

The Mechanisms of Manual Therapy: A Living Review
of Systematic, Narrative, and Scoping ReviewsThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: PLoS One 2025 (Mar 18); 20 (3): e0319586 ~ FULL TEXT
OPEN ACCESS Damian L Keter • Joel E Bialosky • Kevin Brochetti • Carol A Courtney
Martha Funabashi • Steve Karas • Kenneth Learman • Chad E Cook
Physical Medicine and Rehabilitation Department,
United States Department of Veterans Affairs,
Cleveland, Ohio, United States of America.
Introduction: Treatment mechanisms are the underlying process or pathway through which a treatment influences the body. This includes molecular, cellular and physiological processes or pathways contributing to treatment effect. Manual therapy (MT) evokes complex mechanistic responses across body systems, interacting with the individual patient and context to promote a treatment response. Challenges arise as mechanistic studies are spread across multiple professions, settings and populations. The purpose of this review is to summarize treatment mechanisms that have been reported to occur with MT application.
Methods: Four electronic databases were searched (Medline, CINAHL, Cochrane Library, and PEDro) for reviews investigating mechanistic responses which occur during/post application of MT. This review was registered a priori with PROSPERO (CRD42023444839). Methodological quality (AMSTAR-2) and risk of bias (ROBIS) were assessed for systematic and scoping reviews. Data were synthesized by mechanistic domain.
Results: Sixty-two reviews were included. Systematic reviews (n = 35), narrative reviews (n = 24), and scoping reviews (n = 4) of asymptomatic (n = 37), symptomatic (n = 43), non-specified human subjects (n = 7) and animals (n = 7) were included. Reviews of moderate quality supported neurovascular, neurological, and neurotransmitter/neuropeptide changes. Reviews of low quality supported neuroimmunce, neuromuscular, and neuroendocrine changes. Reviews of critically low quality support biomechanical changes.
Conclusions: Findings support critically low to moderate quality evidence of complex multisystem mechanistic responses occurring with the application of MT. Results support peripheral, segmental spinal, and supraspinal mechanisms occurring with the application of MT, which can be measured directly or indirectly. The clinical value of these findings has not been well established. While MT has proven to be an effective intervention to treat conditions such as pain, the current body of literature leaves uncertainty as to 'why' MT interventions work, and future research should look to better define which mechanisms (or combinations of mechanisms) are mediators of clinical response.
From the FULL TEXT Article:
Introduction
Manual Therapy (MT) is a type of force-based manipulation which has been defined as “passive application of mechanical force to the outside of the body with therapeutic intent, often as part of pain management care (e.g., low-back pain), rehabilitation care, or general wellness and disease prevention”. [1] Techniques associated with MT include soft tissue mobilization (STM), joint mobilization (non-thrust), and manipulation (thrust). These techniques are used by healthcare professionals such as osteopaths, massage therapists, chiropractors, and physical therapists (PT). Whereas historical models of MT attributed the clinical effect to biomechanical changes within tissues directly related to the technique applied [2, 3], recent evidence-based models support more complex interactive mechanistic responses across body systems, interacting with the individual patient and context to promote a treatment response. [4–6]
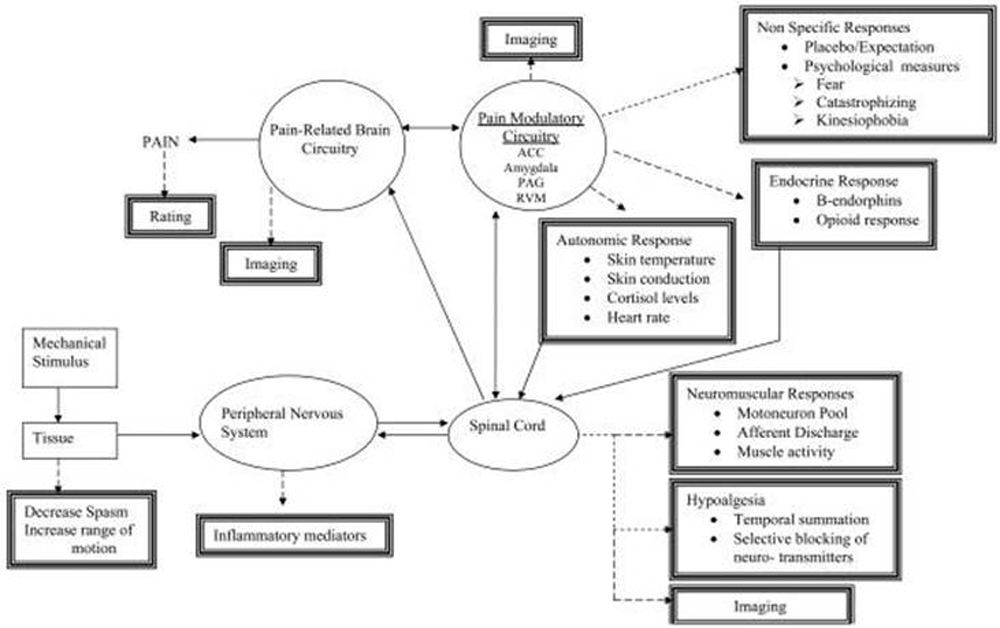
Mechanisms are “the molecular, cellular, physiological processes or pathways contributing to a) disease development, b) treatment action, or c) pain signal sensation, transmission, perception, and modulation”. [7] Treatment mechanisms are “the underlying process or pathway through which a specific treatment produces an influence on the body”. [7] Potential treatment mechanisms associated with MT include: biomechanical (altered tissue movement, fluid loading, etc.), neurological (fMRI activation, altered neural conduction, etc.), neuroimmune (release of inflammatory and anti-inflammatory mediators, etc.), neurovascular (sympathetic response, etc.), neurotransmitter and neuropeptide (release of serotonin, beta endorphin, etc.), neuromuscular (altered neuromuscular tone, muscle recruitment), neuroendocrine (release of cortisol etc.) and other mechanisms. [8]
Mechanisms are processes that can be measured in a number of different ways. Measurements can be direct or indirect. Higher level (cortical and subcortical) changes typically represent initial efferent activity (direct measure), while measurements of downstream effects represent indirect or proxy measures of the process (e.g., skin conductance as a proxy measure of ANS response, fMRI as proxy measure of cortical activation, neuroimmune markers as proxy measures of multisystem subcortical activation, somatosensory reflexes as a measure of spinal excitability, etc.) rather than direct/primary measures (e.g., EEG as a measure of cortical activity, MRI as a measure of joint position, etc.). [9] Defined mechanistic domains and proposed direct and indirect measures within these domains are presented in S1 Appendix. Studies investigating treatment mechanisms associated with MT are of interest as recent National Institute of Health (NIH) funding has been designated to better understand the mechanisms associated with the application of force during MT. [1]
MT techniques have demonstrated efficacy/effectiveness in improving range of motion, reducing disability, improving function and modulating pain. [10–12] Based on these findings, the use of selected MT techniques are commonly cited in high-level clinical practice guidelines as recommended interventions for various conditions. [13–17] Despite this endorsement, variability exists in the strength of recommendations, [18, 19] suggesting an inconclusive body of literature. Furthermore, reported treatment effect sizes for MT are small to moderate [20], which is likely due to individual variability in treatment response [21] when provided with a one-size-fits-all treatment approach. [22] Mechanistic-based treatment stratification represents a potential approach to match patients to treatments and improve outcomes. [21, 23, 24] Such an approach allows the matching of an intervention of known mechanisms to patients with underlying conditions responsive to these mechanisms. [25] Clarifying the mechanisms through which MT inhibits musculoskeletal pain could improve the effectiveness in clinical practice by better informing a mechanistic approach to identifying individuals who will respond positively to these interventions. Despite progress in this area of study the mechanisms underpinning the demonstrated effectiveness of MT remains unclear due to two notable limitations:
Mechanism-based studies are spread across multiple professions and settings including lab-based and clinical-based designs, animal and human models, and asymptomatic and symptomatic specimens.
Mechanism-based studies often lack translation of causality between treatment mechanisms and clinical outcomes (translational studies).
A recent interprofessional panel reached a consensus on current gaps that are present in mechanistic research [8]; however, the literature involves multiple physiological systems, often explored heterogeneously, making it challenging to interpret and summarize. The purpose of this review of reviews was to identify and summarize the neurological, neuroimmune, biomechanical, neurovascular, neurotransmitter/neuropeptide, neuroendocrine, and other not previously categorized treatment mechanism systems that have been reported to occur with MT application. Reviews of reviews play a crucial role in synthesizing and evaluating existing research, providing a comprehensive perspective on a specific topic or question therefore aiding both researchers and clinicians to make sense of a vast complex topic. [26]
Methods
Protocol and registration
A review of systematic, scoping, and narrative reviews was performed to assess and summarize the mechanisms associated with MT application. To encompass new evidence as it becomes available, a living review building off the findings of this study will be hosted digitally at the Duke Center for Excellence in Manual and Manipulative Therapy (CEMMT). This study was registered with PROSPERO on September 03, 2023, prior to the initial literature search (CRD42023444839).
Eligibility criteria
Systematic reviews, scoping reviews, and narrative reviews with or without meta-analyses were included. Reviews including MT techniques within the scope of Physical Therapy (PT) practice were included (mobilization (non-thrust), manipulation (thrust), STM/massage, light touch). Manual techniques controlled or performed by external, non-human forces were excluded except for instrument-assisted STM in which a human provider was manually controlling a device to assist in external tissue mobilization. Internal (invasive) STM techniques such as dry needling and acupuncture were excluded. Outcomes (mechanisms) required for inclusion were neurological, neuroimmune, biomechanical, neurovascular, neurotransmitter, neuroendocrine, and other non-aforementioned mechanisms associated with MT application. In vivo models including living human and animal subjects were included. In-vitro models and cadaveric studies were excluded as the treatment mechanisms are assumed to differ in these models. Comparators included control, sham, or other MT procedures. Reviews were excluded if they did not include an outlined literature search strategy.
Information sources
Four electronic databases were searched including: Medline, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Library, and Physiotherapy Evidence Database (PEDro). Reviews published from inception to October 3, 2023 were included in initial search. An updated search was performed September 23, 2024 to include reviews published through that date. The search strategy for each of the included databases was validated by a Health Sciences librarian and uploaded to PROSPERO prior to the search. The comprehensive search strategy is available in S2 Appendix.
Data selection
Two review authors performed title (DK, KB), abstract (DK, MF), and full text (DK, KB) screenings independently. Discrepancies between reviewers were resolved by a third review author (CC, KB). Microsoft Excel (Microsoft Corporation; version 2205–2211) was utilized to manage and organize the search results throughout the review process. Cohen’s Kappa Scores (95% CI) were calculated to assess agreement between reviewers.
Data extraction
Data were extracted using a self-developed tool to extract appropriate variables. The following items were extracted: author, year, type of review, database(s) searched, number of included studies, mechanistic domain, MT intervention, comparator, outcome and results/conclusion. Data were extracted independently by two review authors (DK, KB) with all discrepancies discussed and agreed upon by the two authors.
Methodological quality appraisal
Methodological quality for each included systematic and scoping review was performed using the AMSTAR-2 quality assessment measure. [27] Risk of Bias was assessed using the ROBIS tool. [28] Two review authors independently performed quality appraisal (KL, CC) and risk of bias assessment (SK, JB) with discrepancies resolved by a third review author (DK). Quality assessment and risk of bias was not assessed for narrative reviews.
Data synthesis
Studies were grouped by mechanistic domains (S1 Appendix) outlined in previous work [8] with mechanisms outside of those domains categorized within an ‘other’ category. No synthesized quality or GRADE was used given the focus on mechanistic outcomes rather than clinical effectiveness.
Data analysis
No analysis of data occurred. The goals of this review were to outline and summarize the status of the available literature.
Results
Selection of sources of evidence

Figure 1
Page 5The search identified 442 reviews after duplicate removal. After title and abstract screening, 173 full-text reviews were agreed to be assessed for eligibility. Cohens Kappa coefficients to assess agreement between reviewers demonstrated moderate to strong agreement for title (k = .77; 95% CI .69–.84) abstract (k = .83; 95% CI .78–.89), and full text (k = .98; 95% CI .94–.99) screening. Sixty-two reviews were agreed upon to be included in this review of reviews. A flowchart representing the process for evidence selection including rationale for full texts which were screened and excluded is presented in Figure 1. Detailed rationale for full texts which were screened and excluded are presented in S3 Appendix.
Study characteristics
Included reviews weresystematic reviews (n = 35),
narrative reviews (n = 24), and
scoping reviews (n = 4).Databases searched within these reviews included CINAHL (n = 35), Cochrane (n = 27), PubMed/Medline (n = 61), PEDro (n = 17), SCOPUS (n = 10), and EMBASE (n = 19). Forty-five of the included reviews also included other search strategies (e.g., searching references of included studies, consulting experts in the field) and databases (PsycINFO, AMED, MANTIS, Google Scholar, Elsevier, Science Direct, Web of Science, Index of Chiropractic Literature, SciELO, etc.).
Subjects includedasymptomatic humans (n = 37),
symptomatic humans (n = 43),
human subjects without specifications regarding status (n = 7) and
animal models (n = 6).MT techniques included
manipulation (n = 41),
mobilization (n = 23), and
STM or massage (n = 19).Reviews included studies
comparing MT to sham intervention (n = 37),
comparing MT to control (no intervention) (n = 45), and
14 reviews that did not specify a comparator.Treatment mechanisms from
the biomechanical domain (n = 14),
neurovascular domain (n = 32),
neurological domain (n = 23),
neurotransmitter/neuropeptide domain (n = 16),
neuroimmune domain (n = 12),
neuroendocrine domain (n = 11),
neuromuscular domain (n = 10), and
other domains (n = 7) were identified (Figure 2).Characteristics of the included reviews are presented in Table 1 with more detailed extracted data presented in S4 Appendix. Reported treatment mechanisms across the aforementioned domains are presented in Tables 2–11.
Quality assessment and risk of bias

Figure 2
Page 6

Tables 2–12
Page 7–22Thirty-nine reviews were appropriate for quality and risk of bias appraisal. The included reviews were primarily of critically low (n = 23) to low-quality (n = 12) with the exception of four reviews of moderate quality. Overall quality of the included reviews is presented in Table 12 with itemized scoring presented in S5 Appendix. Fourteen reviews were rated at high risk of bias and twenty-five rated as low risk of bias. Overall risk of bias of the included reviews is presented in Table 12 with itemized scoring presented in S6 Appendix.
Biomechanical mechanisms
Fourteen reviews of critically low quality reported biomechanical treatment mechanisms associated with MT. (Table 2) Five reviews reported changes in joint position associated with MT techniques. [42, 61, 70, 83, 89] One of these reviews reported no correlation between joint changes and improvement in pain or impairment. [83] Two reviews questioned the concept of joint position changes with MT, most specifically at the cervical spine. [52, 61] Five reviews supported physiological changes in soft tissue associated with MT (such as viscoelastic properties). [43, 50, 58, 62, 89] Four reviews reported changes in disc characteristics following MT techniques (e.g., intradiscal pressure). [45, 58, 65, 89] All four reviews supported increased disc diffusion with two of these studies supporting translational association with improved clinical outcomes. [45, 65]
Neurovascular mechanisms
Thirty-two studies of critically low to moderate quality reported neurovascular mechanisms associated with MT. (Table 3) Twelve of the included reviews favored sympathoexcitation across outcome measures. [30,34,36,54, 60, 61, 71, 73, 76, 77, 83, 86] One review favored sympathoexcitation if the MT technique was noxious and sympathoinhibition if the technique was non-noxious. [78] A decrease in alpha-amylase levels, a proposed measure of Autonomic Nervous System (ANS) function, was reported across 3/3 reviews, indicating a sympathoinhibitory effect of MT. [51, 69, 88] Increased skin conductance was reported in 12 reviews following MT intervention. [30, 33, 36, 51, 60, 67, 69, 71, 73, 77, 86, 90] No change in skin temperature was reported in 14 reviews post MT intervention. [30, 33, 36, 51, 54, 60, 67, 69, 71, 73, 77, 78, 86, 90] One review, however, reported inverse responses related to both skin conductance and skin temperature in individuals with LBP [90] while other symptomatic populations did not demonstrate the same effect. Heart rate, heart rate variability and blood pressure demonstrated a change of variable direction without a clear rationale for variations.
Neurological mechanisms
Twenty-three reviews of critically low to moderate quality reported neurological treatment mechanisms associated with MT. Twenty reviews investigated changes in pain threshold following MT application (Table 4). Increases in local pressure pain threshold (PPT) versus control and sham were demonstrated in 12 reviews. [39, 46, 55, 58, 61, 62, 64, 71, 76, 77, 82, 85] Two reported no difference in effect between mobilization and manipulation [40, 55], one reported larger PPT increase in the manipulation group [82] and one reported mixed results. [72]
Two reviews reported no difference in PPT between MT and active PT management. [46, 55] Several reviews reported the remote effect of MT on PPT with general support for an increase in PPT however not consistent across reviews. Four reviews reported no effect of MT on thermal pain threshold (TPT). [64, 77, 83]
Seven reviews reported other neurological mechanisms (Table 5), including changes in EEG activity [56, 63, 68, 81], nerve characteristics [62], and cerebral blood flow. [62, 63]
Improved conditioned pain modulation (CPM) and reduced temporal summation (TS) were supported by 1 review. [31]
Neurotransmitter/neuropeptide mechanisms
Sixteen reviews of critically low to moderate quality reported neurotransmitter and/or neuropeptide treatment mechanisms associated with MT. (Table 6) Increase in oxytocin levels post MT application was reported in 4 reviews [43, 49, 74, 84] with the exception of 1 review reporting increased levels with STM and decreased levels with manipulation. [84] Substance P was included in 5 reviews with 3 reviews on spinal manipulation favoring an increase, 1 review on mobilizations favoring a decrease, and 1 review on spinal manipulation favoring no change. [33, 35, 49, 62, 74] Increased β-endorphin was reported in 5 reviews following MT application versus control, however less consistent results and less significant changes when compared with sham intervention. [33, 40, 54, 71, 84] Little to no change in Norepinephrine (NE) and Epinephrine (Epi) levels with MT were reported in 7 reviews based on low quality evidence. [30, 35, 49, 69, 74, 75, 84]
Neuroimmune mechanisms
Twelve reviews of critically low to low quality reported neuroimmune treatment mechanisms associated with MT. (Table 7) General support was demonstrated for changes in cytokine levels with MT application. Trends towards a decrease in pro-inflammatory cytokines (IL-1β, TNF-α) and an increase in anti-inflammatory cytokines (IL-2, IL-10) were seen across reviews with some variability. This was supported across symptomatic and asymptomatic populations and was more significant with MT application than control and sham interventions. Other immune markers including leukocytes, [62, 81, 88] natural killer cells [43, 53], Immunoglobin (Ig)-A [81], Ig-G [33, 35], and Ig-M [33, 35] also demonstrated modulation with MT intervention.
Neuroendocrine mechanisms
Twelve reviews of critically low to low quality reported neuroendocrine treatment mechanisms associated with MT. (Table 8) All reviews investigated changes in cortisol levels with general support for modulation of variable direction and effect sizes. Little to no difference from sham and control was reported in 5 reviews [32, 33, 66, 68, 81], larger response in MT groups reported in two reviews [35, 74], and longer carryover of effects with MT vs control was reported in one review. [32]
Neuromuscular mechanisms
Ten reviews of critically low to low quality reported neuromuscular mechanisms associated with MT. (Table 9) Lima et al. assessed muscle activity during mobilization and manipulation and reported changes in muscle spindle afferent discharge, which demonstrated variability based on targeted segment and thrust velocity. [62] Post treatment responses across included reviews support increased maximum voluntary contraction [41, 56, 71], reduced EMG activity [62, 70, 71, 77, and reduced muscle interference during contraction. [52, 56, 58, 70]
Other mechanisms
Six reviews of critically low quality included treatment mechanisms outside of the previous domains. (Table 10) Three studies investigated cardiopulmonary responses to MT. Results suggested increased forced vital capacity, forced expiratory volume, and O2 saturation without supporting changes in VO2 Max, total lung capacity, blood lactate levels, or other reported measures of cardiopulmonary function. [33, 41, 68] Other reviews reported on changes in gene expression [62], intestinal function [62], mitochondrial function [62, 81] and enzyme, protein and amino acid profiles. [56, 62, 81]
Discussion
Findings from this review support complex multisystem biomechanical, neurovascular, neurological, neurotransmitter/neuropeptide, neuroimmune, neuroendocrine, neuromuscular, and other mechanistic responses occurring with the application of MT. The overall quality of evidence supporting these responses was critically low to moderate, therefore these results should be interpreted with caution. Furthermore, care should be taken in assuming translation to clinical relevance as these processes are influenced by a multitude of intrinsic and extrinsic factors and are likely to demonstrate variability between individuals.
Some included reviews attempted to establish clinical relevance, including Jun et al. [58], which reported correlation between being a positive responder to spinal manipulation, and improved multifidi recruitment post technique application; however, non-investigated translation to clinical outcomes should not be assumed. For example, neuroimmune treatment mechanisms favor an increase in anti-inflammatory mediators and decrease in inflammatory mediators. These changes are not unique to MT [38] and the relevance of these changes to immune system status was questioned in several of the included reviews [35, 49] and furthermore by the chiropractic community in a recent statement paper. [91]
Overall, the current review supports peripheral, segmental spinal, and supraspinal neurological mechanisms occurring with the application of MT, which can be measured directly or indirectly. MT has been shown to attenuate nociceptive spinal excitability. [92] This alteration in neural excitability as well as changes in tissue sensitivity as measured via PPT are theorized to occur due to facilitation of descending inhibitory mechanisms. [93] Previous animal model research [94] demonstrated that joint-based MT likely induces analgesia via non-opioidergic inhibitory pathways, that include noradrenergic and serotonergic mechanisms in the central nervous system. Changes in tissue sensitivity may also be related to changes in functional connectivity involving the PAG. [95] One included review [46] reported that 11 studies reported correlation between hypoalgesia and clinical pain reduction; however, the degree to which changes in quantitative sensory testing translate to clinical outcomes has demonstrated question [96–98], likely due to poor baseline assessment of which aberrant neurophysiological mechanisms are present within the study participant group. Descending regulatory mechanisms have also been proposed to influence neuroimmune [99, 100], neuroendocrine [101], neurovascular [101], and neuromuscular responses. [102] The crosstalk between mechanisms further complicates research within this field, as discussed in a recent review on neuroimmune mechanisms associated with MT. [38]
While historic models of MT promote assessment and treatment based on biomechanical principles, the overwhelming majority of mechanisms studied suggest stronger support for neurological changes than biomechanical. These findings agree with several recent reviews suggesting non-specific analgesic effects associated with MT. [103, 104] Several recent publications have emphasized the need for updated training paradigms and modernized practice patterns to accommodate what is currently known and unknown regarding these complex mechanistic responses. [12, 105–108]
This review summarizes treatment mechanisms associated with MT application supporting complex multisystem responses; however, care must be taken in interpreting these findings due to two distinct realizations:
Treatment mechanisms that occur are unlikely to be unique to a specific MT intervention. It is unclear based on the results of this review which mechanisms are specific to MT versus those which are related to the fact that ‘an intervention’ was applied. This can be seen with the significant reduction in effect size across several treatment mechanisms when compared to other active controls and sham techniques. Recent work has cited the importance of better understanding the specific and shared mechanisms associated with MT. [109]
Treatment mechanisms that occur are unlikely to be consistent across different populations. Contextual factors such as patient factors, provider factors, and environmental factors have been shown to influence mechanistic response to MT forces and therefore should be considered when investigating and interpreting mechanistic responses to MT. While contextual factors have been solidified as a critical component of mechanistic response, two recent studies obtained consensus on gaps within this field specifically related to MT treatment mechanisms. [110, 111]
Clinical implications
Clinicians using MT interventions should appreciate that multisystem mechanisms occur beyond the local tissue to which MT is targeted. While not reasonable to assess these mechanisms clinically in real time, understanding the complex interactions across systems regulating processes such as immune function, cardiovascular function, and neuroendocrine function are important factors to consider. Many of the included reviews looked at these mechanistic responses in isolation and clinicians should appreciate the complex interaction between these systems producing the observed response which they see clinically are the sum of these mechanisms with interaction from contextual variables.
Research implications
High quality primary and secondary research within this area of study is needed to further investigate changes in the mechanistic domains outlined within this review. Researchers should address identified gaps within MT mechanisms research. [110, 111] Collaboration between clinical researchers and basic scientists should be leveraged to establish translational value of these mechanisms to clinical outcomes, assess contextual factor influence on both mechanistic and clinical response, and determine if there are pain phenotypes which provide different mechanistic and clinical responses. Research should be focused on symptomatic patient populations to promote relevance of findings. Furthermore, emphasis should be placed on study designs effective in establishing causation such as those which have been proposed in previous work. [6]
Limitations
Several limitations are present which must be considered in interpreting the findings of this review. Although reporting of different MT techniques occurred, this review did not attempt to differentiate between treatment mechanisms for different MT techniques (STM, manipulation, mobilization). Several of the included reviews did report on these findings in their results. Significant heterogeneity was present between the included reviews related to type of MT technique, type of mechanistic measure, and subjects. Several of the included reviews were not in English which required translation, therefore language barriers may have been a limitation during screening, quality assessment, risk of bias assessment, and data extraction. Furthermore, this review included narrative reviews which are less structured and transparent than systematic/scoping reviews allowing increased potential for bias. These reviews were included to broaden the investigated mechanisms and the results demonstrated beneficial information extracted from these reviews which would have otherwise been excluded. Inclusion criteria were used (search strategy outlined in review) in an attempt to include more transparent narrative reviews.
Summary
This review supports multisystem mechanistic responses with the application of hands-on intervention across the biomechanical, neurological, neurovascular, neuroendocrine, neurotransmitter/neuropeptide, and neuromuscular domains. The clinical value of these mechanistic responses has not been well established. Clinicians should appreciate the uncertainty related to ‘why’ these interventions work and future research should look to better define which mechanisms (or combinations of mechanisms) are mediators of clinical response.
Statement on living review
With permission from the publisher, results from this living review will be housed at the Duke Center for Excellence in Manual and Manipulative Therapy (CEMMT) website at https://sites.duke.edu/cemmt/. Results will be updated every 6 months to include newly published research. Please reach out to the corresponding author with any potential reviews which may meet the inclusion criteria to be included on the next revision.
Supplementary Material
S1 Appendix. Definition of mechanisms table.
S2 Appendix. Search strategy.
S3 Appendix. Excluded Full texts
S4 Appendix. Extracted data.
S5 Appendix. Quality scores (AMSTAR-2).
S6 Appendix. Risk of bias scores (ROBIS).
S1 Checklist. PRISMA 2020 Checklist.Acknowledgments
We the authors would like to thank Colleen Duchon, Health Sciences Librarian at Youngstown State University for validation of search strategy. We would also like to thank Dr. Weiqing Ge and Dr. Jean-Michel Brismée for assistance with article translation.
References
National Institutes of Health (NIH).
In: Neural Mechanisms of Force-Based Manipulations:
High Priority Research Networks [Internet]. 2 Feb 2023.
Available: https://grants.nih.gov/grants/guide/rfa-files/RFA-AT-21-006.html#
:~:text=Force-based%20manipulations%20refer%20to%20the%20passive%20
application%20of,rehabilitation%20care%2C%20or%20general%20
wellness%20and%20disease%20preventionCook C.
The demonization of manual therapy.
MSK – Muskuloskelettale Physiotherapie. 2021;25:125–32.Pettman E.
A history of manipulative therapy.
J Man Manip Ther. 2007;15(3):165–74. pmid:19066664Bialosky JE, Beneciuk JM, Bishop MD, Coronado RA, Penza CW, Simon CB, et al.
Unraveling the mechanisms of manual therapy: modeling an approach.
J Orthop Sports Phys Ther. 2018;48(1):8–18. pmid:29034802Courtney C, Fernández de las Peñas C.
Manual Therapy for Chronic Conditions:
A Mechanistic Approach to Modern Manual Therapy.
In: Simoneau G, editor. Mechanisms of Manual Therapy Interventions.
Lacrosse, WI: Academy of Orthopaedic Physical Therapy. APTA; 2021. p. 5–18.Damian K, Chad C, Kenneth L, David G.
Time to evolve: the applicability of pain phenotyping in manual therapy.
J Man Manip Ther. 2022;30(2):61–7. pmid:35344468Cook C, Abraira V, Burns J, Degenhardt B, Kawchuk G, Keter D, et al.
Categorizing treatment mechanisms for complementary
and integrative musculoskeletal interventions.
Int J Osteopath Med. 2024.Keter D, Bent J, Bialosky J, Courtney C, Esteves J, Funabashi M.
An International Consensus on Gaps In Mechanisms
of Forced-based Manipulation Research: Findings
From a Nominal Group Technique.
J Man Manip Ther 2024 (Feb); 32 (1): 111–117Lok JJ.
Defining and estimating causal direct and indirect effects when setting
the mediator to specific values is not feasible.
Stat Med. 2016;35(22):4008–20. pmid:27229743Cross KM, Kuenze C, Grindstaff TL, Hertel J.
Thoracic spine thrust manipulation improves pain, range of motion,
and self-reported function in patients with mechanical neck pain:
a systematic review.
J Orthop Sports Phys Ther. 2011;41(9):633–42. pmid:21885904Nim CG, Weber KA, Kawchuk GN, O’Neill S.
Spinal manipulation and modulation of pain sensitivity in persistent
low back pain: a secondary cluster analysis of a randomized trial.
Chiropr Man Therap. 2021;29(1):10. pmid:33627163Grenier J-P, Rothmund M.
A critical review of the role of manual therapy in the
treatment of individuals with low back pain.
J Man Manip Ther. 2024;32(5):464–77. pmid:38381584Bier JD, Scholten-Peeters WGM, Staal JB, Pool J, van Tulder MW, et al.
Clinical Practice Guideline for Physical Therapy Assessment
and Treatment in Patients With Nonspecific Neck Pain.
Phys Ther. 2018;98(3):162–71. pmid:29228289George SZ, Fritz JM, Silfies SP, Schneider MJ, Beneciuk JM, Lentz TA, et al.
Interventions for the management of acute and chronic
low back pain: revision 2021.
J Orthop Sports Phys Ther. 2021;51(11):CPG1–60. pmid:34719942Pangarkar SS, Kang DG, Sandbrink F, Bevevino A, Tillisch K, Konitzer L, et al.
VA/DoD clinical practice guideline:
diagnosis and treatment of low back pain
J Gen Intern Med. 2019;34(11):2620–9. pmid:31529375Qaseem A, Wilt TJ, McLean RM, Forciea MA,
Amir Qaseem, MD, PhD, MHA; Timothy J. Wilt, MD, MPH
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530WHO.
Guideline for Non-surgical Management of Chronic Primary Low Back
Pain in Adults in Primary and Community Care Settings
Geneva: World Health Organization; 2023.Oliveira CB, Maher CG, Pinto RZ, Traeger AC, Lin C-WC, Chenot J-F, et al.
Clinical practice guidelines for the management of non-specific
low back pain in primary care: an updated overview.
Eur Spine J. 2018;27(11):2791–803. pmid:29971708Parikh P, Santaguida P, Macdermid J, Gross A, Eshtiaghi A.
Comparison of CPG’s for the diagnosis, prognosis and management
of non-specific neck pain: a systematic review.
BMC Musculoskelet Disord. 2019;20(1):81. pmid:30764789Rubinstein SM, de Zoete A, van Middelkoop M, Assendelft WJJ, de Boer MR.
Benefits and Harms of Spinal Manipulative Therapy for the Treatment
of Chronic Low Back Pain: Systematic Review and Meta-analysis
of Randomised Controlled Trials
British Medical Journal 2019 (Mar 13); 364: 1689Edwards RR, Dworkin RH, Turk DC, Angst MS, Dionne R, Freeman R, et al.
Patient phenotyping in clinical trials of chronic pain treatments:
IMMPACT recommendations.
Pain. 2016;157(9):1851–71. pmid:27152687Hancock MJ, Hill JC.
Are Small Effects for Back Pain Interventions Really Surprising?
J Orthop Sports Phys Ther. 2016;46(5):317–9. pmid:27133941Cruz-Almeida Y, Fillingim RB.
Can quantitative sensory testing move us closer to
mechanism-based pain management?
Pain Med. 2014;15(1):61–72. pmid:24010588Granovsky Y, Yarnitsky D.
Personalized pain medicine: the clinical value of
psychophysical assessment of pain modulation profile.
Rambam Maimonides Med J. 2013;4(4):e0024. pmid:24228167Clauw DJ.
Diagnosing and treating chronic musculoskeletal pain
based on the underlying mechanism(s).
Best Pract Res Clin Rheumatol. 2015;29(1):6–19. pmid:26266995Shi X, Wallach JD.
Umbrella reviews: a useful study design in need of standardisation.
BMJ. 2022;o1740.Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al.
AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised
or non-randomised studies of healthcare interventions, or both.
BMJ. 2017;358:j4008. pmid:28935701Whiting P, Savovic J, Higgins JPT, Caldwell DM, Reeves BC, Shea B, et al.
ROBIS: A new tool to assess risk of bias in systematic reviews was developed.
J Clin Epidemiol. 2016;69:225–34. pmid:26092286Alanazi MS, Degenhardt B, Kelley-Franklin G, Jacobson E, et al.
Autonomic nervous system and viscera-related responses
to manual therapy: A narrative overview.
Int J Osteopath Med. 2024;54:100735.Araujo FX, Ferreira GE, Angellos RF, Stieven FF.
Autonomic effects of spinal manipulative therapy:
systematic review of randomized controlled trials.
J Manipulative Physiol Ther. 2019;42(8):623–34. pmid:31771839Arribas-Romano A, Fernández-Carnero J, Molina-Rueda F.
Efficacy of physical therapy on nociceptive pain processing alterations
in patients with chronic musculoskeletal pain:
a systematic review and meta-analysis.
Pain Med. 2020;21(10):2502–17. pmid:32100027Bernier Carney KM, Young EE, Guite JW, Starkweather AR.
A systematic review of biological mechanisms and chronic
pain outcomes during stress reduction interventions.
Biol Res Nurs. 2020;22(2):205–16. pmid:32174159Bolton PS, Budgell B.
Visceral Responses to Spinal Manipulation
J Electromyogr Kinesiol. 2012 (Oct); 22 (5): 777–784Amoroso Borges BL, Bortolazzo GL, Neto HP.
Effects of spinal manipulation and myofascial techniques
on heart rate variability: A systematic review.
J Bodyw Mov Ther. 2018;22(1):203–8. pmid:29332747Chow N, Hogg-Johnson S, Mior S, Cancelliere C, Injeyan S, et al.
Assessment of studies evaluating spinal manipulative therapy and
infectious disease and immune system outcomes:
a systematic review.
JAMA Netw Open. 2021;4(4):e215493. pmid:33847753Chu J, Allen DD, Pawlowsky S, Smoot B.
Peripheral response to cervical or thoracic spinal manual therapy:
an evidence-based review with meta analysis.
J Man Manip Ther. 2014;22(4):220–9. pmid:25395830Colombi A, Testa M.
The effects induced by spinal manipulative therapy on
the immune and endocrine systems.
Medicina (Kaunas). 2019;55(8):448. pmid:31394861Cook CE, Keter D, Cade WT, Winkelstein BA, Reed WR.
Manual therapy and exercise effects on inflammatory cytokines:
a narrative overview.
Front Rehabil Sci. 2024;5:1305925. pmid:38745971Coronado RA, Gay CW, Bialosky JE, Carnaby GD, Bishop MD, George SZ.
Changes in Pain Sensitivity Following Spinal Manipulation:
A Systematic Review and Meta-analysis
J Electromyogr Kinesiol. 2012 (Oct); 22 (5): 752–767Coronado RA, Bialosky JE, Cook CE.
The temporal effects of a single session of high-velocity, low-amplitude
thrust manipulation on subjects with spinal pain.
Phys Ther Rev. 2010;15(1):29–35.Corso M, Mior SA, Batley S, Tuff T, da Silva-Oolup S, Howitt S, et al.
The effects of spinal manipulation on performance-related outcomes
in healthy asymptomatic adult population: a systematic
review of best evidence.
Chiropr Man Therap. 2019;27:25. pmid:31183076Evans DW.
Mechanisms and Effects of Spinal High-velocity,
Low-amplitude Thrust Manipulation: Previous Theories
J Manipulative Physiol Ther 2002 (May); 25 (4): 251–262Field T.
Massage therapy research review.
Complement Ther Clin Pract. 2016;24:19–31. pmid:27502797Galindez-Ibarbengoetxea X, Setuain I, Andersen LL, Ramírez-Velez R, et al.
Effects of Cervical High-Velocity Low-Amplitude Techniques on Range
of Motion, Strength Performance, and Cardiovascular Outcomes:
A Review
J Altern Complement Med 2017 (Sep); 23 (9): 667–675Gay RE, Bronfort G, Evans RL.
Distraction manipulation of the lumbar spine:
a review of the literature.
J Manipulative Physiol Ther. 2005;28(4):266–73. pmid:15883580Gay CW, Alappattu MJ, Coronado RA, Horn ME, Bishop MD.
Effect of a single session of muscle-biased therapy on pain sensitivity:
a systematic review and meta-analysis of randomized controlled trials.
J Pain Res. 2013;6:7–22. pmid:23403507Gera C, Malik M, Kaur J, Saini M.
A systematic review and meta-analysis on effect of spinal
mobilization and manipulation on cardiovascular responses.
Hong Kong Physiother J. 2020;40(2):75–87. pmid:33005072Haavik H, Kumari N, Holt K, Niazi IK, Amjad I, Pujari AN, et al.
The Contemporary Model of Vertebral Column Joint Dysfunction
and Impact of High-velocity, Low-amplitude Controlled
Vertebral Thrusts on Neuromuscular Function
European J Applied Physiology 2021 (Oct); 121 (10): 2675–2720Haavik H, Niazi IK, Kumari N, Amjad I, Duehr J, Holt K.
The Potential Mechanisms of High-Velocity, Low-Amplitude, Controlled
Vertebral Thrusts on Neuroimmune Function: A Narrative Review
Medicina (Kaunas) 2021 (Jun); 57 (6): 536Hartnett DA.
Gua sha therapy in the management of musculoskeletal pathology:
a narrative review.
Physical Therapy Reviews. 2021;27(3):169–75.Hegedus EJ, Goode A, Butler RJ, Slaven E.
The neurophysiological effects of a single session of
spinal joint mobilization: does the effect last?
J Man Manip Ther. 2011;19(3):143–51. pmid:22851877Hennenhoefer K, Schmidt D.
Toward a theory of the mechanism of high-velocity,
low-amplitude technique: a literature review.
J Am Osteopath Assoc. 2019;119(10):688–95. pmid:31566696Hillier SL, Louw Q, Morris L, Uwimana J, Statham S.
Massage therapy for people with HIV/AIDS.
Cochrane Database Syst Rev. 2010;2010(1):CD007502. pmid:20091636Holey LA, Dixon J.
Connective tissue manipulation: a review of theory and clinical evidence.
J Bodyw Mov Ther. 2014;18(1):112–8. pmid:24411158Honoré M, Leboeuf-Yde C, Gagey O.
The regional effect of spinal manipulation on the pressure pain threshold
in asymptomatic subjects: a systematic literature review.
Chiropr Man Therap. 2018;2611. pmid:29713457Jacobson E.
Structural integration, an alternative method of
manual therapy and sensorimotor education.
J Altern Complement Med. 2011;17(10):891–9. pmid:21992437Jones J, Thomson P, Irvine K, Leslie SJ.
Is there a specific hemodynamic effect in reflexology?
A systematic review of randomized controlled trials.
J Altern Complement Med. 2013;19(4):319–28. pmid:23072265Jun P, Pagé I, Vette A, Kawchuk G.
Potential mechanisms for lumbar spinal stiffness change following
spinal manipulative therapy: a scoping review.
Chiropr Man Therap. 2020;28(1):15. pmid:32293493Jung A, Adamczyk WM, Ahmed A, van der Schalk L, Poesl M, Luedtke K, et al.
No Sufficient evidence for an immediate hypoalgesic effect of spinal
manual therapy on pressure pain thresholds in asymptomatic and chronic
pain populations: a systematic review and meta-analysis.
Phys Ther. 2023;103(3):pzad003. pmid:37172128Kingston L, Claydon L, Tumilty S.
The effects of spinal mobilizations on the sympathetic
nervous system: a systematic review.
Man Ther. 2014;19(4):281–7. pmid:24814903Lascurain-Aguirrebeña I, Newham D, Critchley DJ.
Mechanism of action of spinal mobilizations:
a systematic review.
Spine (Phila Pa 1976). 2016;41(2):159–72. pmid:26751060Lima CR, Martins DF, Reed WR.
Physiological Responses Induced by Manual Therapy
in Animal Models: A Scoping Review
Frontiers in Neuroscience 2020 (May 8); 14: 430Meyer A-L, Amorim M-A, Schubert M, Schweinhardt P, Leboeuf-Yde C.
Unravelling functional neurology: does spinal manipulation have
an effect on the brain? - a systematic literature review.
Chiropr Man Therap. 2019;27:60. pmid:31632640Millan M, Leboeuf-Yde C, Budgell B, Amorim M-A.
The Effect of Spinal Manipulative Therapy on Experimentally
Induced Pain: A Systematic Literature Review
Chiropractic & Manual Therapies 2012 (Aug 10); 20 (1): 26Mitchell UH, Helgeson K, Mintken P.
Physiological effects of physical therapy interventions on
lumbar intervertebral discs: A systematic review.
Physiother Theory Pract. 2017;33(9):695–705. pmid:28715273Moyer CA, Seefeldt L, Mann ES, Jackley LM.
Does massage therapy reduce cortisol?
A comprehensive quantitative review.
J Bodywork Mov Ther. 2011;15:3–14.Navarro-Santana MJ, Gómez-Chiguano GF, Somkereki MD.
Effects of joint mobilisation on clinical manifestations of sympathetic
nervous system activity: a systematic review and meta-analysis.
Physiotherapy. 2020;107:118–32. pmid:32026812Nelson NL.
Massage therapy: understanding the mechanisms of action
on blood pressure. A scoping review.
J Am Soc Hypertens. 2015;9(10):785–93. pmid:26324746Picchiottino M, Leboeuf-Yde C, Gagey O, Hallman DM.
The acute effects of joint manipulative techniques on markers of autonomic
nervous system activity: a systematic review and meta-analysis
of randomized sham-controlled trials.
Chiropr Man Therap. 2019;27:17. pmid:30911373Pickar JG.
Neurophysiological Effects of Spinal Manipulation
Spine J (N American Spine Society) 2002 (Sep); 2 (5): 357–371Potter L, McCarthy C, Oldham J.
Physiological effects of spinal manipulation: a review of proposed theories.
Phys Ther Rev. 2005;10(3):163–70.Riley SP, Swanson BT, Shaffer SM, Flowers DW, Hofbauer MA, Liebano RE.
Does manual therapy meaningfully change quantitative sensory testing
and patient reported outcome measures in patients with
musculoskeletal impairments related to the spine?:
A “trustworthy” systematic review and meta-analysis.
J Man Manip Ther. 2024;32(1):51–66. pmid:37622723Rogan S, Taeymans J, Berger I, Baur H.
Manual spinal therapy techniques to stimulate the
autonomic nervous system: a scoping review.
Sportverletz Sportschaden. 2023;37(2):67–78. pmid:37216936Kovanur-Sampath K, Mani R, Cotter J, Gisselman AS, Tumilty S.
Changes in biochemical markers following spinal manipulation-
a systematic review and meta-analysis.
Musculoskelet Sci Pract. 2017;29120–31. pmid:28399479Kovanur Sampath K, Tumilty S, Wooten L, Belcher S, Farrell G, Gisselman AS.
Effectiveness of spinal manipulation in influencing the autonomic
nervous system - a systematic review and meta-analysis.
J Man Manip Ther. 2024;32(1):10–27. pmid:38044657Savva C, Karagiannis C, Korakakis V, Efstathiou M.
The analgesic effect of joint mobilization and manipulation
in tendinopathy: a narrative review.
J Man Manip Ther. 2021;29(5):276–87. pmid:33769226Schmid A, Brunner F, Wright A, Bachmann LM.
Paradigm shift in manual therapy? Evidence for a central nervous system
component in the response to passive cervical joint mobilisation.
Man Ther. 2008;13(5):387–96. pmid:18316238Simmonds N, Miller P, Gemmell H.
A theoretical framework for the role of fascia in manual therapy.
J Bodyw Mov Ther. 2012;16(1):83–93. pmid:22196432Sousa KA de, Cardoso LB, Pirola FM, Auad LG, De Oliveira AS.
Effect of manual therapies on cardiac autonomic control:
a systematic review.
mtprehabjournal. 20201–12.Sullivan SG, Paolacci S, Kiani AK, Bertelli M.
Chiropractic Care for Hypertension: Review of the Literature
and Study of Biological and Genetic Bases
Acta Bomedica 2020 (Nov 9); 91 (13-S): e2020017Tejero-Fernández V, Membrilla-Mesa M, Galiano-Castillo N, Arroyo-Morales M.
Immunological effects of massage after exercise: A systematic review.
Phys Ther Sport. 2015;16(2):187–92. pmid:25116861Vernon H.
Qualitative Review of Studies of Manipulation-induced Hypoalgesia
J Manipulative Physiol Ther 2000 (Feb); 23 (2): 134–138Vicenzino B, Paungmali A, Teys P.
Mulligan’s mobilization-with-movement, positional faults and pain relief:
current concepts from a critical review of literature.
Man Ther. 2007;12(2):98–108. pmid:16959529Vigotsky AD, Bruhns RP.
The role of descending modulation in manual therapy and
its analgesic implications: a narrative review.
Pain Res Treat. 2015;2015292805. pmid:26788367Voogt L, de Vries J, Meeus M, Struyf F, Meuffels D, Nijs J.
Analgesic effects of manual therapy in patients with
musculoskeletal pain: a systematic review.
Man Ther. 2015;20(2):250–6. pmid:25282440Weerapong P, Hume PA, Kolt GS.
The mechanisms of massage and effects on performance,
muscle recovery and injury prevention.
Sports Med. 2005;35(3):235–56. pmid:15730338Xiong XJ, Li SJ, Zhang YQ.
Massage therapy for essential hypertension: a systematic review.
J Hum Hypertens. 2015;29(3):143–51. pmid:24990417Yao S, Hassani J, Gagne M, George G, Gilliar W.
Osteopathic manipulative treatment as a useful adjunctive tool for pneumonia.
J Vis Exp. 2014;(87):50687. pmid:24836893Young KJ, Leboeuf-Yde C, Gorrell L, Bergström C, Evans DW, Axén I, et al.
Mechanisms of Manipulation: A Systematic Review of the Literature on
Immediate Anatomical Structural or Positional Changes in Response
to Manually Delivered High-velocity, Low-amplitude Spinal Manipulation.
Chiropractic & Manual Therapies 2024 (Sep 11); 32 (1): 28Zegarra-Parodi R, Park PYS, Heath DM, Makin IRS, Degenhardt BF, Roustit M.
Assessment of skin blood flow following spinal manual therapy:
a systematic review.
Man Ther. 2015;20(2):228–49. pmid:25261088Côté P, Bussières A, Cassidy JD, Hartvigsen J, Kawchuk GN, et al.
A united statement of the global chiropractic research community against
the pseudoscientific claim that chiropractic care boosts immunity.
Chiropr Man Therap. 2020;28(1):21. pmid:32366319Courtney CA, Witte PO, Chmell SJ, Hornby TG.
Heightened flexor withdrawal response in individuals with knee osteoarthritis
is modulated by joint compression and joint mobilization.
J Pain. 2010;11(2):179–85. pmid:19945353Courtney CA, Steffen AD, Fernández-de-Las-Peñas C, Kim J, Chmell SJ.
Joint Mobilization Enhances Mechanisms of Conditioned Pain
Modulation in Individuals With Osteoarthritis of the Knee.
J Orthop Sports Phys Ther. 2016;46(3):168–76. pmid:26721229Skyba DA, Radhakrishnan R, Rohlwing JJ, Wright A, Sluka KA.
Joint Manipulation Reduces Hyperalgesia By Activation of Monoamine
Receptors But Not Opioid or GABA Receptors in the Spinal Cord
Pain. 2003 (Nov); 106 (1-2): 159–168Gay CW, Robinson ME, George SZ, Perlstein WM, Bishop MD.
Immediate changes after manual therapy in resting-state functional
connectivity as measured by functional magnetic resonance imaging
in participants with induced low back pain.
J Manipulative Physiol Ther. 2014;37(9):614–27. pmid:25284739Wan DWL, Arendt-Nielsen L, Wang K, Xue CC, Wang Y, Zheng Z.
Pain adaptability in individuals with chronic musculoskeletal
pain is not associated with conditioned pain modulation.
J Pain. 2018;19(8):897–909. pmid:29597084Zheng Z, Wang K, Yao D, Xue CCL, Arendt-Nielsen L.
Adaptability to pain is associated with potency of local pain inhibition,
but not conditioned pain modulation: a healthy human study.
Pain. 2014;155(5):968–76. pmid:24502842Gierthmühlen J, Binder A, Förster M, Baron R.
Do we measure what patients feel?: an analysis of correspondence between
somatosensory modalities upon quantitative sensory testing
and self-reported pain experience.
Clin J Pain. 2018;34(7):610–7. pmid:29271799Gonçalves Dos Santos G, Delay L, Yaksh TL, Corr M.
Neuraxial cytokines in pain states.
Front Immunol. 2020;103061. pmid:32047493Wrona D.
Neural-immune interactions: an integrative view of the bidirectional
relationship between the brain and immune systems.
J Neuroimmunol. 2006;172(1–2):38–58. pmid:16375977Ulrich-Lai YM, Herman JP.
Neural regulation of endocrine and autonomic stress responses.
Nat Rev Neurosci. 2009;10(6):397–409. pmid:19469025Gritsenko V, Kalaska JF, Cisek P.
Descending corticospinal control of intersegmental dynamics.
J Neurosci. 2011;31(33):11968–79. pmid:21849557Nim CG, Downie A, O’Neill S, Kawchuk GN, Perle SM, Leboeuf-Yde C.
The importance of selecting the correct site to apply spinal manipulation
when treating spinal pain: Myth or reality? A systematic review.
Sci Rep. 2021;11(1):23415. pmid:34862434Sørensen PW, Nim CG, Poulsen E, Juhl CB.
Spinal manipulative therapy for nonspecific low back pain: does targeting
a specific vertebral level make a difference?:
a systematic review with meta-analysis.
J Orthop Sports Phys Ther. 2023;53(9):529–39. pmid:37506306Keter D, Griswold D, Learman K, Cook C.
Priorities in updating training paradigms in orthopedic
manual therapy: an international Delphi study.
J Educ Eval Health Prof. 2023;20:4. pmid:36702788Keter D, Griswold D, Learman K, Cook C.
Modernizing patient-centered manual therapy: Findings from
a Delphi study on orthopaedic manual therapy application.
Musculoskelet Sci Pract. 2023;65102777. pmid:37257320Keter D, Hutting N, Vogsland R, Cook CE.
Integrating person-centered concepts and modern manual therapy.
JOSPT Open. 2024;2(1):60–70.Kerry R, Young KJ, Evans DW, Lee E, Georgopoulos V, Meakins A, et al.
A modern way to teach and practice manual therapy.
Chiropr Man Therap. 2024;32(1):17. pmid:38773515McDevitt AW, O’Halloran B, Cook CE.
Cracking the code: unveiling the specific and shared
mechanisms behind musculoskeletal interventions.
Arch Physiother. 2023;13(1):14. pmid:37415258Keter DL, Bent JA, Bialosky JE, Courtney CA, Esteves JE, Funabashi M, et al.
An international consensus on gaps in mechanisms of forced-based
manipulation research: findings from a nominal group technique.
J Man Manip Ther. 2024;32(1):111–7. pmid:37840477Griswold D, Learman K, Rossettini G, Palese A, Ickert E, Wilhelm M, et al.
Identifying priority gaps in contextual factors research and
force-based manipulation. An international and
interdisciplinary Delphi study.
J Man Manip Ther. 2024;32(1):118–26. pmid:37697816
Return to SPINAL PAIN MANAGEMENT
Since 3-20-2025


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |