a syndrome is not necessarily associated with traumatic instability; and
(4) the radiographic criterion “abnormal movement or alignment on flexion/extension radiographs” is vaguely described, and “interspinous widening” should be removed.Our sensitivity analysis indicated that our results did not change when the lower overlapping response categories were excluded. Therefore, we presented our results including all participants.
Discussion
This is the first consensus-based study to offer a radiographic definition of cervical instability for routine use in chiropractic patients who sustain trauma to the cervical spine. The participants agreed that the presence of 1 or more of the 6 clinical signs and symptoms or 1 or more of the 5 radiographic criteria on routine static radiographic studies suggests TCSI. The panel also agreed that flexion and extension radiographs should be obtained for patients with chronic neck pain and a past history of trauma.
Our results differ from the list developed by White and Panjabi. [11, 12] In 1975, White and Panjabi conducted the first biomechanical investigation designed to analyze clinical stability. The definition was amended in 1990: “Clinical instability is the loss of the ability of the spine under physiologic loads to maintain its pattern of displacement so that there is no initial or additional neurological deficit, no matter major deformity, and no incapacitating pain.”
Although their definition was not validated, it became the most commonly used definition for cervical instability. In contrast to the list proposed by White and Panjabi, our consensus-derived criteria do not include 2 elements (positive stretch test and flexion/extension studies) because these items were eliminated during pilot testing of the baseline questionnaire. A positive stretch test and flexion/extension studies may not be compatible with the current standards of practice when assessing patients with traumatic brain or cervical spine injuries. Our definition also differs from that of White and Panjabi because we considered only static routine radiographs, whereas they considered both static and flexion/extension radiographs. Finally, abnormal disk narrowing and a developmentally narrow spinal canal were eliminated in round 1, and nerve root damage was eliminated in round 2 of our consensus process. The clinical criteria that our expert panel retained from the definition of White and Panjabi are spinal cord damage and a dangerous loading anticipated (similar to our criterion: dangerous mechanism of injury). The panel agreed that horizontal translation of ≥3.5 mm and an angular deformity of ≥11° were important radiographic criteria.
One criterion retained by our panel is controversial and has been discussed widely in the literature. The panel voted to recommend flexion/extension radiographs to assess patients with chronic neck pain and a history of trauma. However, recent studies suggest that flexion/extension views are inadequate, unreliable, and inferior compared with CT and MRI in detecting ligamentous injury.
Sim et al [8] conducted a review in 2013 with 355 flexion/extension views of patients presenting to emergency rooms and found that 51% had an incomplete visualization of the C0 to T1 region. Moreover, they reported that in those with appropriate visualization, there was an insufficient range of motion (≥30° of angulation in both flexion and extension) in 44% of the studies. A recent systematic review conducted to investigate whether flexion/extension radiographs add diagnostic value to CT or MRI in the detection of cervical spine ligamentous injury concluded that flexion/extension radiography provides no additional information. [6] This evidence suggests that patients with potential instability identified on static radiographs should be referred for advanced imaging. This agrees with the American College of Radiology appropriateness criteria that conventional radiographs should be used as a screening method for identifying potential cervical spine trauma and flexion/extension views have a weak predictive ability. [33] If TCSI is suspected, the patient should be referred to the closest imaging center to undergo advanced imaging.
Strengths and Limitations
Our study had several strengths. First, we pilot-tested the round 1 questionnaire with 3 experienced chiropractic radiologists to ensure that the questionnaire was clear and simple to complete. Second, we used a modified Delphi technique to identify important clinical and radiographic criteria and to reach a consensus among an expert panel by surveying a panel of 29 chiropractic radiologists from various educational facilities and with different training backgrounds. Finally, we used a high threshold for consensus (85%), which provides a high level of confidence in the final list of criteria.
Limitations
We had 2 inclusion criteria with overlapping response options (ie, 0–5 and 5–10 response options in items that assessed potential frequency of screening for TCSI). However, our sensitivity analysis suggests that this issue did not bias our results. Second, the dropout rate was 24% in round 2 and 31% in round 3. It is possible that loss of follow-up of participants may have biased our results. As stated by Powell in 2003, “respondents with more extreme views are more likely to drop out of a Delphi study than participants with more moderate views.” [34] Third, chiropractic radiologists do not practice in emergency rooms, but rather in private practice, and consult mostly for patients attending care by doctors of chiropractic. Fourth, the list of signs and symptoms and criteria applied through the modified Delphi process was obtained from published literature, including literature from other clinical professions. Therefore, all imaging findings assessed by doctors of chiropractic and chiropractic radiologists must be interpreted in the context of findings from the clinical history and physical examination.
The panel recommended flexion and extension radiographs for patients with chronic neck pain and a history of trauma. However, the validity of this criterion is challenged by recent evidence, which suggests that CT or MRI studies should be ordered instead of flexion and extension views. Future research is needed to assess the validity and reliability of the consensus-derived criteria identified in this study.
Conclusion
Our study provides a consensus-based definition of traumatic cervical spine instability (TCSI). The screening criteria comprise 6 clinical signs and symptoms and 5 radiographic criteria.
Practical Applications
The participants agreed that the presence of 1 or more of the 6 clinical signs
and symptoms or 1 or more of the 5 radiographic criteria on routine static
radiographic studies suggests that there may be cervical spine instability.The panel also agreed that flexion and extension radiographs should be obtained
for patients with chronic neck pain and a history of trauma.In contrast to the list proposed by Panjabi and White, our consensus-derived
criteria do not include a positive stretch test and flexion/extension studies
because of comments from experienced chiropractic radiologists when
developing our questionnaire.Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): J.A.T., J.M.G., P.C., M.S.
Design (planned the methods to generate the results): M.S., P.C.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): M.S., P.C.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): S.D.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): S.D., M.S.
Literature search (performed the literature search): S.D.
Writing (responsible for writing a substantive part of the manuscript): S.D., M.S.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): M.S., P.C., J.A.T., J.M.G.
References:
Stiell, IG, Clement, CM, McKnight, RD et al.
The Canadian C-Spine rule versus the NEXUS low-risk criteria in patients with trauma.
N Engl J Med. 2003; 349: 2510–2518Côté, P, Cassidy, JD, and Carroll, L.
The epidemiology of neck pain: what we have learned from our population-based studies.
J Can Chiropr Assoc. 2003; 47: 284–290Ding, A, Abujudeh, H, and Novelline, RA.
Diagnosing cervical spine instability: role of the post-computed tomography scan out-of-collar lateral radiograph.
J Emerg Med. 2011; 40: 518–521Hoffman, JR, Mower, WR, Wolfson, AB, Todd, KH, and Zucker, MI.
Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National emergency x-radiography utilization study group.
N Engl J Med. 2000; 343: 94–99Murray, CJ, Atkinson, C, Bhalla, K et al.
The state of US health, 1990-2010: burden of diseases, injuries, and risk factors.
JAMA. 2013; 310: 591–608Sierink, JC, van Lieshout, WA, Beenen, LF, Schep, NW, Vandertop, WP, and Goslings, JC.
Systematic review of flexion/extension radiography of the cervical spine in trauma patients.
Eur J Radiol. 2013; 82: 974–981Farrokhi, MR and Motallebi, H.
Comparison of outcome of surgical and nonsurgical methods in the treatment of unstable traumatic lesions of the lower cervical spine.
Neurosciences (Riyadh). 2006; 11: 252–255Sim, V, Bernstein, MP, Frangos, SG et al.
The (f)utility of flexion-extension C-spine films in the setting of trauma.
Am J Surg. 2013; 206: 929–934Schmorl, G and Junghanns, H.
The human spine in health and disease.
Grune & Stratton, New York; 1971: 213–220Farfan, HF and Gracovetsky, S.
The nature of instability.
Spine (Phila Pa 1976). October 1984; 9: 714–719White, AA, Southwick, WO, and Panjabi, MM.
Clinical instability in the lower cervical spine: a review of past and current concepts.
Spine. 1976; 1: 15–27White, AA, Johnson, RM, Panjabi, MM, and Southwick, WO.
Biomechanical analysis of clinical stability in the cervical spine.
Clin Orthop Relat Res. 1975; 109: 85–96Uchida, K, Nakajima, H, Sato, R et al.
Cervical spondylotic myelopathy associated with kyphosis or sagittal sigmoid alignment: outcome after anterior or posterior decompression.
J Neurosurg Spine. 2009; 11: 521–528Bucholz, RW, Heckman, JD, Court-Brown, CM, and Tornetta, P.
Rockwood and Green’s Fractures in Adults. vol. 2. 7th ed.
Lippincott Williams & Wilkins, Philadelphia, PA; 2010: 1305–1307Fengbin, Y, Deyu, C, Xinwei, W et al.
Trauma-induced spinal cord injury in cervical spondylotic myelopathy with or without lower cervical instability.
J Clin Neurosci. 2013; 20: 419–422Gerrelts, BD, Petersen, EU, Mabry, J, and Petersen, SR.
Delayed diagnosis of cervical spine injuries.
J Trauma. 1991; 31: 1622–1626Delfini, R, Dorizzi, A, Facchinetti, G, Faccioli, F, Galzio, R, and Vangelista, T.
Delayed post-traumatic cervical instability.
Surg Neurol. 1999; 51: 588–595Hsu, CC and Sandford, BA.
The Delphi technique: making sense of consensus.
Pract Assess Res Evaluation. 2007; 12: 1–8Akins, RB, Tolson, H, and Cole, BR.
Stability of response characteristics of a Delphi panel: application of bootstrap data expansion.
BMC Med Res Methodol. 2005; 5: 37Balasubramanian, R and Agarwal, D.
Delphi technique- a review.
Int J Public Health Dent. 2012; 3: 16–25Du Plessi, E and Human, SP.
The art of the Delphi technique: highlighting its scientific merit.
Health Sa Gesondheid. 2007; 12: 13–24Gordon, TJ.
The Delphi method. (Available at:) (Accessed December 27, 2017)
http://www.gerenciamento.ufba.br/downloads/delphi_method.pdfHasson, F, Keeney, S, and McKenna, H.
Research guidelines for the Delphi survey technique.
J Adv Nurs. 2000; 32: 1008–1015Rowe, G and Wright, G.
The Delphi technique as a forecasting tool: issues and analysis.
Int J Forecasting. 1999; 15: 353–375Skulmoski, GJ, Hartman, FT, Krahn, J et al.
The Delphi method for graduate research.
J Inf Technol Educ. 2007; 6: 1–21Stanton, TR, Latimer, J, Maher, CG, and Hancock, MJ.
A modified Delphi approach to standardize low back pain recurrence terminology.
Eur Spine J. 2011; 20: 744–752Cook, C, Brismée, JM, Fleming, R, and Sizer, PS Jr.
Identifiers suggestive of clinical cervical spine instability: a Delphi study of physical therapists.
Phys Ther. 2005; 85: 895–906Murphy, MK, Black, NA, Lamping, DL et al.
Consensus development methods, and their use in clinical guideline development: a review. (1-88)
Health Technol Assess. 1998; 2: i–ivStreiner, DL, Norman, GR, and Cairney, J.
Health Measurement Scales a Practical Guide to their Development and Use.
(New York, NY: Oxford University Press)3rd ed. ; 2003Mack, N, Woodsong, C, MacQueen, KM, Guest, G, and Namey, E.
Qualitative Reasearch Methods: A Data Collector’s Field Guide.
Family Health International, Durham, NC; 2005in: M Lewis-Beck, A Bryman, TF Liao (Eds.)
The SAGE Encyclopaedia of Social Science Research Methods. vol. 1.
SAGE Publishing, Thousand Oaks, CA; 2004in: TR Yochum, LJ Rowe (Eds.)
Essential of Skeletal Radiology. Vol. 1. 3rd ed.
Lippincott Williams & Wilkins, ; 2004Daffner, RH, Weissman, BN, Wippold, FJ et al.
Expert Panels on Musculoskeletal and Neurologic Imaging, ACR Appropriateness Criteria Suspected Spine Trauma.
American College of Radiology, Reston, VA; 2012: 20Powell, C.
The Delphi technique: myths and realities.
J Adv Nurs. 2003; 41: 376–382
Return to RADIOLOGY
Since 1-12-2018


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |