

Development of a Clinical Decision Aid for Chiropractic
Management of Common Conditions Causing Low Back
Pain in Veterans: Results of a Consensus ProcessThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Manipulative Physiol Ther. 2019 (Nov); 42 (9): 677–693 ~ FULL TEXT
OPEN ACCESS Robert D. Vining, DC, DHSc, Zacariah K. Shannon, DC, MS, Stacie A. Salsbury, PHD, RN, Lance Corber, MSITM, Amy L. Minkalis, DC, MS, Christine. M. Goertz, DC, PhD
Palmer Center for Chiropractic Research,
Davenport, Iowa.
robert.vining@palmer.edu
Thanks to JMPT for permission to reproduce this Open Access article! OBJECTIVE: The purpose of this study was to develop a clinical decision aid for chiropractic management of common conditions causing low back pain (LBP) in veterans receiving treatment in US Veterans Affairs (VA) health care facilities.
METHODS: A consensus study using an online, modified Delphi technique and Research Electronic Data Capture web application was conducted among VA doctors of chiropractic. Investigators reviewed the scientific literature pertaining to diagnosis and treatment of nonsurgical, neuromusculoskeletal LBP. Thirty seed statements summarizing evidence for chiropractic management, a graphical stepped management tool outlining diagnosis-informed treatment approaches, and support materials were then reviewed by an expert advisory committee. Email notifications invited 113 VA chiropractic clinicians to participate as Delphi panelists. Panelists rated the appropriateness of the seed statements and the stepped process on a 1–to–9 scale using the RAND/University of California, Los Angeles methodology. Statements were accepted when both the median rating and 80% of all ratings occurred within the highly appropriate range.
RESULTS: Thirty-nine panelists (74% male) with a mean (standard deviation) age of 46 (11) years and clinical experience of 17 (11) years participated in the study. Accepted statements addressed included (1) essential components of chiropractic care, (2) treatments for conditions causing or contributing to LBP, (3) spinal manipulation mechanisms, (4) descriptions and mechanisms of commonly used chiropractic interventions, and (5) a graphical stepped clinical management tool.
CONCLUSION: This study group produced a chiropractic clinical decision aid for LBP management, which can be used to support evidence-based care decisions for veterans with LBP.
KEYWORDS: Decision Support Techniques, Low Back Pain, Chiropractic, Complementary Therapies, United States, Consensus, Veterans
From the FULL TEXT Article:
Introduction
A clinical decision aid is an instrument providing information to assist clinicians and patients in making decisions about health care. [1] Inherent within an evidence-based decision aid is the concept that decisions practitioners make should include careful integration of experiential knowledge, scientific evidence, and patient preferences. [2] Decision aids are not designed to dictate decisions. Rather, they are designed to organize and summarize information gleaned from the scientific literature to help inform decision-making.
Low back pain (LBP) is highly prevalent, often leading to substantial disability. [3] The absence of tests that definitively categorize the many conditions causing LBP adds to the challenge of identifying a specific diagnosis to inform management decisions. [4] Although diagnoses often simply describe the main symptom, such as lumbalgia or low back pain, they can be more specific, theoretically leading to more informed clinical decision-making. [5–7] Several evidence-based classification systems are available to guide diagnostic evaluation. [8–11]
Doctors of chiropractic (DCs), including those employed within US Veterans Affairs (VA) health care facilities, provide nonpharmacologic, multimodal, conservative care primarily for musculoskeletal conditions, most often for LBP. [12] A fast-growing discipline within VA, chiropractic services are available at over 65 clinics nationwide, accounting for over 159,000 patient visits in 2016. [12] US Department of Defense and VA clinical practice guidelines recommend identifying specific diagnoses such as radiculopathy, neurogenic claudication, and psychosocial factors contributing to LBP. These recommendations are based on the premise that specific management options for these conditions are known, or considered, to be more appropriate than others. [13] Alhough guidelines generally describe evidence-based treatments for persons with LBP, they typically do not provide chiropractic management recommendations at a condition level for a range of commonly occurring diagnoses causing or contributing to neuromusculoskeletal LBP/ [14–16]
To address this information gap, the authors searched the scientific literature for evidence to inform chiropractic management decisions for patients with specific known or suspected LBP diagnoses and other factors that contribute to symptom augmentation or perpetuation. The purpose of this research was to develop and present an evidence-based chiropractic, multimodal treatment decision aid for managing LBP in US veterans using a consensus-building Delphi process.
Methods
Project Overview
This study was part of a funded research project (5UG3AT009761-02) designed to evaluate the comparative effectiveness of various treatment dose levels of chiropractic care for veterans with LBP. Two thematically related studies accompanied this project. The first was a systematic review of evidence for diagnosing common conditions causing LBP and recommendations for standardized terminology use. The systematic review then informed the development of a practical diagnostic checklist and clinical exam leading to evidence-based and specific working diagnoses. [17, 18] The purpose of this study was to develop an in-office resource functioning as a treatment decision aid summarizing research evidence to inform VA chiropractic providers caring for US military veterans with LBP.
Human Participant Considerations
This study, using modified Delphi panel consensus methods, was exempted by the Palmer College of Chiropractic Institutional Review Board with the assurance number X2018-4-10-V on May 14, 2018. All expert advisors and Delphi panelists provided consent to participate in the study and those acknowledged in the manuscript provided signed permission. Expert advisors were offered an honorarium for their involvement in the project.
Research Personnel and Participants
The investigative team consisted of members with expertise in chiropractic, clinical research, and Delphi process methodology. This team reviewed relevant research literature, developed seed statements and supporting documents, identified external advisors and potential Delphi panelists, managed the data collection process, and finalized all findings. Three leaders in evidence-based chiropractic practice reviewed all Delphi materials and provided iterative feedback. All VA chiropractic providers designated as chiropractor within the VA e-mail system (n = 113), not including chiropractic residents, interns, or students (n = 20), were invited to rate the clinical decision aid materials and provide critical feedback.
Source Documents and Seed Statements
The lead investigator (R.V.) prepared initial seed statements based on literature obtained from topic-based reviews of the published literature. Because clinical management of LBP represents the compilation of many topics, systematic reviews of each area were not performed. Retrieved documents were categorized according to an evidence hierarchy. The highest available levels of evidence, such as systematic reviews and meta-analyses, were prioritized for seed statement development. [19, 20] For some statements, no systematic reviews were available. In these instances, randomized controlled trials and observational studies provided evidentiary support.
Some statements, such as those describing mechanisms influenced by interventions, were supported by basic science research or best-practice documents.
Seed statements were refined though an iterative process among 3 additional investigators (S.S., Z.S., A.M.), then organized into thematic headings. Statements included a graphical, stepped-process, clinical management tool for patients with LBP. The external advisors reviewed and rated each seed statement and the stepped-process clinical management tool and provided written feedback, which included suggestions for additional references to support statements. Using ratings and comments from external advisors conducted through 2 separate rounds, the investigative team finalized revisions and approved statements for distribution to Delphi panelists.
Modified Delphi Consensus Process
We used a modification of the RAND Corporation/University of California, Los Angeles consensus methodology on appropriateness ratings to conduct this study. [21] Data collection was conducted electronically using Research Electronic Data Capture (REDCap) (Vanderbilt University, Nashville, Tennessee).
REDCap is a secure web-based application designed for research, providing(1) an interface for validated data entry,
(2) audit trails for tracking data manipulation and export procedures,
(3) automated export procedures for analysis with common statistical packages, and
(4) procedures for importing data from external sources. [22] Electronically facilitated Delphi processes have been used within the profession to develop guidelines and best-practice documents. [15, 23, 24]The Delphi process launched in August 2018 and concluded in September 2018. Potential panelists first received an informational e-mail about the upcoming Delphi-process study from the chiropractic program director for VA. One week later, e-mail invitations were sent through REDCap to 113 potential panelists. This invitation contained a description of the decision aid development process and a link to a consent document. Potential panelists who agreed to be part of the Delphi panel submitted a recent curriculum vitae to confirm eligibility. Eligible panelists received an e-mailed link to the first-round survey in REDCap. Panelists completed demographic information and an investigator-designed questionnaire to assess self-reported knowledge of evidence-based, multimodal chiropractic interventions for LBP. Responses were recorded on a 5-point scale ranging from not at all knowledgeable (1) to very knowledgeable (5), with results collapsed into 3 categories for reporting purposes.
Individual panelists rated each seed statement and the stepped management tool along a 9–item numeric scale. Possible ratings ranged from 1 to 3 (highly inappropriate), 4 to 6 (undecided), and 7 to 9 (highly appropriate). Appropriateness was defined as a statement suggesting the expected health benefit to the patient exceeds the expected negative consequences by a sufficiently wide margin that the recommendation is worth doing, exclusive of cost.21 To increase transparency, each seed statement included electronic links to PubMed abstracts for supporting references and a classification list identifying the study design of supporting references. For any statements not receiving a 7–to–9 rating, we asked panelists to provide rationale and references. Comments about seed statements, regardless of rating, were encouraged through instructions and with available free text boxes throughout the survey. Consensus was defined when at least 80% of panelists rated a statement within a 7–to–9 range and the median rating was also located within the same range. Before panelist review, the authors determined that statements not meeting consensus would be revised after each round and removed after the third round if no consensus was achieved.
Panelists’ rating and feedback data were exported from REDCap as a de-identified data set into Microsoft Excel. Deidentified demographic data were analyzed separately in SPSS Statistics for Windows, version 25.0 (Armonk, NY, IBM Corp).
Results

Table 1

Table 2 Thirty-nine VA DCs served as consensus panelists (35% response rate). Demographic characteristics (Table 1) included a mean (standard deviation) age of 46 (11) years, 17 (11) years of clinical experience in chiropractic, and 5 (5) years employed as a VA chiropractor. Over 50% of panelists reported prior involvement in a Delphi consensus study, 77% reported using a decision aid in practice, and 92% reported using tissue-specific diagnoses to characterize LBP. Table 2 displays self-reported knowledge of multimodal chiropractic care. Most panelists reported being “quite” or “very” knowledgeable (≥85%) regarding spinal manipulation (thrust), patient education, self-management, home/general exercise, myofascial therapies, lumbar mobilization exercise, and flexibility exercise.
Seed statements included definitions of 6 distinct components of chiropractic care. Each component was reviewed under the framework that VA DCs should consider each component for each patient. In some instances, an individual component may not be employed owing to circumstances or characteristics unique to each patient.
Consensus Statements: 6 Components of Multimodal Chiropractic Care
Education: All chiropractic care or evaluation should include education to inform patients about their condition and interventions and to foster health literacy. The goal of such education is to provide information to enable patients to make appropriate health care decisions. [13, 25] Education can provide long-term reassurance, and it is recommended to help patients manage chronic conditions. [26, 27] Conversely, low health literacy is associated with poor health outcomes through limiting the capacity to acquire self-care knowledge and skills. [28, 29]
Passive interventions: Passive interventions require patients to receive treatment rendered by another person, such as spinal manipulation and acupuncture. Continuous dependence on passive treatments can reinforce patient feelings of powerlessness, create dependency on providers, and place the majority of pain management responsibility on providers. [30]
Transitional interventions: Transitional interventions are monitored or guided by a provider but performed by a patient during active care to reinforce or enhance the effectiveness of provider-based passive treatment. An example of a transitional treatment is repeated motion exercise, designed for patients to conduct on their own and between visits to reduce pain and improve flexibility. [30]
Active interventions: Active interventions are controlled and performed by a patient independent from passive or transitional interventions. Examples of active interventions are mindfulness, general exercise, yoga, and tai chi. [30]
Self-management: Self-management refers to a process individuals use to self-monitor, control, or reduce the impact of a condition over time. [31] This continuous process requires sufficient knowledge of a condition and skills necessary to maintain good psychosocial function. [31] Doctors of chiropractic should recommend self-management strategies, such as general exercise, as appropriate. [32–34]
Visit frequency and duration (intervention dose): Visit frequency and duration should be determined by synthesizing clinical information such as the diagnosis, physical condition, care goals, intervention options, and expected response. Although general visit frequency and duration should be planned before treatment begins, response to care and changes in patient presentation, or other new information, may warrant changing a prescribed visit frequency and duration at any point during care. [35]
Evidence-Based Interventions for Conditions That Cause, Complicate,
or Otherwise Contribute to Low Back Pain
Facet (zygapophysial/z-joint) joint pain: pain perceived from nociceptive signaling originating within or surrounding a facet joint [36]
Interventions:
Education about the condition [13, 25–29, 33, 34]
Spinal manipulation (thrust or non-thrust as tolerated) [10, 13, 37–39]
Heat, massage, low-level laser [37, 38]
Motor control exercise [37, 38]
General self-care and self-management advice [37, 38]
Consider recommending mindfulness-based stress reduction, tai chi, yoga, and progressive relaxation [37, 38]
Sacroiliac joint pain: Pain stemming from a sacroiliac joint [36]
Interventions:
Education about the condition [13, 25–29, 33, 34]
Spinal manipulation [40]
Regional muscle strengthening [41]
Motor control exercise [37, 38]
Heat, massage, low-level laser [37, 38]
General self-care and self-management advice [37, 38]
Consider recommending mindfulness-based stress reduction, tai chi, yoga, and progressive relaxation [37, 38]
Discogenic pain: lumbar spinal pain, with or without referred pain, stemming from a lumbar intervertebral disk [36]
Interventions:
Education about the condition [13, 25–29, 33, 34]
Spinal manipulation (thrust and/or non-thrust as tolerated) [37, 38]
Directional preference exercises [9, 42]
Motor control exercise [37, 38]
Heat, massage, low-level laser [37, 38]
General self-care and self-management advice [37, 38]
Consider recommending mindfulness-based stress reduction, tai chi, yoga, and progressive relaxation [37, 38]
Myofascial pain: pain arising from muscles or related fascia [43]
Interventions:
Education about the condition [13, 25–29, 33, 34]
Myofascial-oriented therapies such as ischemic compression as indicated and as tolerated[44]
Spinal manipulation [37, 38]
Motor control exercise [37, 38]
Heat, massage, low-level laser [37, 38]
Self-management advice such as self-stretching, self-massage, home exercise, and home heat/ice44
Comanage with other provider(s) when neede [44]
Consider recommending mindfulness-based stress reduction, tai chi, yoga, and progressive relaxation [37, 38]
Pain of radicular origin: As defined by the International Association for the Study of Pain, radiculopathy and radicular pain are separate and distinct. However, the conditions may coexist or be caused by a single pathology. [45] Radiculopathy is defined as the loss of sensory or motor axon conduction owing to nerve root compression or ischemia. [45] Radicular pain is defined as ectopic nociceptive firing within spinal nerves due to inflammation, mechanical strain, or possible ischemic damage to dorsal root ganglia, resulting in pain perceived in the nerve-supplied territory. [45]
Interventions:
Education about the condition [13, 25–29, 33, 34]
Neurodynamics (neural mobilization) when tolerated [46]
Spinal manipulation (thrust and/or non-thrust as tolerated) [10, 14, 16, 39, 47]
Directional preference exercises [42]
Neurogenic claudication: pain caused by intermittent compression and/or ischemia of a single or multiple nerve roots [48]
Interventions:
Education about the condition [13, 25–29, 33, 34]
Spinal manipulation (thrust and/or non-thrust as tolerated) [49–51]
Neurodynamics (neural mobilization) [49–51]
Muscle stretching [49, 51]
Lumbar mobilization exercise [49, 51]
Self-management via a cognitive behavioral approach including goal-setting, graded activity, pacing, relaxation, and body positioning techniques to reduce lumbar lordosis [49, 51]
Home exercises when tolerated [49, 51]
Comanage with other providers when needed [52]
Central sensitization: increased responsiveness of nociceptive neurons to their normal input or recruitment of a response to normally subthreshold inputs [36]
Interventions:
Education about chronic pain mechanisms [53–55]
Myofascial therapy to prevent and/or manage myofascial derangement from painful postures and/or movements [56]
Spinal manipulation exhibits short-term influence on neural pain processes [57–62]
Consider recommending graded exposure training [63] and mindfulness-based stress reduction [37, 38]
Poor muscle coordination potentially reducing functional spinal stability:
Interventions:
Education about the condition [13, 25–29, 33, 34]
Motor control or other exercise training [37, 38, 64]
Spinal stabilization or other forms of exercise such as brisk walking or cycling [65]
Self-management advice such as movement-based strategies for spine stability [9, 25]
General muscle weakness or improving overall physical fitness:
Interventions:
Education about the condition [13, 25–29, 33, 34]
Activity-specific or physical fitness exercise [66]
Self-management advice such as nutritional, and general activity advice to improve fitness/strength [9]
Psychosocial factors or conditions
(eg, fear, emotional trauma, depression, anxiety, social disconnection, passive coping):Interventions:
Education to prevent/reduce fears, passive coping, and catastrophizing, and to promote self-efficacy [53]
Refer/comanage with mental health provider [67–69] for evidence-based treatments such as cognitive behavioral therapy, [70, 71] and acceptance and commitment therapy [72] when appropriate
Mindfulness-based stress reduction [37, 38]
Spinal Manipulation
Research evidence supports the skilled use of spinal manipulation for a wide range of conditions that cause low back pain. The American College of Physicians recommends spinal manipulation along with other conservative treatments as an appropriate first-line therapeutic approach for low back pain. [13, 16, 37]
Currently, both manual thrust (high-velocity, low amplitude) and non-thrust (low-velocity, variable amplitude) spinal manipulative procedures show roughly equal therapeutic benefit for patients with low back pain. This suggests the choice of manipulative technique to use for patients should be determined by patient history, preference, tolerance to a given procedure, available equipment, and provider familiarity and skill. [73–77]
Suspected Mechanisms Underlying Spinal Manipulation
Pain reduction: Research evidence suggests spinal manipulation has a pain-modulating effect on central nervous system processing in the short term. Research is inconclusive if central nervous system changes influenced by spinal manipulation occur in the long term. [58, 61, 78–80]
Joint or regional mobility: Tissue stretching and neurophysiological mechanisms initiated during spinal manipulation are thought to contribute to increased joint or regional mobility. [81, 82]
Muscular effects: Research evidence suggests spinal manipulation can potentially alter motor neuron facilitation or disinhibition. [83–85] Other not fully understood, but observed, effects include changes in muscle tone [86, 87] and increased trunk and multifidus muscle thickness. [88]
Joint function: Theoretical and basic science evidence suggests that spinal manipulation may disrupt intra- or periarticular adhesions located in disused, injured, or degenerated tissues within and around spinal joints. [89–91] However, this has not yet been observed in human studies.
Myofascial tissues: Theoretical and basic science evidence suggests that tissue stretching during spinal manipulation may generate shearing movements between fascial layers of paraspinal tissues. [92]
Other Interventions
Friction massage: repeated rubbing over designated areas (muscles, tendons, fascia) to generate friction within myofascial tissues, applied manually or with specialized tools [93]
Suspected/proposed mechanism(s):
Treatment goal(s):
Disrupt adhesions between adjacent tissues that restrict movement or cause pain
Temporarily increase blood or lymphatic flow
Reduce pain, disrupt adhesions, reduce muscle tone, and stimulate lymphatic flow
Improve joint or myofascial motion, improve local circulation, and reduce pain
Myofascial techniques (soft tissue manipulation or mobilization): pressure applied to myofascial tissues, sometimes combined with stretching [94, 95]
Suspected/proposed mechanism(s):
Treatment goal(s):
Disrupt myofascial adhesions that restrict movement or cause pain
Stretch contracted tissue(s)
Stimulate or improve lymphatic circulation
Improve joint and/or myofascial motion, improve local circulation, and reduce pain
Strengthening, fitness, motor control, or stability exercises: activities focused on developing strength, endurance, coordination, or joint/regional stability through enhancing muscle function [64]
Suspected/proposed mechanism(s):
Treatment goal(s):
Improve muscle strength, endurance, and/or coordination through exercises designed to enhance targeted performance
Improve ability to perform specific activities, reduce pain, and/or prevent injury during identified activity
Neurodynamics (neural mobilization): carefully controlled movement of the head, spine, or limb(s) causing nerve stretching or movement [46, 96, 97]
Suspected/proposed mechanism(s):
Treatment goal(s):
Improve nerve or lower extremity mobility by reducing abnormal tension and disrupting adhesions located around nerves
Desensitize neural structures
Reduce nerve tension-related pain
Reduce or prevent fibrous neural entrapment
Improve lower extremity flexibility
Reduce pain and disability
Graded activity and exposure training: graded activity and exposure to progressively more functional activities and behaviors using a cognitive behavioral approach [63, 98, 99]
Suspected/proposed mechanism(s):
Treatment goal(s):
Decrease disability
Improve patient understanding of condition
Understand and set feasible activity goals
Improve self-efficacy, active coping
Reduce catastrophizing
Desensitize neural structures
Reduce fear of activities through education and experience with safe activities
Achieve progressive functional improvement, especially in areas where patient is fearful of safe-to-perform activities
Directional preference exercise: repeated movement causing centralization, symptom reduction, or improved range of motion [42]
Suspected/proposed mechanism(s):
Treatment goal(s):
Relieves or reduces mechanical irritation or inflammation of pain-producing tissue(s)
Reduce pain, increase range of motion, and encourage self-care and safe movement
Low-level laser: noninvasive and painless light generated
Suspected/proposed mechanism(s):
Treatment goal(s):
May produce anti-inflammatory effects and/or stimulate other physiological changes within tissues and individual cells
Stimulate tissue repair, stimulate acupuncture points

Figure 1
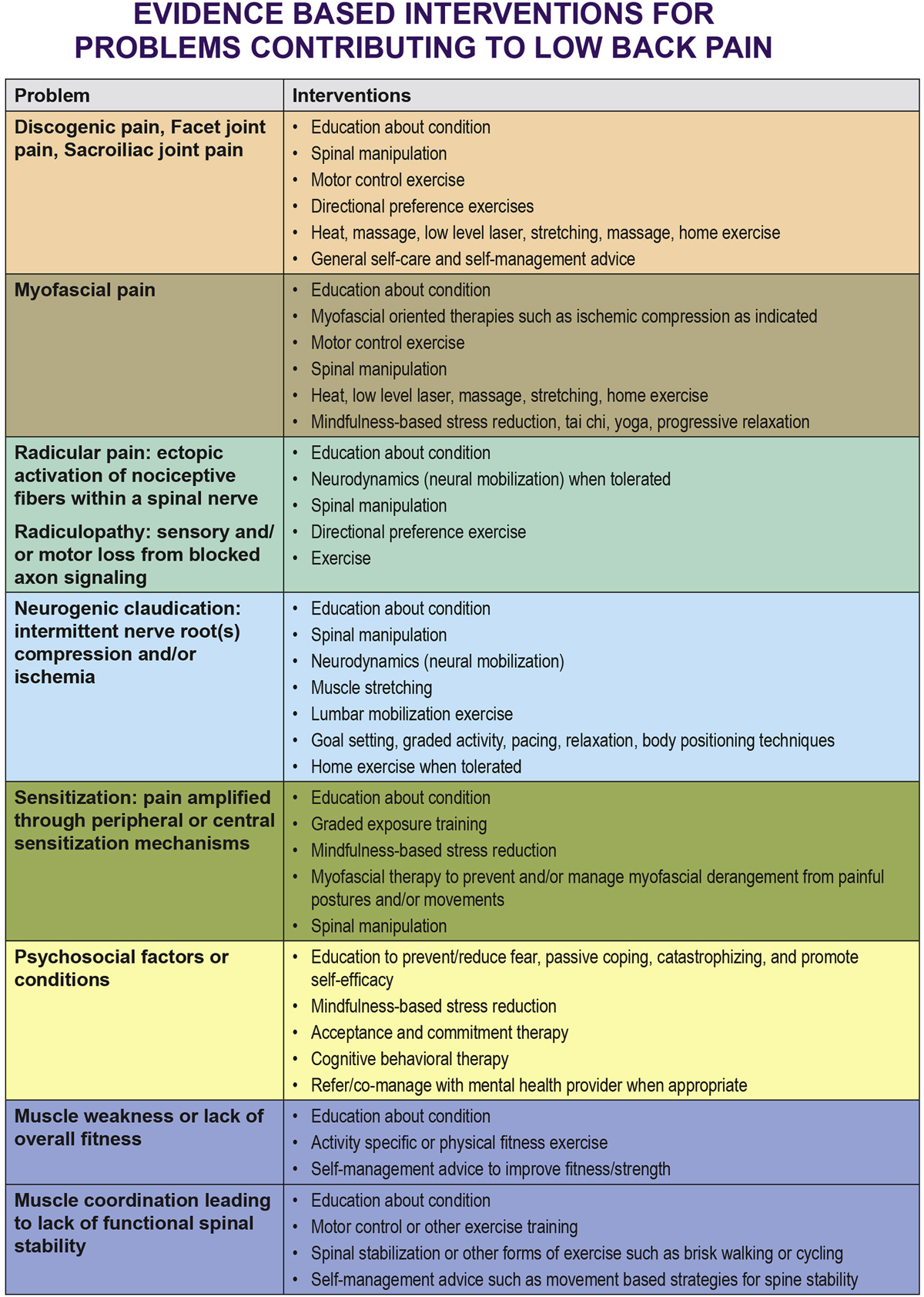
Figure 2

Figure 3
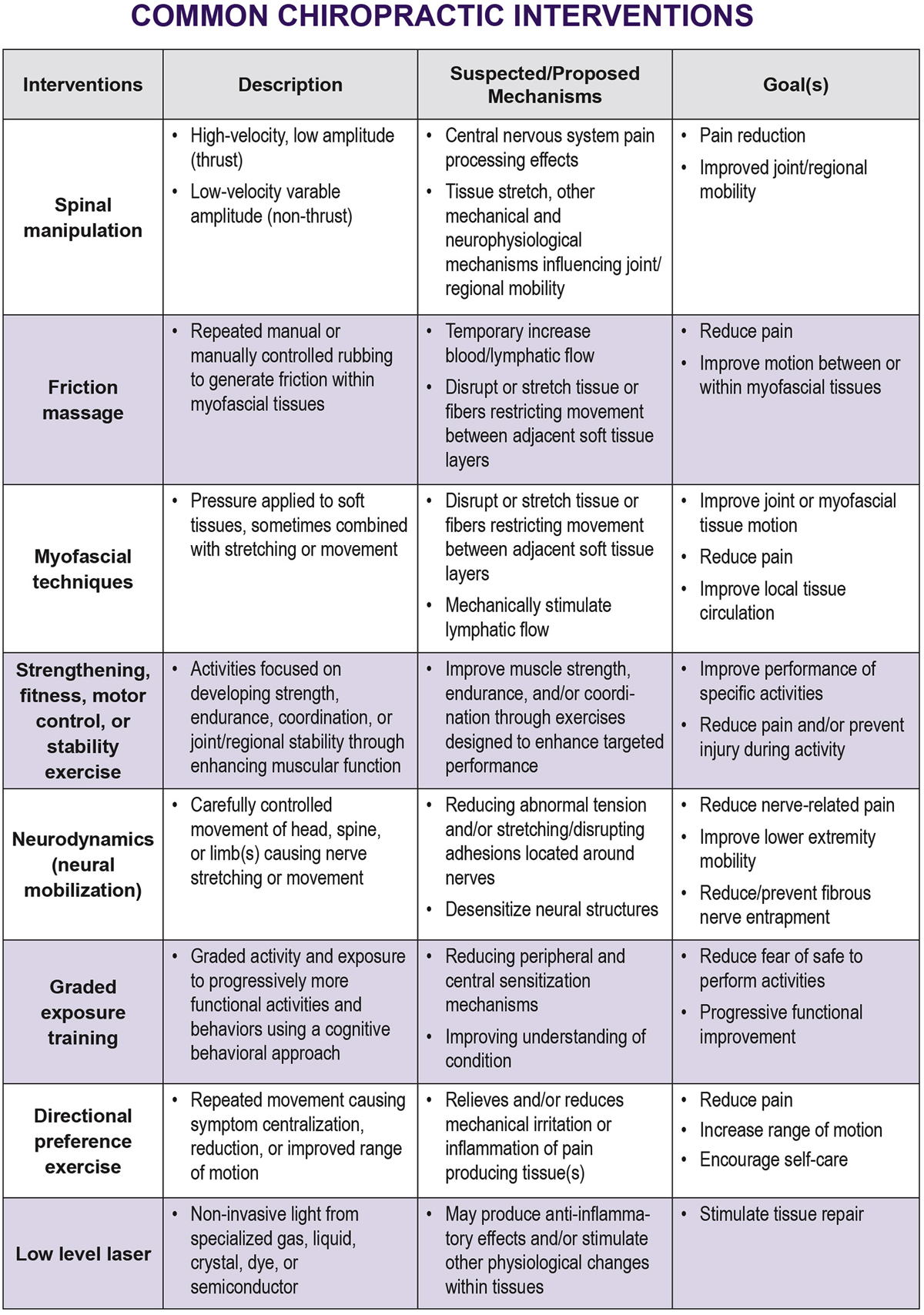
Figure 4
Figure 1 displays the management tool modeling a process with 5 distinct decision-making steps. Although each step is discrete from others, decision-making may occur simultaneously. Figure 2 lists evidence-based interventions by diagnostic category. Figure 3 lists 6 essential components of chiropractic care. Figure 4 displays evidence-based intervention descriptions. Each figure was designed as a single-page summary of results from this study. The resulting 4–page document provides a quick-access, topical information resource for clinical office settings.
We have provided an instructional video that provides an overview of this information (see video file online).
Discussion
Although multimodal chiropractic care is a prominent practice pattern, DCs select from among dozens of possible interventions. [101, 102] Few tools are available to assist in this decision-making process. The decision aid developed in this study is supported by varying levels of evidence. Whenever possible, systematic reviews and meta-analyses, or guidelines and reports based on systematic reviews and meta-analyses, were used to support statements. Other evidence considered lower on the evidence hierarchy was used when systematic reviews and meta-analyses were unavailable or when reviews were incomplete or missing relevant studies.
Perhaps the most significant factors influencing the quality of research involving manual therapies employed by DCs is the inability to blind patients and practitioners in clinical trials and the absence of inert sham procedures. Other factors influencing the quality of research supporting some statements is the relative absence of randomized controlled trials conducted in symptomatic populations combined with the current limited understanding of the mechanisms underlying spinal manipulation. Statements describing suspected or proposed mechanisms underlying spinal manipulation and other manual treatments are typically based on basic science research using animal models, studies with asymptomatic persons, or clinical studies measuring associations without the ability to draw clear causal relationships. There is a general lack of evidence for noninvasive treatments focused on managing specific conditions causing or contributing to LBP. Many of the references supporting statements represent research on the effect of noninvasive treatments for LBP labeled as nonspecific, including some used to support statements on central sensitization, poor muscle coordination, and psychosocial factors. Studies on interventions for more specific diagnoses were referenced when available.
General exercise and specific exercises, such as lumbar mobilization, stabilization, and neurodynamics, are suggested as intervention options in this decision aid. Systematic reviews suggest there is no difference in outcomes when comparing specific versus general exercises in clinical studies. [65] Therefore, recommending an exercise enjoyed by a patient or one a patient is willing to perform may be better than a limited or condition-specific exercise regimen.
Strengths and Limitations
There were 3 unique strengths of this study. The first was incorporating definitions into the seed statements. Diagnostic terminology is not used consistently in the literature or among clinicians. Referenced definitions helped avoid confusion and provided a common framework to assess statement appropriateness. The second was the ability of panelists to link directly to the PubMed abstract and, oftentimes the peer-reviewed publication, for every supporting reference. Evidence that this feature was used by panelists was indicated in their numerous comments referring to abstract review. Third, we included a description of the type of research supporting each reference, such as systematic review and meta-analysis, randomized controlled trial, observational study, narrative review, clinical guideline, and expert recommendations. These descriptors added another level of transparency.
This study had several limitations. Although the inclusion of 39 panelists was considered a good response rate (35%), it is possible that additional respondents could have alternately influenced results. Many consensus process studies are conducted among recognized experts among several disciplines. This study was conducted with VA providers from a single discipline without explicitly seeking expert status. These factors may also influence results. A systematic review of the literature pertaining to each topic in the decision aid was not performed. Literature supporting or refuting some statements may have been missed. Several statements were supported by limited evidence and thus could change when new or higher-quality research becomes available. Evidence interpretation of authors and expert advisors may also influence results. Some research supporting statements evaluated multimodal treatment approaches to a specific patient diagnosis. Conclusions regarding single therapies used within a multimodal treatment package should be made with caution because these studies did not assess the relative contribution of individual treatments.
As expected, we observed disparate views of evidence interpretation. For example, except for the statement describing joint mobility, at least 1 panelist expressed that statements describing mechanisms initiated or influenced by spinal manipulation were insufficiently supported by the references provided. Most panelists reported limited knowledge of several evidence-based approaches to LBP management, such as graded exposure training, tai chi, yoga, mindfulness-based stress reduction, and cognitive behavioral therapy, which has implications for the validity of the panelists’ appropriateness ratings. This finding also suggests potential training opportunities for DCs and chiropractic students, both within and outside VA. For example, VA Patient Centered Care and Whole Health for Life initiatives seek to enhance self-care by veterans, particularly those with chronic health conditions. [103] Although it is unlikely that most chiropractors would apply cognitive behavioral therapy or mindfulness-based stress reduction in their clinics, additional training about such modalities may help DCs better identify and refer individuals most likely to benefit from such activities.
Lastly, the materials that we present in this study need to be tested clinically. We cannot say if these documents will help with providing improved diagnoses or better care for patients. Additional research is needed to understand the effects of this decision aid on management decisions and clinical outcomes.
Conclusion
This article offers an evidence-based clinical decision aid for multimodal chiropractic care for veterans with LBP. A 4–page document outlines the management process, evidence-based treatments for specific conditions, intervention descriptions, and definitions for 6 essential components of chiropractic care. The decision aid was validated through a web-based consensus process including DCs practicing in VA health care facilities.
Appendix A.
Acknowledgments:
The authors thank our external advisory committee members for their assistance with seed statement review and development: Cheryl Hawk, DC, PhD, Donald R. Murphy, DC, and Michael J. Schneider, DC, PhD. We also thank Anthony Lisi, DC, for advising investigators on implementation of this Delphi process with DCs within Veterans Affairs. The feedback from Delphi panelists who participated in this study was essential to successful completion of this study. Delphi panelists were Michael T. Anderson, DC, Shery Assal, DC, Gina M. Bonavito-Larragoite, DC, FIAMA, Kathy Boulet, DC, Dipl. Acup., Kimberly S. Brown, MA, DC, Nathan J. Campbell, MSM, DC, DACBSP, Zachary A. Cupler, DC, Jessica J. Dziurkowski, DC, Lance R. Formolo, DC, MS, Richard Forrette, DC, Ryan Furniss, DC, Jason Gibson, DC, DABCA, Valerie Johnson, DC, DABCI, DACBN, Monte C. Lindmier, DC, Nathaniel C. Majoris, DC, ATC, Shawn M. Neff, DC, MAS, Christopher Pierson, DC, Roger Kevin Pringle, DC, MEd, Lindsay Rae, DC, Todd S. Rubley, MS, DC, Alec Schielke, DC, C. Bret Sullivan, DC, FACO, Jeffrey M. Warner, MPH, DC, and Clint J. Williamson, DC.
Funding Sources and Conflicts of Interest
This work is supported by the National Institutes of Health (NIH) through cooperative agreement U24AT009769 from the National Center for Complementary & Integrative Health ( NCCIH ) and cooperative agreement 5UG3AT009761-02 , and from the Office of Research on Women's Health (ORWH) UH3 AT 09761. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Drs Vining, Salsbury, Shannon, Minkalis, and Goertz and Mr Corber report grant support from NIH/NCCIH for the work reported in this article. Dr Goertz reports grants from NIH/NCCIH and personal fees from Palmer College of Chiropractic, the American Chiropractic Association, Spine IQ, Prezacor Inc, and the Patient-Centered Outcomes Research Institute. Dr Shannon reports grants from NIH/NCCIH and the NCMIC Foundation. No other conflicts of interest were reported for this study.
References:
Trevana L. McCaffery K. Salkeld G. et al.
Clinical decision-making tools: how effective are they in improving the quality of health care?
Deeble Institute Issues Brief, 2014Sackett D. Straus S. Richardson W. Rosenberg W. Hayes R.
Evidence-Based Medicine: How to Practice and Teach EBM.
2nd ed. Churchill Livingstone, New York, NY2000Hoy D, March L, Brooks P, et al.
The Global Burden of Low Back Pain: Estimates from the Global Burden of Disease 2010 study
Ann Rheum Dis. 2014 (Jun); 73 (6): 968–974Negrini S. Zaina F.
The chimera of low back pain etiology: a clinical rehabilitation perspective.
Am J Phys Med Rehabil. 2013; 92: 93-97Petersen T, Laslett M, Juhl C.
Clinical Classification in Low Back Pain: Best-evidence Diagnostic Rules Based on Systematic Reviews
BMC Musculoskelet Disord. 2017 (May 12); 18 (1): 188Simopoulos T. Manchikanti L. Singh V. et al.
A systematic evaluation of prevalence and diagnostic accuracy of sacroiliac joint interventions.
Pain Physician. 2012; 15: E305-E344Nijs J., Apeldoorn A., Hallegraeff H., et al.
Low Back Pain: Guidelines for the Clinical Classification of Predominant Neuropathic, Nociceptive,
or Central Sensitization Pain
Pain Physician. 2015 (May); 18 (3): E333–346Vining R, Potocki E, Seidman M, Morgenthal AP.
An Evidence-based Diagnostic Classification System For Low Back Pain
J Canadian Chiropractic Assoc 2013 (Sep); 57 (3): 189–204Alrwaily M. Timko M. Schneider M. et al.
Treatment-based classification system for low back pain: revision and update.
Phys Ther. 2016; 96: 1057-1066Murphy DR, Hurwitz EL.
Application of a Diagnosis-Based Clinical Decision Guide in Patients with Neck Pain
Chiropractic & Manual Therapies 2011 (Aug 27); 19: 19Haldeman S., Johnson C.D., Chou R. et al.
The Global Spine Care Initiative: Classification System for Spine-related Concerns
European Spine Journal 2018 (Sep); 27 (Suppl 6): 889–900Lisi AJ, Brandt CA.
Trends in the Use and Characteristics of Chiropractic Services
in the Department of Veterans Affairs
J Manipulative Physiol Ther. 2016 (Jun); 39 (5): 381–386The Diagnosis and Treatment of Low Back Pain Work Group.
VA/DoD Clinical Practice Guideline for Diagnosis and Treatment of Low Back Pain
Washington, DC: The Office of Quality, Safety and Value, VA, &
Office of Evidence Based Practice, U.S. Army MedicalCommand, 2017, Version 2.0.Bussieres AE, Stewart G, Al-Zoubi F, Decina P, Descarreaux M, Haskett D, Hincapie C, et al.
Spinal Manipulative Therapy and Other Conservative Treatments for Low Back Pain:
A Guideline From the Canadian Chiropractic Guideline Initiative
J Manipulative Physiol Ther. 2018 (May); 41 (4): 265–293Globe, G, Farabaugh, RJ, Hawk, C et al.
Clinical Practice Guideline: Chiropractic Care for Low Back Pain
J Manipulative Physiol Ther. 2016 (Jan); 39 (1): 1–22Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, et al.
Nonpharmacologic Therapies for Low Back Pain: A Systematic Review for an
American College of Physicians Clinical Practice Guideline
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 493–505Vining R, Shannon Z, Minkalis A, Twist E.
Current Evidence for Diagnosis of Common Conditions Causing Low Back Pain:
Systematic Review and Standardized Terminology Recommendations
J Manipulative Physiol Ther. 2019 (Nov); 42 (9): 651–664Vining R, Minkalis A, Shannon Z, Twist E.
Development of an evidence-based practical diagnostic checklist and corresponding clinical exam for low back pain.
J Manipulative Physiol Ther, in press.Evans D.
Hierarchy of evidence: a framework for ranking evidence evaluating healthcare interventions.
J Clin Nurs. 2003; 12: 77-84Harbour R. Miller J.
A new system for grading recommendations in evidence based guidelines.
BMJ. 2001; 323: 334-336Fitch K. Bernstein S. Aguilar M. et al.
RAND UCLA Appropriateness Method User’s Manual.
RAND, Santa Monica, CA2001Harris P.A. Taylor R. Thielke R. Payne J. Gonzalez N. Conde J.G.
Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process
for providing translational research informatics support.
J Biomed Inform. 2009; 42: 377-381Hawk C, Schneider M, Dougherty P, Gleberzon BJ, Killinger LZ.
Best Practices Recommendations for Chiropractic Care for Older Adults:
Results of a Consensus Process
J Manipulative Physiol Ther 2010 (Jul); 33 (6): 464–473Hawk C, Schneider M, Evans MW Jr, Redwood D:
Consensus Process to Develop a Best-Practice Document on the Role of Chiropractic Care
in Health Promotion, Disease Prevention, and Wellness
J Manipulative Physiol Ther. 2012 (Sep); 35 (7): 556–567Wong JJ, Cote P, Sutton DA, et al.
Clinical Practice Guidelines for the Noninvasive Management of Low Back Pain: A Systematic Review
by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration
European J Pain 2017 (Feb); 21 (2): 201–216Snelgrove S. Liossi C.
Living with chronic low back pain: a metasynthesis of qualitative research.
Chronic Illn. 2013; 9: 283-301Traeger A.C. Hübscher M. Henschke N. Moseley G.L. Lee H. McAuley J.H.
Effect of primary care-based education on reassurance in patients with acute low back pain:
systematic review and meta-analysis.
JAMA Intern Med. 2015; 175: 733-743Dewalt D.A. Berkman N.D. Sheridan S. Lohr K.N. Pignone M.P.
Literacy and health outcomes: a systematic review of the literature.
J Gen Intern Med. 2004; 19: 1228-1239Edward J. Carreon L.Y. Williams M.V. Glassman S. Li J.
The importance and impact of patients' health literacy on low back pain management:
a systematic review of literature.
Spine J. 2018; 18: 370-376Cosio D. Lin E.
Role of active versus passive complementary and integrative health approaches in pain management.
Glob Adv Health Med. 2018; 7 (2164956118768492)Barlow J. Wright C. Sheasby J. Turner A. Hainsworth J.
Self-management approaches for people with chronic conditions: a review.
Patient Educ Couns. 2002; 48: 177-187Du S. Hu L. Dong J. et al.
Self-management program for chronic low back pain: a systematic review and meta-analysis.
Patient Educ Couns. 2017; 100: 37-49Woby S.R. Urmston M. Watson P.J.
Self-efficacy mediates the relation between pain-related fear and outcome in chronic low back pain patients.
Eur J Pain. 2007; 11: 711-718Main C.J. Foster N. Buchbinder R.
How important are back pain beliefs and expectations for satisfactory recovery from back pain?
Best Pract Res Clin Rheumatol. 2010; 24: 205-217Lisi AJ, Salsbury SA, Hawk C, Vining RD, Wallace RB, Branson R, et al.
Chiropractic Integrated Care Pathway for Low Back Pain in Veterans:
Results of a Delphi Consensus Process
J Manipulative Physiol Ther. 2018 (Feb); 41 (2): 137–148International Association for the Study of Pain
Classification of Chronic Pain. 2nd ed (revised). (Available at:)
https://www.iasp-pain.org/PublicationsNews/Content.aspx?ItemNumber=1673&navItemNumber=677
Date accessed: November 5, 2018Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, et al.
Noninvasive Treatments for Low Back Pain
Comparative Effectiveness Review no. 169
Agency for Healthcare Research and Quality; (February 2016)Murphy DR, Hurwitz EL, McGovern EE:
A Nonsurgical Approach to the Management of Patients With Lumbar Radiculopathy
Secondary to Herniated Disk: A Prospective Observational Cohort Study With Follow-Up
J Manipulative Physiol Ther 2009, 32(9):723-733Kamali F. Shokri E.
The effect of two manipulative therapy techniques and their outcome in patients with sacroiliac joint syndrome.
J Bodyw Mov Ther. 2012; 16: 29-35Rashbaum R.F. Ohnmeiss D.D. Lindley E.M. Kitchel S.H. Patel V.V.
Sacroiliac joint pain and its treatment.
Clin Spine Surg. 2016; 29: 42-48May S. Aina A.
Centralization and directional preference: a systematic review.
Man Ther. 2012; 17: 497-506Bennett R.
Myofascial pain syndromes and their evaluation.
Best Pract Res Clin Rheumatol. 2007; 21: 427-445Lisi A.J., Breuer P., Gallagher R.M., et al.
Deconstructing Chronic Low Back Pain in the Older Adult - Step by Step Evidence and Expert-Based
Recommendations for Evaluation and Treatment. Part II: Myofascial Pain
Pain Medicine 2015 (Jul); 16 (7): 1282–1289International Association for the Study of Pain. C
Spinal pain, section 1: spinal and radicular pain syndromes. (Available at:)
https://s3.amazonaws.com/rdcms-iasp/files/production/public/Content/ContentFolders/Publications2/
ClassificationofChronicPain/PART_I-C.pdf
Date accessed: November 5, 2018Neto T. Freitas S.R. Marques M. Gomes L. Andrade R. Oliveira R.
Effects of lower body quadrant neural mobilization in healthy and low back pain populations:
a systematic review and meta-analysis.
Musculoskelet Sci Pract. 2017; 27: 14-22Peterson C.K. Leemann S. Lechmann M. Pfirrmann C.W.A. Hodler J. Humphreys B.K.
Symptomatic magnetic resonance imaging-confirmed lumbar disk herniation patients:
a comparative effectiveness prospective observational study of 2 age- and sex-matched
cohorts treated with either high-velocity, low-amplitude spinal manipulative therapy
or imaging-guided lumbar nerve root injections.
J Manipulative Physiol Ther. 2013; 36: 218-225Katz J. Harris M.
Lumbar spinal stenosis.
N Engl J Med. 2008; 358: 818-825Ammendolia C. Chow N.
Clinical outcomes for neurogenic claudication using a multimodal program for
lumbar spinal stenosis: a retrospective study.
J Manipulative Physiol Ther. 2015; 38: 188-194Murphy DR, Hurwitz EL, Gregory AA, Clary R.
A Non-surgical Approach to the Management of Lumbar Spinal Stenosis:
A Prospective Observational Cohort Study
BMC Musculoskelet Disord. 2006 (Feb 23); 7: 16Ammendolia C. Côté P. Southerst D. et al.
Comprehensive nonsurgical treatment versus self-directed care to improve walking ability
in lumbar spinal stenosis: a randomized trial.
Arch Phys Med Rehabil. 2018; 99: 2408-2419.e2Fritz J.M., Rundell S.D., Dougherty P., et al.
Deconstructing Chronic Low Back Pain in the Older Adult - Step by Step Evidence and Expert-Based
Recommendations for Evaluation and Treatment. Part VI: Lumbar Spinal Stenosis
Pain Medicine 2016 (Mar); 17 (3): 501–510Puentedura E.J. Flynn T.
Combining manual therapy with pain neuroscience education in the treatment of chronic
low back pain: a narrative review of the literature.
Physiother Theory Pract. 2016; 32: 408-414Woods M.P. Asmundson G.J.G.
Evaluating the efficacy of graded in vivo exposure for the treatment of fear
in patients with chronic back pain: a randomized controlled clinical trial.
Pain. 2008; 136: 271-280Louw A. Zimney K. Puentedura E.J. Diener I.
The efficacy of pain neuroscience education on musculoskeletal pain: a systematic review of the literature.
Physiother Theory Pract. 2016; 32: 332-335Langevin H.M., Sherman K.J.
Pathophysiological Model for Chronic Low Back Pain Integrating Connective Tissue
and Nervous System Mechanisms
Medical Hypotheses 2007 (Jan); 68 (1): 74–80George S.Z. Bishop M.D. Bialosky J.E. Zeppieri G. Robinson M.E.
Immediate effects of spinal manipulation on thermal pain sensitivity: an experimental study.
BMC Musculoskelet Disord. 2006; 7: 68Bishop M.D. Beneciuk J.M. George S.Z.
Immediate reduction in temporal sensory summation after thoracic spinal manipulation.
Spine J. 2011; 11: 440-446Bialosky, J.E., Bishop, M.D., Robinson, M.E., Zeppieri, G. Jr, and George, S.Z.
Spinal Manipulative Therapy Has an Immediate Effect on Thermal Pain Sensitivity
in People With Low Back Pain: A Randomized Controlled Trial
Phys Ther. 2009 (Dec); 89 (12): 1292–1303Bialosky JE, George SZ, Horn ME, Price DD, Staud R, Robinson ME.
Spinal Manipulative Therapy-specific Changes in Pain Sensitivity in Individuals with Low Back Pain
Journal of Pain 2014 (Feb); 15 (2): 136–148Randoll C. Gagnon-Normandin V. Tessier J. et al.
The mechanism of back pain relief by spinal manipulation relies on decreased temporal summation of pain.
Neuroscience. 2017; 349: 220-228Penza C.W. Horn M.E. George S.Z. Bishop M.D.
Comparison of 2 lumbar manual therapies on temporal summation of pain in healthy volunteers.
J Pain. 2017; 18: 1397-1408López-de-Uralde-Villanueva I. Muñoz-García D. Gil-Martínez A. et al.
A systematic review and meta-analysis on the effectiveness of graded activity and graded exposure
for chronic nonspecific low back pain.
Pain Med. 2016; 17: 172-188Saragiotto B.T. Maher C.G. Yamato T.P. et al.
Motor control exercise for nonspecific low back pain: a Cochrane Review.
Spine (Phila Pa 1976). 2016; 41: 1284-1295Smith B.E. Littlewood C. May S.
An update of stabilisation exercises for low back pain: a systematic review with meta-analysis.
BMC Musculoskelet Disord. 2014; 15: 416Gordon R. Bloxham S.
A systematic review of the effects of exercise and physical activity on non-specific chronic low back pain.
Healthc (Basel). 2016; 4DiNapoli E.A., Craine M., Dougherty P., et al.
Deconstructing Chronic Low Back Pain in the Older Adult - Step by Step Evidence and Expert-Based
Recommendations for Evaluation and Treatment. Part V: Maladaptive Coping
Pain Medicine 2015 (Nov); 16 (11): 2098–2108Carley J.A., Karp J.F., Gentili A., et al.
Deconstructing Chronic Low Back Pain in the Older Adult - Step by Step Evidence and Expert-Based
Recommendations for Evaluation and Treatment. Part IV: Depression
Pain Med. 2015; 16: 2098-2108Weiner D.K. Fang M. Gentili A. et al.
Deconstructing Chronic Low Back Pain in the Older Adult - Step by Step Evidence and Expert-Based
Recommendations for Evaluation and Treatment. Part I: Hip Osteoarthritis
Pain Medicine 2015 (May); 16 (5): 886–897Nijs J. Malfliet A. Ickmans K. Baert I. Meeus M.
Treatment of central sensitization in patients with 'unexplained' chronic pain: an update.
Expert Opin Pharmacother. 2014; 15: 1671-1683Richmond H. Hall A.M. Copsey B. et al.
The effectiveness of cognitive behavioural treatment for non-specific low back pain:
a systematic review and meta-analysis.
PloS One. 2015; 10: e0134192Hughes L.S. Clark J. Colclough J.A. Dale E. McMillan D.
Acceptance and Commitment Therapy (ACT) for chronic pain: a systematic review and meta-analyses.
Clin J Pain. 2017; 33: 552-568Xia T. Long C.R. Gudavalli M.R. et al.
Similar effects of thrust and nonthrust spinal manipulation found in adults with subacute and chronic
low back pain: a controlled trial with adaptive allocation.
Spine (Phila Pa 1976). 2016; 41: 702-709Hadler N.M. Curtis P. Gillings D.B. Stinnett S.
A benefit of spinal manipulation as adjunctive therapy for acute low-back pain: a stratified controlled trial.
Spine (Phila Pa 1976). 1987; 12: 702-706Hondras MA, Long CR, Cao Y, et al.
A Randomized Controlled Trial Comparing 2 Types of Spinal Manipulation
and Minimal Conservative Medical Care for Adults 55 Years and Older
With Subacute or Chronic Low Back Pain
J Manipulative Physiol Ther. 2009 (Jun); 32 (5): 330–343Cook C. Learman K. Showalter C. Kabbaz V. O’Halloran B.
Early use of thrust manipulation versus non-thrust manipulation: a randomized clinical trial.
Man Ther. 2013; 18: 191-198Learman K.E. Showalter C. O’Halloran B. Cook C.E.
Thrust and nonthrust manipulation for older adults with low back pain: an evaluation of pain and disability.
J Manipulative Physiol Ther. 2013; 36: 284-291Coronado RA, Gay CW, Bialosky JE, Carnaby GD, Bishop MD, George SZ.
Changes in Pain Sensitivity Following Spinal Manipulation: A Systematic Review and Meta-analysis
J Electromyogr Kinesiol. 2012 (Oct); 22 (5): 752–767Boal R.W. Gillette R.G.
Central neuronal plasticity, low back pain and spinal manipulative therapy.
J Manipulative Physiol Ther. 2004; 27: 314-326Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ.
The Mechanisms of Manual Therapy in the Treatment of Musculoskeletal Pain: A Comprehensive Model
Man Ther. 2009 (Oct); 14 (5): 531–538Pickar JG.
Neurophysiological Effects of Spinal Manipulation
Spine J (N American Spine Society) 2002 (Sep); 2 (5): 357–371Fritz JM, Koppenhaver SL, Kawchuk GN, Teyhen DS, Hebert JJ, Childs JD.
Preliminary Investigation of the Mechanisms Underlying the Effects of Manipulation:
Exploration of a Multivariate Model Including Spinal Stiffness,
Multifidus Recruitment, and Clinical Findings
Spine (Phila Pa 1976). 2011 (Oct 1); 36 (21): 1772-1781Suter E. McMorland G.
Decrease in elbow flexor inhibition after cervical spine manipulation in patients with chronic neck pain.
Clin Biomech (Bristol, Avon). 2002; 17: 541-544Suter E. McMorland G. Herzog W. Bray R.
Decrease in quadriceps inhibition after sacroiliac joint manipulation in patients with anterior knee pain.
J Manipulative Physiol Ther. 1999; 22: 149-153Dishman J.D. Burke J.R. Dougherty P.
Motor neuron excitability attenuation as a sequel to lumbosacral manipulation in subacute low back pain
patients and asymptomatic adults: a cross-sectional H-reflex study.
J Manipulative Physiol Ther. 2018; 41: 363-371Nansel D.D. Waldorf T. Cooperstein R.
Effect of cervical spinal adjustments on lumbar paraspinal muscle tone:
evidence for facilitation of intersegmental tonic neck reflexes.
J Manipulative Physiol Ther. 1993; 16: 91-95DeVocht J.W. Pickar J.G. Wilder D.G.
Spinal manipulation alters electromyographic activity of paraspinal muscles: a descriptive study.
J Manipulative Physiol Ther. 2005; 28: 465-471Koppenhaver S.L. Fritz J.M. Hebert J.J. et al.
Association between changes in abdominal and lumbar multifidus muscle thickness and clinical
improvement after spinal manipulation.
J Orthop Sports Phys Ther. 2011; 41: 389-399Cramer, G, Henderson, C, Little, J, Daley, C, and Grieve, T.
Zygapophyseal Joint Adhesions After Induced Hypomobility
J Manipulative Physiol Ther. 2010 (Sep); 33 (7): 508–518Evans DW.
Mechanisms and Effects of Spinal High-velocity, Low-amplitude Thrust Manipulation:
Previous Theories
J Manipulative Physiol Ther 2002 (May); 25 (4): 251–262Taylor DN.
A Theoretical Basis for Maintenance Spinal Manipulative Therapy for the Chiropractic Profession
J Chiropractic Humanities 2011 (Dec); 18 (1): 74–85Engell S. Triano J.J. Fox J.R. Langevin H.M. Konofagou E.E.
Differential displacement of soft tissue layers from manual therapy loading.
Clin Biomech (Bristol, Avon). 2016; 33: 66-72Joseph M.F. Taft K. Moskwa M. Denegar C.R.
Deep friction massage to treat tendinopathy: a systematic review of a classic treatment
in the face of a new paradigm of understanding.
J Sport Rehabil. 2012; 21: 343-353Piper S. Shearer H.M. Côté P. et al.
The effectiveness of soft-tissue therapy for the management of musculoskeletal disorders
and injuries of the upper and lower extremities: a systematic review by the Ontario Protocol
for Traffic Injury management (OPTIMa) collaboration.
Man Ther. 2016; 21: 18-34Stecco A. Stern R. Fantoni I. De Caro R.
Stecco C. Fascial disorders: implications for treatment.
PM R. 2016; 8: 161-168Ellis R.F. Hing W.A.
Neural mobilization: a systematic review of randomized controlled trials with an
analysis of therapeutic efficacy.
J Man Manip Ther. 2008; 16: 8-22Greening J. Leary R.
Re: improving application of neurodynamic (neural tension) and treatments:
a message to researchers and clinicians.
Man Ther. 2007; 12 (author reply e3-6): e2Nijs J. Clark J. Malfliet A. et al.
In the spine or in the brain? Recent advances in pain neuroscience applied in the intervention
for low back pain.
Clin Exp Rheumatol. 2017; 35 Suppl 107: 108-115Pelletier R. Higgins J. Bourbonnais D.
Addressing neuroplastic changes in distributed areas of the nervous system associated with
chronic musculoskeletal disorders.
Phys Ther. 2015; 95: 1582-1591Huang Z. Ma J. Chen J. Shen B. Pei F. Kraus V.B.
The effectiveness of low-level laser therapy for nonspecific chronic low back pain:
a systematic review and meta-analysis.
Arthritis Res Ther. 2015; 17: 360National Board of Chiropractic Examiners; 2014.
Practice analysis of chiropractic 2015Haldeman S, Dagenais S.
A Supermarket Approach to the Evidence-informed Management of Chronic Low Back Pain
Spine Journal 2008 (Jan); 8 (1): 1–7U.S. Department of Veterans Affairs
Whole health for life. VA patient centered care. (Available at:)
https://www.va.gov/patientcenteredcare/
Date accessed: November 5, 2018
Return to LOW BACK PAIN
Return to LOW BACK GUIDELINES
Return to CLINICAL PREDICTION RULE
Return NON-PHARMACOLOGIC THERAPY
Return to CHIROPRACTIC CARE FOR VETERANS
Since 3-26-2020


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |
