

Review Article: Best Practice Management
of Neck Pain in the Emergency Department
Part 6 of the Musculoskeletal Injuries Rapid Review SeriesThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Emerg Med Australas. 2018 (Dec); 30 (6): 754–772 ~ FULL TEXT
Kirsten STRUDWICK, Megan MCPHEE, Anthony BELL, Melinda MARTIN-KHAN, and Trevor RUSSELL
Emergency Department,
Queen Elizabeth II Jubilee Hospital,
Metro South Hospital and Health Service,
Brisbane, Queensland, Australia.
Neck pain and whiplash injuries are a common presentation to the ED, and a frequent cause of disability globally. This rapid review investigated best practice for the assessment and management of musculoskeletal neck pain in the ED. PubMed, CINAHL, EMBASE, TRIP and the grey literature, including relevant organisational websites, were searched in 2017. Primary studies, systematic reviews and guidelines were considered for inclusion. English-language articles published in the past 12 years addressing acute neck pain assessment, management or prognosis in the ED were included. Data extraction was conducted, followed by quality appraisal to rate levels of evidence where possible. The search revealed 2080 articles, of which 51 were included (n = 22 primary articles, n = 13 systematic reviews and n = 16 guidelines). Consistent evidence was found to support the use of 'red flags' to screen for serious pathologies, judicious use of imaging through clinical decision rule application and promotion of functional exercise coupled with advice and reassurance. Clinicians may also consider applying risk-stratification methods, such as using a clinical prediction rule, to guide patient discharge and referral plans; however, the evidence is still emerging in this population. This rapid review provides clinicians managing neck pain in the ED a summary of the best available evidence to enhance quality of care and optimise patient outcomes.
KEYWORDS: emergency medicine; evidence-based practice; neck injuries; neck pain; review
From the FULL TEXT Article:
Key findings
Highlight any ‘red flags’ for patients with neck pain to ensure serious pathology
is considered in the differential diagnosis.Adhere to validated clinical decision rules when ordering imaging.
For whiplash injury, ‘yellow flags’ and clinical prediction rules assist with
prognostication and follow up planning.
Introduction
Neck pain is the third largest contributor to years lived with disability in Australia, ranked behind only low back pain and major depressive disorder. It has a global prevalence of approximately 5%, equating to 33.6 million years lived with disability globally in 2010. [1] One subset of neck pain is those with whiplash-associated disorders (WAD). People with these injuries from traffic-related incidents have been increasingly seeking healthcare in EDs over the past three decades. [20] The economic costs for treatment of injuries from motor vehicle accidents exceed $350 million per year in Queensland, Australia, of which WAD is a major contributor. [3]
Most people with neck pain do not experience a complete resolution of symptoms; 50–85% of those who experience neck pain at some point will report neck pain again 1–5 years later, [2] indicating that the prognosis for certain neck pain cohorts may be worse. These can include the older population, those with prior neck pain episodes, poor psychological health, passive coping styles, higher initial pain levels, lower expectations of recovery and those who have compensatory or legal factors associated with WAD claims. [2, 4] WAD is often associated with disability, decreased quality of life and psychological distress. These non-physical components contribute significantly to non-recovery following a whiplash injury, and lead to a doubling of healthcare utilisation and considerably greater time off work compared to those with physical injury alone. [4-6] Given the high recurrence of neck pain and its associated disorders, the lifetime impact of neck pain should not be underestimated.
Cervical spine pain and injuries can be challenging for ED clinicians to accurately diagnose and manage. This can be due to the complex anatomy of the neck, the varying mechanisms that can lead to pain, and the risks of worsening a neurological injury if the cervical spine is not stabilised appropriately. Assessment for non-musculoskeletal red flag conditions or signs, cervical spine fractures or dislocations, disc disruptions and radiculopathies are the mainstay of ED care and usually require early imaging. However, in the absence of red flags, most neck pain conditions do not have a definitive pathoanatomical cause identifiable on imaging to diagnose the pain [7] or are non-traumatic in nature. These may include diagnoses such as acute wryneck, cervicogenic headaches and minor WAD. Given that ‘minor trauma’ of the neck makes up 85% of all neck injuries presenting to Queensland EDs, [8] the importance of a thorough history and clinical examination for non-catastrophic neck injuries in ED is crucial to form a diagnosis that will guide appropriate management.
Understanding the modifiable and non-modifiable risk factors, recovery patterns and prognosis of patients with neck pain and WAD is important in the ED, as these patients are a heterogeneous cohort with multifactorial aetiology. As such, patients require individualised assessments, treatments and referral plans by the treating clinicians in the ED to resolve the acute episode of pain, and to minimise the risk of recurrence or progression to chronicity. To address this, a rapid review was undertaken to identify the current best evidence for patients with non-catastrophic cervical spine injuries in the ED setting across the clinical cycle of care. This includes the assessment, imaging, treatment and considerations for discharge and follow up. This rapid review is the final review of a larger series. [9]
Methods
A rapid review, which is a streamlined approach to synthesising evidence, was conducted in October 2017 of the past 12 years of scientific literature on non-catastrophic neck injuries in the ED. Catastrophic neck injuries were defined as, ‘structural distortion of the cervical spinal column associated with actual (or potential) damage to the spinal cord, leading to severe neurologic sequelae’. [10] The search included primary articles, systematic reviews (SRs) and guidelines related to best practice management. Table 1 provides details of the literature search and study selection process for this review.
Study selection and analysis
The methodology for this review, including data collection, extraction methods and data analysis procedures, are outlined in a corresponding methodology paper. [9] Of the primary studies, only level II studies or above were included (i.e. highest level of intervention, diagnostic accuracy and prognostic studies), according to the National Health and Medical Research Council levels of evidence hierarchy. [11] SRs of all evidence levels were included. Guidelines were included if the methodology for development was clearly documented and reproducible.
Results
Search results
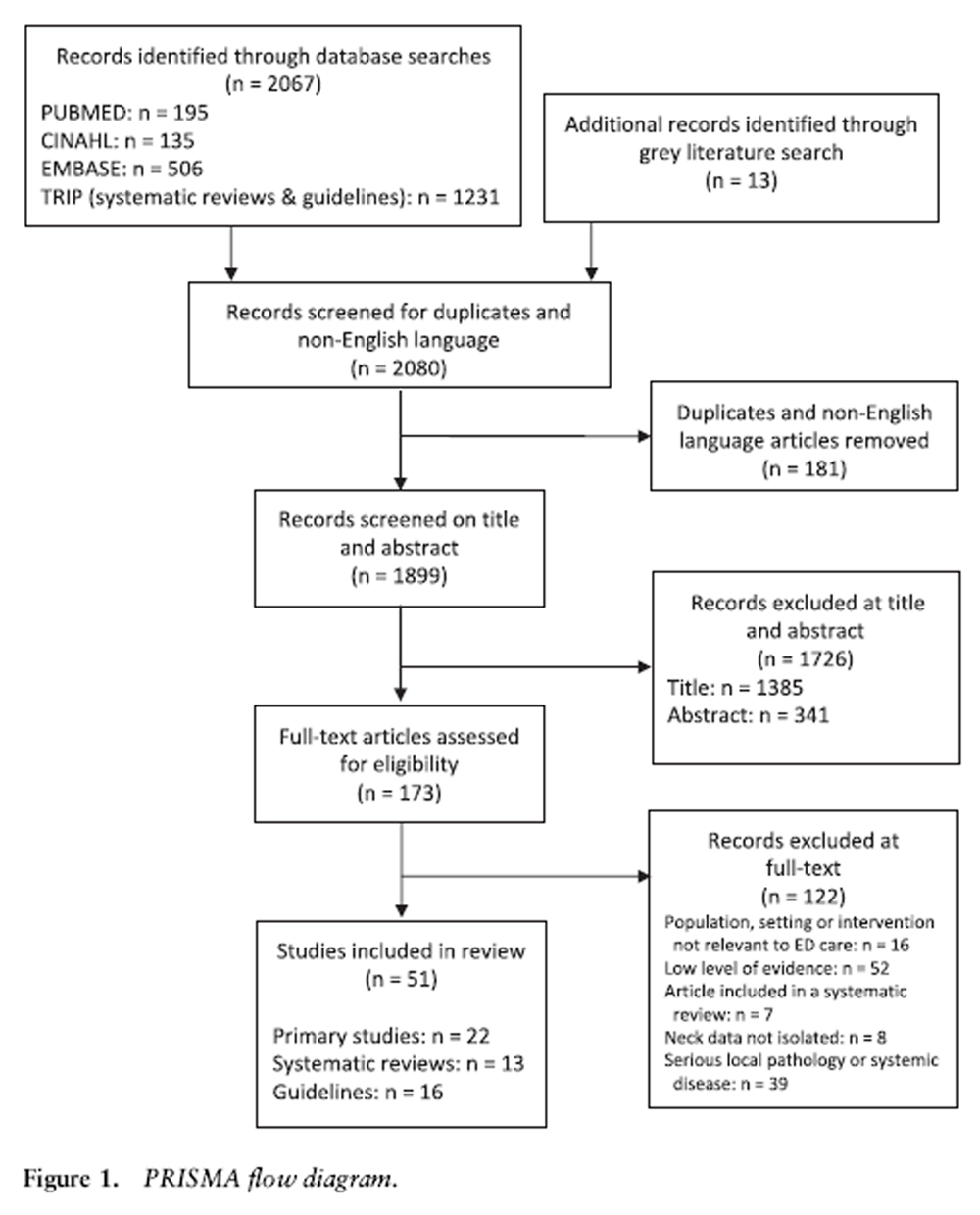
Figure 1 After excluding non-English and duplicate articles, the initial search yielded 1,899 articles for screening (Figure 1). At full text, 22 primary articles, [12-33] 13 SR articles [34-46] and 16 guidelines [47-62] were included in the review.
Article characteristics and levels of evidence
Characteristics of the included articles are displayed in Tables 2–4. Of the 22 primary articles, most were prognostic studies (n = 15), with the remainder being diagnostic accuracy studies (n = 4) and interventional (n = 3) trials, all of level II evidence. SRs were varied, including interventional (n = 6), prognostic (n = 3), diagnostic accuracy (n = 2), aetiological (n = 1) and mixed (n = 1) articles, with varying levels of evidence (n = 2 level I, n = 7 level II, n = 1 level III-3 and n = 3 level IV). All included guidelines were based on literature review and expert consensus, with variable comprehensiveness, and focused primarily on defining imaging appropriateness and recommending best practice interventions.
Evidence across the clinical cycle of care

Figure 2 Included articles covered a range of aspects of the clinical cycle of care for the ED management of acute neck pain and cervical injuries. The major recommendations are summarised and presented in Figure 2, and more detailed results from each individual article are available in Appendix S2.
Initial assessment
The patient history should include demographics, determining the mechanism, severity, nature and progression of the injury, location and/or radiation of pain and symptoms, red and yellow flags, neurological and other associated symptoms (e.g. dizziness, headache, loss of power, discoordination), prior history of neck problems/trauma/ surgeries, systems review (especially history of cancer, gout, arthritis, ankylosing spondylitis, recent infection, hypertension/cardiovascular diseases, diabetes, fractures, mental disorders), determining medication use and establishing functional and recreational pursuits/ requirements (n = 7 guidelines, n = 2 level IV SRs, n = 1 level II primary article). Validated scales for pain and functional assessment are reliable, sensitive to change, have prognostic value and therefore assist in quantifying disease severity and demonstrating changes in status across the patient’s stay (n = 1 guideline).
In the event of a suspected WAD and in addition to that suggested above, the grade of WAD should be quantified (as per the Quebec Task Force [61]). In addition, the administration of the Neck Disability Index Questionnaire, and relevant crash factors (i.e. speed, force direction/impact, driver/passenger, patient perception of severity), hyperarousal (measured by the post-traumatic diagnostic scale [25]) and recovery expectations should be elucidated (n = 1 guideline and n = 4 level II primary articles), as these factors highlight patients at risk of poorer recovery [24, 25] and indicate the need for earlier more-intensive interventions.
As well as identifying clinical findings to determine the potential for the presence of serious pathology, aspects of the initial physical examination (such as range of motion) should be evaluated over the episode of care in order to establish baselines and monitor changes over time. Clinicians should look for consistencies between patient-reported symptoms and physical findings that rule in or rule out a particular diagnosis, and use caution when considering any physical finding independently. Therefore, a thorough physical examination should include observation of posture, gait and a functional assessment (to rule out signs of cord compression or vascular event), vital signs (to rule out hypertension or fever), palpation for cervical spine midline tenderness, range of motion assessment and a neurological examination (upper limb motor, sensory and reflex assessment and cranial nerve testing (to rule out vascular events, space occupying lesions and so on)) (n = 7 guidelines).
If appropriate and considered valuable for clinical decision-making, further physical testing may include ligament integrity testing (the Sharp- Purser test performed by a trained clinician has acceptable levels of predictive value, sensitivity and specificity for suspected atlantoaxial instability); palpation of the internal and common carotid arteries (observation of asymmetry between sides, or a pulsatile, expandable mass typical of arterial aneurysm can be used as part of the work-up for carotid artery dysfunction in the context of other clinical findings; however, there are no meaningful diagnostic utility statistics available); neuro-dynamic and provocative positional testing (sustained end-range rotation is the most provocative and reliable test; however, its predictive ability is lacking) (n = 7 guidelines).
For a radiculopathy, four guidelines suggested a negative neurodynamic test (i.e. upper limb neural tension test) (sensitivity, 0.17–0.78; specificity, 0.72–0.83) may rule it out, while a positive Spurling test (sensitivity, 0.50; specificity, 0.86–0.93), traction/neck distraction test (sensitivity, 0.44; specificity, 0.90–0.97) and Valsalva test (sensitivity, 0.22; specificity, 0.94) will rule it in. [49, 50, 52, 56] Further to this, if suspicious of spinal cord injuries, include sharp and light touch, deep pressure, temperature and proprioceptive sensory function with specific identification of the level of sensory and/or motor deficit, along with strength testing, anal sphincter tone/sensation, reflexes and hip flexion weakness, all while providing manual cervical immobilisation and avoiding movement of the spine (n = 2 guidelines).
Imaging
Many articles focused on imaging, giving detailed recommendations depending on history, suspected pathology and prior radiographic findings, as detailed in Appendix S2 (n = 14 guidelines, n = 2 level II SRs, n = 1 level III-3 SR, n = 1 level IV SR and n = 3 level II primary articles). In general, the use of an imaging rule was recommended with first choice being the Canadian C-spine Rule (CCR), or alternatively the National Emergency X-radiography Utilisation Study (NEXUS) criteria (n = 6 guidelines, n = 1 level II SR, n = 1 level III-3 SR, n = 1 level IV SR and n = 2 level II primary articles). In addition, use of an imaging rule was suggested to significantly reduce both unnecessary radiation doses, as well as drastically reduce costs without compromising fracture diagnostics (n = 1 level II primary article).
The decision to use computed tomography (CT) versus plain radiography should be based on the suspected injury and severity, neurovascular integrity, likelihood of surgical referral, age of the patient and presence of other injuries or conditions (n = 8 guidelines, n = 1 level III-3 SR, n = 1 level IV SR and n = 1 level II primary article). Magnetic resonance imaging (MRI) is indicated in the case of severe trauma, history of cancer, multiple or progressive neurological abnormalities, previous neck surgery with progressive symptoms, suspicious fever with neck pain or suspected myelopathy (n = 6 guidelines and n = 1 level II SR).
For WAD injuries, radiography should only be used when indicated by an imaging rule and in grade III WAD (n = 4 guidelines). Early MRI is not considered prognostic, and therefore is not supported in WAD cohorts (n = 3 guidelines and n = 3 level II primary articles).
Treatment
In the initial treatment of neck pain, simple analgesia including paracetamol and NSAIDs was recommended (n = 4 guidelines and n = 1 level I SR). Muscle relaxants may also be considered in selected cases with evidence of muscle spasm, or moderate to severe pain unresponsive to NSAIDs (n = 3 guidelines), as may opioids in the presence of severe pain (n = 2 guidelines). There was little evidence of superiority between common analgesics compared to each other or over no medication. Heat and ice may also assist in reducing pain, with the choice based on patient preference (n = 2 guidelines and n = 1 level II primary article).
NOTE: According to a recent study in Annals of the Rheumatic Diseases 2017
Non-steroidal Anti-inflammatory Drugs for Spinal Pain: A Systematic Review and Meta-analysis:Commonly used non-steroidal anti-inflammatory drugs used to treat back pain provide little benefit and may make things worse according to new research from The George Institute for Global Health.
The findings of the systematic review, published in the Annals of the Rheumatic Diseases, reveal only one in six patients treated with the pills, also known as NSAIDs, achieve any significant reduction in pain.
The study is the latest work from The George Institute questioning the effectiveness of existing medicines for treating back pain. Earlier research has already demonstrated paracetamol does not speed recovery or reduce pain for acute low back pain, and opioids provide minimal benefit over placebo.Regarding therapeutic interventions, it was recommended that education should be provided initially on the nature of the injury and prognosis, along with reassurance to return to normal activities as soon as able (if appropriate) (n = 6 guidelines and n = 1 level II SR). Exercise was also commonly recommended, although the type of exercise varied from general aerobic, functional and strengthening exercise to specific range of motion movements, stretching and proprioceptive training (n = 5 guidelines and n = 2 level II SRs). There was conflicting evidence for the use of manual therapy, with some articles supporting its short-term use in patients with WAD (n = 2 guidelines), while another did not recommend it on the basis of lacking superiority to placebo (n = 1 guideline). Overall, rest, immobilisation (including soft collars, beyond shortterm use following trauma), acupuncture, manipulation, electrical stimulation and traction were not recommended (n = 3 guidelines).
Referrals and follow up
General follow-up considerations were discussed broadly (n = 5 guidelines, n = 2 level II SRs, n = 1 level IV SR and n = 2 level II primary articles). In the event of significant trauma, ankylosing spondylitis, fractures or neurological deficit, surgical consultation was recommended (n = 3 guidelines and n = 1 level IV SR). Referral for physiotherapy was recommended (n = 2 guidelines and n = 1 level II SR), along with a multimodal therapy approach including manual mobilisation techniques and exercise, particularly for those patients expected to experience a moderate to slow recovery with persistent impairments (n = 1 guideline). Though, early interventions may not be so important for outcomes in some whiplash and general neck pain cohorts (n = 1 level II SR and n = 1 level II primary article). Return to work should be based on the severity of the injury and the occupational requirements (n = 1 guideline). The chance of such return is worsened by the presence of depressive symptoms and other yellow flags, as well as medico-legal engagement (n = 2 level II primary articles). A summary of care received should be sent to the general practitioner and kept in the patient records, and ED staff should ensure all documentation and imaging is moved with the patient when they are transferred to another department or centre (n = 1 guideline).
In relation to WAD, conservative management is indicated, with suggestions that higher grades may require more comprehensive multiprofessional interventions (n = 1 guideline, n = 1 level II SR). However, at this stage these are not necessarily associated with improved outcomes (n = 1 level II primary article). Clinicians should be aware of the many proposed (and refuted) prognostic factors in patients with WAD, of which the most relevant are self-reported pain, disability, expectations of recovery and subjective crash severity (n = 1 guideline, n = 1 level II SR and n = 7 level II primary articles).
Discussion
This rapid review identified several key points integral to providing quality care for patients with neck pain and whiplash injuries in the ED. Broadly, this included conducting a thorough history and physical examination, particularly assessing for red flags and serious pathologies. This is essential given the quantity and seriousness of the differential diagnoses that can exist in patients with symptoms of neck pain. The use of validated clinical decision rules (CDRs) were recommended to guide the appropriate use of imaging in the ED. For whiplash patients, clinicians should be aware of yellow flags and the available clinical prediction rules that may indicate patients at risk of a poorer prognosis. The diagnosis of the severity of neck pain or whiplash should then guide decision-making for treatment and follow-up plans after the ED presentation, as shown in Figure 2.
Many articles included in this review focused on the assessment of patients with neck pain or whiplash, usually targeting a specific pathology (Appendix S2). The very specific focus in these articles may be due to the negative consequences associated with the many differential diagnoses in patients who present with neck pain to the ED (e.g. spinal cord injury, cervical artery dissection, cancer, infection). The focus of this review was musculoskeletal neck pain; however, the included articles consistently noted that failure to consider the diverse differential diagnoses for neck pain, or overreliance on a limited number of assessment items, is a potential danger in the assessment and management neck pain.
Similarly, the large volume of high-level evidence on the use of validated CDRs for imaging of neck pain in the ED is likely explained by the negative consequences of missing a serious neck injury, as well as the economic impact associated with the inappropriate use of imaging. The importance of reducing unnecessary imaging is also supported by national campaigns such as Choosing Wisely Australia, and national bodies such as the Australasian College for Emergency Medicine and The Royal Australian and New Zealand College of Radiologists who have endorsed the use of validated CDRs. [63] Despite the widespread acceptance of the rules, their application can vary considerably. One of the included studies found that the use of CT imaging of the cervical spine following a ground level fall was overused in their institution, with 20.7% (CCR applied) and 22% (NEXUS applied) of patients receiving unnecessary imaging. [14] They concluded that if CDRs had been applied consistently, it would have resulted in a reduction of annual nationwide imaging costs in the USA of $6.8–9.6 million (NEXUS applied) or $6.4–15.6 million (CCR applied), and a significant reduction in radiation dose exposure. Reasons for deviating from the criteria may occur due to a variety of reasons, such as patient request or demand, medical malpractice fears or a physician’s desire to document absence of an injury. [40, 64] However, interventions within the ED to improve compliance with the application of CDRs, such as regular education and teaching sessions, posters, policy change and ‘real-time’ reminders on radiology referrals, can reduce inappropriate imaging. [29, 65]
Compared to ‘assessment’ and ‘imaging’, there was a paucity of high-level evidence on effective interventions for neck pain in the ED. Once red flags are screened and sinister pathologies diagnosed or excluded, there were few recommendations as to how to manage nonserious neck pain patients within the ED setting in terms of controlling their pain, exercise prescription, advice and education or other treatment modalities. Three guidelines recommended classifying neck pain into broad categories, taking the focus away from establishing a specific structural diagnosis (Fig. 2). The more serious classifications of neck pain (i.e. those involving an identifiable structural pathology such as fractures, dislocations or nonmusculoskeletal sources of neck pain) will routinely follow an established management plan and referral pathway usually involving a tertiary or trauma centre. [57] However, it is the patients who fall into the lesser severity categories of neck pain where the evidence for management within the ED is lacking. This may be explained by the nature of nonserious neck pain, which can be episodic over a lifetime with variable recovery between bouts. [7] These patients will likely respond to minimal intervention (such as reassurance) and analgesia, and will not require intensive ongoing treatment or investigations. [56] A consistent finding in the review was the promotion of returning to work and activities that focused on regaining function, which are more effective than interventions without such a focus. Therefore, the role of the ED clinician in managing these patients is to ensure that advice is provided with careful consideration given to the length of sick leave provided on medical certificates, and to ensure linkages with appropriate follow up in the community are made.
There was a large focus in the included literature on the assessment and management of patients with WAD, which is likely due to the chronicity risks and subsequent financial implications associated with these injuries. Despite existing evidence-based strategies to manage these patients early in their presentation, actual practice within the ED is discordant with these recommendations. [64, 66] A national survey of ED consultants in the UK showed that there is a lack of consistency between verbal and written advice, and that the promotion of personal injury claims was a common feature of written advice. [66] Up to 50% of patients with WAD report ongoing pain and disability, and as such it is imperative that WAD is not treated as a homogenous diagnosis and that treatment is targeted to those who need it most. [4]
Among the literature on assessing patients with WAD, were several articles indicating that a clinical prediction rule may be useful to identify patients at higher risk of poor recovery. Consistent with this, a recent survey of Australian healthcare providers showed their ability to identify these high-risk WAD patients was poor. [67] Further, a recent study from The Netherlands highlighted that the majority of patients receive care in line with a moderate-risk, suggesting many low-risk patients are over-treated, and the high-risk patients are potentially undertreated. [68] Nevertheless, despite the development and validation of this clinical prediction rule, [24, 25] and the availability of other risk-stratification approaches (e.g. the STarTBack Screening Tool [69] or Örebro Musculoskeletal Pain Questionnaire [70]) there is not yet sufficient evidence in populations with WAD or neck pain to indicate that risk-stratified treatment provides improved outcomes. [71] However, there is growing evidence from other musculoskeletal conditions, such as low back pain, that a risk-stratified approach is both cost-effective and does improve outcomes compared to usual care, [72] but the evidence in neck pain is still emerging. With this in mind, the ED clinician could consider applying the principles from risk-stratification methods to assist in determining appropriate onward referral until firm guidance is in evidence.
Limitations
There are limitations of this rapid review in that strict inclusion and exclusion criteria were used in order to curtail the duration of the review process. This may have increased the risk of bias; however, the limitations in this instance also serve to provide the best and most recent evidence. For this rapid review on neck pain and whiplash, our criteria excluded catastrophic neck injuries, chronic neck pain and neck pain associated with serious local pathology or systemic disease, except where such studies were related to differential diagnosis of neck pain.
As a result, some topics (e.g. the ED management of spinal cord injuries or fractures/ dislocations) were not covered. Primary articles of a lower level of evidence were not included, which may have resulted in the exclusion of studies where randomised controlled trials or prospective research is unethical to perform. Similarly, systematic database searches were undertaken; however, a systematic and exhaustive hand-search was not, which may mean that some relevant articles were not included. While levels of evidence were allocated to studies, or existing levels of evidence within reviews and guidelines were acknowledged, a formal quality appraisal tool was not utilised to provide a strength of recommendation for each practice point. This was not performed due to the heterogeneity of study designs, and due to time constraints when opting to perform a rapid review.
Conclusion
This rapid review serves to provide a summary of the most recent and highest quality evidence supporting best practice for the assessment, use of diagnostic testing, pharmacological and non-pharmacological management, discharge considerations and advice for patients who present to ED with neck pain or whiplash injuries. There is abundant and strong evidence supporting the exclusion of serious pathology by screening for ‘red flags’ followed by the targeted use of imaging according to CDRs. Clinicians should be aware of ‘yellow flags’, which signify risk factors that may identify patients at risk of a poorer prognosis, along with injury severity, for more targeted discharge planning and referral.
Acknowledgements
Funding from the Emergency Medicine Foundation assisted with the completion of this rapid review.
Author contributions
KS, MM, MM-K and TR contributed to the conception and design of the work, acquisition, analysis and interpretation of data for the work, drafting and revising, final approval of the version to be published and agreement to be accountable for all aspects of the work. AB contributed to the conception and design of the work, drafting and revising, final approval of the version to be published and agreement to be accountable for all aspects of the work.
Competing interests
AB is a section editor for Emergency Medicine Australasia.
References:
Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, Shibuya K
Years Lived with Disability (YLDs) for 1160 Sequelae of 289 Diseases and Injuries
1990-2010: A Systematic Analysis for the Global Burden of Disease Study 2010
Lancet. 2012 (Dec 15); 380 (9859): 2163–2196Haldeman S, Carroll L, Cassidy JD, Schubert J, Nygren Å.
The bone and joint decade 2000–2010 task force on neck pain and its associated disorders.
Eur. Spine J. 2008; 17: 5–7.Motor Accident Insurance Commission.
The Motor Accident Insurance Commission Annual Report 2015–16. [Cited 1 Nov 2017.]
https://maic.qld.gov.au/wp-content/uploads/2016/10/MAIC-Annual-Report-2015-16_WEB.pdfSterling M.
Physiotherapy management of whiplash-associated disorders (WAD).
J. Physiother. 2014; 60: 5–12.Kenardy J, Heron-Delaney M, Warren J, Brown EA.
Effect of mental health on long-term disability after a road traffic crash:
results from the UQ SuPPORT study.
Arch. Phys. Med. Rehabil. 2015; 96: 410–7.Kenardy J, Heron-Delaney M, Charlton E, Bellamy N, Sterling M, Connelly L.
Adults’ adjustment to minor and moderate injuries following road traffic crashes.
CONROD Annual Scientific Meeting; 8 Jun 2012, Brisbane, Queensland, Australia.Jull G, Falla D.
Neck pain.
In: Brukner P, Clarsen B, Cook J et al., eds.
Brukner & Khan’s Clinical Sports Medicine, 5th edn.
Sydney: McGraw-Hill Education, 2017.Lang J, Dallow N, Lang A et al.
Inclusion of ‘minor’ trauma cases provides a better estimate of the total burden of injury:
Queensland trauma registry provides a unique perspective.
Injury 2014; 45: 1236–41.Strudwick K, McPhee M, Bell A, Martin-Khan M, Russell T.
Reveiw article: Methodology for a ‘rapid review’ series on musculoskeletal injuries
in the emergency department.
Emerg. Med. Australas. 2018; 30: 13–7.Langer PR, Fadale PD, Palumbo MA.
Catastrophic neck injuries in the collision sport athlete.
Sports Med. Arthrosc. Rev. 2008; 16: 7–15.National Health and Medical Research Council.
NHMRC Additional Levels of Evidence and Grades for Recommendations for Developers of Guidelines. 2009.
[Cited 23 Feb 2015.]
https://www.nhmrc.gov.au/_files_nhmrc/file/guidelines/developers/
nhmrc_levels_grades_evidence_120423.pdfAckland HM, Cameron PA, Wolfe R et al.
Outcomes at 12 months after early magnetic resonance imaging in acute trauma patients with
persistent midline cervical tenderness and negative computed tomography.
Spine (Phila Pa 1976) 2013; 38: 1068–81.Atherton K, Wiles NJ, Lecky FE et al.
Predictors of persistent neck pain after whiplash injury.
Emerg. Med. J. 2006; 23: 195–201.Benayoun MD, Allen JW, Lovasik BP, Uriell ML, Spandorfer RM, Holder CA.
Utility of computed tomographic imaging of the cervical spine in trauma evaluation of ground-level fall.
J. Trauma Acute Care Surg. 2016; 81: 339–44.Elliott JM, Courtney M, Rademaker A, Pinto D, Sterling MM, Parrish TB.
The Rapid and Progressive Degeneration of the Cervical Multifidus in Whiplash:
An MRI Study of Fatty Infiltration
Spine (Phila Pa 1976). 2015 (Jun 15); 40 (12): E694–700Garra G, Singer AJ, Leno R et al.
Heat or cold packs for neck and back strain: a randomized controlled trial of efficacy.
Acad. Emerg. Med. 2010; 17: 484–9.Girotto D, Ledic D, Strenja-Linic I, Peharec S, Grubesic A.
Clinical and medicolegal characteristics of neck injuries. Coll.
Antropol. 2011; 35 (Suppl 2): 187–90.Jull G, Kenardy J, Hendrikz J, Cohen M, Sterling M.
Management of acute whiplash: a randomized controlled trial of multidisciplinary stratified treatments.
Pain 2013; 154: 1798–806.Kivioja J, Jensen I, Lindgren U.
Early coping strategies do not influence the prognosis after whiplash injuries.
Injury 2005; 36: 935–40.Kongsted A, Sorensen JS, Andersen H, Keseler B, Jensen TS, Bendix T.
Are early MRI findings correlated with long-lasting symptoms following whiplash injury?
A prospective trial with 1-year followup.
Eur. Spine J. 2008; 17: 996–1005.Nederhand MJ, Hermens HJ, Ijzerman MJ, Groothuis KGM, Turk DC.
The effect of fear of movement on muscle activation in posttraumatic neck pain disability.
Clin. J. Pain 2006; 22: 519–25.Pajediene E, Janusauskaite J, Samusyte G, Stasaitis K, Petrikonis K.
Patterns of acute whiplashassociated disorder in the Lithuanian population after road traffic accidents.
J. Rehabil. 2015; 47: 52–7.Pieske O, Weinhold T, Buck J, Piltz S.
Seniority of the first-treating doctor does not influence the outcome of acute whiplash injury:
a prospective cohort study.
Eur. Spine J. 2010; 19: 1627–34.Ritchie C, Hendrikz J, Jull G, Elliott J, Sterling M.
External validation of a clinical prediction rule to predict full recovery and ongoing moderate/
severe disability following acute whiplash injury.
J. Orthop. Sports Phys. Ther. 2015; 45: 242–50.Ritchie C, Hendrikz J, Kenardy J, Sterling M.
Derivation of a clinical prediction rule to identify both chronic moderate/severe disability and full
recovery following whiplash injury.
Pain 2013; 154: 2198–206.Rose MK, Rosal LM, Gonzalez RP et al.
Clinical clearance of the cervical spine in patients with distracting injuries:
it is time to dispel the myth.
J. Trauma Acute Care Surg. 2012; 73: 498–502.Rydman E, Ponzer S, Ottosson C, Järnbert-Pettersson H.
Predicting nonrecovery among whiplash patients in the emergency room and in an insurance company setting.
Eur. Spine J. 2017; 26: 1254–61.Söderlund A, Åsenlöf P.
The mediating role of self-efficacy expectations and fear of movement and (re)injury beliefs
in two samples of acute pain.
Disabil. Rehabil. 2010; 32: 2118–26.Stiell IG, Clement CM, Grimshaw J et al.
Implementation of the Canadian C-spine rule: prospective 12 centre cluster randomised trial.
Br. Med. J. 2009; 339: 1071.Stiell IG, Clement CM, O’Connor A et al.
Multicentre prospective validation of use of the Canadian C-spine rule by triage nurses in
the emergency department.
Can. Med. Assoc. J. 2010; 182: 1173–9.Styrke J, Sojka P, Bjornstig U, Stalnacke BM.
Symptoms, disabilities, and life satisfaction five years after whiplash injuries. Scand.
J. Pain 2014; 5: 229–36.Tishler M, Levy O, Maslakov I, Bar-Chaim S, Amit-Vazina M.
Neck injury and fibromyalgia: are they really associated?
J. Rheumatol. 2006; 33: 1183–5.Ulbrich EJ, Eigenheer S, Boesch C et al.
Alterations of the transverse ligament: an MRI study comparing patients with acute whiplash
and matched control subjects.
AJR Am. J. Roentgenol. 2011; 197: 961–7.Daenen L, Nijs J, Raadsen B, Roussel N, Cras P, Dankaerts W.
Cervical motor dysfunction and its predictive value for long-term recovery in patients with
acute whiplash-associated disorders: a systematic review.
J. Rehabil. Med. 2013; 45: 113–22.Drescher K, Hardy S, Maclean J, Schindler M, Scott K, Harris SR.
Efficacy of postural and neckstabilization exercises for persons with acute whiplash-associated disorders:
a systematic review.
Physiother. Can. 2010; 60: 215.Gottesman RF, Sharma P, Robinson KA et al.
Clinical characteristics of symptomatic vertebral artery dissection: a systematic review.
Neurologist 2012; 18: 245–54.Gross A, Forget M, St George K et al.
Patient education for neck pain.
Cochrane Database Syst. Rev. 2012; CD005106.Holmes JF, Akkinepalli R.
Computed tomography versus plain radiography to screen for cervical spine injury: a meta-analysis.
J. Trauma 2005; 58: 902–5.Hurwitz, EL, Carragee, EJ, van der Velde, G et al.
Treatment of Neck Pain: Noninvasive Interventions: Results of the Bone and Joint Decade
2000–2010 Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S123–152Lekovic GP, Harrington TR.
Litigation of missed cervical spine injuries in patients presenting with blunt traumatic injury.
Neurosurgery 2007; 60: 516–23.Lukins TR, Ferch R, Balogh ZJ, Hansen MA.
Cervical spine immobilization following blunt trauma:
a systematic review of recent literature and proposed treatment algorithm.
ANZ J. Surg. 2015; 85: 917–22.Michaleff ZA, Maher CG, Verhagen AP, Rebbeck T, C-WC L.
Accuracy of the Canadian C-spine rule and NEXUS to screen for clinically important cervical spine injury
in patients following blunt trauma: a systematic review.
Can. Med. Assoc. J. 2012; 184: E867–76.Ojha HA, Wyrsta NJ, Davenport TE, Egan WE, Gellhorn AC.
Timing of physical therapy initiation for nonsurgical management of musculoskeletal disorders
and effects on patient outcomes: a systematic review.
J. Orthop. Sports Phys. Ther. 2016; 46: 56–70.Westerveld LA, Verlaan JJ, Oner FC.
Spinal fractures in patients with ankylosing spinal disorders:
a systematic review of the literature on treatment, neurological status and complications.
Eur. Spine J. 2009; 18: 145–56.Wong JJ, Côté P, Ameis A et al.
Are non-steroidal anti-inflammatory drugs effective for the management of neck pain and associated disorders,
whiplash-associated disorders, or non-specific low back pain? A systematic review of systematic reviews
by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration.
Eur. Spine J. 2016; 25: 34–61.Yu H, Cote P, Southerst D et al.
Does structured patient education improve the recovery and clinical outcomes of patients with neck pain?
A systematic review from the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration.
Spine J. 2016; 16: 1524–40.American College of Occupational and Environmental Medicine.
Cervical and thoracic spine disorders. 2016. [Cited 1 Aug 2016.] Available from URL:
https://www.dir.ca.gov/dwc/MTUS/ACOEM-Guidelines/Cervical-and-Thoracic-Spine-Disorders-Guideline.pdfAustralasian College for Emergency Medicine.
Guidelines on Diagnostic Imaging.
Melbourne: ACEM, 2012.Blanpied PR, Gross AR, Elliott JM et al.
Neck pain: revision 2017: clinical practice guidelines linked to the international classification
of functioning, disability and health from the orthopaedic section of the American Physical Therapy Association.
J. Orthop. Sports Phys. Ther. 2017; 47: A1–83.Bussieres AE, Taylor JA, Peterson C.
Diagnostic imaging guideline for musculoskeletal complaints in adults: an evidence-based approach part 3:
spinal disorders.
J. Manipulative Physiol. Ther. 2008; 31: 33–88.Bykowski J, Aulino JM, Berger KL et al.
ACR Appropriateness Criteria®: Plexopathy.
Reston, VA: American College of Radiology, 2016.Colorado Division of Workers’ Compensation.
Cervical Spine Injury Medical Treatment Guidelines.
Denver, CO: Department of Labor and Employment, 2014.Como JJ, Diaz JJ, Dunham CM et al.
Practice management guidelines for identification of cervical spine injuries following trauma:
update from the eastern association for the surgery of trauma practice management guidelines committee.
J. Trauma 2009; 67: 651–9.Daffner RH, Weissman BN, Wippold FJ et al.
ACR Appropriateness Criteria®: Suspected Spine Trauma.
Reston, VA: American College of Radiology, 2012.Goergen S, Grimm J.
Educational Modules for Appropriate Imaging Referrals:
Point of Care Tools for the Emergency Department.
Sydney: The Royal Australian and New Zealand College of Radiologists, 2014.Guzman J, Haldeman S, Carroll LJ, et al.
Clinical Practice Implications of the Bone and Joint Decade 2000-2010
Task Force on Neck Pain and Its Associated Disorders:
From Concepts and Findings to Recommendations
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S199–S212National Clinical Guideline Centre (UK) (2016)
Spinal Injury: Assessment and Initial Management
National Institute for Health and Care Excellence (UK), LondonNewman JS, Weissman BN, Angevine PD et al.
ACR Appropriateness Criteria®: Chronic Neck Pain.
Reston, VA: American College of Radiology, 2013.Rushton A, Rivett D, Carlesso L, Flynn T, Hing W, Kerry R.
International Framework for Examination of the Cervical Region for Potential of Cervical Arterial Dysfunction
Prior to Orthopaedic Manual Therapy Intervention.
Auckland: International Federation of Orthopaedic Manipulative Physical Therapists, 2012.Ryken TC, Hadley MN, Walters BC et al.
Radiographic assessment.
Neurosurgery 2013; 72(Suppl 2): 54–72.State Insurance Regulatory Authority.
Guidelines for the Management of AcuteWhiplash Associated Disorders: for Health Professionals, 3rd edn.
Sydney: NSWGovernment, 2014.Work Loss Data Institute.
Guideline Summary: Neck and Upper Back (Acute & Chronic). 2013. [Cited 1 Aug 2015.] Available from URL:
http://www.guideline.gov/content.aspx?id=47589&search=neck+and+upper+back+painNPS MedicineWise.
Choosing Wisely Australia, 2016. [Cited 1 Nov 2017.] Available from URL:
http://www.choosingwisely.org.au/homeCourtney DM.
Assessment and management of whiplash from the emergency and acute care setting:
care, questions, and future global research needs.
J. Orthop. Sports Phys. Ther. 2016; 46: 822–5.Desai S, Lui C, Krebs L, Kirkland S, Keto-Lambert D, Rowe B.
Effectiveness of implementing evidence based interventions to reduce C-spine imaging in the emergency department:
a systematic review.
CJEM 2017; 19: S56–7.Lamb SE, Williams MA, Withers E et al.
A national survey of clinical practice for the management of whiplash-associated disorders in UK emergency departments.
Emerg. Med. J. 2009; 26: 644–7.Griffin A, Jagnoor J, Arora M et al.
Evidence-based care (EBC) in highand low-risk groups following whiplash injury:
a multi-centre inception cohort study.
Momentum 2017 Physiotherapy Conference; 19–21 Oct 2017,
ICC Sydney, Australia: Australian Physiotherapy Association.Bier JD, Sandee-Geurts JJ, Ostelo RW, Koes BW, Verhagen AP.
Can primary care for back and/or neck pain in the Netherlands benefit from stratification
for risk groups according to the STarT Back Tool Classification?
Arch. Phys. Med. Rehabil. 2018; 99: 65–71.Hill JC, Dunn KM, Lewis M, et al.
A Primary Care Back Pain Screening Tool: Identifying Patient Subgroups For Initial Treatment
(The STarT Back Screening Tool)
Arthritis Rheum. 2008 (May 15); 59 (5): 632–641Linton SJ, Nicholas M, MacDonald S.
Development of a short form of the Örebro musculoskeletal pain screening questionnaire.
Spine (Phila Pa 1976) 2011; 36: 1891–5.Wingbermühle RW, van Trijffel E, Nelissen PM, Koes B, Verhagen AP.
Few promising multivariable prognostic models exist for recovery of people with non-specific neck pain
in musculoskeletal primary care: a systematic review.
J. Physiother. 2018; 64: 16–23.Hill JC, Whitehurst DG, Lewis M et al.
Comparison of Stratified Primary Care Management for Low Back Pain
with Current Best Practice (STarT Back): A Randomised Controlled Trial
Lancet. 2011 (Oct 29); 378 (9802): 1560–1571
Return to CHRONIC NECK PAIN
Return to NECK DISORDER GUIDELINES
Since 5-04-2019


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |