

A Systematic Review of Chiropractic Care for
Fall Prevention: Rationale, State of the
Evidence, and Recommendations for Future ResearchThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: BMC Musculoskelet Disord 2022 (Sep 5); 23 (1): 844 ~ FULL TEXT
OPEN ACCESS Weronika Grabowska, Wren Burton, Matthew H. Kowalski, Robert Vining, Cynthia R. Long, Anthony Lisi, Jeffrey M. Hausdorff, Brad Manor, Dennis Muñoz-Vergara & Peter M. Wayne
Brigham and Women's Hospital and Harvard Medical School Division of Preventive Medicine,
Osher Center for Integrative Medicine,
900 Commonwealth Avenue, 3rd Floor,
Boston, MA, 02215, USA.Background: Falls in older adults are a significant and growing public health concern. There are multiple risk factors associated with falls that may be addressed within the scope of chiropractic training and licensure. Few attempts have been made to summarize existing evidence on multimodal chiropractic care and fall risk mitigation. Therefore, the broad purpose of this review was to summarize this research to date.
Main text: Systematic review was conducted following PRISMA guidelines. Databases searched included PubMed, Embase, Cochrane Library, PEDro, and Index of Chiropractic Literature. Eligible study designs included randomized controlled trials (RCT), prospective non-randomized controlled, observational, and cross-over studies in which multimodal chiropractic care was the primary intervention and changes in gait, balance and/or falls were outcomes. Risk of bias was also assessed using the 8-item Cochrane Collaboration Tool. The original search yielded 889 articles; 21 met final eligibility including 10 RCTs. One study directly measured the frequency of falls (underpowered secondary outcome) while most studies assessed short-term measurements of gait and balance. The overall methodological quality of identified studies and findings were mixed, limiting interpretation regarding the potential impact of chiropractic care on fall risk to qualitative synthesis.
Conclusion: Little high-quality research has been published to inform how multimodal chiropractic care can best address and positively influence fall prevention. We propose strategies for building an evidence base to inform the role of multimodal chiropractic care in fall prevention and outline recommendations for future research to fill current evidence gaps.
Keywords: Balance; Chiropractic; Chiropractic care; Fall prevention; Falls; Gait.
From the FULL TEXT Article
Background
Almost 30% of adults over 65 years of age fall each year in the United States (US). [1] The prevalence of falls and mobility limitations increase with age with most older adults experiencing these by age 85. [2–5] Among community-living older adults, falls are the leading cause of serious injury, disability, nursing home placement, and injury-related death. [6–9] Fatal falls in older persons exceed the death rate from the opioid epidemic by a factor of four. [10, 11] Even non-traumatic falls can lead to fear of falling, reduced physical activity, psychosocial dysfunction, and loss of autonomy. [12–15]
The high incidence and long-term effects of falls among older adult results in substantial medical costs to individuals and society. [16] Falls and their consequences account for about 1–2% of all healthcare expenditures in the US, with estimates for fatal and non-fatal falls in 2015 of $637.5 million and $31.3 billion, respectively. [17] As the average age in developed countries continues to rise, both the prevalence of falls and their economic burden are expected to increase substantially. [16] This burgeoning public health crisis requires practical and effective strategies that can be readily implemented by health care providers on a national scale. The Centers for Disease Control and Prevention (CDC) recommends a multifactorial approach to fall prevention including identification of patient-specific fall risk factors, targeted exercises, and education. [18] Providers across all healthcare disciplines are being called upon to adapt to the changing needs of the older population, who are increasingly seeking alternative healthcare to address their specific needs. [19, 20]
The chiropractic profession represents one of the largest health care disciplines in the world [21–23] and is utilized by an estimated 18.5% of older adults in the US. [24] Chiropractic care is provided by licensed doctors of chiropractic (DC) who focus on prevention, diagnosis, and non-pharmacological treatment of neuro-musculoskeletal conditions. [25, 27] Chiropractors have been recognized by both the American Chiropractic Association and World Federation of Chiropractic as potentially playing a key role in reducing risk of falls in aging populations. [27] Interventions included within the scope of multimodal chiropractic care are utilized by DCs dependent on factors such as individual patient diagnosis and patient treatment preferences. These interventions include passive treatments (spinal manipulation (SM) and myofascial therapies), active treatments (therapeutic exercises and mind-body interventions), or educational treatments (lifestyle modifications, self-monitoring or self-management advice). [28] Though these nonpharmacologic therapies are used by other provider types, their use may differ substantially because factors such as specific training, practice scope, setting, and clinical skillsets likely influence how care is delivered. The benefit of these combined interventions as routinely delivered by chiropractors warrants further research.
In principle and practice, multimodal chiropractic care has the potential to mitigate many factors that contribute to fall risk in older adults including: reduced musculoskeletal strength and flexibility; chronic pain and polypharmacy; diminished proprioception and vestibular function; and overall compromised gait health, mobility, balance confidence and self-efficacy. [29, 30] The multimodal nature of chiropractic care has the potential to target multiple risk factors, and thus may afford advantages over unimodal approaches, which address a single risk factor, to managing fall risks in older adults. [31, 32] To date, little research has been devoted to evaluating the impact of multimodal chiropractic interventions on falls in older adults. [33, 34] Therefore, the broad purpose of this text is to collate research to date and to map out an evidence-based framework for studying and implementing chiropractic care strategies and programs for fall prevention in older adults. We begin by outlining a conceptual framework that includes key modifiable risk factors associated with falls in older adults, and how, in principle, components of chiropractic interventions might impact these factors. We then present methods and findings of a formal systematic review of published evidence regarding the effects of components of multimodal chiropractic care on the prevalence of falls and clinical measures of balance and gait health. Finally, based on these findings, we outline suggestions for future research to address knowledge gaps and expand the evidence-base regarding multimodal chiropractic care for fall prevention in older adults.
Main text
Conceptual framework for studying the impact of multimodal
chiropractic care on falls, postural control, and gait health

Figure 1 Key modifiable factors that are targeted by multimodal chiropractic care include musculoskeletal strength and flexibility, pain, proprioception, vestibular function, and polypharmacy. In addition, knowledge gained through falls-related education could mitigate fall risks. [18] Figure 1 outlines a simplified schema of these key modifiable risk factors potentially influenced by multimodal chiropractic care. More comprehensive models that account for the complex interactions between fall risk factors are described by Shumway-Cook and Woollacott. [30] The evidence for multimodal chiropractic care influencing each of these factors is discussed below and schematically depicted in Figure 1.
Musculoskeletal strength
Loss of musculoskeletal strength is a significant risk factor for falls and fall-related fractures in older adults. [35, 36] A meta-analysis of studies in older adults reported that lower extremity weakness was associated with a 70% higher likelihood for any fall and 3–fold increased risk for recurrent falls. [37] Individual studies have implicated deficits in strength in toe flexor [38], knee extension [39], and hip abductor muscles. [40] Increased fall risk is also associated with upper extremity weakness [37], and more limited evidence suggests correlations between diminished trunk muscle strength and fall risk. [41] Experimental studies have also reported that sub-normative levels of isokinetic and isometric lower extremity strength increase the likelihood of falling following an induced gait perturbation. [42, 43]
Interventions commonly used in multimodal chiropractic care have the potential to positively impact musculoskeletal strength. [44, 45] These approaches can work to improve strength of targeted sets of muscles, as well as the efficiency of the overall musculoskeletal system. However, evidence that a typical course of chiropractic care can improve musculoskeletal strength, specifically in older adults, is limited. One recent randomized controlled trial (RCT) observed significant positive outcomes regarding isometric strength and core endurance in active-duty military personnel who received multimodal chiropractic care which included SM, education, advice, and reassurance. [46] Another RCT of adults with chronic non-specific neck pain, reported that a course of SM combined with exercise led to greater gains in neck strength and endurance as compared with a course of physical therapy. [47] However, parallel studies targeting chronic low back pain (LBP) did not report benefits of SM to lower extremity strength. [48]
A handful of smaller studies have also evaluated the short-term impact of individual sessions of SM on changes in muscle strength. One randomized controlled crossover trial in elite Taekwondo athletes (17–50 y) reported that, compared with a passive control movement, a single session of SM increased muscle strength and corticospinal excitability to ankle plantar flexor muscles. [49] Another study in younger healthy adults (mean age 28 y) reported that lumbo-pelvic joint manipulation, compared to a lumbar passive range of motion (ROM) control, resulted in a significant increase in quadriceps force and activation immediately following intervention, but this was not sustained after 40 minutes. [50] Finally, in healthy younger adults (< 45 y) a single session of SM targeting the sacroiliac (SI) joint resulted in increased quadriceps muscle strength. [51] While the findings of these studies support a potential benefit of SM on muscle strength, because of the relatively young populations evaluated, the results are not directly applicable to older adults.
In addition to SM, other techniques commonly used as part of multimodal chiropractic care also have the potential to impact musculoskeletal strength including prescriptive or supervised rehabilitative exercise, myofascial release, and other soft-tissue techniques [52] that center largely around improving muscle tone and function. One RCT in the elderly compared the effectiveness of utilizing core stabilization exercises alone versus combined myofascial release technique and core stabilization exercise. Improvements were seen in the combined care group’s core stability endurance (measured by the supine bridge test). [53] The utilization of exercise which targets muscular strength, balance, and gait, is widely supported in the literature as an effective component of multifactorial fall prevention strategies. [31, 64] However, as with SM, evidence regarding soft-tissue techniques is mixed [55, 56] and delivery of these interventions by chiropractors specifically has not been evaluated in older adults.
Musculoskeletal flexibility
Lower extremity and trunk flexibility are also associated with fall risk . In two cross-sectional studies of older adults, fallers exhibit decreased ankle dorsiflexion ROM compared to those who did not fall. [57, 58] In another cross-sectional study of older women, higher fall risk was associated with decreased trunk flexion ROM. [59] Studies in older adults have also reported that reduced extension mobility of the lower spine [60], and less flexible patterns of arm and trunk motions [61], are associated with increased fall risk.
There is evidence to support that components of multimodal chiropractic care can improve musculoskeletal flexibility, with limited studies evaluating the impact of SM alone on flexibility. One systematic review concluded that some short-term SM protocols result in clinically meaningful improvements in hamstring flexibility. [62] Another recent meta-analysis, evaluating the impact of cervical high-velocity low-amplitude manipulation reported a large positive effect on cervical ROM. [45] While links between cervical ROM and balance are not well understood, it has been suggested that in patients with neck pain there is a correlation between cervical joint stiffness, the hypertonicity of upper cervical musculature, and the presence of dizziness. [63]
Techniques used by chiropractors which target the myofascial system such as Instrument Assisted Soft Tissue Manipulation (IASTM) [64], proprioceptive neuromuscular facilitation (PNF) stretching [65], and myofascial release [66, 67] may positively impact musculoskeletal flexibility. IASTM has shown benefit in multiple reviews to improve ankle dorsiflexion in both athletic and ordinary populations. [64, 68, 69] PNF stretching is known to provide short term benefits to ROM. [70] In one RCT, combined IASTM and PNF stretching showed improvements in hamstring flexibility when compared to static stretching. [71] There is limited evidence to support the success of myofascial release alone in improving ROM, but one recent systematic review reported some improvement in trunk flexibility when paired with prescriptive stretching and exercise in patients with LBP. [72] A comparative effectiveness trial in a physically active young adult population evaluated the use of myofascial release technique compared to Graston Technique (an IASTM protocol). [73] Results showed improvements in ankle dorsiflexion with both treatments compared to a no-treatment control group. [73]
Pain
Pain has been shown to be an independent predictor of falls. [74–76] Chronic pain is strongly associated with poor gait measures, especially while performing cognitively demanding tasks, which suggests that it may act similarly to a cognitive distraction during walking for elderly. [75, 77] Consequently, pain can contribute to difficulties with mobility and thus to an increased fall risk. [57, 75, 78–80] Pain may have additional neuromuscular effects that lead to lower extremity weakness and slower response time, caused by both lack of physical activity and reflex muscle inhibition. [76, 81]
A substantiative body of research has evaluated the potential for multimodal chiropractic care to reduce or manage musculoskeletal pain. Recent systematic reviews and meta-analyses have concluded that SM as a part of multimodal chiropractic care has favorable outcomes on pain severity in patients with chronic LBP [82, 83] and acute LBP with radiculopathy. [84] Additional reviews also support that SM can be a beneficial component of treatment plans for reducing the severity of both neck [85, 86] and LBP. [87, 88] Of note, one review contrasted SM with both inactive and active (mobilization) controls. Findings were variable but indicated similar improvements in pain severity when SM was compared to the active control, and short-term improvements in pain severity when SM was compared to an inactive control. [86]
Systematic reviews support the use of myofascial massage to reduce pain in the short term for chronic neck and back pain. [89] Myofascial massage has also been reported as beneficial for improving multi-site pain [90] and post-operative pain. [84] Several trials [68, 91, 92] and one systematic review [69] support the use of IASTM to reduce pain severity. Preliminary research on PNF stretching has shown improvements in pain intensity in adults with chronic LBP. [93]
Exercise to reduce pain severity and disability is recognized in the literature as a crucial component of managing the severity of chronic neck and LBP. [89, 94] One systematic review reported benefits with both progressive aerobic training and progressive resistance training at reducing pain intensity. [95] Some benefit to pain management has also been noted in structured or community-based exercise programs such as yoga [96] and tai chi. [94, 97]
Preliminary research also shows promise for additional therapeutic modalities used by chiropractors to manage pain including transcutaneous electrical nerve stimulation (TENS) [92] and superficial heat. [84] One randomized controlled trial reported decreased pain levels in patients with chronic LBP following a course of combined TENS and IASTM. [92, 98] Further, reviews have shown short-term benefit with utilizing superficial heat to reduce pain severity. [84, 99]
Proprioception
Proprioception is essential for normal functioning of the body during movements, including maintaining balance and spatial awareness. [36, 100] Age-related decline in proprioception is associated with decreased functioning in muscle spindle proprioceptors, resulting in detrimental changes to sensitivity, acuity, and integration of sensory signals leading to increased risk of falls. [36, 101–103] Inhibition of input from the ankle specifically has been shown to negatively impact joint position sense [104] and altered balance. [101, 105, 106] Additional signals from proprioceptors found in the sole of the foot contribute sensory information regarding changes in distribution of contact pressures and the position of the body during stance and movement. [107, 108] Furthermore, as a result of aging and comorbid conditions, like diabetic peripheral neuropathy and lumbar nerve root impingement, sensitivity in these regions decrease and are frequently associated with a higher risk of falls. [109–111]
While it has been suggested that SM can impact spinal biomechanics, paravertebral muscle activation patterns, and proprioceptor signaling [112], there is a paucity of evidence supporting the benefits of components of multimodal chiropractic care in enhancing proprioceptive function. Early research has found decreased elbow joint position sense in participants with subclinical neck pain and reported no improvement of this measure following cervical SM. [113] A more recent RCT found improvements in ankle joint position sense in community-dwelling older adults in the intervention group which received multimodal chiropractic care (variable based on provider discretion). [114] Little research has been completed on the direct effects of SM on plantar sensation.
Components of multimodal chiropractic care such as soft tissue massage, prescriptive exercise, and kinesiology taping have shown mixed effectiveness in enhancing proprioception. Older adults who received massage following exercise saw benefit in measures of joint position sense [115] and changes in plantar sensation have been observed following the use of plantar massage. [116] The use of prescriptive exercise for the direct purpose of improving proprioceptive functioning is supported by one study showing improvement with lumbopelvic motor control exercise [117] but countered by another showing no changes following tactile acuity training. [115] A pilot study assessing the effectiveness of barefoot exercise on fall prevention in older adults found favorable effects on plantar sensation. [119] Lastly, another study reported that the use of kinesiology tape had no significant effect on lumbar repositioning errors. [120]
Vestibular function
Along with proprioception and vision, the vestibular system is a key contributor to postural stability and control. [36, 121] Dizziness, a widespread and significant symptom of age-related vestibular hypofunction, is associated with an increased fall risk. [122, 123] Data from the National Health and Nutrition Examination Survey supports a relationship in the elderly between vestibular impairment and an increased risk of falling. [124]
Evidence of chiropractic interventions to directly address vestibular dysfunction in the elderly is limited, but there is some which suggests procedures used within chiropractic may be effective for managing symptoms of dizziness. A small randomized trial evaluating the effectiveness of instrument assisted cervical or thoracic manipulation plus multimodal chiropractic care (manual soft-tissue therapy, mobilization, prescriptive exercise, and advice) reported favorable trends toward improvement measured with the Dizziness Handicap Inventory (DHI). [63] More broadly, systematic reviews focused on treatment of cervicogenic dizziness conclude that there is moderate evidence to support the use of manual therapies, including spinal mobilization and manipulation. [125, 126]
Some studies support a combination of other interventions which may be employed by chiropractors, for example physical (repositioning) maneuvers and exercise-based vestibular rehabilitation for longer-term functional recovery, including decreased levels of dizziness. [127] One study reported that the Epley maneuver was effective for long-term reduction of nystagmus among people with Benign Paroxysmal Positional Vertigo (BPPV). [128] Others showcase chiropractic clinical utilization of the Epley maneuver for BPPV with positive results. [129, 130] Additional evidence supports that movement-based interventions, which can be prescribed by a DC as part of a treatment plan, including vestibular rehabilitation exercises and Tai Chi can improve dizziness and balance resulting from vestibular dysfunction. [127, 131, 132]
Polypharmacy
Polypharmacy, which entails the use of multiple medications at the same time, is yet another independent fall risk factor in the elderly. [133–135] Several studies have shown the impact of polypharmacy on increasing fall risk in elderly populations, with some suggesting a monotonic dose-response relationship between the number of prescription drugs and the ensuing risk of injurious falls. [136–138] Polypharmacy increases risk of falls through adverse events such as dizziness and reduced cognitive function. [139] Opioid pain medications have been shown to either contribute directly to these symptoms, or increase the likelihood of their occurrence through drug-drug interactions. [140]
Although the vast majority of chiropractors are not trained or licensed to prescribe medications, through the positive impact of non-pharmacologic interventions on pain, it is plausible that chiropractic care can facilitate reduced pain medication use. A recent retrospective study utilizing medical claims data reported patients who saw a chiropractor for their spinal pain had half the risk of filling a prescription for opioids. [141] Others have found promising negative correlations between the use of chiropractic care and opioid prescription in both the private sector and the United States Department of Veterans Affairs (VA). [142, 143] Further, a recent large-scale observational study found that patients who had an initial visit for LBP with a chiropractor had 90% lower risk of using opioids in the short- and long-term, compared to those who sought their initial care from a primary care physician. [144] A recent systematic review and meta-analysis of observational studies in multidisciplinary healthcare systems reported that, compared to patients who do not receive chiropractic care for non-cancer pain, patients who do receive chiropractic are 64% less likely to be prescribed an opioid. [145]
While direct research evaluating the impact of utilizing specific chiropractic modalities on general medication use in the older population is scarce, early trials have assessed medication use as a secondary outcome measure. One study found significant decreases in the duration of medication use in an elderly population after receiving SM and completing prescriptive home exercises. [48] The same team studied adolescent populations, comparing interventions of exercise therapy alone or a combination of SM and exercise therapy, reporting an 80% decrease in medication use for both interventions. [146] Longer-term trials of prescriptive exercise have reported small but beneficial trends toward reducing medication use over time. [147, 148]
Education
Patient-centered education efforts have been acknowledged by the CDC as an essential part of fall prevention. [18] The efficacy of a multifactorial educational fall prevention program showed positive outcomes regarding functional improvements of an elderly population. [149] Several studies have shown benefit in reducing hospital-based falls by administering educational videos to both patients and families. [150, 151] The inherent multifactorial nature of education enhances its applicability in multiple settings by utilizing techniques such as structured health education classes, brochures, or home hazards evaluation.
Chiropractors are well-positioned to provide educational fall prevention efforts, as older patients are increasingly selecting manipulative therapies [20], and chiropractors frequently witness the outcomes of falls in their older patients. [152] One study suggests an important role of chiropractors in fall prevention may be in providing appropriate referral to patients with a history of falls. [153] Through evaluation of gait patterns they can also advise on footwear or determine if a podiatric intervention is necessary. [153] Other studies support a more active role of chiropractors as patient educators, offering advice to address environmental fall hazards in the home such as poor lighting, uneven or torn carpets, slippery floors and unsteady stationary objects. [18] However, the effectiveness of fall prevention-related education delivered by chiropractors has not been well studied.In summary, an incomplete but growing and compelling body of studies support the concept that multiple components of chiropractic care, both independently and together, may positively impact key risk factors for falls in older adults. Below we present the findings from a formal systematic review of published studies evaluating the effect of chiropractic care on fall prevalence, as well as its impact on clinical measures of balance and gait associated with fall risk.
Systematic review of the impact of chiropractic care
on falls, postural control, and gait health
The primary goal of this systematic review, embedded within this broader narrative review, is to identify and synthesize studies to date that evaluated the impact of components of multimodal chiropractic care on prevalence of falls. Given the limited evidence on this topic, and the well-established link between clinical measures of balance and gait and fall risk [29, 154, 155], we also include studies that have assessed the impact of chiropractic care on balance and gait related outcomes. Specific components of the chiropractic scope of practice assessed in this review include SM, myofascial therapies, thermal modalities (hot and cold packs), and prescriptive rehabilitative exercises. To be comprehensive, our search was neither limited to a specific timeframe, nor by population, medical conditions, or intervention duration.
Methods
Literature search

Table 1 Electronic literature searches were performed using PubMed, Embase, Cochrane Library, Physiotherapy Evidence Database (PEDro), and Index to Chiropractic Literature (ICL). The search was limited to the English language, and publication dates ranged from database inception to June 27, 2022. The search terms included, for example, “chiropractic,” “chiro*,” “manipulation” in combination with “gait,” “falls,” “vestibul*”, “dizz*”, or “balance.” Additional manual searches, based on references listed in the retrieved articles, were performed to complete the search. The full list of search terms is detailed in Table 1.
Eligibility criteria and synthesis
RCTs, prospective non-randomized controlled trials, observational single arm clinical trials, and crossover studies published in English, in which chiropractic manipulation or multimodal care was the primary intervention and the changes in falls, clinical measures of gait, balance and balance related outcomes (e.g., vestibular function, proprioception, dizziness) were the outcomes measured. Due to the great heterogeneity and small sample sizes of the identified studies meta-analysis was not employed. Synthesis was limited to narrative summaries.
Study selection and data extraction
Study eligibility assessment was performed independently by three researchers (WG, DMV, and WB) who applied eligibility criteria using an agreed upon protocol. Data were extracted by three reviewers (WG, DMV, and WB) independently using a standardized template generated in Microsoft Excel. Data related to study design, duration and frequency of the intervention program, type of the control group, sample size, and outcome measures were extracted for qualitative analysis in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklists (PRISMA) and are reported in Additional Files 1 and 2. [156]
Risk of bias assessment
Three researchers (WG, DMV, and WB) independently assessed the methodological quality of 13 RCTs and randomized crossover studies, using the updated 8 item Cochrane Collaboration Tool for assessing risk of bias. [157] The assessed criteria which included: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment for self-reported and objective measures, incomplete outcome data (attrition rates or intention to treat), selective reporting, and other bias (e.g., carry-over effects in cross-over trials or recruitment bias in randomized controlled trials). [157] The evaluated domains were assessed as low risk of bias (“+”), unclear risk of bias (“?”), high risk of bias (“–“), or, in certain cases, not applicable (“N/A”) according to the established criteria. [58] Any discrepancies in the evaluations conducted by two authors were discussed, and when need, resolved with the input of a fourth evaluator (PMW).
Results
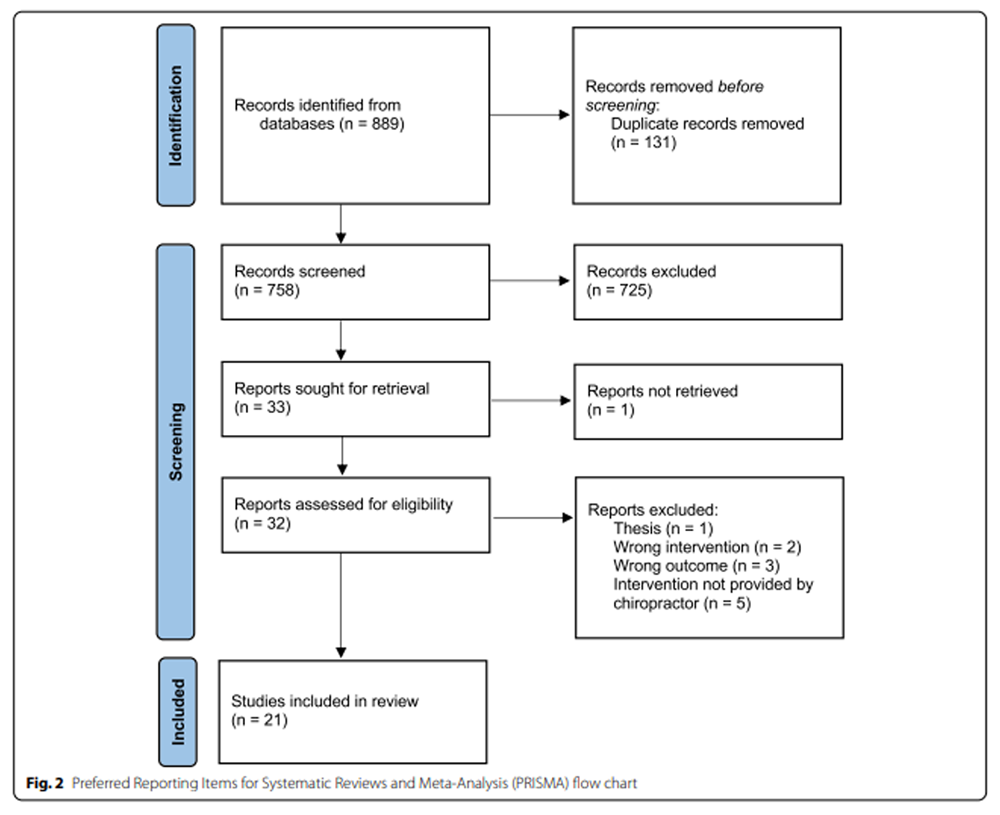
Figure 2 Figure 2 summarizes the flow of the literature search and selection process following PRISMA guidelines. An initial search identified 889 records from multiple databases and manual searches. Removing duplicates resulted in 758 records. The title and abstracts of these records were screened according to the inclusion criteria. A total of 32 full text articles met the initial eligibility criteria and were further reviewed. An additional 11 studies were excluded for no chiropractic intervention (n = 2), the intervention not being delivered by a chiropractor (n = 5), not reporting the outcomes of interest (n = 3), and a thesis (n = 1). Of the remaining 21 eligible studies, 10 were RCTs [27, 46, 63, 114, 158–163], 6 were single arm clinical trials [164–169], and 3 were cross-over studies [170,171,172]. One case series [173], and one observational study [34] were included.
Seven of the studies were purely descriptive and did not include inferential statistics. [34, 63, 158, 159, 164–166].
Fourteen of the included studies utilized inferential statistics, and reported p-values are included, when possible, in the summary of main findings. [46, 114, 160–163, 167–174]
Only three prospective studies had sample sizes greater than 100. [46, 161, 174]. The remainder had small sample sizes (< 32 per group) and thus were likely underpowered for formal inferential statistical analyses [114, 160, 162, 163, 167–173]
Three of these smaller studies included a power calculation completed a priori [114, 170, 172] and one was completed as part of the post hoc analysis. [162]
The remaining studies did not complete power calculations. [160, 163, 167–169, 171, 173]
Participants’ characteristics and study settings

Table 2 Table 2 summarizes the 21 included studies, reporting the most relevant findings pertaining to this systematic review. A total of 976 subjects were included. Data on baseline demographic characteristics regarding age were not reported in three studies [167–169], two studies reported median age of participants, and thus were not included in calculation of average participant age. [164, 166]
Of the remaining 16 studies (n = 909), the average participant age was approximately 52.25 years. Two studies did not report gender distribution [168, 169] and of the remaining studies (n = 965) approximately 48% of participants were female and 52% were male. Two of the 21 studies recruited young and healthy adults (20–40 years of age) [171, 172], and 8 studies included older adults (60+ years of age). [34, 63, 114, 158, 159, 161, 165, 174]
Five studies enrolled participants with SI joint conditions [160, 167–169, 173], 4 included subjects with neck pain or vertigo [63, 161, 164, 166], and 2 focused on subjects with LBP. [46, 169] No studies specifically included populations at high risk of falling.
Intervention and control group characteristics
Interventions are summarized in Table 2. Interventions employed within the scope of chiropractic practice were used in all 21 studies. The most commonly used interventions were SM (high-velocity low-amplitude (HVLA) or low-velocity mobilization) [34, 46, 114, 158–160, 162–170, 173], soft tissue manipulation (myofascial release and stretching) [63, 158, 159, 164–166], and thermal therapies (hot or cold packs). [63, 158, 159, 165, 166]. Two studies combined the chiropractic intervention with supervised rehabilitative exercises (SRE). [27, 161] Nine studies utilized specific techniques such as bioenergetic synchronization (n = 1) [158], Activator IItm instrument assisted manipulation (n = 1) [63], flexion-distraction (n = 1) [166], or specific joint manipulation such as the extremities (n = 2) [171, 172], ilium elongation (n = 1) [152], and SI joint mobilization (n = 3). [163, 168, 169]
Intervention duration ranged from a single session to 20 sessions delivered over 12 weeks. Individual intervention sessions ranged from 4 to 30 minutes, and the frequency of sessions varied between 1 to 3 times per week. Six studies adjusted the frequency and quantity of the SM based on individual needs of participants. [34, 46, 114, 161, 164, 174]
Thirteen out of 21 studies used comparison groups in their design. Three studies compared SM with an inactive or waitlist control group. [46, 162, 163] Four used home-based balance exercises or a mix of SM and exercise [158–161], and one compared a short-duration of these combined treatments to a long-duration. [174] One study used sham manipulation [63], and one used usual care as their comparison groups. [114] Finally, three studies used a crossover design; one used SM in combination with facet nerve blockade [170] and two used upper extremity and lower extremity manipulation in alternating order. [171, 172]
Outcome measures
Findings of the included studies were organized into 3 categories within the following text with respect to their outcomes, which included falls (n = 4) [114, 158, 159, 174], balance (n = 11) [34, 46, 63, 158, 159, 164–166, 170–172], and gait (n = 10). [63, 114, 160–163, 167–169, 173] These outcomes were considered even when they were not identified as the primary outcome of the study by the authors. Some studies included more than one category of outcomes (n = 5). [158, 159, 164, 170, 174]
Four studies reported frequency of self-reported falls; three measured falls prospectively as a secondary outcome measure or as part of adverse events monitoring [114, 158, 159, 174], and one observational study used self-reported falls as a covariate for a separate analysis on neck pain. [34] Clinical measures of balance included the Berg Balance Scale (BBS) (n = 4) [34, 158, 159, 165] and short form (SF)-BBS (n = 1) [166], measures of center of pressure (n = 1) [34], posturography for standing sway/stability (n = 4) [34, 170–172], single leg balance assessments (n = 4) [46, 158, 159, 165], Activities-specific Balance Confidence Scale (n = 1) [34], DHI (n = 5) [63, 158, 159, 165, 166], and vertigo severity (n = 1). [164] Measures of gait or mobility included gait symmetry (n = 4) [160, 167–169], Timed Up and Go (TUG) (n = 2) [63, 161], stepping reaction time (n = 1) [114], double support time (n = 2) [162, 163], and gait variability (n = 2). [162, 163]
Adverse events
Ten of the 21 studies provided limited descriptions of their AE monitoring protocols or procedures. [46, 63, 114, 158, 159, 161, 165, 166, 172, 174]. All of these reported AEs related to the provided interventions or study procedure including muscle soreness, neck pain, back pain, stiffness, dizziness, and headaches, which resolved within a range of 24–72 h post-manipulation. Only one study reporting AEs mentioned a serious AE that was unrelated to the study intervention. [161]
Risk of bias assessment

Table 3
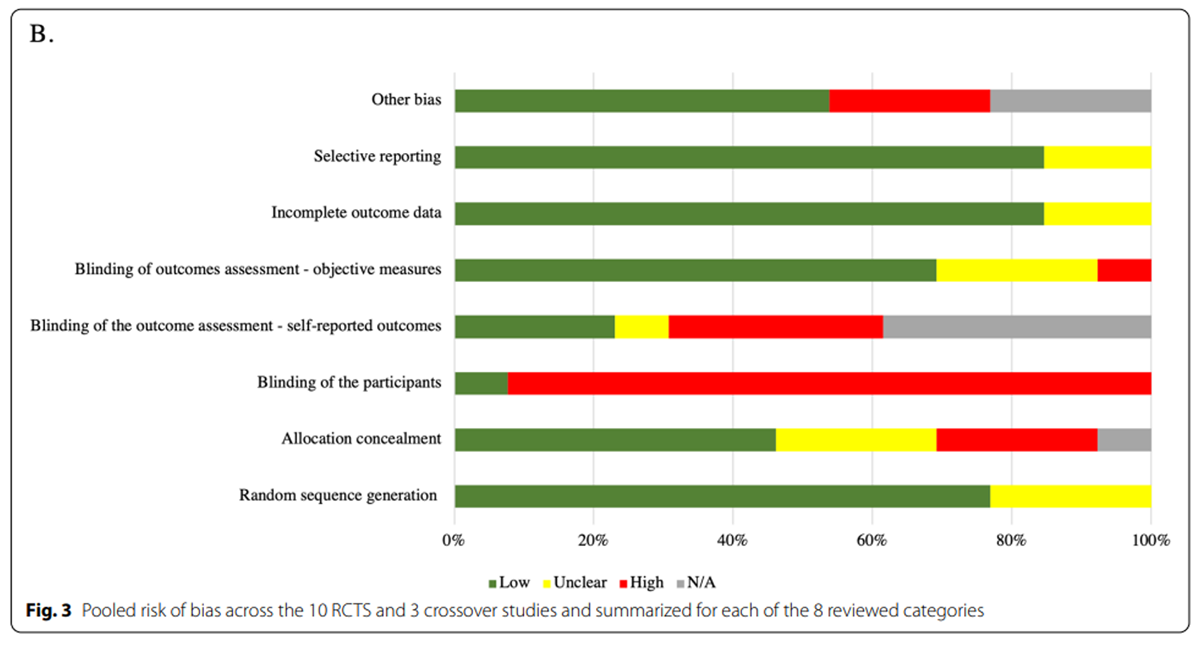
Figure 3 Ten RCTs and three cross-over studies were assessed for risk of bias (Table 3 and Figure 3). Randomization generation procedures were described in 10 (77%) studies; of those none had a high risk of bias. Low risk of bias was present in 6 studies (46%) for the allocation concealment and only in 1 (8%) for participants’ blinding. 5 studies (38%) did not collect any self-reported outcomes, while the remaining studies had differing risks of bias in this domain with 3 (23%) reporting low risk of bias, 1 (8%) reporting unclear risk of bias, and 4 (31%) reporting high risk of bias. Risk of bias associated with objective measures was low for 9 studies (69%), unclear for 3 (23%), and high for 1 (8%). 11 studies (85%) had low risk of bias for incomplete outcome data and selective reporting, while for the remaining 2 studies (15%) the risk of bias was unclear. High risk for other bias was present in 3 studies (23%), while it was unavailable in 3 (23%) and low in 7 (54%).
Summary of main findingsImpact of Chiropractic Care on Falls, Balance, and Gait.
Direct measures of falls
Four studies prospectively measured the impact of a chiropractic intervention on fall frequency. [114, 158, 159, 174] Maiers and colleagues evaluated falls as a secondary outcome in a RCT assessing the effectiveness of a long-term combined chiropractic and exercise intervention (36 weeks) compared to a short-term treatment plan consisting of the same combined interventions (12 weeks) for spinal disability (n = 182). [174] Fall incidence was assessed through self-report and direct questioning by the study staff at a clinical encounter every 12 weeks and collected for a 78–week period. In the short-term treatment group, the proportions of fallers reported at each 12–week measure ranged from 6 to 13%; in the long-term treatment group, values ranged from 10 to 13%. Between group differences were not statistically different at any measurement time, and within group changes were not reported for the falls data.
Two small RCTs that used multimodal chiropractic care as an intervention also reported on fall frequency. In 2007, Hawk and colleagues randomly assigned patients (n = 11) to two groups that received either multimodal chiropractic care or supervised exercise twice weekly for 8 weeks total. [158] Data on fall frequency and severity was collected at an intake interview section at each appointment, and during an exit interview following study completion. No obvious trends in fall frequency were observed; no statistical analyses were performed. A follow-up study by the same group compared three groups (n = 34) –– short-term multimodal chiropractic care (group 1), long-term multimodal chiropractic care (group 2), and home based exercise (group 3). [159] Frequency of falls were collected through direct questioning at each chiropractic visit and multiple outcome assessments over a period of 1 year. Group one, two and three had six, nine, and zero reported falls, respectively; no statistical analyses or descriptive statistics were reported. Lastly, an RCT (n = 60) by Holt and colleagues documented falls as part of adverse events monitoring, reporting seven total falls over the 13–month study period; five in the control group and two in the intervention group. [114] No statistical analyses were reported.
One other study by Holt and colleagues ascertained the history of falls retrospectively from 101 older (mean age 72 y) chiropractic patients using structured interviews, and reported that 34.6% experienced a fall in the previous year; however, no attempt was made to evaluate whether fall history was associated with any aspect of the received care. [34]
Clinical measures of balance
Various measures of balance were collected across 11 studies (total n = 391). [34, 46, 63, 158, 159, 164–166, 170–172] Five studies used BBS or SF-BBS to assess balance characteristics among the study participants, with lower scores indicating a greater risk of falling. [34, 158, 159, 165, 166] A small RCT (n = 11) by Hawk and colleagues reported a trend towards improvements in the BBS scores (diminished fall risk) following 8 weeks of multimodal chiropractic care [158], but no descriptive or inferential statistical analysis was used in this study. Similar descriptive trends were reported in another small pilot RCT (n = 34) conducted by the same group. [159] Another pre-post single arm study (n = 21) limited to descriptive statistics reported that 7 of the 15 patients over the age of 50 treated with multimodal chiropractic care, attained at least a 4–point improvement in the SF-BBS over the 8–week study period, suggesting a possible reduction in fall risk. [166] In another small (n = 14) single arm clinical trial assessing multimodal chiropractic care on older adults, findings were limited to descriptive statistics and suggest SF-BBS was largely unchanged after 16 visits [165]. Finally, an observational study (n = 101) described, on average, relatively high BBS scores amongst participating chiropractic patients. [34]
Four eligible studies used single leg standing outcomes to assess the balance among the participants who received multimodal chiropractic care. [46, 158, 159, 165]. One study utilized a single-leg protocol with eyes open and eyes closed, timed with floor sensors (n = 109). [46] Findings from this study indicated statistically significant and favorable results with eyes closed in the group receiving chiropractic care vs. the control group (p = 0.01), but no difference in single-leg balance with eyes open (p = 0.43). The remaining three studies used the one-leg standing test (OLST) including two RCT’s (n < 20 per group) and one single arm clinical trial (n = 14). Studies assessed varying frequencies of multimodal chiropractic care. None of these three studies used formal inferential statistics to assess the change in OLST over time. Descriptive summaries of findings suggest no consistent or clinically meaningful changes in OLST scores over the study period.
Another 4 studies used various measures of posturography and standing stability to assess balance. [34, 170–172] One small crossover study (n = 6) reported outcomes of posturography, which suggested no significant trends either on anteroposterior (AP) or mediolateral (ML) axis over the study periods. [170] In an observational study of elderly chiropractic patients (n = 101), posturographic stability measures including center of pressure and vertical force, were collected from 60 participants standing on a force plate for 20s with their eyes closed, and large impairments were observed. [34] Two crossover RCT studies utilized sensors that gathered outcomes of AP and ML translation, rotation (pitch and roll), pathlength, range, and Sample Entropy (SampEn) from three different anatomic locations (occiput, second sacral tubercle, and the surface participants stood on) during static postural assessments before and after chiropractic manipulation of the extremities. [171, 172] One of these (n = 24) reported significant improvements from the sensors at the second sacral tubercle and surface during the AP rocker board condition following upper extremity manipulation (both path p < 0.05). Significant improvements were also reported after lower extremity manipulation from the same sensor location and during the same surface condition (SampEn p < 0.05). Additionally, greater improvements were reported in range (p < 0.05) from the second sacral tubercle sensor in the upper extremity manipulation group when compared to the lower extremity manipulation group. The second study (n = 23) followed a similar design, but recorded outcomes related to center of pressure (COP) from force plates rather than from different surface conditions. A reduction of pathlength in the ML COP was observed after both upper and lower extremity manipulation (p = 0.005).
Five studies collected data on dizziness using the DHI (n = 104) with mixed and inconclusive results. [63, 158, 159, 165, 166]. An RCT by Hawk (n = 34) showed significant improvements from baseline DHI scores in the two intervention groups receiving different durations of multimodal chiropractic care compared to one group completing balance exercises. [159] Another RCT (n = 24) by Kendall and colleagues showed DHI scores with over 10 points decrease in both the intervention (4 weeks of multimodal chiropractic care including instrument assisted spinal manipulation, massage, heat, and exercise) and sham intervention groups. [63] A third RCT (n = 11) and a single arm clinical trial (n = 21) utilized intervention groups which received 16 sessions of multimodal chiropractic care. Both trials showed little to no improvement in DHI scores. [158, 166] An additional small single arm clinical trial (n = 14) utilizing the same intervention showed mixed results regarding participant’s DHI scores following the intervention period. [165] Lastly, a single arm clinical trial (n = 15) completed by Bracher and colleagues measured the severity of cervical vertigo symptoms following a novel combined treatment intervention including spinal manipulation, electrotherapy, medication and biofeedback exercise. Results showed that 12 of the study participants experienced either remission or improvement of cervical vertigo over the course of treatment; however, the results varied by the measured severity of the subjects’ vertigo. [164]
Gait
Ten studies collected data on mobility and gait health parameters (total n = 434). [63, 114, 160–163, 167–169, 173] Two studies used TUG tests to assess mobility in older adults (n = 265). Maiers and colleagues reported on TUG test times in two experimental groups, one receiving multimodal chiropractic combined with home exercise and one receiving SRE combined with home exercise, as well as one control group which completed only home exercise. [161] Results showed no significant between group differences in TUG test time measures taken at 12 weeks compared to baseline. [161] Measures from two-arm RCT by Kendall and colleagues (n = 24) reported small TUG test time improvements in the group receiving chiropractic between baseline and 4–week completion, however no statistical analysis was performed. [63]
In an RCT (n = 60) comparing individualized chiropractic treatment vs ‘usual care’ in community-dwelling older adults [114], chiropractic treatment lead to improvements in choice stepping reaction time (p < 0.05) and ankle joint position sense (p < 0.05) compared to the control group. [114] Two small RCTs (n = 11) completed by Ward and colleagues measured the impact of bilateral SI joint manipulation on gait variability (defined as approximate entropy of the hip, knee, and ankle joint angles over multiple gait cycles) captured with a VICON motion analysis system among individuals with a leg length inequality. [162, 163] Neither of these studies reported improvements in gait variability measures following the intervention. [162, 163]
A 2–week single arm clinical trial (n = 11) by Herzog and colleagues utilizing force platform analysis, resulted in a statistically significant difference between the distribution of gait loading forces (i.e., vertical and mediolateral) post SI joint manipulation. [167] Reduction in pain on visual analogue scale was also associated with improved gait parameters and decreased ground reaction forces in AP and ML directions, indicative of decreased gait asymmetry. [167] However, the results from follow-up studies by Herzog and colleagues were not consistent. In a single arm clinical trial (n = 11) no changes in gait asymmetry were found following a single manipulation session [168], while a 4–week RCT (n = 37) completed afterwards showed a significant improvement on all measured ground reaction forces in the spinal manipulation group compared to a physiotherapy ‘Back School’ intervention. [160, 168]
Another small single arm clinical trial (n = 9) evaluated the effect of a single manipulation by utilizing force platform analysis which measured temporal and kinetic variables, and showed SI joint manipulation has a tendency to reduce gait asymmetries assessed through a symmetry index. [169] Conversely, a biomechanical analysis of gait conducted in a 5–week case series (n = 10) focused on the use of mechanical and manually assisted SM for SI joint mobility, showed no differences in gait or gait asymmetry in study subjects pre- and post- treatment. [173]
Discussion
The initial narrative section of this paper on the impact of chiropractic care and its individual component modalities on multiple fall-related risk factors supports the idea that chiropractic care targeting musculoskeletal strength and flexibility, pain, proprioception, vestibular function, polypharmacy, and education could be a promising intervention for reducing falls and improving balance and mobility in older adults. However, our embedded formal systematic review did not identify a single clinical trial designed and adequately powered to directly evaluate the long-term impact of chiropractic care on the prevalence of falls in older adults. Moreover, the majority of studies evaluating the impact of chiropractic care on clinical measures of balance and mobility known to be associated with fall risk, were small, statistically underpowered, of low methodological quality, and typically did not target older adults at risk for falls. Thus, while the potential seems to be clear, our findings both highlight a significant gap in the evidence base for the use of chiropractic care for fall prevention, and underscore the need for developing future directions for research evaluating both the effectiveness of chiropractic care for reducing falls and fall-related injuries in older adults. Our findings also point to the need for research aimed at understanding the mechanistic processes through which the individual and combined components of chiropractic care impact fall-related risk, which could help refine and target intervention to meet the needs of populations with specific risk factors and related comorbidities.
Four clinical trials prospectively measured the impact of elements of chiropractic care on falls. The largest and most methodologically sound study was a 2 arm RCT by Maiers and colleagues that compared two durations of combined chiropractic care with SRE, and collected falls data via self-report. [174] Findings from this study, however, are limited by lack of a non-intervention control group and lack of information regarding the statistical power required to detect between group differences in falls (which were defined a priori as a secondary outcome). Variability in how and when falls data were collected, and complete reliance on self-report and recall, with no method to adjudicate falls, also limit the rigor of this and all studies in this review with respect to evaluating falls. [175] A second study was also not designed or powered for detecting changes in fall frequency following an intervention, with information only collected as part of adverse events monitoring. [114] Additionally, both studies completed by Hawk and colleagues were also underpowered to detect falls and data were not statistically analyzed. [158, 159] Collectively, these studies illustrate the challenges researchers face in quantifying fall frequency in the context of clinical trials. Recent trials on multifactorial fall prevention programs offer some guidance for improving the rigor associated with estimating fall frequency including combining the use of patient completed fall logs with systematic phone or in-person queries [176–180], or adjudicating logs with reports embedded within medical records (e.g., emergency department visits or radiographic records. [181–183] Other approaches that leverage emerging technologies include the use of wearable sensors or camera-based home surveillance for long-term continuous monitoring of high-risk populations. [184, 185]
The most commonly assessed outcome measures in the studies identified by our formal systematic review were related to measures of balance and gait. With respect to balance, five studies collected BBS (or SF-BBS) scores [34, 158, 159, 165, 166], which in recent reviews has shown conflicting agreement for its suitability in predicting falls. [186, 187] Five of the included studies collected DHI scores [63, 158, 159, 165, 166], which is a widely accepted clinical measure for assessing the impact of dizziness on quality of life and activities of daily living. [188, 189] All of the studies reporting BBS (or SF-BBS) and DHI scores were small and used descriptive statistics to report their data, therefore no conclusions can be drawn on the impact chiropractic care may have on either of these outcomes. Four studies collected posturography measures for standing sway or stability using ground reaction forces from force plates or body sensors [34, 170–172], and an additional four collected measures of gait symmetry. [160, 167–169] While each of these clinical balance outcomes evaluated has shown some links to fall risk [154, 187, 190–192], there remains much debate about the best measures of balance for predicting falls. [193–195] Future studies should consider recently validated outcome measures, which take into account the dynamic conditions of balance such as the Balance Evaluation Systems Test (BEST), or miniBEST, which have shown promise in identifying and differentiating balance and gait deficits [196–198] as well as correlations to falls in the older population. [199, 200] Similarly, multiple characteristics of gait, including speed and stride time variability, have also been associated with fall risk. [154] Unfortunately, most of the identified studies that evaluated gait were small and did not include statistical analyses, limiting their contribution to our understanding of chiropractic care on mobility and fall prevention. Well-designed studies evaluating the impact of chiropractic care on key parameters of gait health in at risk older adults should be a priority area for research. In addition to outcomes associated with gait health informing practical issues of mobility and functional ability to engage in everyday activities of daily living, they also provide insight into the biomechanical and neurophysiological processes underlying fall risk. There is also growing evidence that gait assessed outside the laboratory using wearable sensors, during activities of daily living, may be particularly helpful in predicting falls, and thus future studies should also consider outcomes assessing gait under daily living conditions. [201, 202]
Proposed strategies for building an evidence base to inform
the role of chiropractic in fall prevention
Below we propose several strategies that may be used to begin addressing the evidence gap related to chiropractic care and fall prevention. While ultimately, fully powered multi-site RCTs will provide the least biased and most rigorous source of evidence, given both the cost of such trials as well as the current paucity of studies to inform their design, large scale RCTs may not be the most effective strategy for beginning to build an evidence base. Rather, initial approaches which aim to build foundational knowledge to inform such trials, including the leveraging of existing large healthcare databases for observational or retrospective analyses, pilot clinical trials, and mechanistic studies to better understand the effects of specific components of multimodal chiropractic care on known fall risk factors are likely to yield the most pragmatic and initially informative evidence.
Observational studies leveraging existing databases
One practical first step to better understanding the association between chiropractic care and fall risk would be to leverage data from existing large databases available through managed care facilities, health claims data, and clinical systems such as the VA. Previous studies utilizing such databases, for example, have determined that chiropractic care is associated with reduced likelihood of adverse drug events [203] and filling opioid prescriptions [204], as well as determining correlations between chiropractic patient characteristics (i.e. gender, age, body mass index) and clinical outcomes such as pain and disability. [205, 206] Such databases could be leveraged to characterize the relationship between incidence of falls related outcomes and prior and/or future exposure to chiropractic care. For example, retrospective analyses could include comparisons between chiropractic and non-chiropractic patients in terms of frequency of reported falls, fall-related injuries, and medical costs associated with falls. Importantly, large databases could include invaluable information related to comorbidities (e.g., pain conditions, depression), risk factors for falls (e.g., polypharmacy), and multiple sociodemographic factors known to impact fall risk. Integrating these variables into thoughtful, pre-specified analyses could lead to more focused, population specific hypotheses to evaluate in clinical trials. Such approaches could rely on well-established statistical approaches, including multivariate modeling, propensity score matching, and machine learning. [207–211]
One potential challenge in retrospective studies using databases could be the availability of consistent and reliable data on falls. Prior studies suggest that this information is not always clearly coded in an electronic medical record but may be obtained through more innovative methods such as natural language processing or machine learning algorithms applied to medical notes within electronic health records. Several approaches have been shown to be successful utilizing International Classification of Disease codes in medical claims data to determine risk of opioid prescription for chiropractic patients [141, 181, 212–216] and developing sophisticated algorithms for the analysis of falls and related outcomes such as injuries and cost. [181] Chiropractic health care services at the VA show promise in this regard due to both the increasing number of chiropractors nationwide in their complete health care system and previous research which has extracted data on falls utilizing the above-described methods. [217]
Another alternative observational study approach would be a non-randomized prospective cohort study with a non-exposed group control. For example, patients in a large Health Maintenance Organization who are screened for high fall risk and enrolled in chiropractic care could be longitudinally and systematically monitored for fall related outcomes and compared to equivalent patients not receiving chiropractic care. Advantages to this approach include interventions reflecting real-world care, reduced effort in patient recruitment, and higher enrollment rates (due to certainty of allocation). Limitations to this approach include difficulty in matching groups with respect to potential confounders even with large sample sizes. As with retrospective observational studies, non-randomized prospective trials may be useful in the early stages of research by informing design features of future randomized trials, such as most responsive population, dosage for exposure, and specific components of multimodal interventions.
Randomized controlled trials
An essential step to further progress in building an evidence base for chiropractic services in the realm of fall prevention would be the initiation of large-scale prospective RCTs specifically targeting adults at risk for falling, fully-powered to detect changes in frequency and severity of falls. Based on both the general literature on the efficacy of multifactorial interventions for falls [201], as well as the effectiveness of chiropractic care for many musculoskeletal conditions, the evaluated chiropractic interventions should be multimodal as opposed to isolated components (e.g. SM alone). Promising interventions provided by chiropractors should likely include combinations of SM, myofascial therapies, supervised and prescriptive exercise, and self-management strategies. Pragmatic designs might be used to evaluate the relative effectiveness of different combinations of these interventions, different dosages, and different strategies for implementation (e.g., combining in person care with virtual education or exercise training). Comparisons may also be made to existing programs recommended by the National Council on Aging, such as Tai Chi or Otago, or usual medical care, employing comparative effectiveness designs, or equivalency or non-inferiority designs. [218, 219] As noted above, advances in digital medicine regarding the use of wearable devices have recently established the relationship between everyday gait and injurious falls in the older population, providing an alternative approach to objectively assessing gait health and fall risk following well-defined exposures. [202, 220] Finally, these studies could be combined with data regarding medical utilization and costs to evaluate the cost effectiveness of these interventions.
As with every large-scale trial, smaller scale feasibility and pilot trials should be conducted to inform final study features including recruitment and retention procedures, fidelity of intervention delivery, selection of primary and secondary outcomes and protocols for outcomes assessment, infrastructure for data management and ethical oversight across multiple sites. Consolidated Standards of Reporting Trials (CONSORT) and other guidelines for the design and reporting of pilot clinical trials are now widely available. [221, 222]
Additional consideration could be given to experimentally evaluating the benefits of delivering existing validated fall preventions resources to chiropractic providers in order to better identify fall risks within their older adult patients. Existing high-quality educational resources which recommend multifactorial approaches to fall prevention include the CDC’s Stopping Elderly Accidents, Deaths & Injuries (STEADI) Older Adult Fall Prevention [18], or those endorsed by the United States Preventive Services Task Force [223], could be administered to and adopted by chiropractors in private clinical practice and within large healthcare systems. Once identified, high-risk fallers could be triaged to specific evidence-based interventions or protocols, or ongoing trials evaluating novel therapeutic approaches.
Mechanistic studies
Elucidating the mechanism underlying any therapeutic intervention is important, as plausible mechanistic models are considered to be part of the totality of evidence for any modality. Chiropractic care’s multimodal nature and heterogeneity in its delivery poses challenges to simple, single-factor, cause-and-effect reductionist models. As is emphasized in the narrative part of our review, the impact of a chiropractic care intervention on fall risk is likely to result from changes in multiple physiological processes, individually, additively, and synergistically. For example, observed changes in falls following a multimodal intervention could be results of improvements in lower extremity strength and flexibility, enhanced proprioception, and reduced pain and associated executive function distraction. These changes could lead to behavioral changes (e.g., reduced fear of falling and enhanced exercise self-efficacy) or underlying changes in brain network dynamics, which might feedback and further alter physiological process previously mentioned. For these reasons, a strong case can be made for focusing limited resources on pragmatic trials that evaluate overall effectiveness of chiropractic intervention.
Despite complexity and heterogeneity related challenges inherent to chiropractic care, mechanistic research can be advanced in three complementary ways. First, specific cause and effect hypotheses could be tested with carefully designed efficacy trials, extending some of the studies cited in this review. For example, RCTs could evaluate the impact of a well-defined and systemically delivered SM protocol on pelvis or lower extremity electromyography (EMG) dynamics and resulting biomechanics of gait known to contribute to balance and postural control. Attention or sham manipulation experimental controls could be utilized, as can dose escalation designs, to infer cause and effect. Recent studies have used such designs to probe the impact of short-term SM on brain neural networks. [224, 225]
Another approach to inform a mechanistic understanding could be based on traditional factorial designs, or newer strategies including Multiphase Optimization Strategy (MOST) and the Sequential Multiple Assignment Randomized Trial (SMART) designs. Such approaches can inform interactions between therapeutic components on both specific physiological outcomes (e.g., joint biomechanics) or more synthetic clinical outcomes (frequency of falls). Examples of factorial designs being employed in chiropractic research includes evaluating the individual and combined effects SM and prescribed exercise, or SM and self-care on musculoskeletal pain. [47, 48, 86, 146, 148, 161, 174]
A third and complementary approach would be to embed a variety of carefully chosen physiological markers into pragmatic trials to test specific secondary hypotheses regarding their association with falls. For example, laboratory measures ranging from brain function assessed during movement tasks using functional magnetic resonance imaging (fMRI) to conventional markers of gait health (e.g., gait initiation, speed, stride time variability, dual task gait performance) could be assessed longitudinally over the course of an intervention. Multivariate analyses, including tools such as structural equation modeling could be employed to inform or test causal hypotheses linking specific physiological or biomechanical processes to clinical outcomes of interest (e.g., fall frequency or severity). As noted above, recent advances in wearable technology could be used to assess a diverse array of mobility markers during everyday living over extended periods of time. Observational studies using machine learning show promise informing the relationship between these physiologic markers assessed in the real world and fall risk [182, 183, 217], but have not yet been widely used in intervention studies.
Limitations
There are a number of limitations to this study. First, only studies in the English language were included, the search strategy was developed without formal help from a librarian, and a protocol was not developed or registered a priori. Second, based on the limited evidence to date, only a small number of studies met our inclusion and exclusion criteria. Third, there was a great deal of heterogeneity across the included studies in terms of study design characteristics, methodologic quality, demographics of participants, interventions, outcomes, and settings, excluding the possibility of quantitative synthesis with meta-analysis, and significantly constraining narrative synthesis. Of note, the majority of included studies were small pilot studies, with overall low methodological quality. Collectively, this heterogeneity and low methodological quality limits the conclusions that can be drawn from these data. Fourth, our inclusion criteria targeted studies that included evaluations of components of multimodal chiropractic care (e.g. SM, myofascial therapies), as delivered by a DC. Some of these modalities are also delivered by other professions (e.g., osteopath, physical therapist), and because of the limits of our search strategy, our findings cannot distinguish chiropractic-specific impacts of the included interventions compared to the impacts of these interventions as delivered by other professions.
Conclusions
Falls in the older population represent a large and growing public health issue. Based first on principle, multimodal chiropractic care shows promise in contributing positively to fall prevention efforts. In addition, the chiropractic profession is well positioned for implementation on a wide scale, however, to date limited evidence is available. Through a well-coordinated set of observational, mechanistic and randomized-controlled studies, this evidence gap can be filled and the potential of multimodal chiropractic care can be evaluated. Future research on falls and mobility represents both an exciting area of contribution for the chiropractic profession and a critical topic for public health.
Supplementary Information
Abbreviations
ABCs = Activities-Specific Balance Confidence Scale
AE = Adverse Events
AP = Anteroposterior
APA = Anticipatory Postural Adjustments
BBS = Berg Balance Scale
BEST = Balance Evaluation Systems Test
CDC = Centers for Disease Control and Prevention
COG = Center of Gravity
CONSORT = Consolidated Standards of Reporting Trials
COP = Center of Pressure
DC = Doctor of Chiropractic
DHI = Dizziness Handicap Inventory
DS time = Double Support time
DSP% = Double Stance Phase Percentage
EMG = Electromyography
EQ-5D = European Quality of Life Five Dimensional Instrument
FABQ = Fear Avoidance Beliefs Questionnaire
FES-I = Falls Efficacy Scale International
fMRI = Functional Magnetic Resonance Imaging
GDS = Geriatrics Depression Scale
GRF = Ground Reaction Forces
HVLA = High-Velocity Low-Amplitude
IASTM = Instrument Assisted Soft Tissue Manipulation
LBP = Low Back Pain
ML = Mediolateral
MMSE = Mini-Mental State Examination
MOST = Multiphase Optimization Strategy
NDI = Neck Disability Index
ODI = Oswestry Disability Index
OLST = One-Leg Stance Test
PDI = Pain Disability Index
PNF = Proprioceptive Neuromuscular Facilitation
PRISMA = Preferred Items Reporting for Systematic Reviews and Meta-Analysis
PROMIS-29 = Patient-Reported Outcomes Measurement Information System
RCT = Randomized Controlled Trial
RMDQ = Roland Morris Disability Questionnaire
ROM = Range Of Motion
SACT = Single Arm Clinical Trial
SF-36 = 36 Item Short Form Survey
SF-BBS = Short-Form Berg Balance Scale
SI = Sacroiliac
SM = Spinal Manipulation
SMART = Sequential Multiple Assignment Randomized Trial
SPPB = Short Physical Performance Battery
SRE = Supervised Rehabilitative Exercise
STEADI = Stopping Elderly Accidents, Deaths & Injuries
TENS = Transcutaneous Electrical Nerve Stimulation
TO = Toe-Off
TSK = Tampa Scale of Kinesiophobia
TUG = Timed Up and Go
VA = United States Department of Veterans Affairs
VAS = Visualized Analog Scale
Funding
PMW is funded by a K24 grant. WB receives funding from National Chiropractic Mutual Insurance Company (NCMIC). These funding bodies have no impact on the design of the study, collection, analysis, interpretation of data, or writing of the manuscript. No other authors have funding to declare.
Contributions
Weronika Grabowska and Wren Burton are co-first authors. WB, WG, and PMW contributed to the study design and drafting the manuscript. WG and DMV contributed to the acquisition and screening of the articles to be included in the embedded systematic review. WG, WB, and DMV independently extracted data from the included studies and assessed for risk of bias. MHK, RV, CRL, AL, JMH, BM, DMV, and PMW substantively revised this work. All authors read and approved the final manuscript.
Competing interests
No authors report financial or non-financial competing interests.
References
Masud T, Morris RO.
Epidemiology of falls.
Age Ageing. 2001;30(Suppl 4):3–7.Tinetti ME, Speechley M, Ginter SF.
Risk factors for falls among elderly persons living in the community.
N Engl J Med. 1988;319(26):1701–7.Jehu DA, Davis JC, Falck RS, Bennett KJ, Tai D, Souza MF, et al.
Risk factors for recurrent falls in older adults: A systematic review with meta-analysis.
Maturitas. 2021;144:23–8.Gawronska K, Lorkowski J.
Falls, aging and public health - a literature review.
Ortop Traumatol Rehabil. 2020;22(6):397–408.Sousa LM, Marques-Vieira CM, Caldevilla MN, Henriques CM.
Risk for falls among community-dwelling older people: systematic literature review.
Rev Gaucha Enferm. 2017;37(4):e55030.Tinetti ME, Williams CS.
Falls, injuries due to falls, and the risk of admission to a nursing home.
N Engl J Med. 1997;337(18):1279–84.Shaver AL, Clark CM, Hejna M, Feuerstein S, Wahler RG, Jacobs DM.
Trends in fall-related mortality and fall risk increasing drugs
among older individuals in the United States,1999–2017.
Pharmacoepidemiol Drug Saf. 2021;30(8):1049–56.James SL, Lucchesi LR, Bisignano C, Castle CD, Dingels ZV, Fox JT, et al.
The Global Burden of Falls: Global, Regional and National Estimates
of Morbidity and Mortality From the Global Burden of Disease Study 2017
Injury Prevention 2020 (Oct); 26 (Supp 1): i3-i11Drake SA, Conway SH, Yang Y, Cheatham LS, Wolf DA, Adams SD, et al.
When falls become fatal-clinical care sequence.
Plos One. 2021;16(1):e0244862.Persons AGSPoPMoPPiO.
Pharmacological management of persistent pain in older persons.
J Am Geriatr Soc. 2009;57(8):1331–46.Hedegaard H, Miniño AM, Warner M.
Drug overdose deaths in the United States, 1999–2018.
NCHS Data Brief, no 356.
Hyattsville, MD: National Center for Health Statistics; 2020.Delbaere K, Crombez G, Vanderstraeten G, Willems T, Cambier D.
Fear-related avoidance of activities, falls and physical frailty.
A prospective community-based cohort study.
Age Ageing. 2004;33(4):368–73.Liu M, Hou T, Li Y, Sun X, Szanton SL, Clemson L, et al.
Fear of falling is as important as multiple previous falls in terms
of limiting daily activities: a longitudinal study.
BMC Geriatr. 2021;21(1):350.Zijlstra GA, van Haastregt JC, van Eijk JT, van Rossum E, Stalenhoef PA, Kempen GI.
Prevalence and correlates of fear of falling, and associated avoidance
of activity in the general population of community-living older people.
Age Ageing. 2007;36(3):304–9.Montero-Odasso M, van der Velde N, Alexander NB, Becker C, et al.
New horizons in falls prevention and management for older adults:
a global initiative.
Age Ageing. 2021;50(5):1499–507.Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C.
Medical costs of fatal and nonfatal falls in older adults.
J Am Geriatr Soc. 2018;66(4):693–8.Burns ER, Stevens JA, Lee R.
The direct costs of fatal and non-fatal falls
among older adults - United States.
J Saf Res. 2016;58:99–103.Centers for Disease Control and Prevention NCfIPaC.
STEADI—Older Adult Fall Prevention 2020 updated 08.12.2020. Available from:
https://www.cdc.gov/steadi/materials.htmlCheung CK, Wyman JF, Halcon LL.
Use of complementary and alternative therapies in community-dwelling older adults.
J Altern Complement Med. 2007;13(9):997–1006.Caron A, Gallo WT, Durbin LL, Mielenz TJ.
Relationship between falls and complementary and alternative medicine use
among community-dwelling older adults.
J Altern Complement Med. 2017;23(1):41–4.Tindle HA, Davis RB, Phillips RS, Eisenberg DM.
Trends in use of complementary and alternative medicine by US adults: 1997-2002.
Altern Ther Health Med. 2005;11(1):42–9.Mullner RM.
Encyclopedia of health services research.
Thousand Oaks: SAGE Publications; 2009. p. 166.Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, Kessler RC.
Trends in Alternative Medicine Use in the United States, 1990 to 1997:
Results of a Follow-up National Survey
JAMA 1998 (Nov 11); 280 (18): 1569–1575Himelfarb I, Hyland JK, Ouzts NE, Russel M, Sterling T, Johnson C, et al.
Practice Analysis of Chiropractic 2020
a project report, survey analysis, and summary of the practice
of chiropractic within the United States.
Greeley: National Board of Chiropractic Examiners; 2020.Chapman-Smith D.
In the chiropractic profession:
its education, practice, research and future directions.;
2001. Report No.: 6.Vining R, Mathers S.
Chiropractic medicine for the treatment of pain in the rehabilitation patient.
Comprehensive pain Management in the Rehabilitation Patient.
Cham: Springer; 2017. p. 575–3.Maiers M, Agaoglu M, Brown R, Cassirer C, DaSilva K, Lystad RP, et al.
Chiropractic in global health and wellbeing: a white paper
describing the public health agenda of the World Federation of Chiropractic.
Chiropr Man Therap. 2018;26:26.Vining RD, Shannon ZK, Salsbury SA, Corber L, Minkalis AL, Goertz CM.
Development of a Clinical Decision Aid for Chiropractic Management
of Common Conditions Causing Low Back Pain in Veterans:
Results of a Consensus Process
J Manipulative Physiol Ther. 2019 (Nov); 42 (9): 677–693Ambrose AF, Paul G, Hausdorff JM.
Risk factors for falls among older adults:
a review of the literature.
Maturitas. 2013;75(1):51–61.Shumway-Cook A, Woollacott MH.
Motor control: translating research into clinical practice.
Alphen aan den Rijn: Wolters Kluwer; 2017.Hopewell S, Adedire O, Copsey BJ, Boniface GJ, Sherrington C, Clemson L, et al.
Multifactorial and multiple component interventions for preventing falls
in older people living in the community.
Cochrane Database Syst Rev. 2018;7:CD012221.Tricco AC, Thomas SM, Veroniki AA, Hamid JS, Cogo E, Strifler L, et al.
Comparisons of interventions for preventing falls in older adults:
a systematic review and Meta-analysis.
JAMA. 2017;318(17):1687–99.Dougherty P.E., Hawk C., Weiner D.K., Gleberzon B., Andrew K., Killinger L.
The Role of Chiropractic Care in Older Adults
Chiropractic & Manual Therapies 2012 (Feb 21); 20 (1): 3Holt KR, Noone PL, Short K, Elley CR, Haavik H.
Fall risk profile and quality-of-life status of older chiropractic patients.
J Manip Physiol Ther. 2011;34(2):78–87.Horlings CG, van Engelen BG, Allum JH, Bloem BR.
A weak balance: the contribution of muscle weakness to postural instability and falls.
Nat Clin Pract Neurol. 2008;4(9):504–15.Woollacott M, Shumway-Cook A.
Attention and the control of posture and gait:
a review of an emerging area of research.
Gait Posture. 2002;16(1):1–14.Moreland JD, Richardson JA, Goldsmith CH, Clase CM.
Muscle weakness and falls in older adults:
a systematic review and meta-analysis.
J Am Geriatr Soc. 2004;52(7):1121–9.Mickle KJ, Munro BJ, Lord SR, Menz HB, Steele JR.
ISB clinical biomechanics award 2009: toe weakness and deformity
increase the risk of falls in older people.
Clin Biomech (Bristol, Avon). 2009;24(10):787–91.Bobowik P, Wiszomirska I.
Diagnostic dependence of muscle strength measurements
and the risk of falls in the elderly.
Int J Rehabil Res. 2020;43(4):330–6.Gafner SC, Bastiaenen CH, Ferrari S, Gold G, Terrier P, Hilfiker R, et al.
Hip muscle and hand-grip strength to differentiate between older
fallers and non-fallers: a cross-sectional validity study.
Clin Interv Aging. 2018;13:1–8.Granacher U, Gollhofer A, Hortobágyi T, Kressig RW, Muehlbauer T.
The importance of trunk muscle strength for balance, functional performance,
and fall prevention in seniors: a systematic review.
Sports Med. 2013;43(7):627–41.Pavol MJ, Owings TM, Foley KT, Grabiner MD.
Influence of lower extremity strength of healthy older adults
on the outcome of an induced trip.
J Am Geriatr Soc. 2002;50(2):256–62.Ding L, Yang F.
Muscle weakness is related to slip-initiated falls
among community-dwelling older adults.
J Biomech. 2016;49(2):238–43.Giacalone A, Febbi M, Magnifica F, Ruberti E.
The effect of high velocity low amplitude cervical manipulations
on the musculoskeletal system: literature review.
Cureus. 2020;12(4):e7682.Galindez-Ibarbengoetxea X, Setuain I, Andersen LL, Ramírez-Velez R, et al.
Effects of cervical high-velocity low-amplitude techniques on
range of motion, strength performance, and cardiovascular outcomes:
a review.
J Altern Complement Med. 2017;23(9):667–75.Vining R, Long CR, Minkalis A, Gudavalli MR, Xia T, Walter J, et al.
Effects of Chiropractic Care on Strength, Balance, and Endurance
in Active-Duty U.S. Military Personnel with Low Back Pain:
A Randomized Controlled Trial
J Altern Complement Med 2020 (Jul); 26 (7): 592–601–693Bronfort G, Evans R, Nelson B, Aker PD, Goldsmith CH, Vernon HT.
A Randomized Clinical Trial of Exercise and Spinal Manipulation
for Patients with Chronic Neck Pain
Spine (Phila Pa 1976) 2001 (Apr 1); 26 (7): 788–797Schulz C, Evans R, Maiers M, Schulz K, Leininger B, Bronfort G (2019)
Spinal Manipulative Therapy and Exercise for Older Adults
with Chronic Low Back Pain: A Randomized Clinical Trial
Chiropractic & Manual Therapies 2019 (May 15); 27: 21Christiansen T.L., Niazi I.K., Holt K., Nedergaard R.W., Duehr J., Allen K., et. al.
The effects of a single session of spinal manipulation on
strength and cortical drive in athletes .
Eur. J. Appl. Physiol. 2018; 118: 737–749Grindstaff TL, Hertel J, Beazell JR, Magrum EM, Ingersoll CD.
Effects of lumbopelvic joint manipulation on quadriceps activation
and strength in healthy individuals.
Man Ther. 2009;14(4):415–20.Hillermann B, Gomes AN, Korporaal C, Jackson D.
A pilot study comparing the effects of spinal manipulative therapy
with those of extra-spinal manipulative therapy on quadriceps muscle strength.
J Manip Physiol Ther. 2006;29(2):145–9.Ghasemi C, Amiri A, Sarrafzadeh J, Jafari H, Dadgoo M.
The effect of soft tissue manipulation and rest on knee extensor
muscles fatigue: do torque parameters and induced perception
following muscle fatigue have enough reliability?
J Family Med Prim Care. 2020;9(2):950–6.Ozsoy G, Ilcin N, Ozsoy I, Gurpinar B, Buyukturan O, Buyukturan B, et al.
The effects of myofascial release technique combined with Core stabilization
exercise in elderly with non-specific low Back pain:
a randomized controlled Single-Blind Study
Clin Interv Aging. 2019;14:1729–40.Sherrington C, Fairhall NJ, Wallbank GK, Howard K, et al.
Exercise for preventing falls in older people living in the community.
Cochrane Database Syst Rev. 2019;1:CD012424.Gong W.
Impact of longus colli muscle massage on the strength
and endurance of the deep neck flexor muscle of adults.
J Phys Ther Sci. 2013;25(5):591–3.Kalichman L, Ben DC.
Effect of self-myofascial release on myofascial pain,
muscle flexibility, and strength: a narrative review.
J Bodyw Mov Ther. 2017;21(2):446–51.Menz HB, Auhl M, Spink MJ.
Foot problems as a risk factor for falls in community-dwelling
older people: a systematic review and meta-analysis.
Maturitas. 2018;118:7–14.Menz HB, Morris ME, Lord SR.
Foot and ankle risk factors for falls in older people:
a prospective study.
J Gerontol A Biol Sci Med Sci. 2006;61(8):866–70.da Silva RB, Costa-Paiva L, Morais SS, Mezzalira R, Ferreira Nde O, Pinto-Neto AM.
Predictors of falls in women with and without osteoporosis.
J Orthop Sports Phys Ther. 2010;40(9):582–8.Demarteau J, Jansen B, Van Keymolen B, Mets T, Bautmans I.
Trunk inclination and hip extension mobility, but not thoracic
kyphosis angle, are related to 3D-accelerometry based
gait alterations and increased fall-risk in older persons.
Gait Posture. 2019;72:89–95.Shishov N, Gimmon Y, Rashed H, Kurz I, Riemer R, Shapiro A, et al.
Old adult fallers display reduced flexibility of arm and trunk
movements when challenged with different walking speeds.
Gait Posture. 2017;52:280–6.Maxwell CM, Lauchlan DT, Dall PM.
The effects of spinal manipulative therapy on lower limb
neurodynamic test outcomes in adults: a systematic review.
J Man Manip Ther. 2020;28(1):4–14.Kendall JC, French SD, Hartvigsen J, Azari MF.
Chiropractic Treatment Including Instrument-assisted Manipulation
for Non-specific Dizziness and Neck Pain in Community-dwelling
Older People: A Feasibility Randomised Sham-controlled Trial
Chiropractic & Manual Therapies 2018 (May 10); 26: 14Cheatham SW, Lee M, Cain M, Baker R.
The efficacy of instrument assisted soft tissue mobilization:
a systematic review.
J Can Chiropr Assoc. 2016;60(3):200–11.Sharman MJ, Cresswell AG, Riek S.
Proprioceptive neuromuscular facilitation stretching:
mechanisms and clinical implications.
Sports Med. 2006;36(11):929–39.Manheim CJ, Lavett DK.
The myofascial release manual. 4th ed.
Thorofare. Thorofare: SLACK Inc; 2020.Greenman PE.
Principles of manual medicine. 2nd ed.
Baltimore: Lippincott Williams & Wilkins; 1996.Kim J, Sung DJ, Lee J.
Therapeutic effectiveness of instrument-assisted soft tissue
mobilization for soft tissue injury: mechanisms and
practical application.
J Exerc Rehabil. 2017;13(1):12–22.Seffrin CB, Cattano NM, Reed MA, Gardiner-Shires AM.
Instrument-assisted soft tissue mobilization:
a systematic review and effect-size analysis.
J Athl Train. 2019;54(7):808–21.McAtee RE.
Facilitated stretching.
Champaign: Human Kinetics Publishers; 1993.Gunn LJ, Stewart JC, Morgan B, Metts ST, Magnuson JM, Iglowski NJ, et al.
Instrument-assisted soft tissue mobilization and proprioceptive
neuromuscular facilitation techniques improve hamstring
flexibility better than static stretching alone:
a randomized clinical trial.
J Man Manip Ther. 2019;27(1):15–23.Chen Z, Wu J, Wang X, Ren Z.
The effects of myofascial release technique for patients with
low back pain: a systematic review and meta-analysis.
Complement Ther Med. 2021;59:102737.Stanek J, Sullivan T, Davis S.
Comparison of compressive myofascial release and the
Graston technique for improving ankle-dorsiflexion
range of motion.
J Athl Train. 2018;53(2):160–7.Cai Y, Leveille SG, Shi L, Chen P, You T.
Chronic pain and risk of injurious falls in
community-dwelling older adults.
J Gerontol A Biol Sci Med Sci. 2020;76:179–86.Ogawa EF, Shi L, Bean JF, Hausdorff JM, Dong Z, Manor B, et al.
Chronic pain characteristics and gait in older adults:
the MOBILIZE Boston study II.
Arch Phys Med Rehabil. 2020;101(3):418–25.Leveille SG, Jones RN, Kiely DK, Hausdorff JM, Shmerling RH, et al.
Chronic musculoskeletal pain and the occurrence of falls
in an older population.
JAMA. 2009;302(20):2214–21.Poole E, Treleaven J, Jull G.
The influence of neck pain on balance and gait parameters
in community-dwelling elders.
Man Ther. 2008;13(4):317–24.Blyth FM, Noguchi N.
Chronic musculoskeletal pain and its impact on older people.
Best Pract Res Clin Rheumatol. 2017;31(2):160–8.Schwan J, Sclafani J, Tawfik VL.
Chronic pain Management in the Elderly.
Anesthesiol Clin. 2019;37(3):547–60.Leveille SG, Bean J, Bandeen-Roche K, Jones R, Hochberg M, Guralnik JM.
Musculoskeletal pain and risk for falls in older disabled
women living in the community.
J Am Geriatr Soc. 2002;50(4):671–8.Graven-Nielsen T, Lund H, Arendt-Nielsen L, Danneskiold-Samsøe B, Bliddal H.
Inhibition of maximal voluntary contraction force by
experimental muscle pain: a centrally mediated mechanism.
Muscle Nerve. 2002;26(5):708–12.Coulter ID, Crawford C, Hurwitz EL, Vernon H, Khorsan R, et al.
Manipulation and Mobilization for Treating Chronic Low Back Pain:
A Systematic Review and Meta-analysis
Spine J. 2018 (May); 18 (5): 866–879Walker BF, French SD, Grant W, Green S.
Combined chiropractic interventions for low-back pain.
Cochrane Database Syst Rev. 2010;(4):CD005427.
https://doi.org/10.1002/14651858.CD005427.pub2Chou R, Wagner J, Ahmed AY, Blazina I, Brodt E, Buckley DI, et al.
Treatments for Acute Pain: A Systematic Review
Comparative Effectiveness Review, No. 240
Rockville (MD): Agency for Healthcare Research and Quality (US);
2020 Dec. Report No.: 20(21)-EHC006Coulter ID, Crawford C, Vernon H, Hurwitz EL, Khorsan R, Booth MS, et al.
Manipulation and Mobilization for Treating Chronic
Nonspecific Neck Pain: A Systematic Review and
Meta-Analysis for an Appropriateness Panel
Pain Physician. 2019 (Mar); 22 (2): E55–E70Gross A, Langevin P, Burnie SJ, Bedard-Brochu MS, Empey B, Dugas E, et al.
Manipulation and mobilisation for neck pain contrasted against
an inactive control or another active treatment.
Cochrane Database Syst Rev. 2015(9):Cd004249.
https://doi.org/10.1002/14651858.CD004249.pub4Paige NM, Miake-Lye IM, Booth MS, Beroes JM, Mardian AS, Dougherty P, et al.
Association of Spinal Manipulative Therapy With Clinical
Benefit and Harm for Acute Low Back Pain:
Systematic Review and Meta-analysis
JAMA. 2017 (Apr 11); 317 (14): 1451–1460Rubinstein SM, De Zoete A, Van Middelkoop M, Assendelft WJJ, De Boer MR, Van Tulder MW.
Benefits and Harms of Spinal Manipulative Therapy for the Treatment
of Chronic Low Back Pain: Systematic Review and Meta-analysis
of Randomised Controlled Trials
British Medical Journal 2019 (Mar 13); 364: l689Skelly AC, Chou R, Dettori JR, Turner JA, Friedly JL, et al.
Noninvasive Nonpharmacological Treatment for Chronic Pain:
A Systematic Review Update
Comparative Effectiveness Review Number 227
Rockville (MD): Agency for Healthcare Research and Quality (2020)Piper S, Shearer HM, Côté P, Wong JJ, Yu H, Varatharajan S, et al.
The effectiveness of soft-tissue therapy for the management of
musculoskeletal disorders and injuries of the upper and
lower extremities: a systematic review by the Ontario
protocol for traffic injury management (OPTIMa) collaboration.
Man Ther. 2016;21:18–34.Ge W, Roth E, Sansone A.
A quasi-experimental study on the effects of instrument assisted
soft tissue mobilization on mechanosensitive neurons.
J Phys Ther Sci. 2017;29(4):654–7.Kim YK, Cho SY, Lee KH.
Effects of transcutaneous electrical nerve stimulation and
instrument-assisted soft tissue mobilization combined
treatment on chronic low back pain:
a randomized controlled trial.
J Back Musculoskelet Rehabil. 2021;34:895–902.Areeudomwong P, Buttagat V.
Proprioceptive neuromuscular facilitation training improves
pain-related and balance outcomes in working-age patients
with chronic low back pain: a randomized controlled trial.
Braz J Phys Ther. 2019;23(5):428–36.Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH.
Physical activity and exercise for chronic pain in adults:
an overview of cochrane reviews.
Cochrane Database Syst Rev. 2017;4:CD011279.Wewege MA, Booth J, Parmenter BJ,
Aerobic vs. Resistance exercise for chronic non-specific
low back pain: a systematic review and meta-analysis.
J Back Musculoskelet Rehabil. 2018;31(5):889–99.Wieland LS, Skoetz N, Pilkington K, Vempati R, D'Adamo CR, Berman BM.
Yoga treatment for chronic non-specific low back pain.
Cochrane Database Syst Rev. 2017;1:CD010671.Qin J, Zhang Y, Wu L, He Z, Huang J, Tao J, et al.
Effect of Tai chi alone or as additional therapy on low back
pain: systematic review and meta-analysis of
randomized controlled trials.
Medicine (Baltimore). 2019;98(37):e17099.Coutaux A.
Non-pharmacological treatments for pain relief:
TENS and acupuncture.
Joint Bone Spine. 2017;84(6):657–61.French SD, Cameron M, Walker BF, Reggars JW, Esterman AJ.
Superficial heat or cold for low back pain.
Cochrane Database Syst Rev. 2006;(1):CD004750.
https://doi.org/10.1002/14651858.CD004750.pub2Maravita A, Spence C, Driver J.
Multisensory integration and the body schema:
close to hand and within reach.
Curr Biol. 2003;13:R531–R9.Han J, Anson J, Waddington G, Adams R, Liu Y.
The role of ankle proprioception for balance control
in relation to sports performance and injury.
Biomed Res Int. 2015;2015:842804.MacKinnon CD.
Sensorimotor anatomy of gait, balance, and falls.
Handb Clin Neurol. 2018;159:3–26.Henry M, Baudry S.
Age-related changes in leg proprioception:
implications for postural control.
J Neurophysiol. 2019;122(2):525–38.Nakasa T, Fukuhara K, Adachi N, Ochi M.
The deficit of joint position sense in the chronic unstable ankle
as measured by inversion angle replication error.
Arch Orthop Trauma Surg. 2008;128(5):445–9.Theisen A, Day J.
Chronic ankle instability leads to lower extremity
kinematic changes during landing tasks: a systematic review.
Int J Exerc Sci. 2019;12(1):24–33.Lephart SM, Fu FH.
Proprioception and neuromuscular control in joint stability.
Champaign: Human Kinetics; 2000.Pizzigalli L, Filippini A, Ahmaidi S, Jullien H, Rainoldi A.
Prevention of falling risk in elderly people: the relevance of
muscular strength and symmetry of lower limbs
in postural stability.
J Strength Cond Res. 2011;25(2):567–74.Manor B, Lipsitz LA, Wayne PM, Peng CK, Li L.
Complexity-based measures inform Tai Chi’s impact on standing
postural control in older adults with peripheral neuropathy.
BMC Complement Altern Med. 2013;13:87.Viseux FJF.
The sensory role of the sole of the foot:
review and update on clinical perspectives.
Neurophysiol Clin. 2020;50(1):55–68.Frost LR, Bijman M, Strzalkowski ND, Bent LR, Brown SH.
Deficits in foot skin sensation are related to alterations in
balance control in chronic low back patients experiencing
clinical signs of lumbar nerve root impingement.
Gait Posture. 2015;41(4):923–8.Macgilchrist C, Paul L, Ellis BM, Howe TE, Kennon B, Godwin J.
Lower-limb risk factors for falls in people with diabetes mellitus.
Diabet Med. 2010;27(2):162–8.Herzog W:
The Biomechanics of Spinal Manipulation
J Bodyw Mov Ther. 2010 (Jul); 14 (3): 280–286Haavik, H and Murphy, B.
Subclinical Neck Pain and the Effects of Cervical
Manipulation on Elbow Joint Position Sense
J Manipulative Physiol Ther. 2011 (Feb); 34 (2): 88–97Holt, KR, Haavik, H, Lee, ACL, Murphy, B, and Elley, CR.
Effectiveness of Chiropractic Care to Improve Sensorimotor Function
Associated With Falls Risk in Older People:
A Randomized Controlled Trial
J Manipulative Physiol Ther. 2016 (May); (39) 4: 267–278Naderi A, Aminian-Far A, Gholami F, Mousavi SH, Saghari M, Howatson G.
Massage enhances recovery following exercise-induced
muscle damage in older adults.
Scand J Med Sci Sports. 2021;31(3):623–32.Collins KA, Turner MJ, Hubbard-Turner T, Thomas AC.
Gait and plantar sensation changes following massage and
textured insole application in patients after
anterior cruciate ligament reconstruction.
Gait Posture. 2020;81:254–60.Gutknecht M, Mannig A, Waldvogel A, Wand BM, Luomajoki H.
The effect of motor control and tactile acuity training on
patients with non-specific low back pain and
movement control impairment.
J Bodyw Mov Ther. 2015;19(4):722–31.van Baal K, Allofs J, Ehrenbrusthoff K, Grüneberg C, Hering T, Kopkow C, et al.
Effects of a movement control and tactile acuity training in
patients with nonspecific chronic low back pain and control
impairment - a randomised controlled pilot study.
BMC Musculoskelet Disord. 2020;21(1):794.Korchi K, Noé F, Bru N, Paillard T.
Optimization of the effects of physical activity on
plantar sensation and postural control with barefoot
exercises in institutionalized older adults: a pilot study.
J Aging Phys Act. 2019;27(4):452–65.Abbasi S, Hadian Rasanani MR, Ghotbi N, Olyaei GR, Bozorgmehr A, Rasouli O.
Short-term effect of kinesiology taping on pain, functional
disability and lumbar proprioception in individuals with
nonspecific chronic low back pain:
a double-blinded, randomized trial.
Chiropr Man Therap. 2020;28(1):63.Khan S, Chang R.
Anatomy of the vestibular system: a review.
NeuroRehabilitation. 2013;32(3):437–43.Coto J, Alvarez CL, Cejas I, Colbert BM, Levin BE, Huppert J, et al.
Peripheral vestibular system: age-related vestibular loss
and associated deficits.
J Otol. 2021;16(4):258–65.Herdman SJ, Blatt P, Schubert MC, Tusa RJ.
Falls in patients with vestibular deficits.
Am J Otol. 2000;21(6):847–51.Agrawal Y, Carey JP, Della Santina CC, Schubert MC, Minor LB.
Disorders of balance and vestibular function in US adults:
data from the National Health and nutrition
examination survey, 2001-2004.
Arch Intern Med. 2009;169(10):938–44.Lystad RP, Bell G, Bonnevie-Svendsen M, Carter CV.
Manual Therapy With and Without Vestibular Rehabilitation
for Cervicogenic Dizziness: A Systematic Review
Chiropractic & Manual Therapies 2011 (Sep 18); 19: 21Reid S, Rivett D.
Manual Therapy Treatment of Cervicogenic Dizziness:
A Systematic Review
Man Ther. 2005 (Feb); 10 (1): 4–13McDonnell MN, Hillier SL.
Vestibular rehabilitation for unilateral peripheral vestibular dysfunction.
Cochrane Database Syst Rev. 2015;1:Cd005397.Foster CA, Ponnapan A, Zaccaro K, Strong D.
A comparison of two home exercises for benign positional
vertigo: half somersault versus Epley maneuver.
Audiol Neurotol Extra. 2012;2(1):16–23.Nørregaard AR, Lauridsen HH, Hartvigsen J.
Chiropractic management of a patient with benign
paroxysmal positional vertigo: a case report.
J Manip Physiol Ther. 2009;32(5):387–90.Sajko SS, Stuber K, Welsh TN.
Chiropractic Management of Benign Paroxysmal Positional Vertigo
Using the Epley Maneuver: A Case Series
J Manipulative Physiol Ther. 2013 (Feb); 36 (2): 119–126Wayne PM, Krebs DE, Wolf SL, Gill-Body KM, Scarborough DM, McGibbon CA, et al.
Can Tai chi improve vestibulopathic postural control?
Arch Phys Med Rehabil. 2004;85(1):142–52.McGibbon CA, Krebs DE, Parker SW, Scarborough DM, Wayne PM, Wolf SL.
Tai chi and vestibular rehabilitation improve vestibulopathic
gait via different neuromuscular mechanisms: preliminary report.
BMC Neurol. 2005;5(1):3.Richardson K, Bennett K, Kenny RA.
Polypharmacy including falls risk-increasing medications and subsequent
falls in community-dwelling middle-aged and older adults.
Age Ageing. 2015;44(1):90–6.Maher RL, Hanlon J, Hajjar ER.
Clinical consequences of polypharmacy in elderly.
Expert Opin Drug Saf. 2014;13(1):57–65.Halli-Tierney AD, Scarbrough C, Carroll D.
Polypharmacy: evaluating risks and deprescribing.
Am Fam Physician. 2019;100(1):32–8.Dhalwani NN, Fahami R, Sathanapally H, Seidu S, Davies MJ, Khunti K.
Association between polypharmacy and falls in older adults:
a longitudinal study from England.
BMJ Open. 2017;7(10):e016358.Morin L, Calderon Larrañaga A, Welmer AK, Rizzuto D, Wastesson JW, Johnell K.
Polypharmacy and injurious falls in older adults:
a nationwide nested case-control study.
Clin Epidemiol. 2019;11:483–93.Montero-Odasso M, Sarquis-Adamson Y, Song HY, Bray N.
Polypharmacy, gait performance, and falls in community-dwelling
older adults. Results from the gait and brain study.
J Am Geriatr Soc. 2019;67(6):1182–8.Davies LE, Spiers G, Kingston A, Todd A, Adamson J, Hanratty B.
Adverse outcomes of polypharmacy in older people:
systematic review of reviews.
J Am Med Dir Assoc. 2020;21(2):181–7.Els C, Jackson TD, Kunyk D, Lappi VG, Sonnenberg B, Hagtvedt R, et al.
Adverse events associated with medium- and long-term use of
opioids for chronic non-cancer pain: an overview
of cochrane reviews.
Cochrane Database Syst Rev. 2017;10:CD012509.Whedon JM, Toler AWJ, Kazal LA, Bezdjian S, Goehl JM, Greenstein J.
Impact of Chiropractic Care on Use of Prescription
Opioids in Patients with Spinal Pain
Pain Medicine 2020 (Dec 25); 21 (12): 3567–3573
There are more like this at: SPINAL PAIN MANAGEMENTLisi AJ, Salsbury SA, Twist EJ, Goertz CM.
Chiropractic Integration into Private Sector Medical Facilities:
A Multisite Qualitative Case Study
J Altern Complement Med. 2018 (Aug); 24 (8): 792–800Lisi AJ, Corcoran KL, DeRycke EC, et al.
Opioid Use Among Veterans of Recent Wars Receiving
Veterans Affairs Chiropractic Care
Pain Medicine 2018 (Sep 1); 19 (suppl 1): S54–S60Kazis LE, Ameli O, Rothendler J, et al.
Observational Retrospective Study of the Association of Initial
Healthcare Provider for New-onset Low Back Pain
with Early and Long-term Opioid Use
BMJ Open. 2019 (Sep 20); 9 (9): e028633
There are more like this at: INITIAL PROVIDERCorcoran KL, Bastian LA, Gunderson CG, et al.
Association Between Chiropractic Use and Opioid Receipt
Among Patients with Spinal Pain: A Systematic Review
and Meta-analysis
Pain Medicine 2020 (Feb 1); 21 (2): e139–e145
There are more like this at: NON-PHARMACOLOGIC THERAPYEvans R, Haas M, Schulz C, Leininger B, Hanson L, Bronfort G.
Spinal Manipulation and Exercise for Low Back Pain
in Adolescents: A Randomized Trial
Pain. 2018 (Jul); 159 (7): 1297–1307Evans R, Bronfort G, Nelson B, Goldsmith CH.
Two-year Follow-up of a Randomized Clinical Trial of
Spinal Manipulation and Two Types of Exercise
Patients With Chronic Neck Pain
Spine (Phila Pa 1976). 2002 (Nov 1); 27 (21): 2383–2389Bronfort G, Maiers MJ, Evans RL, Schulz CA, Bracha Y, Svendsen KH, et al.
Supervised Exercise, Spinal Manipulation, and Home Exercise
for Chronic Low Back Pain: A Randomized Clinical Trial
Spine J. 2011 (Jul); 11 (7): 585–598Lee HC, Chang KC, Tsauo JY, Hung JW, Huang YC, Lin SI, et al.
Effects of a multifactorial fall prevention program on fall incidence
and physical function in community-dwelling older adults with risk of falls.
Arch Phys Med Rehabil. 2013;94(4):606–15, 15.e1.Opsahl AG, Ebright P, Cangany M, Lowder M, Scott D, Shaner T.
Outcomes of adding patient and family engagement education
to fall prevention bundled interventions.
J Nurs Care Qual. 2017;32(3):252–8.Heng H, Jazayeri D, Shaw L, Kiegaldie D, Hill AM, Morris ME.
Hospital falls prevention with patient education: a scoping review.
BMC Geriatr. 2020;20(1):140.W A-F.
World health organization global report on falls prevention in older age. 2007. Available from:
http://www.who.int/ageing/publications/Falls_prevention7March.pdfBauman CA, Milligan JD, Patel T, Pritchard S, Labreche T, et al.
Community-based falls prevention:
lessons from an Interprofessional mobility clinic.
J Can Chiropr Assoc. 2014;58(3):300–11.Hausdorff JM, Rios DA, Edelberg HK.
Gait variability and fall risk in community-living older adults:
a 1-year prospective study.
Arch Phys Med Rehabil. 2001;82(8):1050–6.Hausdorff JM.
Gait dynamics, fractals and falls: finding meaning in the
stride-to-stride fluctuations of human walking.
Hum Mov Sci. 2007;26(4):555–89.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al.
The PRISMA 2020 statement: an updated guideline for reporting systematic reviews.
BMJ. 2021;372:n71.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al.
The Cochrane Collaboration’s tool for assessing risk
of bias in randomised trials.
BMJ. 2011;343:d5928.Hawk C, Pfefer M, Strunk R, Ramcharan M, Uhl N.
Feasibility Study of Short-term Effects of Chiropractic
Manipulation on Older Adults With Impaired Balance
J Chiropractic Medicine 2007 (Dec); 6 (4): 121–131Hawk C, Cambron JA, Pfefer MT.
Pilot Study of the Effect of a Limited and Extended Course of
Chiropractic Care on Balance, Chronic Pain, and Dizziness
in Older Adults
J Manipulative Physiol Ther. 2009 (Jul); 32(6): 438–447Herzog W, Conway PJ, Willcox BJ.
Effects of different treatment modalities on gait symmetry
and clinical measures for sacroiliac joint patients.
J Manip Physiol Ther. 1991;14(2):104–9.Maiers M, Bronfort G, Evans R, Hartvigsen J, Svendsen K, Bracha Y, et al.
Spinal Manipulative Therapy and Exercise For Seniors
with Chronic Neck Pain
Spine J. 2014 (Sep 1); 14 (9): 1879–1889Ward JS, Coats J, Sorrels K, Walters M, Williams T.
Pilot study of the impact sacroiliac joint manipulation has
on walking kinematics using motion analysis technology.
J Chiropr Med. 2013;12(3):143–52.Ward J, Sorrels K, Coats J, Pourmoghaddam A, Deleon C, Daigneault P.
Pilot study of the impact that bilateral sacroiliac joint manipulation
using a drop table technique has on gait parameters in asymptomatic
individuals with a leg length inequality.
J Can Chiropr Assoc. 2014;58(1):85–95.Bracher ES, Almeida CI, Almeida RR, Duprat AC, Bracher CB.
A Combined Approach for the Treatment of Cervical Vertigo
J Manipulative Physiol Ther. 2000 (Feb); 23 (2): 96–100Hawk C, Cambron J.
Chiropractic Care for Older Adults: Effects on Balance,
Dizziness, and Chronic Pain
J Manipulative Physiol Ther. 2009 (Jul); 32 (6): 431–437Strunk R, Hawk C.
Effects of Chiropractic Care on Dizziness, Neck Pain, and Balance:
A Single-group, Preexperimental, Feasibility Study
J Chiropractic Medicine 2009 (Dec); 8 (4): 156–164Herzog W, Nigg BM, Read LJ.
Quantifying the effects of spinal manipulations on gait
using patients with low back pain.
J Manip Physiol Ther. 1988;11(3):151–7.Herzog W, Read LJ, Conway PJ, Shaw LD, McEwen MC.
Reliability of motion palpation procedures to
detect sacroiliac joint fixations.
J Manip Physiol Ther. 1989;12(2):86–92.Robinson RO, Herzog W, Nigg BM.
Use of force platform variables to quantify the effects
of chiropractic manipulation on gait symmetry.
J Manip Physiol Ther. 1987;10(4):172–6.Palmgren PJ, Lindeberg A, Nath S, Heikkilä H.
Head repositioning accuracy and posturography related to cervical
facet nerve blockade and spinal manipulative therapy in healthy volunteers:
a time series study.
J Manip Physiol Ther. 2009;32(3):193–202.Malaya CA, Haworth J, Pohlman KA, Powell C, Smith DL.
Impact of extremity manipulation on postural sway characteristics:
a preliminary, randomized crossover study.
J Manip Physiol Ther. 2020;43(5):457–68.Malaya CA, Haworth J, Pohlman KA, Smith DL.
Immediate Impact of Extremity Manipulation on Dual Task
Performance: A Randomized,Crossover Clinical Trial
Chiropractic & Manual Therapies 2021 (Feb 5); 29: 6Osterbauer PJ, De Boer KF, Widmaier R, Petermann E, Fuhr AW.
Treatment and biomechanical assessment of patients with
chronic sacroiliac joint syndrome.
J Manip Physiol Ther. 1993;16(2):82–90.Maiers M, Hartvigsen J, Evans R, Westrom K, Wang Q, Schulz C, et al.
Short or Long-term Treatment of Spinal Disability
in Older Adults with Manipulation and Exercise
Arthritis Care Res (Hoboken) 2019 (Nov); 71 (11): 1516–1524Althubaiti A.
Information bias in health research: definition, pitfalls, and adjustment methods.
J Multidiscip Healthc. 2016;9:211–7.Fairhall N, Sherrington C, Lord SR, Kurrle SE, Langron C, Lockwood K, et al.
Effect of a multifactorial, interdisciplinary intervention on
risk factors for falls and fall rate in frail older people:
a randomised controlled trial.
Age Ageing. 2014;43(5):616–22.Ferrer A, Formiga F, Sanz H, de Vries OJ, Badia T, Pujol R, et al.
Multifactorial assessment and targeted intervention to reduce
falls among the oldest-old: a randomized controlled trial.
Clin Interv Aging. 2014;9:383–93.Sosnoff JJ, Moon Y, Wajda DA, Finlayson ML, et al.
Fall risk and incidence reduction in high risk individuals
with multiple sclerosis: a pilot randomized control trial.
Clin Rehabil. 2015;29(10):952–60.Uusi-Rasi K, Patil R, Karinkanta S, Kannus P, Tokola K, et al.
Exercise and vitamin D in fall prevention among older women:
a randomized clinical trial.
JAMA Intern Med. 2015;175(5):703–11.Ueda T, Higuchi Y, Imaoka M, Todo E, Kitagawa T, Ando S.
Tailored education program using home floor plans for falls prevention
in discharged older patients: a pilot randomized controlled trial.
Arch Gerontol Geriatr. 2017;71:9–13.Kim SB, Zingmond DS, Keeler EB, Jennings LA, Wenger NS, Reuben DB, et al.
Development of an algorithm to identify fall-related injuries
and costs in Medicare data.
Inj Epidemiol. 2016;3(1):1.Usmani S, Saboor A, Haris M, Khan MA, Park H.
Latest research trends in fall detection and prevention
using machine learning: a systematic review.
Sensors (Basel). 2021;21(15):1–23.Yang R, Plasek JM, Cummins MR, Sward KA.
Predicting falls among community-dwelling older adults:
a demonstration of applied machine learning.
Comput Inform Nurs. 2021;39(5):273–80.Pang I, Okubo Y, Sturnieks D, Lord SR, Brodie MA.
Detection of near falls using wearable devices: a systematic review.
J Geriatr Phys Ther. 2019;42(1):48–56.Baig MM, GholamHosseini H, Moqeem AA, Mirza F, Lindén M.
A systematic review of wearable patient monitoring systems -
current challenges and opportunities for clinical adoption.
J Med Syst. 2017;41(7):115.Lima CA, Ricci NA, Nogueira EC, Perracini MR.
The berg balance scale as a clinical screening tool to
predict fall risk in older adults: a systematic review.
Physiotherapy. 2018;104(4):383–94.Park SH, Lee YS.
The diagnostic accuracy of the berg balance scale in predicting falls.
West J Nurs Res. 2017;39(11):1502–25.Jacobson GP, Newman CW.
The development of the dizziness handicap inventory.
Arch Otolaryngol Head Neck Surg. 1990;116(4):424–7.Mutlu B, Serbetcioglu B.
Discussion of the dizziness handicap inventory.
J Vestib Res. 2013;23(6):271–7.Huang RJ, Smith SL, Brezina L, Riska KM.
A comparison of falls and dizziness handicap by vestibular diagnosis.
Am J Audiol. 2021;30(4):1048–57.Shin S, Valentine RJ, Evans EM, Sosnoff JJ.
Lower extremity muscle quality and gait variability in older adults.
Age Ageing. 2012;41(5):595–9.Callisaya ML, Blizzard L, Schmidt MD, Martin KL, McGinley JL, Sanders LM, et al.
Gait, gait variability and the risk of multiple incident
falls in older people: a population-based study.
Age Ageing. 2011;40(4):481–7.Park SH.
Tools for assessing fall risk in the elderly:
a systematic review and meta-analysis.
Aging Clin Exp Res. 2018;30(1):1–16.Lusardi MM, Fritz S, Middleton A, Allison L, Wingood M, Phillips E, et al.
Determining risk of falls in community dwelling older adults:
a systematic review and meta-analysis using posttest probability.
J Geriatr Phys Ther. 2017;40(1):1–36.Gade GV, Jørgensen MG, Ryg J, Riis J, Thomsen K, Masud T, et al.
Predicting falls in community-dwelling older adults:
a systematic review of prognostic models.
BMJ Open. 2021;11(5):e044170.Horak FB, Wrisley DM, Frank J.
The balance evaluation systems test (BESTest)
to differentiate balance deficits.
Phys Ther. 2009;89(5):484–98.Hausdorff JM.
Gait variability: methods, modeling and meaning.
J Neuroeng Rehabil. 2005;2:19.Gordt K, Gerhardy T, Najafi B, Schwenk M.
Effects of wearable sensor-based balance and gait training on balance,
gait,
and functional performance in healthy and patient populations:
a systematic review and meta-analysis of randomized controlled trials.
Gerontology. 2018;64(1):74–89.Shinohara T, Saida K, Miyata K.
Ability of the brief-balance evaluation systems test to evaluate
balance deficits in community-dwelling older adults:
a cross-sectional study.
Physiother. Theory Pract. 2020:1–8.Magnani PE, Genovez MB, Porto JM, Zanellato NFG, et al.
Use of the BESTest and the Mini-BESTest for fall risk prediction in
community-dwelling older adults between 60 and 102 years of age.
J Geriatr Phys Ther. 2020;43(4):179–84.Montero-Odasso MM, Kamkar N, Pieruccini-Faria F, et al.
Evaluation of clinical practice guidelines on fall prevention
and MANAGEMENT for older adults: a systematic review.
JAMA Netw Open. 2021;4(12):e2138911.Nouredanesh M, Godfrey A, Howcroft J, Lemaire ED, Tung J.
Fall risk assessment in the wild: a critical examination
of wearable sensor use in free-living conditions.
Gait Posture. 2021;85:178–90.Whedon JM, Toler AWJ, Goehl JM, Kazal LA.
Association between utilization of chiropractic services for
treatment of low back pain and risk of adverse drug events.
J Manip Physiol Ther. 2018;41(5):383–8.Whedon JM, Toler AWJ, Goehl JM, Kazal LA.
Association between utilization of chiropractic services for
treatment of low-back pain and use of prescription opioids.
J Altern Complement Med. 2018;24(6):552–6.Okamoto CS, Dunn AS, Green BN, Formolo LR, Chicoine D.
Correlation of body composition and low back pain severity
in a cross-section of US veterans.
J Manip Physiol Ther. 2017;40(5):358–64.Corcoran KL, Dunn AS, Formolo LR, Beehler GP.
Chiropractic Management for US Female Veterans with Low Back
Pain: A Retrospective Study of Clinical Outcomes
J Manipulative Physiol Ther. 2017 (Oct); 40 (8): 573–579Ciminata G, Geue C, Wu O, Deidda M, Kreif N, Langhorne P.
Propensity score methods for comparative-effectiveness analysis:
a case study of direct oral anticoagulants in the atrial fibrillation population.
Plos One. 2022;17(1):e0262293.Speiser JL, Callahan KE, Houston DK, Fanning J, Gill TM, Guralnik JM, et al.
Machine learning in aging: an example of developing prediction models
for serious fall injury in older adults.
J Gerontol A Biol Sci Med Sci. 2021;76(4):647–54.Dubois A, Bihl T, Bresciani JP.
Identifying fall risk predictors by monitoring daily activities at home
using a depth sensor coupled to machine learning algorithms.
Sensors (Basel). 2021;21(6):1–10.Reches T, Dagan M, Herman T, Gazit E, Gouskova NA, Giladi N, et al.
Using wearable sensors and machine learning to automatically detect
freezing of gait during a FOG-provoking test.
Sensors (Basel). 2020;20(16):1–16.Mirelman A, Ben Or Frank M, Melamed M, Granovsky L, Nieuwboer A, et al.
Detecting sensitive mobility features for Parkinson’s disease
stages via machine learning.
Mov Disord. 2021;36(9):2144–55.Min L, Tinetti M, Langa KM, Ha J, Alexander N, Hoffman GJ.
Measurement of fall injury with health care system data and
assessment of inclusiveness and validity of measurement models.
JAMA Netw Open. 2019;2(8):e199679.Hoffman GJ, Hays RD, Shapiro MF, Wallace SP, Ettner SL.
Claims-based identification methods and the cost of
fall-related injuries among US older adults.
Med Care. 2016;54(7):664–71.Bohl AA, Fishman PA, Ciol MA, Williams B, Logerfo J, Phelan EA.
A longitudinal analysis of total 3-year healthcare costs for
older adults who experience a fall requiring medical care.
J Am Geriatr Soc. 2010;58(5):853–60.Bohl AA, Phelan EA, Fishman PA, Harris JR.
How are the costs of care for medical falls distributed?
The costs of medical falls by component of cost,
timing, and injury severity.
Gerontologist. 2012;52(5):664–75.Roudsari BS, Ebel BE, Corso PS, Molinari NA, Koepsell TD.
The acute medical care costs of fall-related injuries among
the U.S. older adults.
Injury. 2005;36(11):1316–22.Womack JA, Murphy TE, Bathulapalli H, Smith A, Bates J, Jarad S, et al.
Serious falls in middle-aged veterans: development and
validation of a predictive risk model.
J Am Geriatr Soc. 2020;68(12):2847–54.Sox HC, Goodman SN.
The methods of comparative effectiveness research.
Annu Rev Public Health. 2012;33:425–45.Stefanos R, Graziella D, Giovanni T.
Methodological aspects of superiority, equivalence, and non-inferiority trials.
Intern Emerg Med. 2020;15(6):1085–91.Benson LC, Clermont CA, Bošnjak E, Ferber R.
The use of wearable devices for walking and running gait analysis
outside of the lab: a systematic review.
Gait Posture. 2018;63:124–38.Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al.
CONSORT 2010 statement:
extension to randomised pilot and feasibility trials.
BMJ. 2016;355:i5239.Homer V, Yap C, Bond S, Holmes J, Stocken D, Walker K, et al.
Early phase clinical trials extension to guidelines
for the content of statistical analysis plans.
BMJ. 2022;376:e068177.Guirguis-Blake JM, Michael YL, Perdue LA, Coppola EL, Beil TL.
Interventions to prevent falls in older adults: updated evidence report
and systematic review for the US preventive services task force.
JAMA. 2018;319(16):1705–16.Ellingsen DM, Napadow V, Protsenko E, Mawla I, Kowalski MH, Swensen D, et al.
Brain mechanisms of anticipated painful movements and their modulation
by manual therapy in chronic low Back pain.
J Pain. 2018;19(11):1352–65.Isenburg K, Mawla I, Loggia ML, Ellingsen DM, Protsenko E, Kowalski MH, et al.
Increased salience network connectivity following manual therapy is
associated with reduced pain in chronic low Back pain patients.
J Pain. 2021;22(5):545–55.
Return to VERTIGO and BALANCE
Since 9-06-2022


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |
