

Chiropractic Manipulation in
Adolescent Idiopathic Scoliosis:
A Pilot StudyThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Chiropractic & Osteopathy 2006 (Aug 21); 14: 15 ~ FULL TEXT
OPEN ACCESS Dale E Rowe, Ronald J Feise, Edward R Crowther, Jaroslaw P Grod, J Michael Menke, Charles H Goldsmit, Michael R Stoline, Thomas A Souza, and Brandon Kambach
Kalamazoo Center of Medical Studies,
Michigan State University,
1000 Oakland Drive,
Kalamazoo, Michigan, USABackground: Adolescent idiopathic scoliosis (AIS) remains the most common deforming orthopedic condition in children. Increasingly, both adults and children are seeking complementary and alternative therapy, including chiropractic treatment, for a wide variety of health concerns. The scientific evidence supporting the use chiropractic intervention is inadequate. The purpose of this study was to conduct a pilot study and explore issues of safety, patient recruitment and compliance, treatment standardization, sham treatment refinement, inter-professional cooperation, quality assurance, and outcome measure selection.
Methods: Six patients participated in this 6-month study, 5 of whom were female. One female was braced. The mean age of these patients was 14 years, and the mean Cobb angle was 22.2 degrees. The study design was a randomized controlled clinical trial with two independent and blinded observers. Three patients were treated by standard medical care (observation or brace treatment), two were treated with standard medical care plus chiropractic manipulation, and one was treated with standard medical care plus sham manipulation. The primary outcome measure was Cobb, and the psychosocial measure was Scoliosis Quality of Life Index.
Results: Orthopedic surgeons and chiropractors were easily recruited and worked cooperatively throughout the trial. Patient recruitment and compliance was good. Chiropractic treatments were safely employed, and research protocols were successful.
Conclusion: Overall, our pilot study showed the viability for a larger randomized trial. This pilot confirms the strength of existing protocols with amendments for use in a full randomized controlled trial.
From the Full-Text Article:
Background
Adolescent idiopathic scoliosis (AIS) remains the most common deforming orthopedic condition in children. [1, 2] It is manifested as a spinal curvature presenting at or about puberty which in its most aggressive form leads to progressive spinal curvature and vertebral rotation. In children it is associated with increased pain, reduced function and poor self-image. [3, 4] In adults it is associated with increased back pain, poor quality of life and self-reported disability. [5] Estimates of prevalence of mild curvature, those varying from five to twenty degrees, is thought to be between 1 to 3% of adolescents with a male to female ratio of 1:2. [6, 7] In moderate to severe curves requiring medical management, the prevalence varies between .03 and .09% [711], with a male to female ratio of 1:7. [10, 12]
Usual and customary medical management includes observation in early stages, bracing between 20 to 40 degrees curve progression, and surgical intervention for curves greater than 40 degrees. [13] Although bracing and surgery provide benefit, neither is free of shortfalls [1416]. Bracing effectiveness is compromised by poor compliance [16], and surgical intervention is associated with negative side-effects (implant failure, wound infections and increased morbidity) [14, 15]. These findings (both benefit and side-effects) are mostly based upon observational designed studies without controls [1416].
Increasingly, adults [17, 18] and children [19] are seeking complementary and alternative therapy, including chiropractic treatment, for a wide variety of health concerns. Approximately 2.7 million patient visits are made to American chiropractors each year for scoliosis and scoliosis-related complaints [20]. Chiropractors are using manipulation and other chiropractic approaches with these patients based largely on historical and anecdotal information, and without any scientific evidence.
A large scale, multi-disciplinary, collaborative clinical trial is needed to explore the effectiveness of chiropractic manipulation of patients with AIS. But prior to conducting such a trial, we needed to perform a pilot randomized controlled trial to explore issues of safety, patient recruitment and compliance, treatment standardization, sham treatment refinement, inter-professional cooperation, quality assurance, outcome measure selection and statistical analysis.
Methods
Design
The study design is a randomized controlled clinical trial with two independent and blinded observers. Two strata were studied: an unbraced group and a braced group. Each stratum had patients treated by standard medical care (observation or brace treatment), standard medical care plus chiropractic manipulation, or standard medical care plus sham manipulation. Patient blinding was attempted in the manipulation and sham manipulation interventions only.
Sample specification
The target population was children aged 1016 years who had been diagnosed (via x-ray) with AIS curves ranging from 20 to 30 degrees, and those with curves varying from 30 to 40 degrees who were undergoing bracing treatment. Study participants were recruited from the pediatric orthopedic clinic at The Kalamazoo Center for Medical Studies. Potential patients were screened using patient clinic records for inclusion and exclusion criteria. Those that met the study's criteria were invited to participate.
Inclusion criteria
Children aged 1016 years
Diagnosis of Adolescent Idiopathic Scoliosis
Spinal curvature on P/A radiographs of between 20 and 30 degrees measured by the Cobb method in non-braced individuals and 30 to 40 degrees in braced individuals
Palpatory evidence of subluxation (manipulative lesion) on chiropractic screening examination
Signed informed consent by parent/guardian
Signed child assent form
Availability for follow-up evaluation Exclusion criteria
Age <10 or >16 years
Diagnosis other than AIS following clinical, radiographic and advanced imaging assessment
Contraindications to manipulation: inflammatory arthritides, osteomyelitis, neoplasm, metabolic disturbances affecting the integrity of bone structure, fracture/dislocation/spinal instability, blood clotting disorders and connective tissue disorders
Congenital or acquired structural spinal abnormalities
Leg length inequality >3/8 inch (measured via x-ray)
Pregnancy
Pain as a primary clinical feature
Mental incapacitation
Previous back surgery
Significant recent trauma
Obesity impairing ability to manipulate
The Institutional Review Board of Borgess Medical Center, Kalamazoo approved the study protocol. Patients and their parents/guardians were informed and signed consent forms (parents/guardians) and assent forms (study participants) prior to participation. Following consent, further screening procedures and baseline data were gathered, including health history, physical exam (vital signs), neurological exam (deep tendon reflex, sensory deficit testing, muscle strength testing, Babinski), chiropractic spinal exam (static palpation, motion palpation, postural assessment), biomechanical evaluation (Shobers' modified-modified technique, Adams test, thoracic range of motion), quality-of-life self-report (Scoliosis Quality of Life Index, general health) and plain film radiographs. Patient recruitment occurred between March and July of 2003.
"Costs per randomization" were calculated by dividing the recruitment costs (the personnel time necessary to screen and recruit potential patients) by the number of randomizations. This information allowed assessment of future full-scale trial recruitment costs.
Allocation
Prior to the start of the study, a computer-generated randomization schedule was prepared. Eligible patients were randomly assigned to 1 of 3 treatment groups (standard medical care, standard medical care plus chiropractic manipulation, or standard medical care plus sham manipulation). The allocation ratio was 1:1:1. Neither the participants nor the investigators knew whether a particular participant had been assigned to a study group or to a control group (standard medical care or standard medical care plus sham manipulation) until after assignment. The clinical research assistant e-mailed a member of the randomization team (off site) regarding the need for an assignment for a "qualified" participant by providing the clinic numeric code and bracing status. A member of the randomization team then provided the random assignment by return e-mail to the clinical research assistant.
Study participants randomized to the simulated and real treatment groups were given their choice of participating chiropractic treatment clinics. Once a clinic had been selected for attendance and treatment, the subject remained with that clinic for the duration of the trial. The treating chiropractor was provided with radiographs and Cobb angle measures for each study participant.
Study sites
Participating treating chiropractors were recruited from Kalamazoo and Battle Creek, Michigan. Five chiropractic treatment centers were credentialed for the study and all used Diversified Technique as their primary method of treatment. Diversified technique is a widely used chiropractic manipulative technique that entails a high velocity, low-amplitude thrust.
Treating chiropractors were trained, tested and certified in study protocols and treatment methods. Three training sessions (approximately 2 hours each) were held at the medical center with the treating chiropractors, orthopedic surgeons and research staff. Each treating chiropractor was provided with a packet of training materials prior to the sessions. The first session focused on the study's research design and protocols and presented background information on adolescent idiopathic scoliosis. The second training session included an explanation of a standardized approach for detecting dysfunctional vertebrae, adjusting procedures and sham adjusting procedures. The final training session included a review of the study research design and protocols, standardized approach for detecting dysfunctional vertebras, adjusting procedures and sham adjusting techniques. During the last hour of the session, participants were evaluated using the Objective Structured Clinical Examination [21, 22].
Upon entry to a participating chiropractic clinic, each subject underwent a standardized consultation, history and physical examination, including a chiropractic assessment. The patient and his or her parent/guardian were given a report of findings, a standardized explanation of chiropractic principles related to scoliosis, and an outline of the treatment schedule and procedures to be performed. On subsequent visits, pre-treatment analysis, treatment, post-treatment analysis and adverse reaction were recorded on standardized study treatment sheets. The treating chiropractors followed a scripted interview for each patient visit.
Interventions
Usual and customary medical care for AIS patients with a Cobb of 20 to 25 degrees consists of careful observation (e.g., physical and radiographic examination twice a year). Patients with curves between 26 and 40 degrees are potential candidates for bracing with physical and radiographic examination twice a year, and patients beyond 40 degrees are potential candidates for surgery [23]. All groups received usual and customary medical care, including follow-up examination and x-ray at 6 months.
Active chiropractic treatment for this study consisted of prone, side posture and supine adjustments in conjunction with manual soft tissue therapy to the overlying tissues. Treatment consisted of the full spine chiropractic manipulation technique known as The Diversified Technique [24, 25]. Because this was intended to be a pragmatic study within the domains of adjustive and soft tissue therapies, the specifics of the treatment (i.e. vertebral segments, direction of manipulation and use of soft tissue therapy) were left to the discretion of the treating practitioner.
Sham (pretend) chiropractic treatment consisted of a standardized approach which mimics regular chiropractic treatment, but which does not have the same mechanical effect. Subjects were placed prone on the treatment table and the spine was palpated lightly in a posterior-anterior direction. In this prone position, the head was rotated first to the right, then to the left, and held for a few moments while the chiropractor palpated the ankles and feet (a distraction maneuver). Following this distraction, the patient was positioned in a side-lying posture, and positioned for a low back adjustment (superior leg and hip flexed) without joint slack taken up. This position was held for a few moments, and the chiropractor contacted the soft tissues overlying the gluteal region and administered a light (non-therapeutic) impulse. This was repeated on the opposite side. The patient was then placed prone on the table, and the chiropractor administered a light impulse bilaterally to the muscles overlying the scapulae. The subject was then positioned supine, and the neck was palpated gently. Following this, the head was rotated to the side and held for a few moments, followed by a light impulse on the cranium over the external occipital protuberance.
Schedule of visits
The schedule of treatment represents the frequency and duration of treatment typically used by the chiropractic profession. To form an estimate for the frequency and duration of care, a pre-study survey was administered to a random sample of American chiropractors (90% response rate) assessing treatment dosage for chiropractic management of AIS [26]. Generally, treatment consisted of three treatments per week for the first month, two treatments per week for the second month, one treatment per week for the third and fourth months, followed by a maintenance program of two treatments per month for the fifth and sixth months. Our treatment protocol was chosen based on the results of the survey of the American chiropractors [26]. For this effectiveness study, treating practitioners were allowed to increase or decrease the frequency of care, depending on clinical presentation (i.e. pain, postural changes, and changes evident on assessment). Patient compliance was deemed adequate when a patient received between 80% and 120% of the above-described treatments.
Data collection and statistical analysis
All patients followed the same algorithmic protocols for initial evaluation and follow-up review. We collected data on radiographs, demographics, clinical history and quality-of-life domains at entry. Radiographs and quality-of-life measures were evaluated at baseline and at 6 months.
Cobb is the primary outcome measure for this study and is the gold standard for the measurement of curve magnitude in scoliosis [2729]. Endorsed by the Scoliosis Research Society, measurement of the Cobb angle on full spine serial radiographs is used to make clinical decisions regarding initiation, termination and success of treatment. The reliability of the Cobb angle measure has been evaluated in many studies. When strict measurement protocols are used, consisting of sharpening marking instruments, standardizing protractors, and standardizing end plate selection, examiner error can be minimized [30]. In this study, strict measurement protocols were used and intra- and inter-examiner reliability was measured using two independent orthopedic surgeons blinded to treatment allocation.
Because there is a clinically important increase of curve severity (5 degrees) in moderate idiopathic scoliosis between morning and evening, the comparative x-rays were taken at approximately the same time of day (+one hour) as the entry x-ray [31]. Additionally, braced patients were required to remove their brace 6 hours prior to radiographic examination [32].
Quality of life is important in AIS because of the psychosocial stresses experienced by these patients. As a secondary outcome measure, we used Scoliosis Quality of Life Index (SQLI). This measure is a 22 item self-reporting health-related quality-of-life questionnaire for patients 10 to 18 years of age with idiopathic scoliosis [33]. SQLI is reliable (test-retest ICC 2,1; 0.80), valid (construct validity with Quality of Life Profile for Spine Deformities, Spearman's rho; 0.79) and demonstrates satisfactory distribution of scores. SQLI has five domains: physical activity performance (the presence and extent of physical limitations); back pain (the intensity and frequency of back pain); self-esteem (social confidence, self-regard, self-appearance, overall life assessment); moods and feelings (anxiety, depression and positive affect); and satisfaction with management. All scales are scored from zero (most pain, worst function, etc.) to 100 (no pain, best function, etc.). A global scale for SQLI (scored 0 to 100) was calculated by averaging the scores of all the scales.
Patient expectations about the therapeutic benefit of the treatment were assessed before randomization [34]. Allowing only naive patients is problematic, because it may be difficult to recruit this population. Furthermore, an expectation for or against chiropractic could influence patient scores on subjective measures. If patient preference is disproportionately distributed among the groups, there may be an inflated threat of obtaining a skewed outcome [35]. Patients for this study were asked to describe their expectations for improvement of their spinal condition (without regard to treatment) using a 5point scale with choices varying from "very much improved," to "very much worsened." The patients then rated how helpful they believed chiropractic would be for their current spinal problems using a 5point scale with choices varying from "very helpful" to "very unhelpful".
To provide proof of blinding for patients in the real and sham manipulation groups, patients were questioned after all therapy had been administered about whether they received active or inactive therapy. A 7point scale was used with choices varying from "definitely real therapy," to "definitely pretend therapy." We also asked patients about co-interventions and contamination during the study period.
Touch screen technology (TST) was used to administer SQLI and expectation, blinding, co-Intervention and contamination questions. The quality of the data collected with the touch-screen system has been reported as good, with no missed responses [36, 37]. This method eliminates possible entry errors and the need for double-entry checks. Additionally, it is well accepted by patients, the majority of whom find all aspects of the TST system easy to use [38].
Quality assurance procedures were established and implemented for all aspects of the trial. We developed a manual of operational procedures which included operational definitions of recruitment, measurement procedures, etc. All forms were standardized (pre-coded, self explanatory, easy to read, coherent, pretested, and labeled on every page with an ID number).
Simple descriptive analyses were used to report the findings. Outcome measures were not aggregated, but were reported individually because of insufficient sample size and the high risk of committing sampling errors. To assess intra- and inter-reliability, intraclass correlation coefficients (ICC 2,1) were calculated for the Cobb measures [39]. All data were entered into a spreadsheet and analyzed with Minitab 12 (State College, PA). All data were checked for accuracy.
Results

Table 1 Baseline characteristics of the subjects are presented in Table 1. These patients reported no comorbidities, recent accidental injuries, previous chiropractic treatment or significant pain associated with their scoliosis. Self report of general health using a question from the SF-36 scale was rated as either "very good" or "good" for these participants, and all thought chiropractic treatment could be somewhat helpful to their condition. Patients' expectations for future improvement of their spinal condition was rated as "very much improved" by one patient, "somewhat improved" by two patients, and "neither" by three patients.

Table 2 Table 2 describes AIS radiograph assessment categories. Riser sign describes bone maturity (0 = immature to 5 = mature) [40], and Nash-Moe classification describes vertebral body rotation (0 is not rotated, 3 is fifty percent rotated) [41]. The Lenke classification system consists of 3 components: Lenke curve type (the curve types have specific characteristics that differentiate structural and nonstructural curves in the proximal thoracic, main thoracic, and thoracolumbar-lumbar regions), the lumbar spine modifier (based on the relation of the center sacral vertical line to the apex of the lumbar curve) and the sagital thoracic modifier (differentiates the degree of Cobb Angle; T5T12 Cobb Angle from 10 to 40 degrees is N and above is "+") [42]. Inter-rater reliability, estimated as percent of agreement for the scoliosis classifications (Risser, Nash-Moe, Lenke curve type, Lenke spine modifier, and Lenke sagittal thoracics modifier), varied between 0.72 and 0.92.

Table 3 Table 3 demonstrates the findings of the Cobb Angle pre- and post-testing. Every patient had more than one curve that was measured at baseline and at follow-up. The intra-examiner reliability intraclass correlation coefficients (ICC 2,1) for Cobb measurement scores were 0.96 and 0.98 with inter-examiner at 0.96. (SEM 0.69 and SD 1.38). Although, there is no gold standard for declaring the failure or success of progression for Cobb, Rowe recommended 10 degrees from start of treatment, and Nachemson used 6 degrees or more on two consecutive radiographs [16, 32]. We tested two discriminatory points by establishing benchmarks at 6 degrees and 10 degrees. Failure was deemed as a progression of at least 6 degrees or at least 10 degrees, and success was deemed as curve improvement of at least 6 degrees or at least 10 degrees. For the 6 degree benchmark, the standard medical care group had no curves that achieved success and one curve that was rated as a failure; the standard medical care plus sham manipulation patient had both curves rated as failures; and the standard medical care plus chiropractic manipulation group had no curves that achieved failure and one curve that was rated as a success.
For the 10 degree benchmark, the standard medical care group had no curves that achieved success or failure; the standard medical care plus sham manipulation patient had one curve rated as failure; and the standard medical care plus chiropractic manipulation group had no curves that achieved failure and one curve that was rated as a success. Chiropractic manipulation was delivered on 52 visits and resulted in two benign reactions. One reaction with a moderate amount of pain lasted for 24 hours; the other produced mild pain lasting 6 hours. Neither reaction reduced the normal activities of the patients. All patients meet the established compliance standards. The patient in the sham group thought she probably had real treatment. Whereas, the chiropractic treatment patients thought their treatment was definitely real or possibly real.

Table 4 Table 4 documents the findings from measuring quality of life domains before and after the intervention period. An absolute change in score of more than 15 points is considered minimum clinically important for either the sub-scales or global score [33]. The standard medical care group had one patient whose scores in the domains of self-esteem, back pain, physical activity, moods and feelings and the global score expressed a clinically important deterioration. This patient was compliant with the study protocols, including follow-up x-ray, but underwent surgical therapy. The quality of life measure was not administered until after surgery The standard medical care plus sham manipulation patient expressed no clinically important changes from baseline. The standard medical care plus chiropractic manipulation group had one patient who reported a clinically important improvement in the moods and feelings domain and the global score.
Health provider recruitment
We easily recruited both orthopedic surgeons and chiropractors for this study. Treating chiropractors were in practice a mean of 11.6 years (min. 2.5 years to max. 30 years). In an exit survey, orthopedic surgeons and chiropractors rated cooperation between groups above 9, with 10 representing "extremely cooperative" and 0 "not cooperative." Treating chiropractors rated our training program at 9, with 10 representing "extremely effective" and 0 "not effective." The treating chiropractors felt no burden to their practice during this study, and all would participate in a full study. The treating chiropractors, orthopedic surgeons and research team rated the overall experience of the study at 8, with 10 representing an "outstanding experience" and 0 a "horrible experience."
Protocol compliance
Observation by the research team found no breach in standardized chiropractic treatment. An exit survey of patients, treating chiropractors, research staff and orthopedic surgeons found one patient with a co-intervention. That patient, from the standard medical care group, underwent a surgical intervention. This study suffered from one protocol failure: the sham patient received 34 visits (8 visits more than the ideal of 26 visits), but this did not exceed our compliance upper limit of 38 visits. Our exit meeting of treating chiropractors, orthopedic surgeons and research team produced strategies to improve the protocols, data collection, patient recruitment and chiropractic practitioner training process for the full study.
Patient recruitment
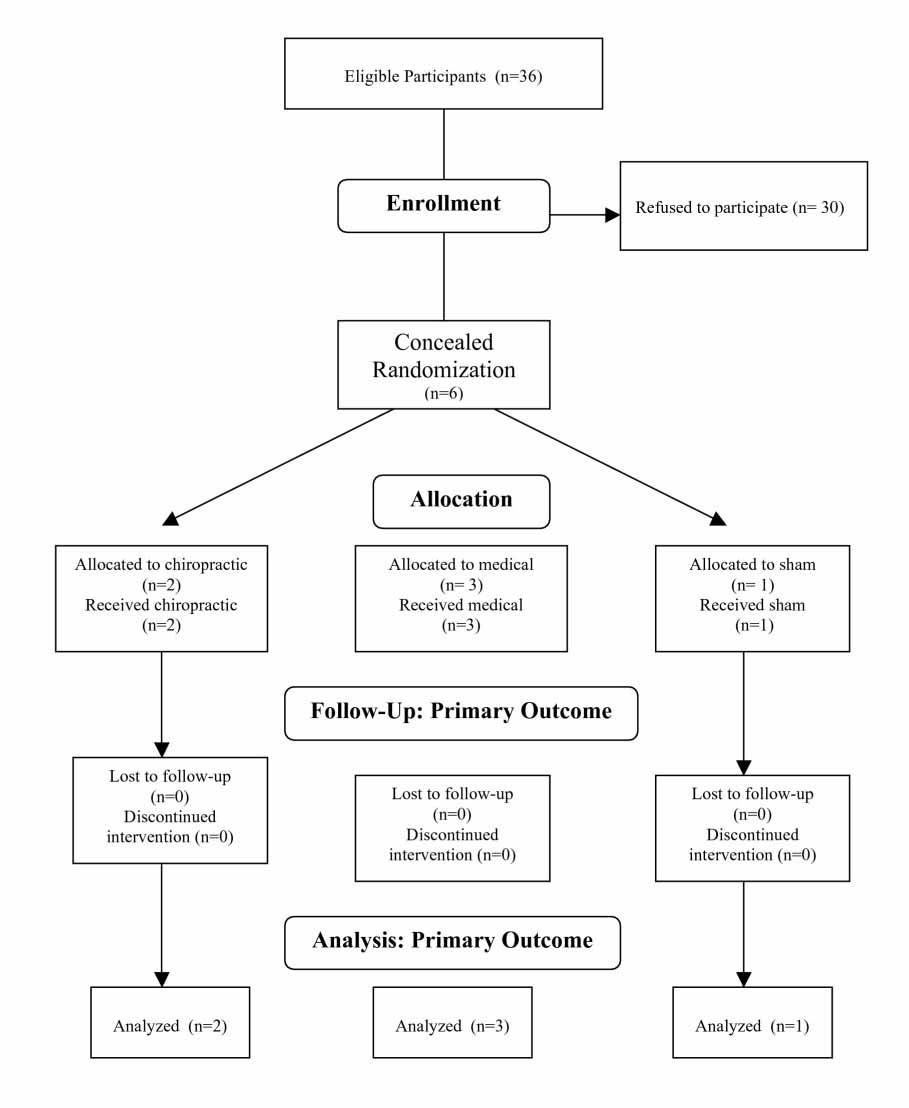
This study had an enrolment rate of 17% (36 patients were eligible, and 6 patients were randomized). Of the 30 patients who qualified but refused to participate, 12 said they did not have enough time, 8 gave no reason, and the remainder had a variety of reasons (transportation, not interested in participating, family issues). All randomized patients accepted assignment (figure 1). Costs for randomization were calculated at $360/randomization (the total cost of personnel time necessary to screen and recruit potential patients was $2,176; US Dollars 2003).
Figure 1. Flow of Participants.
Discussion
Detailed reviews by Harrison et al [3537] and Rhee et al [14] suggest that preserving a normal sagittal spinal contour may be important for long-term health. De Jonge et al [15] described how correction of lateral scoliotic curvatures caused a spontaneous restoration of the sagittal spinal curves, suggesting that loss of sagittal spinal curves may somehow be related to scoliotic curvatures. Scoliosis places otherwise symmetrical muscle groups under longstanding, isometric, asymmetrical loads [3841], which may compromise circulation within the muscle, ultimately leading to myofascial trigger points and chronic inflammation [42]. Weinstein et al [3] reported that scoliosis patients may retain high levels of function in later life, but do report higher instances of chronic back pain.
In addition to higher instances of chronic back pain, significant psychological issues may arise from concern over cosmesis and conventional treatment. Freidel et al [43] measured the self-perceived quality of life in women with scoliosis using the SF-36 questionnaire. They concluded that the psychosocial aspects of scoliosis and scoliosis treatment should be addressed in the treatment of this group of patients. Similarly, Sapountzi-Krepia et al [44] described the psychological distress that adolescents encounter while going through bracing treatment for scoliosis. A case-control study by Danielsson et al [45] identified a potential negative impact on the ability to function sexually due to conventional treatment restraint or self-consciousness of physical appearance. Aside from back pain and psychological disturbance, several studies also suggest that scoliosis affects more than the musculoskeletal system. Curvatures of the thoracic spine are associated with restrictive lung disease due to ribcage deformity and decreased chest wall compliance [46]. Chest wall compliance is inversely proportional to the magnitude of the Cobb angle down to 10°, and vital capacity is reduced by decreased chest wall compliance directly [46, 47]. Exercise endurance is also inversely diminished with increasing Cobb angle, even in patients with normal resting vital capacity [48]. Thoracic scoliosis may also cause shortness of breath and recurrent respiratory infections [46, 49]. Indeed, scoliosis affects more than the musculoskeletal system.
Concerning coronal Cobb angle measurement for scoliosis, manual radiographic measurement has consistently shown good to excellent inter- and intra-observer reliability [5053]. Previous studies demonstrate a manual Cobb angle measurement error on full-spine radiographs of 2.5 4.5° [5153]. However, to achieve this low error, it is imperative that the same end vertebrae, same protractor, and same endplates are consistently chosen. Importantly, these measurement errors were extracted from data collected on full-spine radiographs. Patient positioning can significantly negatively impact measurements on fullspine radiographs [17]. The Cobb angle measurements in our study were taken from sectional radiographs, which reduce the positional distortion caused by inconsistent patient positioning. It is unknown to what extent the use of sectional radiography has on Cobb angle measurement error, if any.
The treatments outlined here required home care exercises, as described earlier. However, these exercises, which take up a combined 60 minutes per day, can be done in private, away from scrutiny by peers, neighbors, or relatives. This is in contrast to bracing treatment, where the brace must be worn at least 18 hours per day to achieve a good clinical result [54].
We placed the headweight, shoulderweight, and hipweights in areas designed to reduce our patient's specific spinal distortion patterns on radiograph. The patient was evaluated radiographically while wearing the headweight and shoulderweights to determine optimal position and weight. Our repeated clinical observation has demonstrated that patients may visually appear to improve with a shoulderweight in a certain position. However, they can look dramatically different on radiograph (migration away from the vertical axis) than they appear in visual posture analysis. This is consistent with recent failed attempts to objectify visual posture analysis as a valid clinical tool [55]. It is prudent to develop alternative methods of evaluation to avoid unnecessary radiation exposure to patients.
Because of the anterior wedging from T7T10 in case #2, it is not surprising that over time a thoracic hyperkyphosis and swayback developed in this patient. As a result, marked anterior weight bearing of the head was required to maintain a horizontal eye level, thus satisfying the postural reflexes [5661] Additionally, the marked forward head posture elicits the pelvo-ocular reflex, causing a forward shift of the pelvic girdle under the forward head position [32]. Therefore, the postural distortions seen in this case may represent compensatory changes over time as a result of thoracic buckling, a posture known to commonly cause increased mechanical stress at the spinal transition areas [4, 24]. Correcting these compensatory postural changes proved to be a challenge, given that the impetus for them (the anteriorly wedged thoracic vertebra) could not be immediately, if ever, changed. However, within the confines of the Hueter-Volkmann law, we postulate that sustained correction of the asymmetrical mechanical spinal loading may theoretically help these vertebrae to remodel to some degree. Although the forward head posture is a compensatory reaction to the hyperkyphosis, the cervical spine soft tissue has likely remodeled to the forward head posture, given the likely duration of its existence [62]. Therefore, we felt that direct correction of the forward head posture must also be achieved to improve overall sagittal alignment, given the neurological control and importance of head position on upright spinal position [63]. This hypothesis remains to be definitively evaluated.
The significance of cases #2 and #3 lies in the location of the scoliotic curvatures. In the vast majority of cases, double major curvatures usually maintain a right thoracic/left lumbar pattern. In this case, the pattern was reversed, showing a left thoracic/right lumbar scoliosis. Several authors have previously discussed the unique presence of a left thoracic right lumbar curvature pattern. McCarver et al [64] showed that only 1% of 550 patients with idiopathic scoliosis had double major curvatures consisting of a left thoracic right lumbar configuration. Winter and Lonstein [65] maintained that any left thoracic curvature should be further evaluated for neurological abnormalities, such as neurofibromatosis, spina bifida, or syringomyelia. Finally, Schwend et al [66] also concluded that additional testing was necessary in left thoracic curvatures, given an observed higher incidence of neurological clinical signs. Case #3 seems to correlate these findings given the left thoracic scoliosis secondary to Scheuermann's Disease. It is important to note, however, that treating the Scheuermann's Disease itself was not our aim. Rather, our goal was to reduce the thoracic scoliosis secondary to it. We are not attempting to show that this treatment may affect the Scheuermann's Disease. In this case, however, additional testing was conducted at the initial time of discovery of the scoliosis. Further, my initial neurological examination also failed to produce any remarkable neurological findings.
Recently, several authors have discussed the relationship between the sagittal spinal contour and scoliosis [14, 15, 67, 68]. Harrison et al [3537] have discussed the pathophysiologic changes associated with the loss of the sagittal curves. Based on this evidence, we decided that it was important to the long-term outcome to address these spinal parameters.
Cases #1 and #2 present what appears to be inconsistent findings. Case #1 initially had a 23° cervical lordosis, below asymptomatic 3140° range identified by McAviney et al [30], and the normal 34° identified by Harrison et al [28]. However, case #2 displayed a 32° initial cervical lordosis despite having a thoracic hyperkyphosis. In case #1, the patient had 31 mm of forward head posture. Since forward head posture reduces the magnitude of the cervical lordosis [69, 70], a 23° cervical lordosis may not be normal for this patient. Additionally, recent evidence suggests that sagittal balance may more closely correlate to symptoms than sagittal alignment [71] Cervical lordosis by itself may not provide an accurate assessment of normal for each patient. Therefore, we suggest that both the cervical lordosis and forward head posture be weighed before a patient's cervical spine may be considered "normal." In contrast, case #2 had a both a normal cervical lordosis and forward head posture (32° and 22 mm, respectively). Therefore, we classified this patient's cervical spine as normal, despite the thoracic hyperkyphosis. We feel that the 55° lumbar hyperlordosis is a direct compensation for the swayback posture created by the thoracolumbar vertebral remodeling. This is consistent with the post treatment reductions in the swayback posture and lumbar lordosis.
In the Pettibon system, most of the manipulative treatment is not administered on a vertebral segmental basis. Rather, it is delivered to a specific region of segments so that the entire region may be mobilized. The goal of manipulative therapy in the Pettibon system is to mobilize several vertebral joints so that the rehab procedures can target the joints while they temporarily have an increased range of motion [33]. The purpose of the Pettibon Weighting System is to artificially alter the centers of mass of the head, trunk, and pelvis, causing reactive corrections by the postural reflexes [7274]. The goal of postural reflexes is to maintain efficient body stance and locomotion using the least energy expenditure possible [56, 63, 75]. In the present cases, each patient was instructed to continue with their home exercise routine on a once weekly basis in attempts to maintain the change in spinal configuration.
The procedures that comprise the Pettibon system have been previously examined in specific clinical cases [5, 76]. Although these techniques have been investigated for preliminary treatment of idiopathic scoliosis [5], they have not, until this point, been used in cases of scoliosis due to structural deformity or left thoracic primary curvatures. Given the perceived results of the cases outlined here, it is worthy of future investigations in such cases. However, case reports and case series designs do not provide substantive evidence of therapeutic effectiveness. This remains the realm of properly conducted prospective clinical trials.
Conservative treatment for scoliosis needs to be examined much more closely in the biomedical literature, as side effects [4446] and compliance issues [54] make conventional treatments such as bracing less attractive to patients and parents of minor patients.
Conclusion
In this case series, we reported the clinical results for 3 distinct types of scoliosis patients. While no firm conclusions relative to cause and effect can be made from these results, the moderation of the spinal curves may have merit. Although reductions in self-rated disability and pain scores were reported, they may not be attributable to the improvement in spinal alignment. Further investigation is required to determine the potential benefits of sagittal spine alignment in the correction of scoliosis and other health benefits.
References:
Dickson RA:
Spinal deformity-adolescent idiopathic scoliosis: nonoperative treatment.
Spine 1999, 24:2601-2606Kelsey J:
Epidemiology of musculoskeletal disorders.
New York: Oxford University Press; 1982Caillet R:
Scoliosis: Diagnosis and management.
Philadelphia: FA Davis; 1975Goldberg MS, Mayo NE, Poitras B, Scott S, Hanley J:
The Ste-Justine Adolescent Idiopathic Scoliosis Cohort Study: part 1: description of the study.
Spine 1994, 19:1551-1561Goldberg MS, Mayo NE, Poitras B, Scott S, Hanley J:
The Ste-Justine Adolescent Idiopathic Scoliosis Cohort Study. Part II: Perception of health, self and body image, and participation in physical activities.
Spine 1994, 19:1562-1572Leaver J, Alvik A, Warren M:
Presciptive screening for adolescent idiopathic scoliosis.
Int J Epidemiol 1982, 11:101-111Moe JH, Winter RB, Bradford DS, Lonstein JE:
Scoliosis and other spinal deformities.
Philadelphia: WB Saunders; 1978Brooks H, Azen S, Gerberg E, Chan L:
Scoliosis: a prospective epidemiological study.
J Bone Joint Surg 1975, 57A:968-972Drennan J, Campbell J, Ridge H:
Denver: a metropolitan public school scoliosis survey.
Pediatrics 1977, 60:193-196Robitaille Y, Villavicencio-Pereda C, Gurr J:
Adolescent idiopathic scoliosis: epidemiology and treatment outcome in a large cohort of children six years after screening.
Int J Epidemiol 1984, 13:319-323Rogala EJ, Drummond DS, Gurr J:
Scoliosis: incidence and natural history. A prospective epidemiological study.
J Bone Joint Surg Am 1978, 60:173-176Morais T, Bernier M, Turcotte F:
Age and sex-specific prevalence of scoliosis and the value of school screening programs.
Am J Public health 1985, 75:1377-1380Lonstein JE:
Scoliosis: surgical versus nonsurgical treatment.
Clin Orthop Relat Res 2006, 443:248-59Bradford DS, Tay BK-B, Hu SS:
Adult scoliosis: surgical indications, operative management, complications and outcomes.
Spine 1999, 24:2617-2628Poitras B, Mayo NE, Goldberg MS, Scott S, Hanley J:
The Ste-Justine adolescent idiopathic scoliosis cohort study. Part IV: Surgical correction and back pain.
Spine 1994, 19:1582-1588Rowe D, Bernstein SM, Riddick MF, Adler F, Emans JB, Gardner-Bonneau :
A meta-analysis of the efficacy of non-operative treatments for idiopathic scoliosis.
J Bone Joint Surg 1997, 79-A:664-674Eisenberg DM, Kessler RC, Foster C:
Unconventional Medicine in the United States: Prevalence, Costs, and Patterns of Use
New England Journal of Medicine 1993 (Jan 28); 328 (4): 246252Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, Kessler RC.
Trends in Alternative Medicine Use in the United States, 1990 to 1997:
Results of a Follow-up National Survey
JAMA 1998 (Nov 11); 280 (18): 15691575Spigelblatt L, Laine-Ammara G, Pless B, Guyver A:
The use of alternative medicine in children.
Pediatrics 1994, 94:811-814Christensen MG, Kerkhoff D, Kollasch MW:
Job Analysis of Chiropractic, 2000
Greeley, Colorado: National Board of Chiropractic Examiners; 2000Stillman P, Swanson D, Regan MB, Philbin MM, Nelson V, Ebert T, Ley B, Parrino T, Shorey J, Stillman A, et al.:
Assessment of clinical skills of residents utilizing standardized patients: a follow-up study and recommendations for application.
Ann Intern Med 1991, 114:393-401Pertusa ER, Blackwell TA, Ainswatch MA:
Reliability and validity of an objective structured clinical examination for assessing the clinical performance of residents.
Arch Intern Med 1990, 150:573-577Reamy BV, Slakey JB:
Adolescent idiopathic scoliosis: review and current concepts.
Am Fam Physician 2001, 64:111-116Gitelman R, Fligg B:
Diversified technique. In Principles and Practice of Chiropractic. 2nd edition.
Edited by Haldeman S. Norwalk, CT: Appleton and Lange; 1992
Szaraz ZT:
Compendium of Chiropractic Techniques.
Toronto, ON: Canadian Memorial Chiropractic College Press; 1990Feise RJ:
An inquiry into chiropractors' intention to treat adolescent idiopathic scoliosis: a telephone survey.
J Manipulative Physiol Ther 2001, 24:177-182Asher M, Lai SM, Burton D, Manna B:
The influence of spine and trunk deformity on preoperative idiopathic scoliosis patients' health-related quality of life questionnaire responses.
Spine 2004, 29:861-868Cobb JR:
Outline for the study of Scoliosis. In Instructional Course Lectures,
The Am Academy of Orthopaedic Surgeons.
Ann Arbor, MI: JW Edwards; 1948Haher TR, Merola A, Zipnick RI, Gorup J, Mannor D, Orchowski J:
Meta-analysis of surgical outcome in adolescent idiopathic scoliosis. A 35-year English literature review of 11,000 patients.
Spine 1995, 20:1575-1584Mior S, Kopansky DR, Crowther ER, Wright JG:
A comparison of radiographic and electrogoniometric angles in adolescent idiopathic scoliosis.
Spine 1996, 21:1541-1555Beauchamp M, Labelle H, Grimard G, Stanciu C, Poitras B, Dansereau J:
Diurnal variation of Cobb angle measurement in adolescent idiopathic scoliosis.
Spine 1993, 18:1581-1583Nachemson AL, Peterson LE:
Effectiveness of treatment with a brace in girls who have adolescent idiopathic scoliosis.
A prospective, controlled study based on data from the Brace Study of the Scoliosis Research Society.
J Bone Joint Surg Am 1995, 77:815-822Feise RJ, Donaldson S, Crowther T, Menke JM, Wright JG:
Construction and Validation of the Scoliosis Quality of Life Index in Non-Surgical Adolescent Idiopathic Scoliosis.
Spine 2005, 30:1310-5Kalauokalani D, Cherkin DC, Sherman KJ, Koepsell TD, Deyo RA:
Lessons from a trial of acupuncture and massage for low back pain: patient expectations and treatment effects.
Spine 2001, 26:1418-1424van der Windt DA, Koes BW, van Aarst M, Heemskerk MA, Bouter LM:
Practical aspects of conducting a pragmatic randomised trial in primary care: patient recruitment and outcome assessment.
Br J Gen Pract 2000, 50:371-374Gostel R:
HyperCard to SPSS: improving data integrity.
Comput Nurs 1993, 11:25-28Velikova G, Wright EP, Smith AB, Cull A, Gould A, Forman D, Perren T, Stead M, Brown J, Selby PJ:
Automated collection of quality-of-life data: a comparison of paper and computer touch-screen questionnaires.
J Clin Oncol 1999, 17:998-1007Buxton J, White M, Osoba D:
Patients' experiences using a computerized program with a touch-sensitive video monitor for the assessment of health-related quality of life.
Qual Life Res 1998, 7:513-519Portney LG, Watkins MP:
Foundations of clinical research: application to practice.
East Norwalk, CT: Appleton and Lange; 1993.Urbaniak JR, Schaefer WW, Stalling FH III:
Iliac apophyses: prognostic value in idiopathic scoliosis.
Clin Orthop 1976, 116:80-85Nash CL, Moe JH:
A study of vertebral rotation.
J Bone Joint Surg Am 1969, 51:223-229Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, Blanke K:
Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis.
J Bone Joint Surg Am 2001, 83:1169-81Bronfort G, Evans R, Nelson B, Aker P, Goldsmith C, Vernon H:
A Randomized Clinical Trial of Exercise and Spinal Manipulation
for Patients with Chronic Neck Pain
Spine (Phila Pa 1976) 2001 (Apr 1); 26 (7): 788797Cambron J:
Recruitment and accrual of women in a randomized controlled trial of spinal manipulation.
J Manipulative Physiol Ther 2001, 24:79-83Cambron JA, Hawk C, Evans R, Long CR:
Recruitment and accrual of women in a placebo-controlled clinical pilot study on manual therapy.
J Manipulative Physiol Ther 2004, 27:299-305Gudavalli MR, Backman-Cambron JA, Jedlicka J, McGregor M, Ardickas Z, Benge K:
Flexion-distraction (chiropractic) vs. conservative medical care for chronic low back pain: progress-to-date, challenges, and lessons.
Proceedings of the International Conference on Spinal Manipulation: 2000; Bloomington, Minnesota 2000Hawk C, Long CR:
Use of a pilot to refine the design of a study to develop a manual placebo treatment.
JNMS 2000, 8:39-48Miller FG, Emanuel EJ, Rosenstein DL, Straus SE:
Ethical issues concerning research in complementary and alternative medicine.
JAMA 2004, 291:599-604Balon J, et al.
A Comparison of Active and Simulated Chiropractic Manipulation as Adjunctive Treatment
for Childhood Asthma
New England Journal of Medicine 1998; 339(15): 1013-1020
Return to the SCOLIOSIS
Since 9-26-2006


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |