Digital Tracking Algorithm Reveals the Influence
of Structural Irregularities on Joint Movements
in the Human Cervical SpineThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Clin Biomech (Bristol, Avon) 2018 (Jul); 56: 11–17 ~ FULL TEXT
Christian Balkovec, Jim Veldhuis, John W Baird, G Wayne Brodland, Stuart M McGill
Department of Kinesiology
University of Waterloo
200 University Avenue
Waterloo, ON, Canada
N2L 3G1Background: Disc height loss and osteophytes change the local mechanical environment in the spine; while previous research has examined kinematic dysfunction under degenerative change, none has looked at the influence of disc height loss and osteophytes throughout movement.
Methods: Twenty patients with pain related to the head, neck or shoulders were imaged via videofluoroscopy as they underwent sagittal-plane flexion and extension. A clinician graded disc height loss and osteophytes as "severe/moderate", "mild", or "none". A novel tracking algorithm quantified motions of each vertebra. This information was used to calculate intervertebral angular and shear displacements. The digital algorithm made it practical to track individual vertebrae in multiple patients through hundreds of images without bias.
Findings: Cases without height loss/osteophytes had a consistent increase in intervertebral angular displacement from C2/C3 to C5/C6, like that of healthy individuals, and mild height losses did not produce aberrations that were systematic or necessarily discernable. However, joints with moderate to severe disc height loss and osteophytes exhibited reduced range of motion compared to adjacent unaffected joints in that patient and corresponding joints in patients without structural irregularities.
Interpretation: Digitally-obtained motion histories of individual joints allowed anatomical joint changes to be linked with changes in joint movement patterns. Specifically, disc height loss and osteophytes were found to influence cervical spine movement in the sagittal plane, reducing angular motions at affected joints by approximately 10% between those with and without height loss and osteophytes. Further, these joint changes were associated with perturbed intervertebral angular and shear movements.
Keywords: Cervical spine; Disc height loss; Flexion/extension; Intervertebral disc; Osteophytes; Quantitative fluoroscopy
From the FULL TEXT Article:
Introduction
Spine health is determined through a complex interplay of a wide range of factors (Figure 1). For example, structural failure and resultant pathological disc height loss (Brinckmann and Horst, 1985; Michalek and Iatridis, 2012; Sharma et al., 2014) not associated with normal aging is an important biomarker for ongoing degenerative changes (Jarman et al., 2015) and at least in the lumbar spine, it increases facet stresses (Dunlop et al., 1984), potentially changes the disc stress profile (Adams et al., 1996b), and can shift load-bearing regions (Pollintine et al., 2004b). Disc height loss, injury or instability at a segment (Kirkaldy-Willis and Farfan, 1982; Neogi et al., 2008; Vernon-Roberts and Pirie, 1977; Videman et al., 1995) through this altered loading (Adams et al., 2000; Adams et al., 1996a; Adams et al., 1996b; Adams et al., 2006; Brinckmann and Grootenboer, 1991; Pollintine et al., 2004a; Pollintine et al., 2004b) can ultimately give rise to osteophytes (Kumaresan et al., 2001), another key anatomical marker. Ultimately, physical disruptions could manifest as pain, which can in turn affect movement of the cervical spine (de Vries et al., 2015). Despite much effort to understand spinal pathophysiological mechanisms, a number of important gaps remain in current knowledge. The goal of this study is to describe how disc height loss and osteophytes affect the motion of specific joints in the cervical spine in patients with pain to address some of these gaps.
Motion of the cervical spine has been investigated from a number of perspectives (Artz et al., 2015; Brown et al., 2005; van Mameren, 1988; White et al., 1975), and aberrant movement patterns have been correlated with degenerative grade (Cheng et al., 2007; Miyazaki et al., 2008), where indicated degeneration can include features associated with normal aging (Adams and Roughley, 2006). Perturbed motion has also been studied in the contexts of fusion (Dekutoski et al., 1994), herniation (Lao et al., 2015), and degeneration (Lee et al., 2015). Although factors such as disc height loss and osteophyte growth might reasonably be expected to influence spine motion, especially in patients experiencing pain, quantitative analyses of individual joint motions in such patients have been lacking.
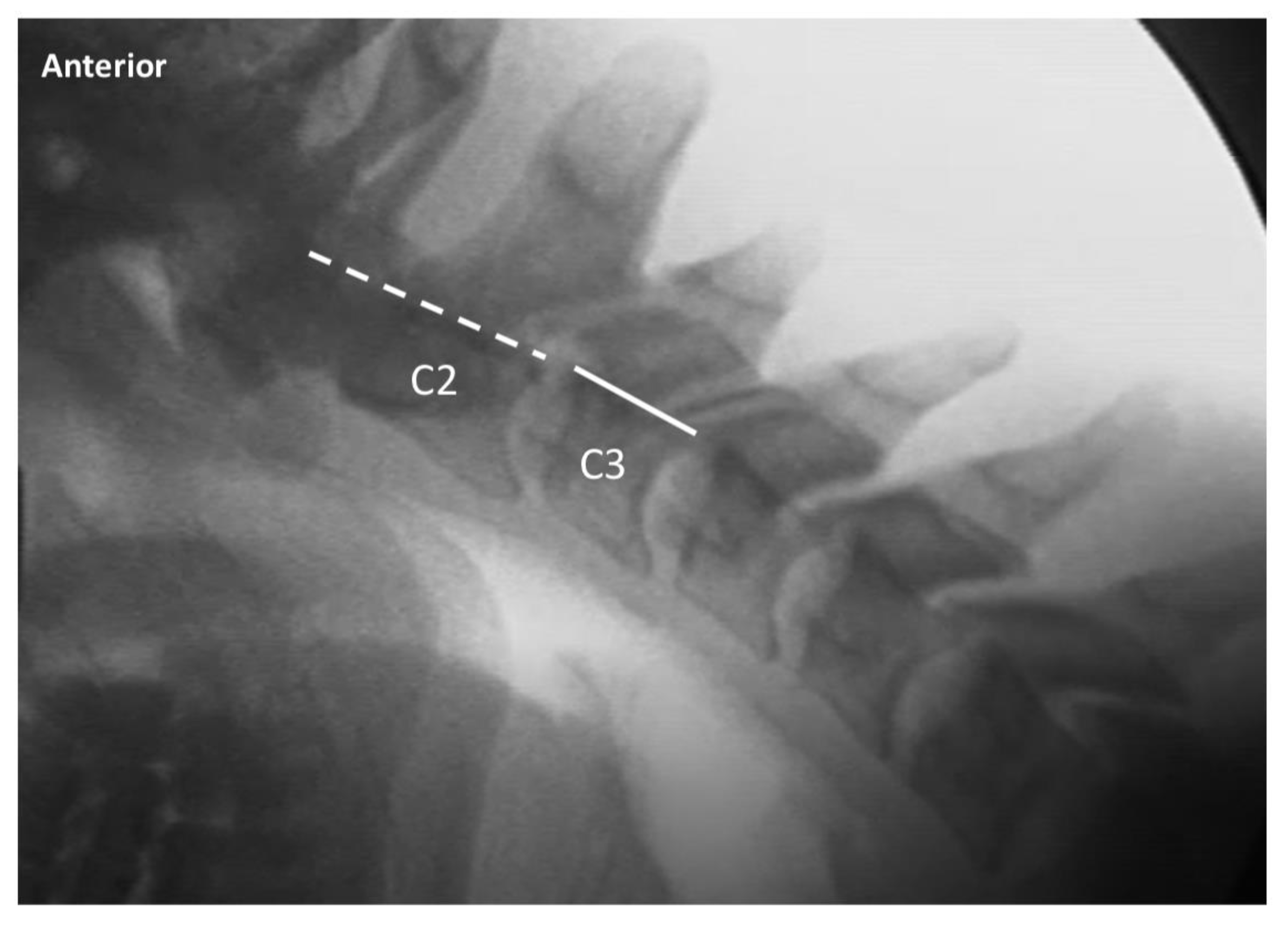
Fortunately, videofluoroscopic imaging allows the motions at individual intervertebral joints to be observed. Midrange movements can be visualized, a feature that static x-ray images of end positions cannot offer, and the kinematics of individual vertebrae can be obtained with accuracy, giving it an advantage over skin-mounted instrumentation. While tracking of individual vertebrae in fluoroscopic videos could allow the time course of individual joint motions to be quantified, manual tracking is expensive, time consuming, and impractical when the number of image frames or patients is large. Digital tracking algorithms have been previously developed (Bifulco et al., 2001; Muggleton and Allen, 1997; Wong et al., 2009; Wong et al., 2006; Zheng et al., 2004), but can rely heavily on operator skill, be difficult to implement, or use rigid template shapes that do not account for the effects of image distortion. A new digital algorithm developed by the authors (Balkovec et al., 2017) makes it practical to track the motions of vertebrae in a fluoroscopic video with relative ease and high accuracy, thereby overcoming these challenges.
The detailed tracking information the algorithm provides could lead to improved understanding of how specific anatomical features are associated with aberrant movements, and how such movements might produce downstream mechanical and physiological consequences (Figure 1). Here, we use this new kinematic data to assess the impact that disc height loss and osteophytes have on the sagittal plane kinematics of individual joints in the human cervical spine. We assess whether disc height loss and osteophytes are associated with diminished mobility in the affected segments.
Materials and Methods
Data Collection
Subjects selected for the study had experienced trauma and, at the time of the study, reported a chief complaint of pain related to their neck, head, or shoulders (Table 1). Patients gave informed consent for their image sequences to be used for research purposes, and all protocols were approved by the appropriate authorities. Radiation exposure for a typical image sequence was between 0.75mSv and 1.5mSv. Under care of a specialist, each patient was asked to start from a neutral position, flex his or her cervical spine fully, and then extend it before returning to the neutral position. Sagittal-plane image sequences of these cervical spine motions were collected using a Digital Motion X-Ray (DMX) that provided continuous x-ray at 70-90 kVp and 2-3.5 mA with a 40-inch flange focal distance. A 9-inch image intensifier (Precise Optics, Bay Shore, NY, USA) transferred the signal to a digital CCD camera outputting a 150dpi stream to a DICOM recorder (NAI Tech Products, Auburn, CA, USA). Data from 20 patients were analyzed.
Pre-trauma images were not available for the patients, and so disc height loss was classified manually based on clinical impression by a clinician certified to perform radiological assessments who had no prior interaction with the patients. Disc height loss and osteophyte severity were both classified separately as either none, mild, moderate, or severe. Of the 20 cases, 9 had no height loss at any of the levels visible in the radiographs (NH group), 8 had mild disc height loss at one level or more (MH group), and 3 had moderate or severe height loss at one level or more (DH group). Disc height loss and osteophyte severity appeared to be linked.
Motion Tracking
The fluoroscopy image sequences of interest typically consisted of 300 frames. Four points on the body of each vertebra were selected manually in the initial neutral-position image, and a digital template matching algorithm (Velduis and Brodland, 1999) developed specifically to track cervical vertebrae was used to quantify the kinematics of each vertebra (Balkovec et al., 2017). The raw coordinate values were filtered using a dual pass 2nd order Butterworth filter with a cut-off frequency of 1Hz, as determined by residual analysis (Wells, 1980). Relative joint angles were obtained for each set of image sequences using the technique described by Veldhuis and colleagues (Veldhuis et al., 2005), while shear displacement was calculated from the method of Frobin and colleagues (Frobin et al., 1996). Validation tests on this sequence of operations (Balkovec et al., 2017) showed that it produces RMS errors in intervertebral joint angle and shear no greater than 0.4° and 0.055mm, respectively.
Analysis
All intervertebral motions were normalized to the maximum total angular excursion of the quantified levels of each patients’ cervical spine. Intervertebral joint angles were plotted as timehistories and examined for features of clinical interest.
Results
Maximum angular excursions and normalized segmental motions for each patient are shown in Table 2. Like previous work on healthy individuals, they show a general consistent increase in intervertebral angular displacement from C2/C3 to C5/C6 (van Mameren, 1988) where the angular displacement of a lower segment is greater than any single segment above it. Group summaries in Table 3 show that the average angular displacement at C5/C6 (20.2% (SD=2.3%)) in the moderate to severe height loss group had notable differences compared to the group with no height loss (30.6% (SD=4.0%)). This group-wise comparison supports the notion that disc height loss and presence of osteophytes reduces motions in the affected joint. To assess whether further information can be garnered from individual patient records, we turn our attention to specific selected patients.
Severe Height Loss Case 1 (DH1)
Patient DH1 presented with moderate disc height loss at the level of C5/C6 and severe height loss at C6/C7 along with moderate anterior osteophytes at C5/C6 and severe at C6/C7 (Figure 2). As the time history shows, flexion occurred primarily about the C2/C3 and C4/C5 joints initially, followed by C3/C4 and C5/C6 motions. In extension, motion about the C5/C6 joint stopped, while motion about the adjacent (C4/C5) joint continued (Figure 2, see video, Supplemental Video 1). Total angular displacement for the C2/C3, C3/C4, C4/C5 and C5/C6 joints were 11.8°, 10.6°, 13.1°, and 8.1° respectively (angular displacement at C6/C7 could not be quantified because C7 moved out of the field of view). This case illustrates height loss being associated with osteophytes and reduced motion.
Severe Height Loss Case 2 (DH2)
DH2 presented with moderate disc height loss at C4/C5 and C6/C7 and severe height loss at C5/C6 (Figure 3). Osteophyte growth was evident anteriorly and classified as mild at C4/C5, moderate at C6/C7 and severe at C5/C6. Due to C7 moving out of the field of view during sagittal plane motions, the angular displacement of the C6/C7 joint could not be quantified. The smallest angular displacement occurred about C5/C6 where there was severe height loss (see video, Supplemental Video 2). Total angular displacement for the C2/C3, C3/C4, C4/C5, and C5/C6 joints were 15.1°, 12.5°, 12.9°, and 9.6° respectively. This case illustrates a correlation between the degree of disc height loss and the extent of motion loss, and is consistent with other cases, such as DH3.
Severe Height Loss Case 3 (DH3)
DH3 presented with moderate height loss at C4/C5 and severe height loss at C5/C6. There was also severe height loss at C6/C7 but due to the positioning of C7, it could not be tracked, as it did not stay within the field of view. Moderate levels of osteophytic lipping were evident at C4/C5, with severe levels at C5/C6 and C6/C7. There was also a kyphotic deformity of the neck in the patient’s neutral posture (Figure 4). The overall range of motion of the neck was severely limited, with most of the motion being qualitatively observed at the craniocervical junction. During flexion, a small amount of motion occurred at C5/C6, the osteophytes at the anterior margins of both vertebral bodies however, appeared to make contact and prevent further motion. As the spine went into extension, the facets of the C5/C6 joint appeared to come close to making contact (see video, Supplemental Video 3) and the range of motion of the segment was severely limited. In total, 7.6° of angular displacement occurred at the joint. Nearly all the angular displacement in extension occurred at the adjacent joint (C4/C5) that had less severe height loss and at the C3/C4 joint which had no height loss (Figure 4). Interestingly, most of the angular displacement (13.6°) occurred at the joint without height loss (C3/C4).
The relative shear measurements are also of note in Case DH3. The C2/C3 joint, where almost no angular displacement occurred, had the highest shear displacement (0.44mm in flexion and 0.27mm in extension). Joints C3/C4 and C4/C5 exhibited a small amount of anterior shear displacement (0.21mm) as the neck flexed, followed by posterior shear displacement (0.35mm) as it extended. Almost no shear displacement occurred at the C5/C6 joint, which had the most severe height loss (Figure 5).
This patient exhibited several noteworthy kinematic characteristics which may have gone unnoticed if only x-rays of end ranges of motion had been available rather than detailed plots of the time course of the individual joint movements.
Mild Height Loss Cases
In contrast to joints that had moderate/severe height loss, joints with mild height loss did not necessarily exhibit reduced mobility. In some instances (MH4, MH8), motions at joints with mild height loss were noticeably larger than at adjacent levels. There were also instances, such as MH3 (Figure 5, see video, Supplemental Video 4) and, MH4 (Figure 6, see video, Supplemental Video 5) where the pattern of consistent angular increase with descending segment level found in patients with no height loss was contravened, and there was less displacement at the C5/C6 joint than at the C4/C5 joint. The limited mobility of the C5/C6 joint in MH3 under extension may have been due to a posterior lip on C6. The lack of mobility in MH4 was in extension, which could indicate facet joint stiffness. These two cases appeared to be unusual in that most cases where there was a non-consistent angular displacement increase with descending segmental level, the discrepancy was less than 6% of total range of motion.
Cases Without Height Loss
In all non-height loss cases, there was a general trend for a consistent increase in intervertebral angular displacement from C2/C3 to C5/C6, and even though these patients presented with pain, their average angular displacement for each level were within 1% of those reported by van Mameren (van Mameren, 1988) (Table 3).
Discussion
This study demonstrates the value of detailed time histories of individual joint motions for identifying connections between anatomy, pathology, and aberrant movement patterns in the human spine (Figure 1). For example, it shows that patients with mild height loss (n=8) did not necessarily follow the consistent angular displacement increase pattern of those with no height loss, nor did they necessarily exhibit diminished segmental mobility at reduced-height joints. In fact, some patients (MH3 and MH4) had unusually high mobility in segments exhibiting mild height loss, and in these cases ligament disruption may be a contributing factor. There were fewer osteophyte growths along the anterior and posterior margins of their vertebral bodies, suggesting that these growths represent relatively early degenerative changes (Kirkaldy-Willis and Farfan, 1982). A threshold at which disc height loss produces aberrant movement has not been established, although overall mobility appears to decline as degenerative features advance. Patients with moderate and severe height loss along with osteophytes (n=3; and always at the C5/C6 level) had notably reduced mobility compared to those without height loss. Thus, the study supports the association between the presence of moderate to severe disc height loss together with osteophytes and a reduction in segmental mobility.
This study confirms that when motion is reduced at one joint, either the overall motion of the cervical spine is reduced (Malakoutian et al., 2015), or adjacent segments compensate by providing increased motion. Neither outcome is ideal, as both have potential negative physiological and structural effects (Figure 1). For example, increased motion at adjacent joints can alter joint loading and initiate damage in facets or other components (Dunlop et al., 1984) – especially under repetitive action.
Structural failure is known to initiate progressive height loss (Brinckmann and Horst, 1985; Michalek and Iatridis, 2012; Sharma et al., 2014). Height loss, in turn, is associated with the presence of osteophytes (Neogi et al., 2008; Vernon-Roberts and Pirie, 1977; Videman et al., 1995), and in this study, osteophytes were observed in all individuals with severe height loss. The height loss-osteophyte connection evidently involves two steps: height loss alters segment loading (Adams et al., 2000; Adams et al., 1996a; Adams et al., 1996b; Adams et al., 2006; Brinckmann and Grootenboer, 1991; Pollintine et al., 2004a; Pollintine et al., 2004b), and as posited (Adams and Roughley, 2006) and supported by finite element investigations, these loading changes facilitate osteophyte growth (Kumaresan et al., 2001). In the lumbar spine, disc height loss is associated with radial bulging of the annulus (Brinckmann and Grootenboer, 1991) and increased loading at the neural arch and vertebral margins (Pollintine et al., 2004b). It would be no surprise, then, to find that disc height loss in the cervical spine is associated with osteophytes and arthritic facets (Videman et al., 1995). While the present study does not establish a causal relationship between osteophytes and mobility, per se, it is consistent with the causal network shown in Figure 1 and with the concept that degenerative features associated with altered loading result in modified movements and mechanical properties (Tanaka et al., 2001). Further, the dysfunction that often accompanies early degeneration can induce physiological stabilization (Kirkaldy-Willis and Farfan, 1982) which can in turn alter mechanics of the spine (Al-Rawahi et al., 2011).
Interestingly, nearly half of the patients selected for this study because of reported head, neck or shoulder pain showed no sign of disc height loss. Those with no height loss or severe osteophyte growth (n=9) exhibit a consistent increase in intervertebral angular displacement from C2/C3 to C5/C6 (Table 2, Table 3), consistent with individuals without pain (van Mameren, 1988). Furthermore, the average intersegmental motions of patients in this study were within 1% of those without pain.
In future studies, the number of cases with moderate and severe disc height loss, might be increased so that our conclusions can be strengthened, and possible additional relationships identified. Disc height loss scoring might be enhanced, although in the absence of pre-trauma imaging, clinical classification is a viable option. While the disc height index (Frobin et al., 2002) offers an alternative approach to scoring, if patients had fractured vertebrae (and associated vertebral height loss) the index would not precisely reflect disc height loss itself. Normalizing disc height to the cumulative height of all the measured discs (Balkovec, 2016) is another possibility, but normal differences in disc height between levels would make interpretation of any inter-segmental differences challenging.
In summary, this study has shown that machine tracking of individual vertebrae motions in fluoroscopic image sequences can reveal intervertebral angular and shear displacements of clinical interest. Analyses of these intervertebral motions can, in turn, bolster our understanding of the factors (Figure 1) that govern the function and health of the human spine.
Acknowledgements
This study was funded by Natural Sciences and Engineering Research Council (NSERC) Discovery Grants to S.M.M. and G.W.B. The authors gratefully acknowledge Dr. Edward Cambridge D.C. for his assistance in grading patient disc height loss and osteophytes.
References:
Adams, M.A., Freeman, B.J., Morrison, H.P., Nelson, I.W., Dolan, P., 2000.
Mechanical initiation of intervertebral disc degeneration.
Spine 25, 1625-1636.Adams, M.A., McMillan, D.W., Green, T.P., Dolan, P., 1996a.
Sustained loading generates stress concentrations in lumbar intervertebral discs.
Spine 21, 434-438.Adams, M.A., McNally, D.S., Dolan, P., 1996b.
'Stress' distributions inside intervertebral discs.
The effects of age and degeneration.
The Journal of bone and joint surgery. British volume 78, 965-972.Adams, M.A., Pollintine, P., Tobias, J.H., Wakley, G.K., Dolan, P., 2006.
Intervertebral disc degeneration can predispose to anterior vertebral fractures
in the thoracolumbar spine.
Journal of bone and mineral research : the official journal of the American
Society for Bone and Mineral Research 21, 1409-1416.Adams, M.A., Roughley, P.J., 2006.
What is intervertebral disc degeneration, and what causes it?
Spine 31, 2151-2161.Al-Rawahi, M., Luo, J., Pollintine, P., Dolan, P., Adams, M.A., 2011.
Mechanical function of vertebral body osteophytes,
as revealed by experiments on cadaveric spines.
Spine 36, 770-777.Artz, N.J., Adams, M.A., Dolan, P., 2015.
Sensorimotor function of the cervical spine in healthy volunteers.
Clinical biomechanics.Balkovec, C., 2016.
Intervertebral Disc Height Loss: Outcomes and Implications, Kinesiology.
University of Waterloo.Balkovec, C., Veldhuis, J.H., Baird, J.W., Brodland, G.W., McGill, S.M., 2017.
A videofluoroscopy-based tracking algorithm for quantifying
the time course of human intervertebral displacements.
Computer methods in biomechanics and biomedical engineering, 1- 9.Bifulco, P., Cesarelli, M., Allen, R., Sansone, M., Bracale, M., 2001.
Automatic recognition of vertebral landmarks in fluoroscopic
sequences for analysis of intervertebral kinematics.
Medical & biological engineering & computing 39, 65-75.Brinckmann, P., Grootenboer, H., 1991.
Change of disc height, radial disc bulge, and intradiscal pressure
from discectomy. An in vitro investigation on human lumbar discs.
Spine 16, 641-646.Brinckmann, P., Horst, M., 1985.
The influence of vertebral body fracture, intradiscal injection, and
partial discectomy on the radial bulge and height of human lumbar discs.
Spine 10, 138-145.Brown, T., Reitman, C.A., Nguyen, L., Hipp, J.A., 2005.
Intervertebral motion after incremental damage to the
posterior structures of the cervical spine.
Spine 30, E503-508.Cheng, J.S., Liu, F., Komistek, R.D., Mahfouz, M.R., Sharma, A., Glaser, D., 2007.
Comparison of cervical spine kinematics using a fluoroscopic model
for adjacent segment degeneration. Invited submission from the
Joint Section on Disorders of the Spine and Peripheral Nerves,
March 2007.
J Neurosurg Spine 7, 509-513.de Vries, J., Ischebeck, B.K., Voogt, L.P., van der Geest, J.N., Janssen, M., 2015.
Joint position sense error in people with neck pain: A systematic review.
Manual therapy 20, 736-744.Dekutoski, M.B., Schendel, M.J., Ogilvie, J.W., Olsewski, J.M., 1994.
Comparison of in vivo and in vitro adjacent segment motion after lumbar fusion.
Spine 19, 1745-1751.Dunlop, R.B., Adams, M.A., Hutton, W.C., 1984.
Disc space narrowing and the lumbar facet joints.
The Journal of bone and joint surgery. British volume 66, 706-710.Frobin, W., Brinckmann, P., Leivseth, G., Biggemann, M., Reikeras, O., 1996.
Precision measurement of segmental motion from flexion-extension radiographs of the lumbar spine.
Clinical biomechanics 11, 457-465.Frobin, W., Leivseth, G., Biggemann, M., Brinckmann, P., 2002.
Vertebral height, disc height, posteroanterior displacement and
dens-atlas gap in the cervical spine:
precision measurement protocol and normal data.
Clinical biomechanics 17, 423-431.Jarman, J.P., Arpinar, V.E., Baruah, D., Klein, A.P., Maiman, D.J., 2015.
Intervertebral disc height loss demonstrates the threshold of major
pathological changes during degeneration.
European spine journal : official publication of the European Spine Society,
the European Spinal Deformity Society, and the European Section
of the Cervical Spine Research Society 24, 1944-1950.Kirkaldy-Willis, W.H., Farfan, H.F., 1982.
Instability of the lumbar spine.
Clinical orthopaedics and related research, 110-123.Kumaresan, S., Yoganandan, N., Pintar, F.A., Maiman, D.J., Goel, V.K., 2001.
Contribution of disc degeneration to osteophyte formation in the cervical spine:
a biomechanical investigation.
Journal of orthopaedic research : official publication of
the Orthopaedic Research Society 19, 977-984.Lao, L., Daubs, M.D., Takahashi, S., Lord, E.L., Cohen, J.R., Zhong, G., 2015.
Kinetic magnetic resonance imaging analysis of lumbar segmental motion at
levels adjacent to disc herniation.
European spine journal : official publication of the European
Spine Society, the European Spinal Deformity Society,
and the European Section of the Cervical Spine Research Society.Lee, S.H., Daffner, S.D., Wang, J.C., Davis, B.C., Alanay, A., Kim, J.S., 2015.
The change of whole lumbar segmental motion according to the mobility
of degenerated disc in the lower lumbar spine: a kinetic MRI study.
European spine journal : official publication of the European
Spine Society, the European Spinal Deformity Society,
and the European Section of the Cervical Spine Research Society
24, 1893-1900.Malakoutian, M., Volkheimer, D., Street, J., Dvorak, M.F., Wilke, H.J., 2015.
Do in vivo kinematic studies provide insight into adjacent segment degeneration?
A qualitative systematic literature review.
European spine journal : official publication of the European Spine Society,
the European Spinal Deformity Society, and the European Section
of the Cervical Spine Research Society 24, 1865-1881.Michalek, A.J., Iatridis, J.C., 2012.
Height and torsional stiffness are most sensitive to annular injury
in large animal intervertebral discs.
The spine journal : official journal of the North American Spine Society 12, 425-432.Miyazaki, M., Hong, S.W., Yoon, S.H., Zou, J., Tow, B., Alanay, A., 2008.
Kinematic analysis of the relationship between the grade of disc degeneration
and motion unit of the cervical spine.
Spine 33, 187-193.Muggleton, J.M., Allen, R., 1997.
Automatic location of vertebrae in digitized videofluoroscopic images of the lumbar spine.
Medical engineering & physics 19, 77-89.Neogi, T., Nevitt, M.C., Ensrud, K.E., Bauer, D., Felson, D.T., 2008.
The effect of alendronate on progression of spinal osteophytes and disc-space narrowing.
Annals of the rheumatic diseases 67, 1427-1430.Pollintine, P., Dolan, P., Tobias, J.H., Adams, M.A., 2004a.
Intervertebral disc degeneration can lead to "stress-shielding" of the
anterior vertebral body: a cause of osteoporotic vertebral fracture?
Spine 29, 774-782.Pollintine, P., Przybyla, A.S., Dolan, P., Adams, M.A., 2004b.
Neural arch load-bearing in old and degenerated spines.
Journal of biomechanics 37, 197-204.Sharma, A., Lancaster, S., Bagade, S., Hildebolt, C., 2014.
Early pattern of degenerative changes in individual components of
intervertebral discs in stressed and nonstressed segments of lumbar spine:
an in vivo magnetic resonance imaging study.
Spine 39, 1084-1090.Tanaka, N., An, H.S., Lim, T.H., Fujiwara, A., Jeon, C.H., 2001.
The relationship between disc degeneration and flexibility of the lumbar spine.
The spine journal : official journal of the North American Spine Society 1, 47-56.van Mameren, H., 1988.
Motion patterns in the cervical spine (Ph. D. Thesis).
Maastricht, The Netherlands: University of Limburg 150.Veldhuis, J.H., Brodland, G.W., Wiebe, C.J., Bootsma, G.J., 2005.
Multiview robotic microscope reveals the in-plane kinematics of amphibian neurulation.
Annals of biomedical engineering 33, 821-828.Velduis, J.H., Brodland, G.W., 1999.
A deformable block-matching algorithm for tracking epithelial cells.
Image and Vision Computing 17, 905-911.Vernon-Roberts, B., Pirie, C.J., 1977.
Degenerative changes in the intervertebral discs of the lumbar spine and their sequelae.
Rheumatology and rehabilitation 16, 13-21.Videman, T., Battie, M.C., Gill, K., Manninen, H., Gibbons, L.E., 1995.
Magnetic resonance imaging findings and their relationships in the thoracic
and lumbar spine. Insights into the etiopathogenesis of spinal degeneration.
Spine 20, 928-935.Wells, R.P.W., D.A., 1980.
Assessment of signal and noise in the kinematics of normal,
pathological and sporting gaits,
Proceedings of the Special Conference of the
Canadian Society for Biomechanics, pp. 92-93.White, A.A., 3rd, Johnson, R.M., Panjabi, M.M., Southwick, W.O., 1975.
Biomechanical analysis of clinical stability in the cervical spine.
Clinical orthopaedics and related research, 85-96.Wong, A., Dunk, N.M., Callaghan, J.P., 2009.
A systematic approach to feature tracking of lumbar spine vertebrae
from fluoroscopic images using complex-valued wavelets.
Computer methods in biomechanics and
biomedical engineering 12, 607-616.Wong, K.W., Luk, K.D., Leong, J.C., Wong, S.F., Wong, K.K., 2006.
Continuous dynamic spinal motion analysis.
Spine 31, 414-419.Zheng, Y., Nixon, M.S., Allen, R., 2004.
Automated segmentation of lumbar vertebrae in digital videofluoroscopic images.
IEEE transactions on medical imaging 23, 45-52.
Return to RADIOLOGY
Since 11-25-2021


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |