

Workers' Compensation, Return to Work, and
Lumbar Fusion for SpondylolisthesisThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Orthopedics. 2016 (Jan); 39 (1): e1-8 ~ FULL TEXT
Joshua T. Anderson, BS; Arnold R. Haas, BS, BA; Rick Percy, PhD;
Stephen T. Woods, MD; Uri M. Ahn, MD; Nicholas U. Ahn, MD
Department of Orthopaedics (JTA, NUA),
University Hospitals Case Medical Center,
Cleveland, Case Western Reserve University School of Medicine (JTA),
Cleveland, and the Ohio Bureau of Workers' Compensation (ARH, RP, STW),
Columbus, Ohio; and the
New Hampshire NeuroSpine Institute (UMA),
Bedford, New Hampshire.
This is an interesting follow-up to a 2011 study drawn from the
Ohio Bureau of Workers Compensation database.
[Startling New Study Reveals That Back Surgery Fails 74% of the Time]
In the 2011 study, two years AFTER surgery, only 26 percent had returned to work.
That translates to a resounding 74% failure rate!
In this current study, researchers reviewed the files of 686 workers who underwent fusion surgery for spondylolisthesis between 1993 and 2013, revealing that only 29.9% of them ever returned to work (for at least 6 months). The failure rate (meaning return-to-work) was 70.1%.
Clearly, it's time to consider more conservative approaches, like early referral for chiropractic care, long before they become chronic pain patients.
The Abstract:
Lumbar fusion for spondylolisthesis is associated with consistent outcomes in the general population. However, workers' compensation is a risk factor for worse outcomes. Few studies have evaluated prognostic factors within this clinically distinct population. The goal of this study was to identify prognostic factors for return to work among patients with workers' compensation claims after fusion for spondylolisthesis. The authors used International Classification of Diseases, Ninth Revision, and Current Procedural Terminology codes to identify 686 subjects from the Ohio Bureau of Workers' Compensation who underwent fusion for spondylolisthesis from 1993 to 2013.
Positive return to work status was recorded in patients who returned to work within 2 years of fusion and remained working for longer than 6 months. The criteria for return to work were met by 29.9% (n=205) of subjects. The authors used multivariate logistic regression analysis to identify prognostic factors for return to work.
Negative preoperative prognostic factors for postoperative return to work included:out of work for longer than 1 year before fusion (P<.001; odds ratio [OR], 0.16)
depression (P=.007; OR<0.01)
long-term opioid analgesic use (P=.006; OR, 0.41)
lumbar stenosis (P=.043; OR, 0.55); and
legal representation (P=.042; OR, 0.63).
Return to work rates associated with these factors were 9.7%, 0.0%, 10.0%, 29.2%, and 25.0%, respectively. If these subjects were excluded, the return to work rate increased to 60.4%. Editors Comment: Evidently, leaving a patient out-of-work for longer than a year is not an effective strategy, most likely contributing to their depression and opoid use, and probably to their desire to seek legal representation.
The 70.1% (n=481) of subjects who did not return to work had markedly worse outcomes, shown by higher medical costs, chronic opioid dependence, and higher rates of failed back syndrome, total disability, and additional surgery. Psychiatric comorbidity increased after fusion but was much higher in those who did not return to work. Future studies are needed to identify how to better facilitate return to work among similar patients with workers' compensation claims.
From the FULL TEXT Article:
Introduction
Lumbar fusion for spondylolisthesis is associated with more consistent and often better outcomes than fusion for disk-related low back pain. [15] In a large systematic review in 2008, Carreon et al [2] reported the greatest improvement in Oswestry Disability Index scores among patients who underwent fusion for spondylolisthesis. A study conducted by the Spine Patient Outcomes Research Trial reported greater pain relief and functional improvement after 4 years in patients who underwent fusion for spondylolisthesis compared with nonoperative control subjects. [5]
In the United States, patients receiving workers' compensation tend to have worse outcomes after lumbar fusion than those without workers' compensation claims. [613] One study reported that patients with workers' compensation claims had worse outcomes after fusion than patients who received disability funds. [7] In 2010, Carreon et al [9] reported worse clinical outcomes in patients receiving workers' compensation, and fewer patients with workers' compensation claims achieved substantial clinical benefit from fusion. Studies of subjects from several workers' compensation jurisdictions reported return to work rates of 26% to 36% and reoperation rates of 22% to 27% after fusion. [6, 1012, 14] Despite these results, fusion rates in patients with workers' compensation claims are steadily increasing. [11, 15]
The ability to return to work is among the most clinically important outcomes in those receiving workers' compensation, especially considering that the estimated cost of treating chronic low back pain is greater than $100 billion annually in the United States; two thirds of this cost is believed to be the result of lost wages and reduced productivity. [16, 17] Preoperative identification of which patients with workers' compensation claims are most likely to have positive outcomes after fusion and return to work is important. Identifying these patients not only leads to the best and most appropriate care for this clinically distinct subset of patients but also may help to curb medical costs and costs to the state. However, relatively few studies have evaluated potential risk factors for poor outcomes after lumbar fusion among those receiving workers' compensation. [6, 12, 14, 18, 19] Therefore, the goal of this study was to identify prognostic factors for return to work status after lumbar fusion for spondylolisthesis within a workers' compensation setting. To the authors' knowledge, this is the first study to identify predictors of return to work specifically among patients with workers' compensation claims who underwent arthrodesis for spondylolisthesis. The authors also compared other secondary outcomes between those who returned to work after fusion and those who did not.
Materials and Methods
This retrospective observational study included 686 patients with workers' compensation claims from the Ohio Bureau of Workers' Compensation who underwent anterior, posterior, or 360° lumbar fusion for spondylolisthesis. International Classification of Diseases, Ninth Revision (ICD-9), codes were used to identify 14,640 subjects from the Ohio Bureau of Workers' Compensation administrative database who were diagnosed with lumbar conditions after a workplace injury from 1993 to 2013. A coding schema reported by Nguyen et al6 using Current Procedural Terminology (CPT) codes was used to identify patients who had lumbar fusion. Because some patients underwent more than 1 fusion procedure while receiving workers' compensation, the current authors based this study and all outcomes on each subject's index fusion after injury. This study did not require institutional review board approval because the authors worked directly with the Legal Department at the Ohio Bureau of Workers' Compensation. All subject data were deidentified before collection.
The authors excluded 13,954 subjects from the initial population. Subjects who were excluded were those who did not undergo lumbar fusion; those who underwent fusion for indications other than spondylolisthesis; those who underwent a fusion approach other than anterior, posterior, or 360°; and those who had fewer than 3 years of postoperative follow-up. The authors excluded subjects with previous lumbar surgery, a history of smoking, or failed back syndrome because these factors negatively affect the outcomes of fusion. [3, 10, 2023] The authors identified lumbar comorbidities and failed back syndrome with ICD-9 codes, and they used ICD-9 codes and use of prescription smoking deterrents to identify a smoking history. The authors used CPT codes to identify subjects with previous lumbar surgery.
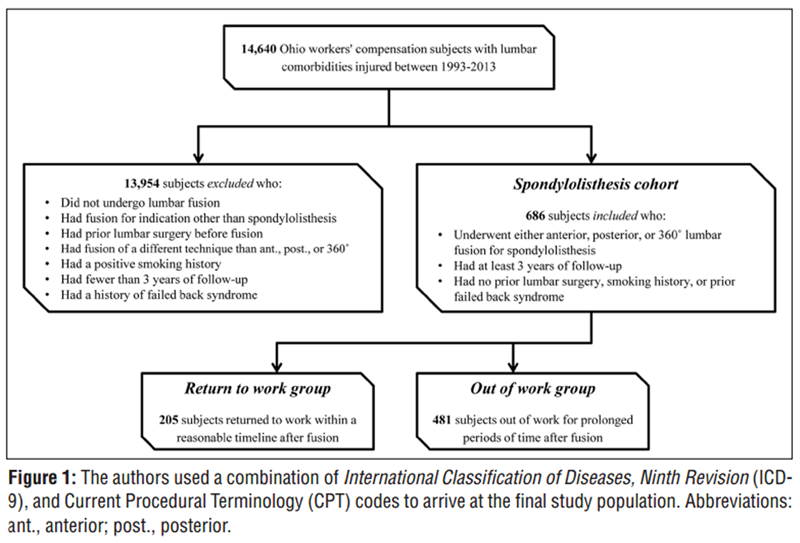
Figure 1

Table 1 There were 686 subjects who met the authors' inclusion criteria, and they formed the final spondylolisthesis cohort. The authors then determined which subjects returned to work within a reasonable amount of time after fusion. Specifically, the authors classified subjects as returning to work if they returned within 2 years after fusion and remained working for more than 6 months. The authors included the latter component in their return to work criteria to ensure that those who were classified as returning to work remained working for a sustained period. Only 205 (29.9%) subjects in the spondylolisthesis cohort met the criteria, forming the return to work group. The remaining 481 (70.1%) subjects formed the out of work group. Figure 1 shows the subject selection process, and Table 1 shows the codes used to form the study population.
The authors' primary outcome was whether the subjects met the return to work criteria. The authors also measured a number of secondary outcomes, all within 3 years after index fusion, including: days out of work, medical costs paid by the Ohio Bureau of Workers' Compensation, use of opioid analgesics, development of new psychiatric comorbidity, use of psychotherapy, and rates of failed back syndrome, permanent disability benefits, all-cause mortality, postoperative infection, pseudarthrosis, and additional lumbar surgery. Data on prescription opioid use were collected for all subjects before index fusion and within 3 years after this procedure. The total number of days that each subject was supplied with opioid analgesics was calculated. All prescription opioids were converted to morphine equivalents, and the authors determined the total morphine equivalents supplied to each subject and the average daily morphine equivalents to quantify daily opioid load.
The following data were also obtained: age at fusion, sex, time out of work, use of physical therapy, chiropractic care, psychotherapy, and approximated income. Exact incomes were unavailable, and the authors correlated zip codes of residence to a mean per capita income value based on the 2010 US Census. Additionally, the authors determined preoperative rates for the following characteristics: age older than 50 years at fusion, out of work status for longer than 1 year, permanent partial or total disability, lumbar diskography, legal representation, obesity, psychiatric or lumbar comorbidities, and psychiatric diagnostic examinations. In addition, for each subject, the fusion approach and the type of graft and instrumentation were characterized.
To identify prognostic factors for postoperative return to work status, the authors used multivariate logistic regression analysis. The dependent variable was whether the return to work criteria were met. In the regression model, the authors adjusted for the following preoperative and operative binary covariates: out of work for longer than 1 year, single-level vs multilevel fusion, decompression with fusion, receipt of permanent disability benefits, age older than 50 years, sex, obesity, approximated income less than the 25th percentile for the study population, isthmic vs degenerative spondylolisthesis, individual lumbar and psychiatric comorbidities, lumbar diskography, use of physical therapy, use of chiropractic care, supplied with opioid analgesics for longer than 1 year, daily opioid load above the 75th percentile for the study population, and legal representation. The authors adjusted for the following categorical variables: type of fusion surgery, instrumentation, and graft used. To compare secondary outcomes and baseline population characteristics between the return to work and out of work groups, the authors used chi-square tests for binary and categorical variables and Student's t tests for continuous variables. P≤.05 was considered statistically significant. For all analyses, Statgraphics Centurion XVI version 16.2.04 software (Statpoint Technologies, Inc, Warrenton, Virginia) was used.
Results

Table 2A

Table 2B

Table 3

Table 4
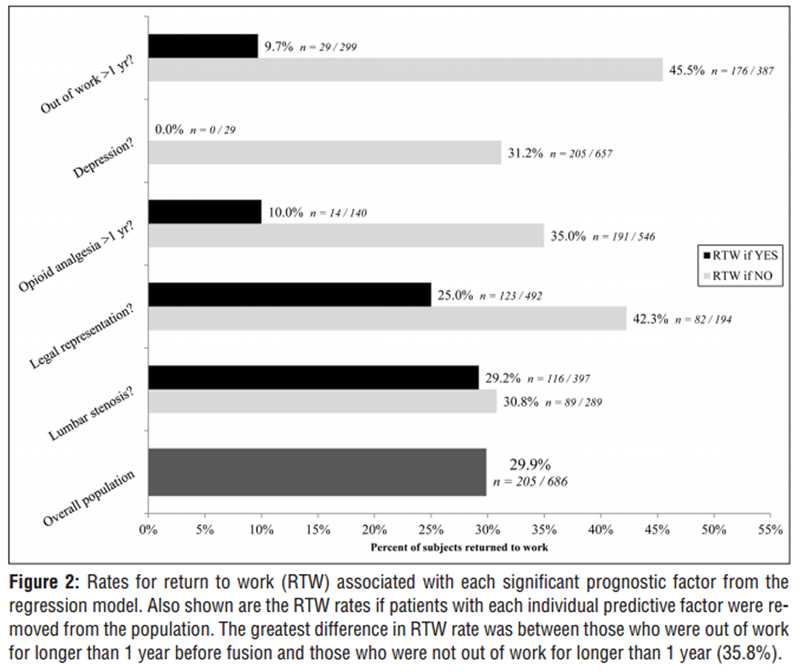
Figure 2

Table 5A

Table 5B The return to work and out of work groups differed significantly across a number of preoperative covariates (Table 2). Before fusion, compared with the out of work group, subjects in the return to work group were 1.9 years younger (P=.029), were out of work 345.3 fewer days (P<.001), used 16.6 fewer physical therapy sessions (P=.034), and were supplied with opioids 219.7 fewer days (P<.001), which equated to 16,663.8 fewer morphine equivalents (P<.001), with a daily opioid load that was 16.2 morphine equivalents lower (P<.001). Before fusion, the return to work group had a 42.0% lower rate of being out of work for longer than 1 year (P<.001), a 7.5% lower rate of diskography (P=.003), a 16.7% lower rate of legal representation (P<.001), a 6.7% lower rate of psychiatric comorbidity (P<.001), a 6.3% lower rate of psychiatric diagnostic examination (P<.001), a 7.7% lower rate of psychotherapy (P<.001), and a 19.4% lower rate of opioid analgesia for longer than 1 year (P<.001).
Regarding surgical covariates, the return to work and out of work groups differed significantly only in types of grafts used (P=.029). Of note, the return to work group had an 11.1% higher rate of autograft. Rates of different fusion techniques and instrumentation did not differ significantly between groups (Table 3).
Only 29.9% (205 of 686) of subjects in the spondylolisthesis cohort had a sustained return to work. Of the return to work group, 79.5% (163 of 205) returned within the first year after fusion. Negative preoperative prognostic factors for postoperative return to work included: out of work for longer than 1 year (P<.001; OR, 0.16), clinically diagnosed depression (P=.007; OR<0.01), use of opioid analgesia for longer than 1 year (P=.006; OR, 0.41), legal representation (P=.042; OR, 0.63), and lumbar stenosis (P=.043; OR, 0.55) (Table 4). No positive predictors were identified. Figure 2 shows the return to work rates for each of these factors as well as the resulting return to work rate when that variable was excluded. The 3 strongest negative predictors were depression, prolonged work loss, and long-term opioid use. If all subjects associated with these variables were eliminated from the cohort, then the overall return to work rate increased to 48.1% (168 of 349). If all subjects associated with any prognostic factor were removed, then the return to work rate increased to 60.4% (67 of 111).
The out of work group had considerably worse postoperative outcomes than the return to work group (Table 5). At 3 years after fusion, the out of work group was, on average, out of work for 646.0 additional days (P<.001), and this was associated with $25,980. [6] higher medical costs per subject paid by the Ohio Bureau of Workers' Compensation (P<.001). In addition, these subjects were supplied with opioids for 428.7 additional days (P<.001), which equated to 42,111.0 more morphine equivalents (P<.001), with a daily opioid load of an additional 15.9 morphine equivalents (P=.002). The out of work group also had a 5.1% higher rate of failed back syndrome (P=.016), a 14.9% higher rate of permanent total disability among those who were not receiving permanent disability payments before fusion (P<.001), and a 16.4% higher rate of additional lumbar surgery (P<.001).
After fusion, the out of work group was diagnosed with new psychiatric disorders, chiefly depression, at a 22.7% higher rate (P<.001) and used psychotherapy at a 28.6% higher rate (P<.001) compared with the return to work group. Of the out of work group, 7.7% were diagnosed with a psychiatric disorder before fusion. Among those with no preoperative psychiatric history, 25.7% were diagnosed with a psychiatric disorder after fusion. Overall, 31.4% (151 of 481) of the out of work group and 3.9% (8 of 205) of the return to work group had a psychiatric diagnosis either before or after fusion. Rates of psychotherapy among the out of work group increased from 7.7% before fusion to 34.9% after fusion. Among the return to work group, this rate increased from 0% to 6.3%. In the out of work group, the average number of psychotherapy sessions increased by more than a factor of 5 after fusion (P<.001), possibly suggesting worsening psychiatric health. Mean number of sessions also increased in the return to work group, but only from 0.0 to 0.9 (P=.008). Additionally, rates of psychiatric diagnostic examinations for the out of work group and the return to work group increased by 22.0% and 3.9% after fusion, respectively. Among subjects with no psychiatric history before fusion, the out of work group had a 24.4% higher rate of index psychiatric diagnostic examination after fusion compared with the return to work group (P<.001).
Discussion
In the general population, lumbar fusion for spondylolisthesis has been associated with consistent outcomes.15 However, patients receiving workers' compensation tend to have inferior outcomes after fusion. [613] Few studies have identified prognostic factors within this clinically distinct population. [6, 12, 14, 18, 19] The current study was the first to do so among patients with workers' compensation claims who underwent arthrodesis for spondylolisthesis. Among 686 subjects who had workers' compensation claims in Ohio and underwent lumbar fusion for spondylolisthesis from 1993 to 2013, the authors identified a number of preoperative prognostic factors for postoperative return to work. The strongest negative predictors were depression, prolonged time out of work, and long-term opioid analgesia. Return to work rates associated with these factors were 0.0%, 9.7%, and 10.0%, respectively. If subjects with these factors were eliminated from the cohort, the return to work rate increased to 48.1%. Of all subjects, 50.9% had 1 or more of these factors. If subjects associated with any of the negative prognostic factors were eliminated, then the return to work rate increased to 60.4% (67 of 111). However, subjects with 1 or more of these factors accounted for 83.8% of the entire spondylolisthesis cohort, 67.3% of the return to work group, and 90.9% of the out of work group.
Because so many subjects had negative prognostic factors, overall return to work outcomes were poor. The overall return to work rate was only 29.9%, with most (79.5%) subjects returning to work within the first year after fusion. This finding suggests that the longer patients with workers' compensation claims are out of work, the less likely they are to return. The 70.1% of subjects who did not return to work had considerably worse outcomes after fusion, including prolonged work loss, higher medical costs, long-term opioid dependence, and higher rates of failed back syndrome, permanent total disability, and additional lumbar surgery. Rates of psychiatric disorders increased after fusion among both the return to work group and the out of work group. However, this finding was far more pronounced in the out of work group. In addition, the out of work group had considerably more psychotherapy sessions after fusion than before fusion, possibly suggesting worsening psychiatric health. Overall rates of psychiatric diagnostic examinations increased greatly after fusion. Given the poor return to work outcomes linked to depression and the apparent increase in psychiatric comorbidity after fusion, this finding may highlight a potential effect of better screening and treatment of psychiatric disorders before lumbar fusion is performed in patients with workers' compensation claims.
Limitations
The current study was limited by its retrospective and observational design. Although the authors adjusted for a number of important covariates in the analysis, unmeasured confounding may still exist. The completeness of the data may have been limited by the use of the administrative database of the Ohio Bureau of Workers' Compensation. However, this database was used in earlier studies. [6, 14] Also, 2 recent studies reported high sensitivity and specificity in administrative billing data when compared with actual medical records, and this finding showed that these databases can provide accurate information, especially when identifying diagnoses, indications for surgery, and the type of procedure performed. [24, 25] In the current study, the authors determined which form of spondylolisthesis each subject had, but they could not determine the grade of slippage. However, this study included the entire population of patients in Ohio with workers' compensation claims who met the inclusion criteria and were treated between 1993 and 2013. This helped to avoid bias and increased the likelihood that the distribution of disease severity would be similar to that in other populations. Finally, the generalizability of the study findings to patients with workers' compensation claims in other jurisdictions may be affected by factors such as different legislative regulations, treatment guidelines, and potential geographic effects on outcomes. This was shown in a 2014 study that reported differences in outcomes between those with workers' compensation claims in California and Washington State because of differences in policies and physician reimbursement. [26]
Conclusion
This study identified a number of prognostic factors for worse return to work outcomes within a large population of patients with workers' compensation claims who underwent fusion for spondylolisthesis. Clinically diagnosed depression, extensive work loss, prolonged opioid use, lumbar stenosis, and legal representation before fusion negatively affected the likelihood that subjects would return to work after fusion. Most of the study subjects had 1 or more of these factors. Overall return to work outcomes were poor. Those who did not return to work also had considerably worse secondary outcomes after fusion. However, spondylolisthesis is a well-accepted indication for spinal fusion among the general population, and this study focused largely on return to work rates and work loss. It is possible that these patients had greater improvement after fusion than was indicated by the findings, although they were not able to return to work at high rates. Future studies are needed to identify how to better facilitate return to work among similar patients with workers' compensation claims. The authors hope that this study helps clinicians to determine which patients with workers' compensation claims who are treated for spondylolisthesis may be at higher risk for poor return to work outcomes.
Authors
The authors are from the Department of Orthopaedics (JTA, NUA), University Hospitals Case Medical Center, Cleveland, Case Western Reserve University School of Medicine (JTA), Cleveland, and the Ohio Bureau of Workers' Compensation (ARH, RP, STW), Columbus, Ohio; and the New Hampshire NeuroSpine Institute (UMA), Bedford, New Hampshire.
Mr Anderson, Mr Haas, and Dr Percy have no relevant financial relationships to disclose. Dr Woods holds stock in OrthoNeuro, Inc. Dr U M Ahn is a paid consultant for, is on the speaker's bureau of, and receives travel expenses from Alphatec, Spine 360, and K1; receives royalties from Alphatec and Spine 360; and holds stock in K1. Dr N U Ahn receives grants and research support from Stryker.
Correspondence should be addressed to: Joshua T. Anderson, BS, 2477 Overlook Rd, Apt 3, Cleveland Heights, OH 44106 (Jta38@case.edu).
References:
Glassman SD, Carreon LY, Djurasovic M, et al.
Lumbar fusion outcomes stratified by specific diagnostic indication.
Spine J. 2009; 9(1):1321Carreon LY, Glassman SD, Howard J.
Fusion and nonsurgical treatment for symptomatic lumbar degenerative disease: a systematic review of Oswestry Disability Index and MOS Short Form-36 outcomes.
Spine J. 2008; 8(5):747755Hanley EN Jr,
The indications for lumbar spinal fusion with and without instrumentation.
Spine (Phila Pa 1976). 1995; 20(suppl 24):143S153SButtermann GR, Garvey TA, Hunt AF, et al.
Lumbar fusion results related to diagnosis.
Spine (Phila Pa 1976). 1998; 23(1):116127Weinstein JN, Lurie JD, Tosteson TD, et al.
Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis: four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts.
J Bone Joint Surg Am. 2009; 91(6):12951304Nguyen TH, Randolph DC, Talmage J, Succop P, Travis R.
Long-term Outcomes of Lumbar Fusion Among Workers' Compensation Subjects:
An Historical Cohort Study
Spine (Phila Pa 1976) 2011 (Feb 15); 36 (4): 320331Gum JL, Glassman SD, Carreon LY.
Is type of compensation a predictor of outcome after lumbar fusion?
Spine (Phila Pa 1976). 2013; 38(5):443448Franklin GM, Haug J, Heyer NJ, McKeefrey SP, Picciano JF.
Outcome of lumbar fusion in Washington State workers' compensation.
Spine (Phila Pa 1976). 1994; 19(17):18971903arreon LY, Glassman SD, Kantamneni NR, Mugavin MO, Djurasovic M.
Clinical outcomes after posterolateral lumbar fusion in workers' compensation patients: a case-control study.
Spine (Phila Pa 1976). 2010; 35(19):18121817DeBerard MS, Masters KS, Colledge AL, Schleusener RL, Schlegel JD.
Outcomes of posterolateral lumbar fusion in Utah patients receiving workers' compensation: a retrospective cohort study.
Spine (Phila Pa 1976). 2001; 26(7):738746Maghout Juratli S, Franklin GM, Mirza SK, Wickizer TM, Fulton-Kehoe D.
Lumbar fusion outcomes in Washington State workers' compensation.
Spine (Phila Pa 1976). 2006; 31(23):27152723DeBerard MS, Wheeler AJ, Gundy JM, Stein DM, Colledge AL.
Presurgical biopsychosocial variables predict medical, compensation, and aggregate costs of lumbar discectomy in Utah workers' compensation patients.
Spine J. 2011; 11(5):395401Mayer TG, Gatchel RJ, Brede E, Theodore BR.
Lumbar surgery in work-related chronic low back pain: can a continuum of care enhance outcomes?
Spine J. 2014; 14(2):263273Anderson JT, Haas AR, Percy R, Woods ST, Ahn UM, Ahn NU.
Single-level lumbar fusion for degenerative disc disease is associated with worse outcomes compared with fusion for spondylolisthesis in a workers' compensation setting.
Spine (Phila Pa 1976). 2015; 40(5):323331Rajaee SS, Bae HW, Kanim LE, Delamarter RB.
Spinal fusion in the United States: analysis of trends from 1998 to 2008.
Spine (Phila Pa 1976). 2012; 37(1):6776Crow WT, Willis DR.
Estimating cost of care for patients with acute low back pain: a retrospective review of patient records.
J Am Osteopath Assoc. 2009; 109(4):229233Katz JN.
Lumbar disc disorders and low-back pain: socioeconomic factors and consequences.
J Bone Joint Surg Am. 2006; 88(suppl 2):2124Hodges SD, Humphreys SC, Eck JC, Covington LA, Harrom H.
Predicting factors of successful recovery from lumbar spine surgery among workers' compensation patients.
J Am Osteopath Assoc. 2001; 101(2):7883Wheeler AJ, Gundy JM, DeBerard MS.
Predicting compensation and medical costs of lumbar fusion patients receiving workers' compensation in Utah using presurgical biopsychosocial variables.
Spine (Phila Pa 1976). 2012; 37(7):605611Miller B, Gatchel RJ, Lou L, Stowell A, Robinson R, Polatin PB.
Interdisciplinary treatment of failed back surgery syndrome (FBSS): a comparison of FBSS and non-FBSS patients.
Pain Pract. 2005; 5(3):190202Jenkins LT, Jones AL, Harms JJ.
Prognostic factors in lumbar spinal fusion.
Contemp Orthop. 1994; 29(3):173180Andersen T, Christensen FB, Laursen M, Hψy K, Hansen ES, Bόnger C.
Smoking as a predictor of negative outcome in lumbar spinal fusion.
Spine (Phila Pa 1976). 2001; 26(23):26232628Cobo Soriano J, Sendino Revuelta M, Fabregate Fuente M, Cimarra Dνaz I.
Predictors of outcome after decompressive lumbar surgery and instrumented posterolateral fusion.
Eur Spine J. 2010; 19(11):18411848Singh JA, Ayub S.
Accuracy of VA databases for diagnoses of knee replacement and hip replacement.
Osteoarthritis Cartilage. 2010; 18(12):16391642Kazberouk A, Martin BI, Stevens JP, McGuire KJ.
Validation of an administrative coding algorithm for classifying surgical indication and operative features of spine surgery.
Spine (Phila Pa 1976). 2015; 40(2):114120Martin BI, Franklin GM, Deyo RA, Wickizer TM, Lurie JD, Mirza SK.
How do coverage policies influence practice patterns, safety, and cost of initial lumbar fusion surgery? A population-based comparison of workers' compensation systems.
Spine J. 2014; 14(7):12371246
Return to LOW BACK PAIN
Return to WORKERS' COMPENSATION
Since 10232010


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |