

Best Practices Recommendations for Chiropractic Care
for Infants, Children, and Adolescents:
Results of a Consensus ProcessThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Manipulative Physiol Ther. 2009 (Oct); 32 (8): 639–647 ~ FULL TEXT
Cheryl Hawk, DC, PhD, Michael Schneider, DC, PhD, Randy J. Ferrance, DC, MD,
Elise Hewitt, DC, Meghan Van Loon, DC, PT, Lora Tanis, DC
Cleveland Chiropractic College,
Overland Park, KS 66210, USA.
These recommendations have been updated by the 2016 article:
Best Practices for Chiropractic Care of Children: A Consensus UpdateOBJECTIVE: There has been much discussion about the role of chiropractic care in the evaluation, management, and treatment of pediatric patients. To date, no specific guidelines have been adopted that address this issue from an evidence based perspective. Previous systematic reviews of the chiropractic literature concluded that there is not yet a substantial body of high quality evidence from which to develop standard clinical guidelines. The purpose of this project was to develop recommendations on "best practices" related primarily to the evaluation and spinal manipulation aspects of pediatric chiropractic care; nonmanipulative therapies were not addressed in detail.
METHODS: Based on both clinical experience and the results of an extensive literature search, a set of seed documents was compiled to inform development of the seed statements. These were circulated electronically to the Delphi panel until consensus was reached, which was considered to be present when there was agreement by at least 80% of the panelists.
RESULTS: A multidisciplinary panel of 37 was made up primarily of doctors of chiropractic with a mean of 18 years in practice, many with post-graduate training in pediatrics. The panel represented 5 countries and 17 states; there were members of the American Chiropractic Association, the International Chiropractors Association, and the International Chiropractic Pediatric Association. The panel reached a minimum of 80% consensus on the 51 seed statements after 4 rounds.
CONCLUSIONS: A broad-based panel of experienced chiropractors was able to reach a high level (80%) of consensus regarding specific aspects of the chiropractic approach to clinical evaluation, management, and manual treatment for pediatric patients, based on both scientific evidence and clinical experience.
From the Full-Text Article:
Introduction

Table 1 The National Center for Health Statistics found that manipulation by chiropractors or osteopathic physicians was the most commonly used provider-based complementary and alternative (CAM) therapy among US children under age 18 in 2007. [1] The most frequent complaint causing children to seek CAM care, in general, was back or neck pain (7%). Because the prevalence of low back pain (LBP) in children has been estimated to be as high as 40%, with recurrent LBP occurring in 20% of older adolescents, this is not surprising. [2] However, children also sought CAM care for a number of other complaints, both musculoskeletal and nonmusculoskeletal, as shown in Table 1. Approximately 12% of US children used some type of CAM therapy in 2007; about 3% used manipulation (chiropractic or osteopathic). Adolescents used CAM more than younger children, and it was more commonly used among children with more health problems and doctor visits. [1]
In order to best serve the health of the public, it is important that all providers maintain and follow the highest standards of patient care. This includes adherence to the principles of evidence-based practice. Evidence-based practice is “the integration of best research evidence with clinical expertise and patient values.” [3] However, in many cases, especially for CAM practices, the higher levels of evidence such as randomized controlled trials or large observational studies are lacking. According to Sackett, the “father” of evidence-based medicine, “evidence based medicine is not restricted to randomized trials and meta-analyses. It involves tracking down the best external evidence with which to answer our clinical questions…” [4, 5]
Chiropractic care, a “package” of conservative approaches, including manipulation, for pain management and/or promoting optimal function, has accumulated a substantial evidence base, primarily for musculoskeletal complaints. [6] Manipulation, performed by trained providers, has been recommended by the American College of Physicians, as having benefit for both acute and chronic LBP in adults. [7] Serious adverse events have been found to be rare for manipulation of the low back (estimated at 1 per 3.72 million manipulations). [8] Manual procedures and exercise, commonly used by chiropractors, were found in a 2008 best evidence synthesis to be beneficial for adult patients with neck pain. [9] A large observational study published in 2008 found no excess risk of vertebrobasilar stroke associated with chiropractic neck manipulation. [10] Another study found that, although minor adverse effects such as transient soreness were commonly associated with manipulation, the overwhelming majority of these resolved within 24 hours of onset and did not affect daily activities. [11] A 2009 systematic review of manipulation for conditions of the lower extremity found limited, but positive, evidence for adult patients with conditions of the hip, knee, and ankle, with no serious adverse events observed. [12]
A 2007 systematic review of chiropractic care for nonmusculoskeletal conditions concluded that “evidence from controlled studies and usual practice supports chiropractic care (the entire clinical encounter) as providing benefit to patients with asthma, cervicogenic vertigo, and infantile colic. The evidence was promising for potential benefit of manual procedures for children with otitis media and elderly patients with pneumonia.” [13] An important distinction should be made between the terms “chiropractic manipulation” and “chiropractic care.” The term “chiropractic care” refers to the entire clinical encounter in a chiropractic setting which may include many nonmanipulative therapies such as dietary advice, nutritional or herbal supplements, posture correction, therapeutic exercise, physiotherapeutic modalities, and behavioral counseling.
However, the large body of evidence for the effectiveness of chiropractic care for adults may not necessarily be directly applicable to infants, children, and adolescents. A 2008 systematic review on chiropractic manipulation for children's health problems concluded that “the evidence rests primarily with clinical experience, descriptive case studies, and very few observational and experimental studies.” [14] The current evidence often does not make a distinction between chiropractic manipulation as a monotherapy and chiropractic care that incorporates multiple nonmanipulative therapies as a “package.”
Therefore, at this time, it is apparent that the scientific evidence base has important gaps in terms of the appropriateness of chiropractic care for infants, children, and adolescents. Safety is one of the most important issues; a recent systematic review recommended that further study is necessary to assess the safety of spinal manipulation for children. [15] There is not yet sufficient research evidence related specifically to children to definitively identify indications for spinal manipulation and other procedures within the chiropractic scope of practice. However, the chief factors cited as concerns in that systematic review were possible direct adverse events related to spinal manipulation and possible indirect adverse events related to delayed diagnosis or delayed medical treatment for serious conditions.
Consequently, we undertook this consensus project in order to bridge this gap in the scientific evidence, and ensure the highest quality of chiropractic care for infants, children, and adolescents. Expert consensus is a form of evidence which must be relied on when higher levels of evidence are lacking. [16] The purpose of the project was to make recommendations on standards of chiropractic care for children, based on the existing evidence and the consensus of a multidisciplinary group of experts on pediatrics and chiropractic. It is essential for the safety of pediatric chiropractic patients that chiropractors who care for infants, children, and adolescents have access to a document that clearly outlines the best practices for chiropractic care of infants, children, and adolescents.
Methods
Overview of Project
The purpose of a “best practices” document related to chiropractic care is to describe the diagnostic and management procedures representing the best scientific evidence, the consensus of the profession, and the most beneficial approach to patient care. The purpose of this project was to develop such a consensus document as it relates to certain aspects of pediatric chiropractic care, primarily evaluation and spinal manipulation; non-manipulative therapies were not addressed.
“Best practice” has been described as follows:“Best practice is not a specific practice per se but rather a level of agreement about research-based knowledge and an integrative process of embedding this knowledge into the organization and delivery of health care. Best practice requires a level of agreement about evidence to be integrated into practice. Best practice…can bridge the practice-research gap and provide a basis for researchers and clinicians to work together to translate research into meaningful practice.” [3]
Human Subjects Considerations
Before the start of any activities, the project was approved by the Cleveland Chiropractic College Institutional Review Board, ensuring that all issues related to the confidentiality and other rights of the participating panelists were addressed. All participants were asked to give written permission for their names to be used in relation to the project or to have their names included in any publication related to the project.
Establishment of a Steering Committee
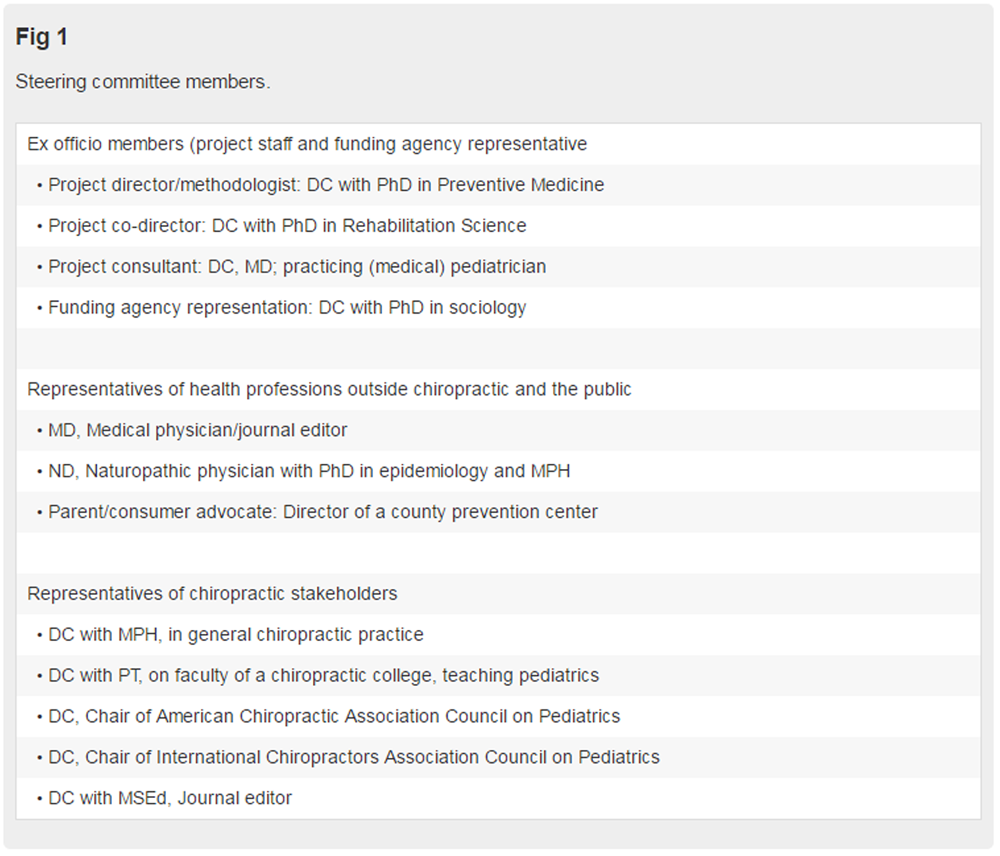
Figure 1 The purpose of the steering committee (SC) was to provide project oversight from a multidisciplinary perspective, ensuring that all stakeholders were represented, from the chiropractic profession as well as other health professions and the public. The head of each of the 3 major chiropractic pediatric organizations was invited to join the SC, with 2 of them accepting our invitation. Figure 1 lists the qualifications of the multidisciplinary steering committee members.
Seed Documents
An extensive literature search was conducted by an experienced research associate to identify relevant literature, updating a previous literature review done by the project director as part of a project for the Council on Chiropractic Guidelines and Practice Parameters. Based on the results of the search and their experience, the project team compiled a set of documents to inform development of the seed statements and to provide background to the Delphi panelists. They sought input from the SC to ensure that the seed documents were comprehensive.
Topics of this background information included:
Adverse events related to chiropractic care for infants, children, and adolescents.
Public health significance, that is, prevalence and social/economic burden of conditions of infants, children, and adolescents that may be responsive to chiropractic care.
Evidence on effectiveness of chiropractic care/manual procedures for conditions that affect infants, children, and adolescents and/or their health and well-being.
Existing guidelines for chiropractic care for infants, children, and adolescents.
The background literature was distilled down to 4 documents for the Delphi panelists:
A discussion of the use of complementary and alternative medicine, including chiropractic, in pediatrics, by a task force of the American Academy of Pediatrics. [11]
A summary document that synthesized the salient points from the following studies:
a. Safety issues and adverse events that may be associated with pediatric manipulation, [15, 17, 18]
b. Two systematic reviews of manual procedures for infants, children, and adolescents [14, 19]
c. A systematic review of chiropractic care for nonmusculoskeletal conditions [13]
d. A systematic review of immunization issues [20]An article on evidence-based physical therapy treatment of children with LBP, to provide context from outside the chiropractic profession on this public health issue [21];
A 2008 guideline from the Australian chiropractic board on chiropractic care for children
(NOTE: The 2015 version is attached
These documents were emailed to the panelists 3 weeks prior to conducting the first Delphi round.
Development of Seed Statements
The project team and steering committee collaborated by email and phone conferences to develop a set of seed statements concerning an appropriate approach to chiropractic care for infants, children, and adolescents. This seed document consisted of 51 seed statements relating to all of the important aspects of the clinical encounter.
Delphi Consensus Process
The purpose of a Delphi process is to elicit information and judgments from participants to facilitate problem-solving, planning, and decision-making. The Delphi communications were conducted electronically. Since panelists did not meet face to face, or even know the identity of other panelists, the possibilities of influencing one another's opinions were greatly reduced.
We followed the rigorous and widely-accepted RAND Corp/University of California, Los Angeles methodology for conducting consensus processes. [22] Panelists were asked to indicate the appropriateness of the procedure or practice described in each seed statement. They were told that “appropriateness” indicates that the expected health benefit to the patient exceeds the expected negative consequences by a sufficiently wide margin that it is worth doing, exclusive of cost. [22] We provided them with a scale of 1 to 9 (highly inappropriate to highly appropriate, scoring 1-3 as “inappropriate,” 4-6 as “undecided,” and 7-9 as “appropriate”). Panelists were required to provide specific reasons for inappropriate ratings, providing a citation from the peer-reviewed literature to support it, if such existed.
In analyzing the responses, agreement on appropriateness was considered to be present if at least 80% of panelists marked 7, 8, or 9, and the median response score was 7 to 9. Rounds were repeated, revising the seed statements as per the panelists' comments each time, until at least 80% level of consensus was reached.
Delphi Panel
The project team circulated a notice about the project to the chiropractic colleges and chiropractic organizations. Nominees completed a demographic form and submitted their CVs. The SC and project team reviewed the nominees and selected panelists to form a multidisciplinary panel with expertise and experience in pediatrics and/or chiropractic as well as representativeness geographically, demographically, and in terms of their approach to practice.
Results
Delphi Panel
Thirty-seven panelists (19 women and 18 men) were selected and agreed to participate. Of these, 35 were doctors of chiropractic (DCs); 1, a doctor of osteopathy (DO) with an MS; and 1, a PhD, non–health care provider. Of the DCs, one also had an MD and one also had a DO degree, while 6 had Masters' degrees and 3 had PhDs. There were panelists from 5 countries (United States, Australia, England, Netherlands, Sweden) and 17 states in the United States (California, Colorado, Connecticut, Georgia, Iowa, Illinois, Massachusetts, Maryland, Maine, Minnesota, Mississippi, North Carolina, New Jersey, New York, Ohio, Oregon, Virginia). In terms of advanced training in pediatrics, the DO was board-certified in pediatrics, 13 of the DCs had postgraduate training in the International Chiropractors Association (ICA) pediatric program, and 2 had postgraduate training in the International Chiropractic Pediatric Association (ICPA) program. One panelist was a diplomate of the American Chiropractic Neurology Board with advanced training in child developmental disorders. Three of the panelists had an MSc in Pediatrics. Sixteen panelists were members of the American Chiropractic Association (ACA), 11 of the ICA and 5 of the ICPA. For the 34 panelists in active practice, the mean number of years in practice was 18 (range, 5-35 years).
Delphi Rounds
Delphi rounds were conducted January to March 2009. All 37 panelists participated in all rounds. Consensus (at least 80% agreement on appropriateness, with a median rating of ≥8) was reached on all statements in 4 rounds.
Seed Statements
After consensus was reached on the statements, the resulting document was circulated to the Steering Committee for approval and recirculated to the Delphi panel for final approval. The statements are shown in the next section.
Best Practices for Chiropractic Care for Children
The purpose of this document is to protect the health of the public by defining the parameters of an appropriate approach to chiropractic care for patients under 18 years of age. The potential benefits of any health care intervention should be weighed against the associated risks and the costs in terms of time and money. There are significant anatomical, physiological, developmental, and psychological differences between children and adults which may affect the appropriateness of any given healthcare intervention.
General Clinical Principles in the Care of Children
The musculoskeletal structure and function of infants, children, and adolescents are less rigid and more flexible than those of an adult. Physical, psychological, and emotional responses to intervention vary.
Regarding patient communication:
Extracting relevant clinical information during the case history of an infant, child, or adolescent patient requires special communication skills and experience.
Age-appropriate communication is necessary to help a child patient actively engage in the clinical encounter.
Infants and toddlers cannot communicate verbally and therefore the clinical encounter requires communication with a parent or legal guardian.
Regarding informed consent:
Informed consent signed by the parent or legal guardian is required before initiating a clinical encounter, including the initial consultation, performing an examination and diagnostic tests, and initiating a management program.
The chiropractor should explain all procedures clearly and simply, and answer both the parent's and child/adolescent's questions to ensure that they can make an informed decision about their health care choices.
Verbal consent should be obtained from the child/adolescent whenever developmentally appropriate.
The diagnosis should be explained to the parent/guardian (and the older child) in an age-appropriate, understandable manner.
The proposed treatment plan and any possible risks of care should be explained along with all other reasonable treatment options.
Chiropractic Management of Pediatric Patients
Chiropractic management of the infant/child/adolescent patient should follow the 3 basic principles of evidence based practice, which are to make clinical judgments based on use of the best available evidence, combined with the clinician's experience and the patient's preference. The research community has just begun to investigate the effectiveness of chiropractic care for many pediatric conditions; however, lack of research evidence does not imply ineffectiveness. Evidence-based practice is the integration of clinical expertise and patient values with the best available research evidence. A therapeutic trial of chiropractic care can be a reasonable approach to management of the pediatric patient in the absence of conclusive research evidence, when clinical experience and patient/parent preferences are aligned.
There are 3 basic chiropractic management approaches
to the care of the infant/child/adolescent patient:(1) sole management by a chiropractic physician,
(2) comanagement with other appropriate health care providers, and
(3) referral to another licensed or certified health care provider/specialist.
Comanagement with other appropriate health care providers
is appropriate under many conditions including the following
circumstances noted below:
The patient is not showing clinically significant improvement after an initial trial of chiropractic care.
The parents of the infant/child/adolescent patient request such a comanagement approach.
There are significant comorbidities that are outside the scope of chiropractic practice or require medication, advanced diagnostic imaging or laboratory studies.
When the chiropractor orders diagnostic imaging or laboratory studies, copies of these results should be forwarded to the patient's primary care physician for coordination of care.
Management of many nonmusculoskeletal conditions may benefit from comanagement with the patient's primary care physician and/or other providers, depending on the condition.
Immediate referral to a medical specialist should occur when the case history and examination reveal any “red flags” suggestive of serious pathology. A list of these red flags is provided in Figure 2.
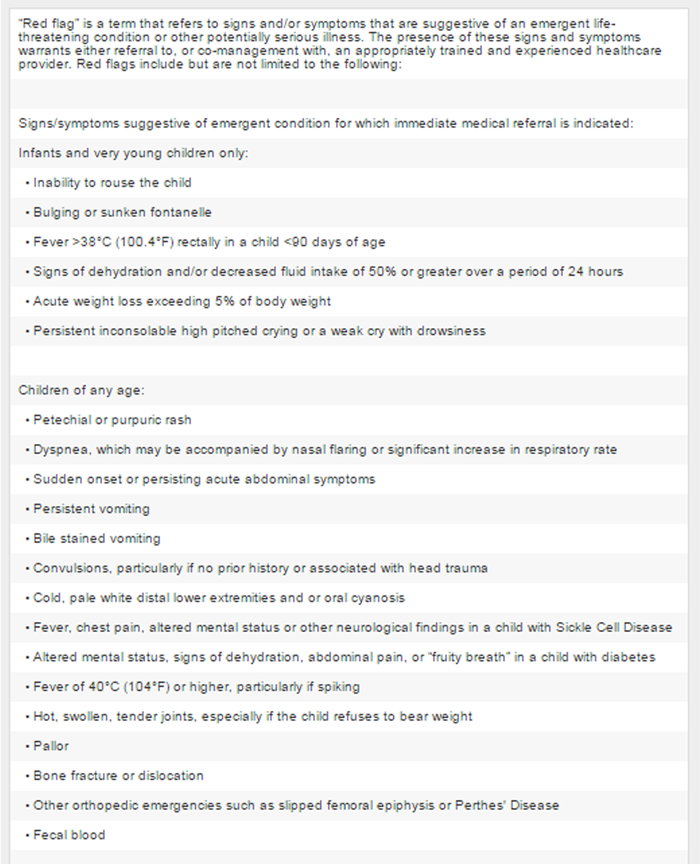
Figure 2-A
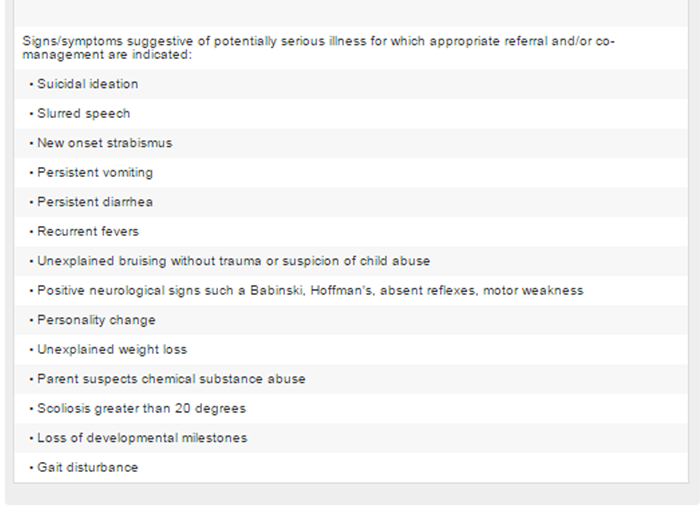
Figure 2-B Clinical History
A focused case history should be conducted at the initial visit. The comprehensive case history at the initial visit should include a review of systems, developmental milestones, family history, healthcare history, concurrent healthcare, and medication use. Information on health habits, including breastfeeding, diet, sleep, physical activity, and injuries should be included. For very young children, a review of relevant pre-natal events, including the health of the mother, as well as a review of the birth history (gestational age, birth weight, perinatal complications) is appropriate. Obtaining case history information for the infant/child/adolescent can be helpful in determining the appropriate case management.
Red Flags in Pediatric Patients
If the history and/or examination reveal “red flags” indicating serious conditions, the infant/child/adolescent should be referred to an appropriate provider for further diagnosis and/or care (see Figure 2 for list of red flags).
Examination
Clinically relevant and valid examination procedures should be used to enable the practitioner to move from a working diagnosis, based on the history, to a short list of differential diagnoses. Necessary diagnostic or examination procedures outside the practitioner's scope of practice or range of experience should be referred to an appropriately qualified and experienced health professional. Vital signs should be recorded, including temperature, heart rate, respiratory rate, weight, height, and blood pressure. For infants, vital signs should include all of the above plus head circumference and fontanelle diameter. An age-appropriate neurodevelopmental examination should be conducted. Neurological tests including balance and gait, neurodevelopmental age-appropriate milestones, cranial nerve examination, and pathological reflexes. Primitive reflexes in the infant should be assessed.
Diagnostic Imaging
Clinical indications for radiographic examination of the pediatric patient are history of trauma, suspicion of serious pathology, and/or assessment of scoliosis. The routine use of radiographs or repeated radiographs for the child patient is not recommended without clear clinical justification. Plain film radiographs may be indicated in cases of clinically suspected trauma-induced injury, such as fracture or dislocation. Radiographs may also be indicated in cases of clinically suspected orthopedic conditions such as hip disorders or pathology, such as bone malignancy. Plain film radiographs may be necessary for determination of contraindications to manipulation; for example: Congenital or genetic conditions that may cause compromise of the spine, spinal cord or extremities. There are limitations to the diagnostic utility of plain film radiograph and/or diagnostic ultrasound for the diagnosis of certain pediatric or adolescent conditions which may require the use of more advanced diagnostic imaging such as magnetic resonance imaging, computed tomography, or bone scan.
Considerations for Treating Infants/Children/Adolescents with Manual Procedures:
Patient size: biomechanical force should be modified in proportion to the size of the patient.
Structural development: manual procedures should be modified to accommodate the developing skeleton.
Flexibility of joints: manual procedures should take into account the greater flexibility and lesser muscle mass, using gentler and lighter forces.
Patient preferences: the clinician should adapt manipulation and soft tissue techniques and procedures that support the needs and comfort of the infant/child/adolescent.
Pediatric Care Planning
“Well child” visits are an established aspect of pediatric health care, and may be indicated for the purpose of health promotion counseling and clinical assessment of asymptomatic pediatric patients. Doctors of chiropractic should emphasize disease prevention and health promotion through counseling on physical activity, nutrition, injury prevention, and a generally healthy lifestyle. Immunization is a well-established medical approach to disease prevention and chiropractors may be asked for information about immunizations by a child's parents. They should provide balanced, evidence-based information from credible resources and/or refer the parents to such resources. Doctors of chiropractic should counsel pediatric patients and their parents in healthy behavior and lifestyle, including but not limited to the following topics: adequate age-appropriate physical activity and decreased screen time, such as TV, electronic games, and computer use; healthy diet; adequate sleep; injury prevention; and substance use (eg, caffeinated beverages, alcohol, tobacco, steroids, illicit drugs, etc).
Public Screening of Children for Health Problems
Any tests or procedures used for public screenings must be based on recognized evidence of their benefit for disease prevention and health promotion.
Discussion
There were several strengths of this consensus process. A key strength was the development and publication of the first comprehensive set of best practice guidelines regarding chiropractic care of children. The consensus statements generated from this panel of experts provide some reasonable and rational parameters to the clinical management of the infant/child/adolescent patient by chiropractic clinicians. This document was produced with the input from a wide variety of panel members; including chiropractic clinicians with extensive experience treating children, chiropractic educators and researchers, and members of the ACA, the ICA, and the ICPA. Over 80% agreement was achieved by the panel members on 51 seed statements; this is certainly an impressive level of consensus. Our panel of experts was clearly representative of the entire spectrum of the chiropractic profession, and therefore, the results can be considered quite generalizable to everyday chiropractic practice.
Another strength of this consensus process was the ability of the panel members to recognize aspects of chiropractic pediatric practice that could benefit from additional research evidence and standardization. As noted above, our panel determined that there was a need for developing standards for chiropractic college pediatric curricula and post graduate educational programs. The panel also recognized that there were only a small number of high-quality clinical studies on the topic of manipulation for a variety of health conditions found in children. They noted that “chiropractic care” was not synonymous with spinal manipulation and that chiropractors often manage infants, children, and adolescents with numerous other interventions such as vitamins, dietary interventions, therapeutic exercise and posture correction, physical agents, and other treatments. The panel suggested that much more research is needed to determine the clinical effects of these various interventions as monotherapies and “packages” of a combination of therapies. Lastly, the panel found that the vast majority of the clinical studies on manipulation and musculoskeletal pain were performed in the adult population and that the findings may not necessarily be generalizable to a pediatric population.
Finally, a key strength of this document is that the information will help to inform numerous stakeholders about a reasonable and rational approach to chiropractic care for the pediatric patient. Chiropractors can use this document as a guide to the current best practices, while patients (and their parents) can use this information to inform treatment decisions. Third-party payors and regulatory agencies may find this information useful for guiding policy decisions about chiropractic care for the pediatric population while recognizing that evidence based practice strongly considers patient-preference to be an important factor in determining the type of treatment provided. This best practice document serves as a synthesis of the best current evidence and collective expert opinion about a reasonable clinical approach to the chiropractic management of infants, children, and adolescents.
Limitations
There were some limitations of this consensus process. This document was focused primarily on examination methods and manual treatment, yet chiropractic care may include many other services in addition to manipulative procedures. Chiropractic care may include the use of physiotherapy modalities, therapeutic exercise, dietary interventions, the use of vitamins and herbs, and other complementary procedures. Clearly, the use of these adjunctive and complementary procedures should be the subject of a future consensus process. One important limitation is the lack of strong evidence regarding the effective use of these procedures for children.
Another limitation was the lack of comprehensive analysis of the chiropractic educational process regarding pediatrics. A review of the chiropractic college pediatric curricula and post graduate pediatric educational programs should be performed with recommendations made by a future consensus panel. Furthermore, it would be an important step to develop a “model curriculum” for chiropractic education that will operationalize the recommendations made in the current document. Current efforts have been initiated by members of the project team to address this step.
Lastly, a limitation of any consensus process is that it represents chiefly expert opinion, which is a less convincing level of evidence than that provided by large-scale experimental studies. However, in the absence of a substantial body of literature and evidence, clinical practice must continue. Providing a reasonable approach to such clinical practice, developed through a formal consensus of expert opinion based upon best available evidence, is an important part of filling the knowledge gap. Meanwhile, it is essential that rigorous observational and experimental studies be implemented to provide a more substantial body of evidence to inform future clinical guidelines.
Conclusion
This consensus document describes the procedures and other features of chiropractic care which, based on the expert panel's clinical experience and the available evidence, represent the most beneficial approach to chiropractic care for infants, children, and adolescents. This document provides a general framework for what constitutes an evidence-based and reasonable approach to the chiropractic management of infants, children, and adolescents. It should not be seen as a final product, but rather as a work-in-progress that will require refinement as new evidence emerges in the future.
Practical Applications
The consensus process using a multidisciplinary panel was successful in developing a set of seed statements concerning the key issues related to chiropractic care for infants, children, and adolescents.
This document provides a general framework for what constitutes an evidence-based and reasonable approach to the chiropractic management of infants, children, and adolescents.
It should not be seen as a final product, but rather as a work-in-progress that will require refinement as new evidence emerges in the future.
Funding Sources and Potential Conflicts of Interest
This study was funded by grant #08-04-01 from the Foundation for Chiropractic Education and Research. No conflicts of interest were reported for this study.
Acknowledgment
The authors thank Cathy Evans, Project Coordinator, for her management of the complex communications required to develop the document. We thank Raheleh Khorsan, MS, who ensured that our background literature search was complete and comprehensive, and Denise Pahmeyer for assisting in data management and literature retrieval. All Delphi panelists served without compensation.
The document was developed with the many experts who generously donated their time and expertise. These include the members of the Steering Committee: Cheryl Hawk, DC, PhD; Michael Schneider, DC, PhD; Randy J. Ferrance, DC, MD; Elise Hewitt, DC; Meghan Van Loon, DC, PT; Lora Tanis, DC; Janine Gracy, MS; Claire Johnson, DC; MSEd; Gene Lewis, DC; MPH; Reed Phillips, DC, PhD; David Riley, MD; and Wendy Weber, ND, PhD, MPH.
The Delphi panelists played a central role in the document development, including: Linda Bowers, DC; Ali Carine, DO; Ezra Cohen, DC; Christina Cunliffe, DC, PhD; Scott Cuthbert, DC; Neill J. Davies, DC; Roger Engel, DC, DO; Karen Erickson, DC; Joan Fallon, DC, MSc; Margaret Finn, DC, MA, RN; Marc S. Gottlieb, DC; Paul J. Greteman, DC; Ronald Guild, DC; Jan Hartvigsen, DC, PhD; Sue Weber Hellstenius, DC, MSc; Lise Hestbaek, DC, PhD; Randy Hewitt, DC; Glenn E. Johnson, DC; Simone Knaap, DC, MSc; Anne Langford, DC; Robert Leach, DC, MS; Marc Malon, DC; Michael Master, DC; Joyce Miller, DC; Laurie Mueller, DC; Stephanie O'Neill, DC; Mary Jo Palmer, DC; Carol Phillips, DC; Ailsa van Poecke, DC, MScChiro; John Reggars, DC, MChiroSc; Anthony Rosner, PhD; Drew Rubin, DC; Todd Shaver, DC; Simone Simaan, MD, DC; Sharon Vallone, DC; Amy Watson, DC; and Kathryn Webb, DC.
References:
Barnes PM , Bloom B , Nahin RL:
Complementary and Alternative Medicine Use Among Adults and Children:
United States, 2007
US Department of Health and Human Services,
Centers for Disease Control and Prevention,
National Center for Health Statistics, Hyattsville, MD, 2008.Jones, MA, Stratton, G, Reilly, R, and Unnithan, VB.
A school-based survey of recurrent non-specific low-back pain prevalence
and consequences in children.
Health Educ Res. 2004; 19: 284–289Driever, MJ.
Are evidence-based practice and best practice the same?
West J Nurs Res. 2002; 24: 591–597Sackett, DL, Rosenberg, WM, Gray, JA,
Haynes, RB, and Richardson, WS.
Evidence-Based Medicine: What It Is and What It Isn't
British Medical Journal 1996 (Jan 13); 312 (7023): 71–72Sackett, DL, Straus, SE, and Richardson, WS.
Evidence-based medicine: how to practice and teach EBM. 2nd ed.
Church Livingston, Edinburgh; 2000Meeker, WC and Haldeman, S.
Chiropractic: A Profession at the Crossroads of Mainstream and Alternative Medicine
Annals of Internal Medicine 2002 (Feb 5); 136 (3): 216–227Chou R, Huffman LH; American Pain Society.
Nonpharmacologic Therapies for Acute and Chronic Low Back Pain:
A Review of the Evidence for an American Pain Society/
American College of Physicians Clinical Practice Guideline
Annals of Internal Medicine 2007 (Oct 2); 147 (7): 492–504Bronfort, G, Haas, M, Evans, R, Kawchuk, G, and Dagenais, S.
Evidence-informed Management of Chronic Low Back Pain
with Spinal Manipulation and Mobilization
Spine J. 2008 (Jan); 8 (1): 213–225Hurwitz, EL, Carragee, EJ, van der Velde, G et al.
Treatment of Neck Pain: Noninvasive Interventions: Results of the Bone and Joint Decade
2000–2010 Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S123–152Cassidy, DJ, Boyle, E, Cote, P et al.
Risk of Vertebrobasilar Stroke and Chiropractic Care:
Results of a Population-based Case-control and Case-crossover Study
SPINE (Phila Pa 1976) 2008 (Feb 15); 33 (4 Suppl): S176–183Hurwitz, EL, Morgenstern, H, Vassilaki, M, and Chiang, LM.
Frequency and clinical predictors of adverse reactions to chiropractic care
in the UCLA neck pain study.
Spine. 2005; 30: 1477–1484Brantingham, JW, Globe, G, Pollard, H,
Hicks, M, Korporaal, C, and Hoskins, W.
Manipulative therapy for lower extremity conditions:
expansion of literature review.
J Manipulative Physiol Ther. 2009; 32: 53–71Hawk C, Knorsa R, Lisi A, Ferrance RJ, Evans MW.
Chiropractic Care for Nonmusculoskeletal Conditions: A Systematic Review
With Implications For Whole Systems Research
J Altern Complement Med. 2007 (Jun); 13 (5): 491–512Gotlib, A and Rupert, R.
Chiropractic Manipulation in Pediatric Health Conditions - An Updated Systematic Review
Chiropractic & Osteopathy 2008 (Sep 12); 16: 11Vohra, S, Johnston, BC, Cramer, K, and Humphreys, K.
Adverse Events Associated With Pediatric Spinal Manipulation: A Systematic Review
Pediatrics. 2007 (Jan); 119 (1): e275-83Manchikanti, L, Boswell, MV, and Giordano, J.
Evidence-based interventional pain management: principles, problems,
potential and applications.
Pain Physician. 2007; 10: 329–356Miller, J and Benfield, K.
Adverse Effects of Spinal Manipulative Therapy in Children Younger Than 3 Years:
A Retrospective Study in a Chiropractic Teaching Clinic
J Manipulative Physiol Ther 2008 (Jul); 31 (6): 419–423Thiel, HW, Bolton, JE, Docherty, S, and Portlock, JC.
Safety of Chiropractic Manipulation of the Cervical Spine:
A Prospective National Survey
Spine (Phila Pa 1976). 2007 (Oct 1); 32 (21): 2375–2378 ([discussion 2379])Gotlib, A and Rupert, R.
Assessing the Evidence for the Use of Chiropractic Manipulation in Paediatric Health Conditions:
A Systematic Review
Paediatr Child Health. 2005 (Mar); 10 (3): 157–161Campbell, JB, Busse, JW, and Injeyan, HS.
Chiropractors and vaccination: a historical perspective.
Pediatrics. 2000; 105: E43Kosseim, M, Rein, R, and McShane, C.
Implementing evidence-based physiotherapy practice for treating children
with low back pain: are we there yet?
Pediatr Phys Ther. 2008; 20: 179–184Fitch, K, Bernstein, SJ, Aquilar, MS, Burnand, B,
LaCalle, JR, Lazaro, P, van het Loo, M, McDonnell, J, Vader, J, and Kahan, JP.
The RAND UCLA Appropriateness Method User's Manual.
RAND Corp., Santa Monica (Calif); 2003
Return to PEDIATRICS
Return to BEST PRACTICES
Return to PEDIATRICS GUIDELINES
Since 10-18-2009


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |