

The Effectiveness of Manual Therapy in Treating
Cervicogenic Dizziness: A Systematic ReviewThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Phys Ther Sci 2018 (Jan); 30 (1): 96-102 ~ FULL TEXT
OPEN ACCESS Khalid Yaseen, MSc, Paul Hendrick, PhD, Ayah Ismail, MSc, Mohannad Felemban, MSc, and Mansour Abdullah Alshehri, MSc
Department of Physical Therapy, Faculty of Physical Therapy, King Abdul Aziz University:
Jeddah, Saudi Arabia.
FROM: J Orthop Sports Phys Ther 2009Purpose: This review provides an evaluation of the evidence for the effectiveness of using manual therapy to treat cervicogenic dizziness.
Subjects and Methods: The literature was systematically searched on the May 2, 2016 using the following online databases: Medline, EMBASE, CINAHL and PEDro. This review included randomised controlled trials and compared the efficacy of manual therapy for the treatment of cervicogenic dizziness, compared to other types of intervention. This study measured changes based on dizziness intensity and frequency.
Results: The primary search found 30 articles, but only four articles met the inclusion criteria. Assessment of methodological quality was performed by two researchers using the PEDro scale. The level of evidence was determined using a recognised grading scale. Three out of the four articles were deemed to have high methodological quality, while the fourth was rated as moderate quality. The attributed level of evidence was moderate (level 2).
Conclusion: Manual therapy is potentially effective for managing cervicogenic dizziness. However, due to the heterogeneity of the results and techniques and the low number of studies, further research is recommended to provide conclusive evidence.
Keywords: Cervicogenic dizziness; Manual therapy; Mobilization.
From the FULL TEXT Article:
INTRODUCTION
Dizziness can be defined as disturbed postural awareness or vertigo, which is a perceived sense of motion. [1] Dizziness is a very common disability; an epidemiological study conducted in France found that 69.4% of the population had complained of dizziness during the past year. [2] Dizziness and vertigo are also common in the elderly population (>65), as revealed by the English Longitudinal Study of Ageing. [3] Dizziness has been classified into a number of types: dizziness originating from ear, nose and throat disorders, dizziness related to the nervous system, benign positional paroxysmal vertigo (BPPV) and cervicogenic dizziness, with some patients experiencing two or more of these types simultaneously. [4]
Cervicogenic dizziness can be distinguished from other forms of dizziness by an imbalance associated with a cervical spine abnormality that is aggravated or eased by movements or positions of the cervical spine. [5, 6] This type of dizziness can lead to a variety of disabling symptoms, which include faintness, unsteadiness, perceptions of spinning and disorientation. These symptoms may consequently cause serious health problems, including (1) physical injuries, i.e., as a result of falling and (2) psychological issues, e.g., depression and anxiety, fear of open spaces, inability to perform activities of daily living and employment difficulties. [7]
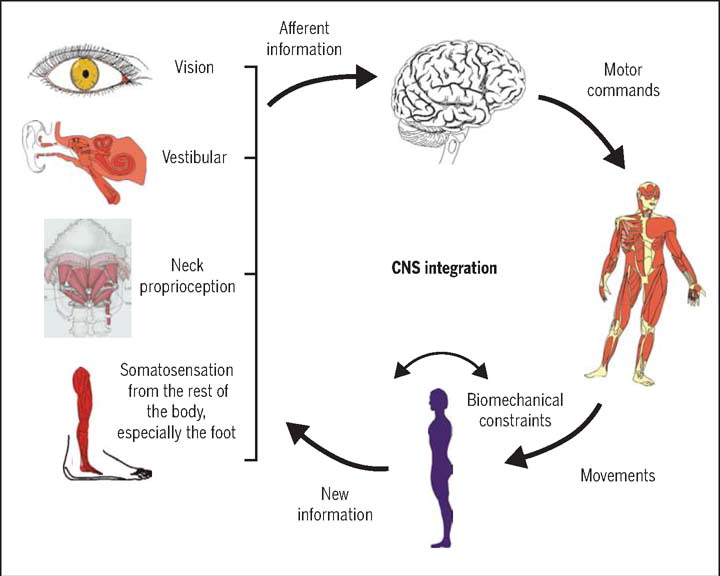
A significant connection has been identified between the cervical muscles, head position and postural stability; in particular, between the cervical spine and the vestibular and visual apparatus and different areas within the central nervous system. [6] However, there is conjecture as to whether cervicogenic dizziness can be distinguished as an independent condition. [8] Some researchers claim that dizziness is rarely cervicogenic [9], while others believe that this is one of the main causes of dizziness. [10] Recently, a review of the literature concluded that it seems very reasonable to acknowledge that cervical spine abnormality can often cause dizziness and vertigo. [8] For clinical purposes, the cervical spine can be targeted for interventions to treat suspected cervicogenic dizziness.
Manual therapy is the most common form of conservative therapy used to manage cervicogenic dizziness. [11] However, evidence of the effectiveness of this therapy remains inconclusive [12], with the last systematic review published in 2005. [13] The authors concluded that there is limited evidence of manual therapy being effective for cervicogenic dizziness and recommended further high quality clinical trials. A more recent review suggested that there is moderate evidence favouring the use of manual therapy for this specific condition. [4]
The current review is an update of the evidence presented in a previous review in 2005. [13] As the review published by Lystad et al. [4], evaluated manual therapy for cervicogenic dizziness but discussed the efficacy of manual therapy with and without vestibular rehabilitation. Therefore, their review differed from this current review in the question aiming to answer; as well as the inclusion criteria. Additionally, a more recent review of the literature was presented in 2015, which narratively discussed literature on cervicogenic dizziness, including management of the condition. [12] However, this review was no systematic nor did it evaluate the evidence for using manual therapy to treat this condition. A number of clinical trials have been published recently on this topic, suggesting several specific manual therapy techniques. [5, 11]
In 2008, a randomised control trial (RCT) evaluated the use of Mulligan’s sustained natural apophyseal glides (SNAGs) on patients with cervicogenic dizziness and the technique was found to be safe and effective in managing the condition. [5] In 2013, Reid et al. [11] published a novel clinical trial using the Maitland approach for cervical dizziness. Thus, synthesis and analysis of the updated evidence are required as well as a systematic review of the results of these studies. This paper provides a systematic review of the literature to evaluate evidence for the efficacy of manual therapy as an intervention for cervicogenic dizziness.
SUBJECTS AND METHODS
Studies consisted of RCTs examining the effect of manual therapy on patients with cervicogenic dizziness were included. All trials focussing on participants with dizziness or vertigo caused by an abnormality in the cervical spine were included in this review, including those with symptoms provoked by neck position or specific movements. Symptoms could consist of dizziness accompanied by pain stiffness. Other types of dizziness were excluded, including those originating from conditions related to the ear, nose and throat, the central nervous system, the cardiovascular system and BPPV.
This review included all clinical trials examining at least one of the following interventions:(1) mobilisation, i.e., slow velocity passive movement, ranging in amplitude from small to large, and
(2) manipulation, i.e. high velocity, small amplitude passive movement.All other hands-on manual treatments were included, even if combined with other treatments. Non-touch interventions were excluded. Primary outcome measures included
(1) the dizziness handicap inventory (DHI) and
(2) the visual analogue scale (VAS) for dizziness.Secondary outcome measures included
(1) the frequency of dizziness and
(2) the duration of dizziness.The following electronic bibliographic databases were searched in May 2016: MEDLINE (OVID, 1988 onwards), EMBASE (OVID, 1988 onwards), the Cochrane Central Register of Controlled Trials (CENTRAL, 1983 onwards), the Physical Therapy Evidence Database (PEDro), the Cochrane Controlled Trials Register in the Cochrane Library and the Cumulative Index for Nursing and Allied Health Literature (CINAHL). The search strategy included terms related to the intervention, such as manual therapy, mobilisation, manipulation, physiotherapy, chiropractic and massage, terms related to the condition of the cervical spine, such as dizziness, vertigo and cervicogenic, and terms related to the method of study, such as RCT, placebo, controlled trial, single blind, double blind and clinical trial. The search included only studies in English. Boolean operators were used to link the terms for searching. The search strategy followed the recommendations of the Cochrane collaboration. [14]
Full text versions of relevant studies were obtained and evaluated by two independent reviewers (K.Y. and P.H.). Reviewers decided whether the studies met the review criteria. Differences were resolved by mutual consensus. The assessment of the methodological quality of the included studies was made by both reviewers, using the PEDro scale. [15] The PEDro scale is a specialised tool for assessing the methodological quality of RCTs based on 11 “yes” or “no” questions. [15] The purpose of using this tool is to enable users to rapidly identify the internal validity of studies. [16] It also helps identify whether the statistical information provided in a study is sufficient for interpreting the results. [16] Data were extracted independently by two reviewers. A modified version of the JBI-MAStARI data extraction tool for experimental and observational studies was employed. The tool contained sections for each of the following: population, intervention, outcome measures and results. [17]
Due to the high level of heterogeneity, performing a meta-analysis was not possible. Therefore, the results were presented and analysed narratively. [14, 18] The qualitative analysis provided levels that were used to rate the scientific evidence as following the criteria developed by van Tulder et al. [18], which are presented below.
Level 1: Strong evidence—The findings are consistent and presented in multiple higher quality RCTs.
Level 2: Moderate evidence—The findings are consistent and provided in one higher quality RCT and one or more lower quality RCTs.
Level 3: Limited evidence—The findings are consistent and provided in one or more lower quality RCTs.
Level 4: No evidence—There are no RCTs, and if the results are conflicting.
Findings were considered consistent if 75% or more of the studies showed similar statistically significant results. [18] The quality of the studies were based on the PEDro scale.
RESULTS
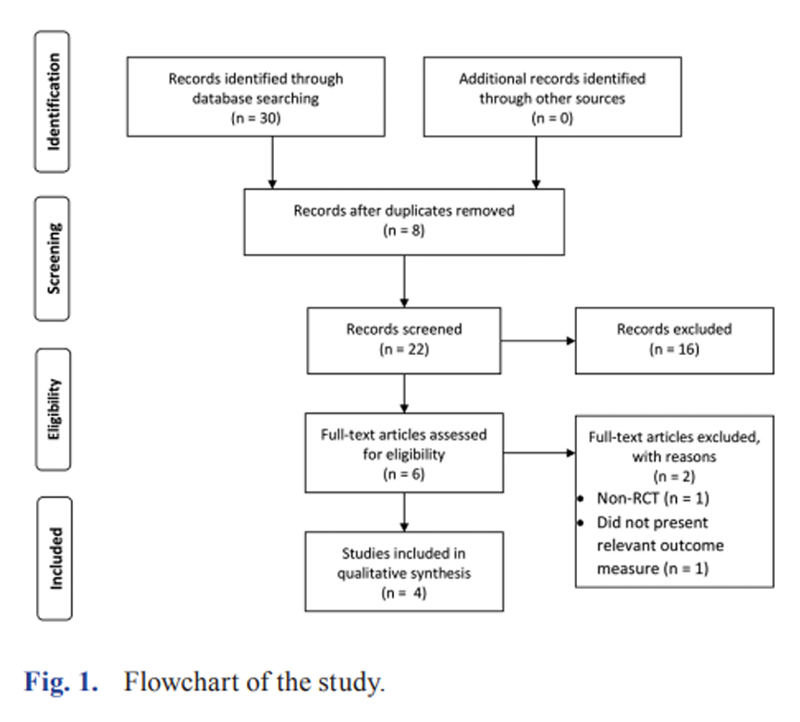
Figure 1

Table 1 Systematic search stages are illustrated in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [19] flow diagram (Figure 1). Initially, the search found 30 studies; however, after screening the titles and abstracts, four studies met the inclusion criteria. [5, 11, 20, 21] These included one trial published as a short-term, 12-week follow-up [11] and other study of same clinical trial [21] presented the results of the long-term effects of the intervention after one year.
The quality assessment results are presented in Table 1. The conflict between reviewers regarding the score was resolved by discussion. Methodological quality of the included studies was high. Two studies [5, 11] scored 9/10 on the PEDro scale, while one [21] scored 8/10. The lowest quality among the included studies was found for the study by Malmström et al. [20], which had a PEDro score of 5/10. The first criterion in the PEDro scale reflects the external validity of a study and is not usually reported in the score given. This criterion is answered as “yes” for all studies. Additionally, questions 10 and 11 are related to the interpretability of the results.
All included studies provided sufficient statistical data to interpret the findings. [5, 11, 21] None of the included trials blinded the therapists because this was not feasible for a manual therapy intervention. However, blinding patients to the intervention was frequently neglected, except in two trials. [5, 11]

Table 2
page 4Details about characteristics of the included studies are provided in Table 2. Participants: There were 136 participants across the included trials, 58.8% of whom were female. The study by Malmström et al. [20] included 17 patients, only two of which were male. The mean age for this study was 37 years, ranging from 26 to 49 years. The trial by Reid et al. [5] included 33 participants consisting of 22 females and 11 males. The mean age for the intervention group was 63.4 years and for the placebo group was 63.6 years. The third trial in this review [11] included 86 subjects, consisting of 43 females and 43 males. The mean age was 60 and 61 years for SNAGs and Maitland mobilisation groups, respectively, and the mean age for the placebo intervention group was 65.6 years.
Manual therapy was provided as the sole intervention in two studies. [5, 11] One used Mulligan’s SNAGs solely for the intervention group and compared the results to those from a control group that received a deactivated laser treatment. [11] The other study [5] used Mulligan’s SNAGs on one intervention group, Maitiland’s passive joint mobilisation on another intervention group and a placebo intervention for the control group. The purpose of having two intervention groups was to compare the two forms of manual therapy. Additionally, the study by Malmström et al. [20] used manual therapy as part of a multimodal intervention that included (1) a stabilisation techniques for the neck, trunk and shoulders and (2) a soft tissue treatment. This study compared a multimodal intervention to a delayed intervention.
Two of the included studies used the DHI, the VAS and dizziness frequency as outcome measures to assess changes in dizziness before and after the intervention. [5, 11] The study by Malmström et al. [20] assessed the intensity of dizziness using a grading system developed by the authors. The scale in this grading system represented the severity of symptoms as 0=no dizziness, 1=mild dizziness, 2=moderate dizziness, 3=severe dizziness and 4=very severe dizziness. The study also used the duration of symptoms (0–3 months, 4–6 months, 7–12 months, 13–24 months, 25 months –5 years and >5 years) as an outcome measure.
In general, the studies showed the consistent beneficial effects of using manual therapy as an intervention to treat cervicogenic dizziness. The level of evidence for this review is moderate (level 2) for supporting manual therapy as an effective intervention for the management of cervicogenic dizziness. [22] Variations were noted in the mode of interventions, outcome measures and follow-up periods. Two clinical trials used manual therapy on its own [5, 11], while another trial used it as part of a multimodal intervention. [20] The DHI and frequency of dizziness were used as outcome measures in two trials. [5, 11] Malmström et al. [20] trial reported a self-developed intensity measure to determine the duration of dizziness before and after the intervention as an outcome measure for dizziness. All studies reported results post-treatment and at 12 weeks, except for one study [21] that reported the results at one year, which adds further heterogeneity to the results. Therefore, due to high heterogeneity, performing a meta-analysis will not be possible.
DISCUSSION
The purpose of this review was to evaluate the evidence regarding the efficacy of manual therapy to manage cervicogenic dizziness. Four studies met the inclusion criteria. Three studies [5, 11, 20] reported short-term (12 weeks), significant improvement in dizziness intensity due to manual therapy (p=0.007; p<0.001; SNAGs p=0.01 and Maitland p=0.03). However, the change in intensity was not significant (SNAGs p=0.15 and Maitland p=0.1) when measured at a one-year follow-up. [21] These results may indicate that manual therapy is effective in the short term, but these effects do not persist long term. None of RCTs included in the previous reviews [4, 13] measured the outcomes of manual therapy on dizziness after the one-year follow-up, which shows a need to examine the long effects of the intervention.
The frequency of dizziness episodes showed a significant difference (SNAGs p=0.001; p=0.01 and Maitland p=0.01; p=0.02) in the short- and long-term measures of Reid et al.’s (2014; 2015) trials. [11, 21] The study in 2008, by Reid et al. [5], also showed a significant difference in the frequency of dizziness (p=0.03). The study by Malmström et al. [20] did not measure frequency of dizziness; therefore, the results were consistent with reports of decreased dizziness frequency in correlation with manual therapy. Furthermore, one study showed significant (p<0.001) change in the DHI using SNAGs [13], while another study showed insignificant changes in the DHI using SNAGs but significant improvement in the DHI (p=0.01) when using the Maitland technique. [11] Long-term effects of all techniques showed significant improvements in the DHI (SNAGs p=0.02; Maitland p=0.001). [21] The trial by Malmström et al. [20] did not include DHI in the outcome measures.
According to the criteria presented by van Tulder et al. [18], the evidence from the review is a level two (moderate evidence). This provides an update to the evidence presented in a previous review by Reid et al. [13], which was level three (limited) due to the poor methodological quality of the studies and conflicting evidence. Therefore, it is suggested that manual therapy be added to management protocols for cervicogenic dizziness. However, caution should be taken due to the limitations of the current evidence. Moreover, the current review presented higher quality clinical trials and more consistent results, although evidence was not level one (strong). The tool used to measure the level of evidence was the same in both reviews, and the results of the current review is consistent with the systematic review by Lystad et al. [4], which both found moderate levels of evidence supporting the use of manual therapy.
However, Lystad et al.’s review [4] differed from the current review in two main aspects:(1) the review focused on comparing manual therapy against manual therapy in addition to vestibular rehabilitation, and
(2) the inclusion criteria were different for the intervention and outcome measurements.Quality assessment of included studies was influenced by a number of factors, including blinding, concealment and sample size. All included studies stated that concealment of allocation was performed during the trials, which minimised the potential of selection bias. [23] Blinding of therapists was neglected in all the studies, and in the study by Malmström et al. [20], blinding was not reported either for therapists, patients or assessors. However, it was reported that blinding of therapists, patients and assessors can be problematic in non-pharmacological studies. [24] Especially in manual therapy interventions, blinding of therapists is usually not feasible. It was noted that the study by Malmström et al. [20] included a relatively small sample size (n=17), which has been shown to have an inaccurate large effect size that may induce publication bias. [25]
Three studies performed manual therapy alone and compared it to placebo interventions. The study by Malmström et al. [20] used a multimodal approach, which provided manual therapy alongside other physiotherapy interventions. This trial was poorly presented, especially regarding the study design and the reporting of treatment outcomes for dizziness. The study applied a number of interventions to the intervention group; however, it was not clear what amount of manual therapy each participant received or whether all participants received all forms of the interventions. Additionally, the trials presented in this review compared the intervention to placebo treatments [11, 21] or to a delayed treatment. [20] No trials compared manual therapy to other conservative interventions, such as neck exercises and stabilisation techniques for the neck and shoulder, for cervicogenic dizziness. [12] Therefore, it remains unclear how manual therapy relates to interventions for the management of the condition, which is an area that requires further investigation.
All studies measured dizziness using different tools. Reid et al. [5, 11, 21] used the same outcome measures in both trials to assess intensity using the VAS, which was found to have high test-retest reliability, as it scored 0.94 Cronbach’s Alpha index. [26] These two studies also used the DHI to assess the impact of dizziness on functional life, which was found to have high internal consistency and sensitivity of 89% in diagnosing dizziness. [27] This tool was found to be significantly correlated with balance and gait abnormalities. [28] These two trials [5, 11] also utilised frequency of dizziness as an outcome measure. Although this tool has been widely used, its validity and reliability have not been reported. The study by Malmström et al. [20] used a self-developed outcome measure for dizziness intensity, which has not previously been used. This tool is considered less descriptive in comparison to the VAS because it provides only five levels of intensity comparing to the 10 level in the VAS.
The populations included in the trials were diverse, and genders were represented almost equally, except for one study [20] in which 88.2% of the participants were female. These disparities in the sample could influence the overall external validity of the results. [29] The participants’ age was diverse, and two studies [5, 11] showed mean age ranges between 60 and 64 years. The other trial presented a mean age of 37 years. [20]
All studies reported that differential diagnosis relied on two facts:(1) having dizziness symptoms related to neck pain or stiffness and
(2) the exclusion of other forms of dizziness through clinical examinations.This was acceptable and consistent with recent evidence regarding differential diagnosis of the condition; however, no clinical tests or consensus guidelines have been published.
Interestingly, the clinical trial by Reid et al. [5] was performed by the same group of researchers as the two included studies [11, 21]; therefore, only one study was performed by other researchers. [20] This may introduce intervention bias, especially during manual therapy, because therapists’ techniques and performance may affect outcomes. It is important to know if other therapists at the same level of experience can produce the same effects. The study by Malmström et al. [20] is not sufficient to answer this query, because manual therapy was provided using a multimodal approach, which makes it difficult to compare to the other studies that used manual therapy alone for interventions groups. A number of factors could have affected this review. Due to clinical heterogeneity, a meta-analysis of the pooled results was not possible. Additionally, unpublished literature, such as conference proceedings, grey literature and guidelines, was included in the search, but languages other than English were not included.
The role of manual therapy in managing cervicogenic dizziness remains unclear. The study identified moderate evidence favouring the use of manual therapy to manage cervicogenic dizziness. The review also showed a potential for manual therapy to improve the intensity, frequency and dizziness handicap inventory (DHI) of cervicogenic dizziness. However, further high quality trials are recommended to provide more conclusive evidence in this regard. Additionally, there is a need for further investigations comparing manual therapy treatments to other conservative interventions in this regard. Also, it is recommended to study the effect of manual therapy in a multimodal intervention plans. That will provide a more conclusive evidence of the rule of manual therapy in the treatment of cervicogenic dizziness.
References:
Strupp M, Brandt T:
Diagnosis and treatment of vertigo and dizziness.
Dtsch Arztebl Int, 2008, 105: 173–180Bisdorff A, Bosser G, Gueguen R, et al.:
The epidemiology of vertigo, dizziness, and unsteadiness
and its links to co-morbidities.
Front Neurol, 2013, 4: 29Stevens KN, Lang IA, Guralnik JM, et al.:
Epidemiology of balance and dizziness in a national population:
findings from the English Longitudinal Study of Ageing.
Age Ageing, 2008, 37: 300–305Lystad RP, Bell G, Bonnevie-Svendsen M, et al.:
Manual therapy with and without vestibular rehabilitation
for cervicogenic dizziness: a systematic review.
Chiropr Man Therap, 2011, 19: 21Reid SA, Rivett DA, Katekar MG, et al.:
Sustained natural apophyseal glides (SNAGs) are
an effective treatment for cervicogenic dizziness.
Man Ther, 2008, 13: 357–366Treleaven J:
Sensorimotor disturbances in neck disorders affecting
postural stability, head and eye movement control.
Man Ther, 2008, 13: 2–11Yardley L, Todd A, Lacoudraye-harter M, et al.:
Psychosocial consequences of recurrent vertigo.
Psychol Health, 1992, 6: 85–96Yacovino DA, Hain TC:
Clinical characteristics of cervicogenic-related dizziness and vertigo.
Semin Neurol, 2013, 33: 244–255Cherchi M:
Infrequent causes of disequilibrium in the adult.
Otolaryngol Clin North Am, 2011, 44: 405–414, ixSomefun OA, Giwa OS, Bamgboye BA, et al.:
Vestibular disorders among adults in a tertiary hospital in Lagos, Nigeria.
Eur Arch Otorhinolaryngol, 2010, 267: 1515–1521Reid SA, Rivett DA, Katekar MG, et al.:
Comparison of mulligan sustained natural apophyseal glides and maitland
mobilizations for treatment of cervicogenic dizziness:
a randomized controlled trial.
Phys Ther, 2014, 94: 466–476Li Y, Peng B:
Pathogenesis, diagnosis, and treatment of cervical vertigo.
Pain Physician, 2015, 18: E583–E595Reid SA, Rivett DA:
Manual therapy treatment of cervicogenic dizziness:
a systematic review.
Man Ther, 2005, 10: 4–13van Tulder MW, Assendelft WJ, Koes BW, et al.:
Method guidelines for systematic reviews in the Cochrane
Collaboration Back Review Group for spinal disorders.
Spine, 1997, 22: 2323–2330PEDro scale.
http://www.pedro.org.au/wp-content/uploads/PEDro_scale.pdf
(Accessed 5 Sep. 5, 2016)de Morton NA:
The PEDro scale is a valid measure of the methodological
quality of clinical trials: a demographic study.
Aust J Physiother, 2009, 55: 129–133JBI data extraction form for Experimental/Observational studies.
http://joannabriggs.org/assets/docs/jbc/operations/
dataExtractionForms/JBC_Form_DataE_ExpObs.pdf
(Accessed May 15, 2016).van Tulder M, Furlan A, Bombardier C, et al.
Editorial Board of the Cochrane Collaboration Back Review Group:
Updated method guidelines for systematic reviews
in the cochrane collaboration back review group.
Spine, 2003, 28: 1290–1299Moher D, Liberati A, Tetzlaff J, et al.
PRISMA Group: Preferred reporting items for systematic
reviews and meta-analyses: the PRISMA statement.
PLoS Med, 2009, 6: e1000097Malmström EM, Karlberg M, Melander A, et al.:
Cervicogenic dizziness - musculoskeletal findings
before and after treatment and long-term outcome.
Disabil Rehabil, 2007, 29: 1193–1205Reid SA, Callister R, Snodgrass SJ, et al.:
Manual therapy for cervicogenic dizziness:
Long-term outcomes of a randomised trial.
Man Ther, 2015, 20: 148–156Furlan AD, van Tulder MW, Cherkin DC, et al.:
Acupuncture and dry-needling for low back pain.
Cochrane Database Syst Rev, 2005, 25: CD001351Berger VW:
Quantifying the magnitude of baseline covariate imbalances
resulting from selection bias in randomized clinical trials.
Biom J, 2005, 47: 119–127, discussion 128–139Boutron I, Tubach F, Giraudeau B, et al.:
Blinding was judged more difficult to achieve and maintain
in nonpharmacologic than pharmacologic trials.
J Clin Epidemiol, 2004, 57: 543–550Slavin R, Smith D:
The relationship between sample sizes and effect sizes
in systematic reviews in education.
Educ Eval Policy Anal, 2009, 31: 500–506. [Google Scholar]Dannenbaum E, Chilingaryan G, Fung J:
Visual vertigo analogue scale:
an assessment questionnaire for visual vertigo.
J Vestib Res, 2011, 21: 153–159Karapolat H, Eyigor S, Kirazli Y, et al.:
Reliability, validity, and sensitivity to change of Turkish
Activities-specific Balance Confidence Scale in patients
with unilateral peripheral vestibular disease.
Int J Rehabil Res, 2010, 33: 12–18Whitney SL, Wrisley DM, Brown KE, et al.:
Is perception of handicap related to functional performance
in persons with vestibular dysfunction?
Otol Neurotol, 2004, 25: 139–143Steckler A, McLeroy KR:
The importance of external validity.
Am J Public Health, 2008, 98: 9–10.
Return to VERTIGO and/or BALANCE
Since 3-04-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |