Access to Chiropractic Care and the Cost
of Spine Conditions Among Older AdultsThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: American Journal of Managed Care 2019 (Aug); 25 (8): e230–e236 ~ FULL TEXT
OPEN ACCESS Matthew A. Davis, PhD, DC, MPH; Olga Yakusheva, PhD; Haiyin Liu, MA; Joshua Tootoo, MS; Marita G. Titler, PhD, RN; and Julie P.W. Bynum, MD, MPH
Matthew A. Davis, PhD, DC, MPH
University of Michigan,
400 N Ingalls St, Room 4347,
Ann Arbor, MI 48109.
mattadav@umich.edu
FROM: Liliedahl, JMPT 2010Objectives: Chiropractic care is a service that operates outside of the conventional medical system and is reimbursed by Medicare. Our objective was to examine the extent to which accessibility of chiropractic care affects spending on medical spine care among Medicare beneficiaries.
Study Design: Retrospective cohort study that used beneficiary relocation as a quasi-experiment.
Methods: We used a combination of national data on provider location and Medicare claims to perform a quasi-experimental study to examine the effect of chiropractic care accessibility on healthcare spending. We identified 84,679 older adults enrolled in Medicare with a spine condition who relocated once between 2010 and 2014. For each year, we measured accessibility using the variable-distance enhanced 2-step floating catchment area method. Using data for the years before and after relocation, we estimated the effect of moving to an area of lower or higher chiropractic accessibility on spine-related spending adjusted for access to medical physicians.
Results: There are approximately 45,000 active chiropractors in the United States, and local accessibility varies considerably. A negative dose–response relationship was observed for spine-related spending on medical evaluation and management as well as diagnostic imaging and testing (mean differences, $20 and $40, respectively, among those exposed to increasingly higher chiropractic accessibility; P <.05 for both). Associations with other types of spine-related spending were not significant.
There are more articles like this @ our: Cost-Effectiveness of Chiropractic Page Conclusions: Among older adults, access to chiropractic care may reduce medical spending on services for spine conditions.
Takeaway Points
This study was published in the American Journal of Managed Care in September, 2019 by Davis et al. In this study, investigators looked at whether access to more or fewer practicing doctors of chiropractic (DC) impacted total spending for spine-related disorders in Medicare beneficiaries with a diagnosis of low back or neck pain. Access was calculated by the number of DCs practicing within a certain drive time from the patient’s home zip code. Study authors found that those “exposed” to areas of “higher chiropractic accessibility” resulted in lower ambulatory care expenditures, primarily for diagnostic imaging and evaluation/management services.
This study is important because it adds to the small but growing cadre of evidence indicating that access to chiropractic may result in lower costs for spine care, in this case for older adults.
— Thanks to Spine IQ BackBlog for the above comments.
Chiropractic care is a Medicare-reimbursed service that operates outside of the conventional medical system and provides a sizable amount of the nation’s spine care.
Medicare beneficiaries can access chiropractic care without a medical referral.
Previous studies have not considered how use of chiropractic care affects spending on costly medical services.
We found some evidence of a relationship between lower accessibility of chiropractic care and higher spending on diagnostic imaging and testing for spine conditions.
From the FULL TEXT Article:
Background
Back pain and neck pain are associated with an estimated direct cost of $86 billion to the United States economy. [1] Among the top contributors to disability, back pain and neck pain outrank chronic diseases such as chronic pulmonary disease, ischemic heart disease, and diabetes. [2] Although back pain can be attributed to a serious underlying medical problem, up to 85% of cases are classified as nonspecific (ie, cases without an underlying pathology). [3] Approximately one-fourth of all adults will experience nonspecific back pain during a 3–month period, and at any one point in time, approximately 30% of older adults suffer from back pain. [4] Older adults are particularly vulnerable to back pain and most who experience nonspecific back pain have future recurrences [4, 5]; thus, it is among the most common reasons older Americans visit physicians. [6]
With more than 100 million visits for spine conditions each year, [7, 8] the chiropractic profession is the largest health service that operates outside of the conventional medical system [9, 10] and the only such service reimbursed by Medicare. [11, 12] Medicare beneficiaries can use chiropractic care without a medical referral; however, the only reimbursable modality is manual therapy, which costs approximately $30 to $50 per visit. Chiropractors cannot be reimbursed directly for diagnostic imaging nor prescribe medications. In light of the ongoing debate regarding coverage of presumably nonessential services, there is a specific need to more rigorously examine how chiropractic care may affect national healthcare spending.
Previous observational research that has examined spending among chiropractic patients compared with medical care patients suggests that chiropractic care may reduce utilization of and expenditures on medical services for back pain. [13, 14] Traditional observational studies use assignment of patients to a specific treatment type (eg, chiropractic vs usual care) to study the cost of chiropractic care. These designs, however, are unable to account for the potential impacts from those who choose to use chiropractic care in place of medical care. To date, previous studies have neglected to consider such indirect effects of the service on the system at large.
Therefore, we performed a quasi-experimental study to examine how accessibility of chiropractic care among Medicare beneficiaries affects healthcare spending for spine conditions. To do so, we used a cohort of older adults in Medicare with back and/or neck pain who relocated and experienced a change in geographic accessibility of chiropractic care. In this way, the change in accessibility of chiropractic care served as a proxy for access to the service among Medicare beneficiaries, providing us with the unique opportunity to observe how either reducing or increasing access affects spine-related spending among older adults.
METHODS
We examined the effect of accessibility of chiropractic care on spine-related spending using a quasi-experimental design. For our study, we geocoded Medicare beneficiaries and identified a cohort with back and/or neck pain who relocated once from 2010 to 2014. Then, using the variable-distance enhanced 2–step floating catchment area method [15, 16] to estimate provider to population ratios, we determined the effect of a change in accessibility of chiropractic care on spine-related spending. This method for estimating provider accessibility is the gold standard because it has a higher resolution that incorporates travel time, takes into account the location of healthcare in adjacent areas, and is less affected by choice of geographic scale.
As our study used administrative claims and publicly available data on healthcare providers, it received an expedited review by the University of Michigan Health Sciences and Behavioral Sciences Institutional Review Board.
Study Population

eAppendix Figures & Tables First, we identified all older adults (65 years and older) enrolled in Medicare Part B throughout 2010 to 2014—this resulted in the identification of 16,842,729 beneficiaries (eAppendix Figure 1. For each calendar year, we merged beneficiary residential zip codes with hospital referral regions (HRRs) that represent the 306 regional US healthcare markets. We then identified 986,076 beneficiaries who relocated at least once by changing HRR. We restricted our sample to the 887,917 beneficiaries who relocated only once during the 5–year time period—634,935 had at least 1 year of data prior to and after the relocation (eAppendix Figure 2).
Of those 634,935, we identified 84,679 beneficiaries who had a back and/or neck pain visit using an established list of International Classification of Disease, Ninth Revision, Clinical Modification codes for spine conditions. [17] Our aim was to identify a cohort of beneficiaries who had back and/or neck pain prior to relocation (ie, those most likely to be affected by accessibility of chiropractic care). Therefore, we restricted our sample to beneficiaries who had 2 separate claims for back or neck pain at least 4 months apart in the year prior to relocation.
Chiropractic Care Accessibility
For each year, we gathered data on provider location from historic versions of the National Plan and Provider Enumeration System (NPPES). We used provider specialty code 35 in NPPES data to identify the practice locations of chiropractors. [18] We removed chiropractors who were clinically inactive in Medicare by linking NPPES provider data to the 20% Carrier file and removing any providers who did not submit a claim in the relevant year. Medicare beneficiaries were aggregated to Zip Code Tabulation Areas (ZCTAs) according to their zip code of residence for each year. ZCTAs are generalized areal representations of US Postal Service zip code service areas. Once assigned a ZCTA, beneficiaries in our study cohort were assigned measures of chiropractic care accessibility. For each ZCTA, we measured chiropractic care accessibility using an enhanced version of the variable-distance enhanced 2–step floating catchment area method first developed by Luo and Wang15 and modified by others. [16]
Our measure was constructed based on the 2010 US Census block–level population aggregated up to ZCTA level in order to assign each patient estimates of chiropractic care accessibility. First, we calculated a drive time–based service area for each practice location. US Census block centroids within each service area provided population estimates. These estimates were summed to generate provider to population ratios for each practice location. Next, we estimated chiropractic care accessibility based on the weighted sum of all practice locations within a given drive time from each Census block centroid. For locations within a threshold distance (eg, 5, 10, or 15 miles), scores were summed and scaled according to drive time from the block centroid. These estimates of chiropractic care accessibility were then aggregated to the ZCTA in order to assign a measure of provider accessibility around each ZCTA population-weighted centroid.
Medicare Spine Spending
Our primary dependent variable was annual spine-related spending. We used the combination of ResDAC Carrier, Medical Provider Analysis and Review (referred to as MedPAR), and Outpatient files to calculate total spending on back and neck pain diagnoses by summing across all types of inpatient and outpatient care for each calendar year. We calculated spine-related spending on inpatient and ambulatory care (office-based and outpatient claims combined) separately. To examine more subtle differences in spending, we used the Berenson-Eggers Type of Service categories for “evaluation and management” and “procedures”; furthermore, we combined the categories “imaging” and “testing.” Healthcare spending was adjusted for inflation to 2014 dollars using the Consumer Price Index for medical services. [19]
Covariates
To adjust for baseline differences, we extracted several sociodemographic characteristics, including age, sex, and race/ethnicity, from the Master Beneficiary Summary File. To account for differences in health status (and changes in health status over time) for each calendar year, we used all administrative data to calculate a comorbidity score using the Charlson-Deyo Comorbidity Index. [20] We adjusted for differences in accessibility of primary care physicians.21 Accessibility of primary care physicians (internal medicine, family practice, and general practitioners) was calculated using an approach identical to that described for chiropractic care.
Statistical Analyses
We displayed our national estimate of chiropractic care accessibility for each ZCTA and calculated the coefficient of variation. In order to illustrate high versus low area accessibility, we converted data to standard normal deviations for 2014 ZCTAs (the most recent year of data). We also plotted the unadjusted chiropractor to population ratios collapsed by quintile (eAppendix Figure 3).
We used data from the year before and the year after relocation (referred to herein as baseline year and postrelocation year). The estimated effect of a change in chiropractic care accessibility was evaluated in 2 ways. First, we simply identified whether the beneficiary relocated to a higher or a lower chiropractic care accessibility quintile relative to their baseline location. Second, we examined the magnitude of the increase or decrease in chiropractic care accessibility by reporting results according to the number of quintiles up or down a beneficiary moved by relocating, regardless of starting point, to identify the equivalent of a dose response. The comparison group in these analyses was all beneficiaries who moved but did not experience a change in accessibility (ie, remained in the same quintile). The 2 approaches highlight different dimensions of relocation change: The first focuses on the initial level of accessibility but aggregates change into broad categories of any increase or decrease, and the second captures how much change in accessibility occurred, with less focus on the starting level.
The end point for all analyses was the change in spine-related spending (eg, spending on inpatient care, ambulatory care), which was normally distributed. Across baseline accessibility of chiropractic care, age and sex differed very little; however, race and health status varied (eAppendix Table 1). Therefore, we adjusted for differences in our analyses using linear regression. Specifically, our models adjusted for baseline chiropractic care accessibility, beneficiary characteristics (age, sex, race, baseline comorbidities, and change in comorbidities), and access to primary care physicians (at baseline and a change in access). Analyses were based on complete case analysis and we assumed any missing values to be missing completely at random. A 2–sided P value of less than .05 was considered statistically significant. Geospatial analyses were conducted using ArcGIS version 10.5 (Esri; Redlands, California) and analyses of claims data were conducted using SAS version 9.4 (SAS Institute; Cary, North Carolina).
Our analyses were restricted to beneficiaries who had evidence of a back and/or neck condition in the baseline year. In a subanalysis we repeated all analyses on a subset of 57,807 older adults who also had spine claims in the postrelocation year.
RESULTS
Characteristics of Study Population
Among the 84,679 older adults enrolled in Medicare with a spine condition prior to relocating, 9.5%, 18.0%, 22.9%, 26.7%, and 22.9% resided in quintiles 1 through 5 of chiropractic care accessibility, respectively. The mean (SD) age of older adults with a spine condition who moved once was 77.0 (7.2) years; 68.4% were female, and 3.9% were black.
Accessibility of Chiropractic Care

Figure 1 The total number of active chiropractors varied little from 2010 to 2014—from a high of 45,264 in 2012 to a low of 44,040 in 2014. Across the country, local accessibility varied considerably, with a higher concentration of chiropractors observed in the upper Midwest and a relatively lower concentration in the South (coefficient of variation = 93%) (Figure 1; eAppendix Figure 3). Across US ZCTAs in 2014, the mean (SD) ratio of chiropractors per 100,000 population was 15.6 (14.4). Ratios for quintile 1 were 0.0 to 4.6; quintile 2, 4.7 to 9.4; quintile 3, 9.5 to 15.0; quintile 4, 15.1 to 23.6; and quintile 5, 23.7 to 445.5. The several ZCTAs with very high chiropractor to population ratios were in the upper Midwest, where the profession originated and a large chiropractic school is located (in Davenport, Iowa).
Chiropractic Care Accessibility and Spine-Related Spending

Table 1

Table 2
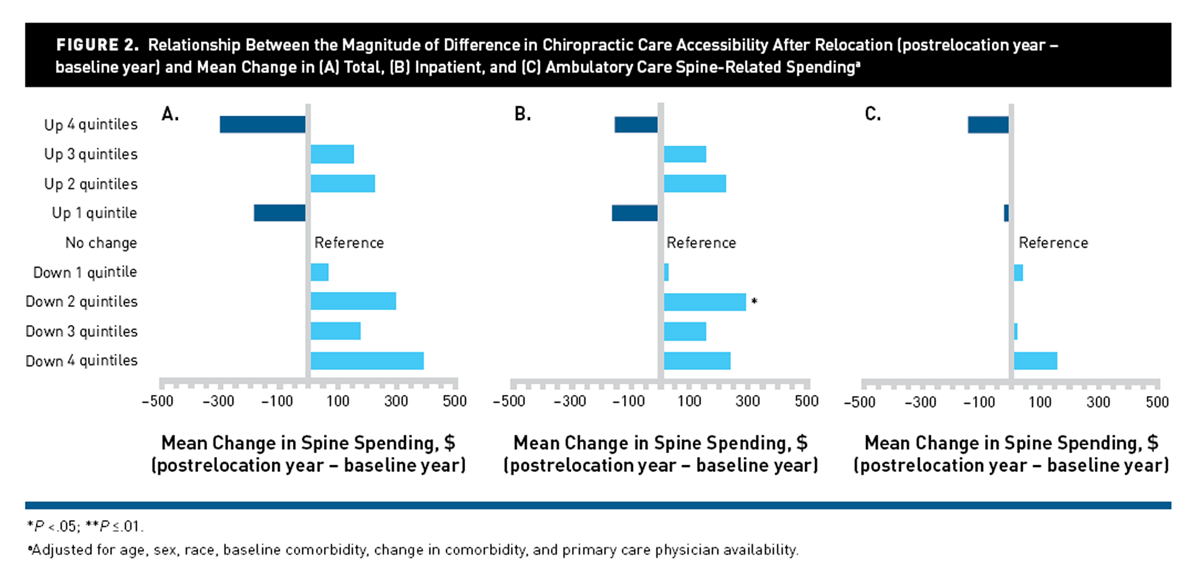
Figure 2
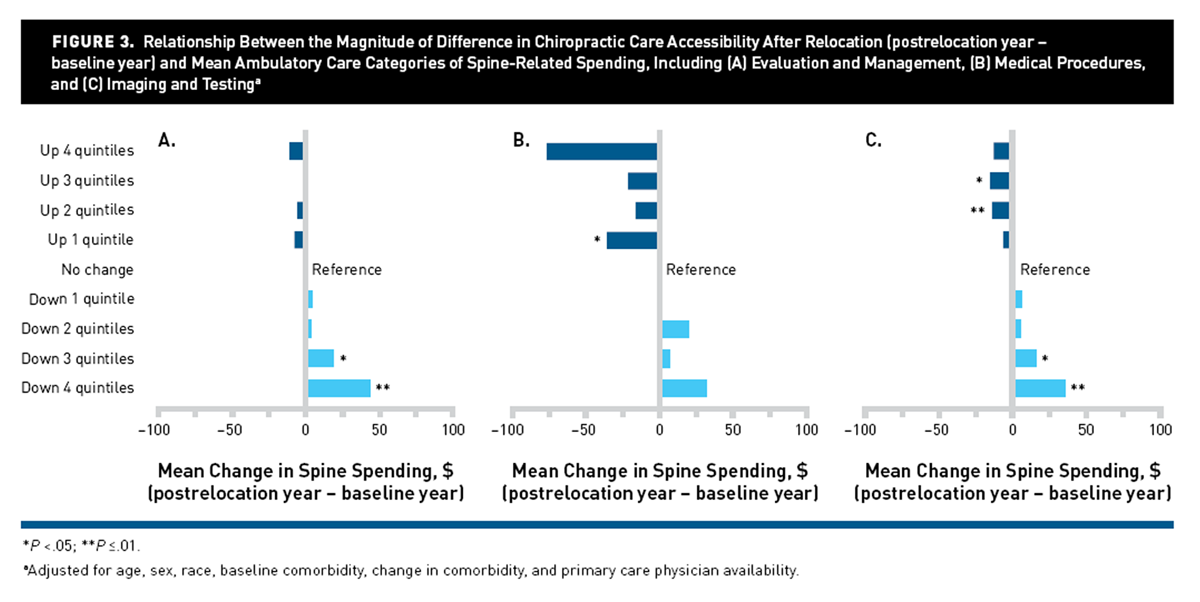
Figure 3 When examining whether the beneficiaries relocated to an area with higher or lower chiropractic care accessibility relative to where they started, we found few differences in mean spending on total, inpatient, and ambulatory spine care (Table 1). The only marginally statistically significant differences in spending were mean increases of $513 in total spine-related spending (P = .05) and $434 in inpatient spine-related spending (P = .06) among older adults who resided in quintile 3 and who moved to an area of lower chiropractic care accessibility. Although attenuated, some small differences were observed by category of ambulatory care spine spending (Table 2).
Among residents of quintile 5 who moved to an area of lower chiropractic care accessibility, mean spending on medical procedures decreased by $53 (P = .04). Residents of quintile 2 who moved to an area of higher chiropractic care accessibility had a decrease of $30 (P <.001) in mean spending on spine diagnostic imaging and tests.
We found more consistent changes when examining the association of spending with the magnitude of the change in chiropractic care accessibility (Figures 2 and 3). In general, increases in spending were observed among older adults who moved to areas with lower accessibility of chiropractic care — however, the only statistically significant increase was for inpatient spending among those who moved to areas with chiropractic accessibility 2 quintiles higher than where they started (mean difference in spending of $291; P = .05). In addition, a small dose–response relationship was observed for ambulatory care spine spending on “evaluation and management” and “imaging and testing” (Figure 3). For both, decreases of 3 and 4 quintiles of chiropractic accessibility were associated with approximate mean increases in spending of $20 (P <.05) and $40 (P <.01), respectively.
The inverse association between accessibility of chiropractic care and spending on spine imaging and testing persisted when restricted to the subset of older adults who had a spine condition in the postrelocation year.
DISCUSSION
Despite a sizable literature devoted to describing health services that function outside of the conventional medical system in the United States, our study is among the first to attempt to quantify the effect of access to such a service on spending using a quasi-experimental approach. We applied state-of-the-art geospatial methods both for developing the geographic accessibility measures and for using relocation as a tool for approximating causal mechanisms in observational studies. Originating from the field of economics, natural experiments are being used by a growing number of health researchers who seek to identify causal mechanisms from nonexperimental data. [22–25] Taking advantage of unique opportunities to balance confounding factors and designs that allow for temporal observations to be made offers stronger evidence of cause and effect. [26] For instance, in an influential report, Song et al used Medicare patients who relocated to examine variation in practice intensity. [24] Although effects of chiropractic care accessibility on spending were inconsistent and overall small, we did find some evidence of chiropractic care accessibility affecting spending on certain types of spine-related care. Specifically, we observed small, consistent differences in spending on diagnostic imaging and tests for spine conditions. This is among the first evidence to suggest a potential reduction in medical service use due to a health service that operates primarily outside of traditional pathways of care.
To our knowledge this is also the first application of the variable-distance enhanced 2–step floating catchment area method to national provider data. This approach has several advantages over other measures, including that it(1) provides a more realistic estimation of impact of moving that incorporates travel time in both the urban and rural settings,
(2) allows for movement/interaction across areas to account for accessibility in adjacent locales, and
(3) is less sensitive to changes in scale because it uses a continuous measure of impedance to calculate provider to population ratios.Use of this method led us to identify relatively high accessibility of chiropractic care in the upper Midwest and lower accessibility in the South, which aligns with previous reports. [21] Although our analyses cannot fully explain this pattern, the profession did originate in the upper Midwest, suggesting that cultural factors may play a role. A recent report that compared availability of different provider types found that chiropractors were more likely to locate in areas of higher income and health status. [27]
Healthcare Policy Implications
In spite of the Choosing Wisely campaign’s mantra that “less is more” for clinical management of back pain, [28, 29] trends indicate worrisome increases in the use of opioid analgesic medications, overreliance on medical specialists, and unwarranted diagnostic imaging. [30–32] All of these practices lead to higher healthcare costs. [3, 33–35]
Medicare spends $400 million to $500 million on chiropractic care each year, [36, 37] and chiropractic care has been scrutinized several times by the Office of the Inspector General. [12, 36–38] A prior study uncovered an association between higher accessibility of chiropractic care and lower reliance on primary care services, suggesting that chiropractic care may substitute for medical care. [39] We sought to determine whether or not chiropractic care is merely additive to the system (ie, patients use chiropractic care who would have otherwise not used health services or patients use chiropractic care in addition to other health services). We find that chiropractic care may be associated with small savings in aspects of ambulatory care. Although these are small per-person dollar differences ($40 reduction in annual spending), the cumulative effect could be quite large given the prevalence of spine conditions among older adults. Thus, it is conceivable that CMS is recapturing a portion of the payout for coverage of chiropractic care.
Limitations
Our study has several potential limitations that must be acknowledged. The cohort consisted of older adult Medicare beneficiaries who relocated once from 2010 to 2014, which could be perceived to limit the generalizability of our findings. However, considering that each beneficiary included in our cohort served as his or her own control, there is no reason to believe that the change in spending is not more broadly generalizable. A particular strength of using Medicare beneficiary relocation as an exogenous change unlikely to be related to our primary variable of interest is that it can be considered a more rigorous study design compared with traditional observational studies. However, we found differences in race and health status according to the change in chiropractic care accessibility. Despite accounting for these differences in our analyses, we cannot completely rule out residual confounding. Lastly, because our study used administrative data, we focused on spending, which is only one aspect of the important issues related to management of back and neck pain. We cannot say whether reductions in pain, improvements in quality of life, or use of pharmacological agents were any different from the data in this study. These are particularly important avenues for investigation in the context of the current opioid crisis and will be addressed in future work.
CONCLUSIONS
This study is among the first to examine whether access to chiropractic care, a health service that provides a significant amount of the nation’s conservative management of nonspecific back pain, has any effect on Medicare spending. We found some evidence of a relationship between lower accessibility of chiropractic care and higher spending on diagnostic imaging and testing. Future work is required to determine if indeed access to chiropractic care for Medicare beneficiaries in any way breaks the pathway to care that is discordant with practice guidelines
Author Affiliations:
University of Michigan Institute for Social Research (MAD), Ann Arbor, MI; University of Michigan School of Nursing (MAD, OY, HL, MGT), Ann Arbor, MI; Institute for Healthcare Policy and Innovation, University of Michigan (MAD, OY, MGT, JPWB), Ann Arbor, MI; University of Michigan School of Public Health (OY), Ann Arbor, MI; National Center for Geospatial Medicine, Rice University (JT), Houston, TX; Department of Internal Medicine, Geriatric and Palliative Medicine, University of Michigan Medical School (JPWB), Ann Arbor, MI.
Source of Funding:
This work was supported by award number 1R01AT009003 from the National Center for Complementary and Integrative Health at the National Institutes of Health. The views expressed herein do not necessarily represent the official views of the National Center for Complementary and Integrative Health nor the National Institutes of Health.
Author Disclosures:
The authors report no relationship or financial interest with any entity that would pose a conflict of interest with the subject matter of this article.
References:
Martin BI. Deyo R. Mirza SK, et al.
Expenditures and Health Status Among Adults With Back and Neck Problems
JAMA 2008 (Feb 13); 299 (6): 656–664Murray CJL, Atkinson C, Bhalla K, Birbeck G, Burstein R, Chou D, et al.
The State of US Health, 1990-2010: Burden of Diseases, Injuries, and Risk Factors
JAMA 2013 (Aug 14); 310 (6): 591–608Deyo RA, Weinstein JN.
Low back pain.
N Engl J Med. 2001;344(5):363-370. doi: 10.1056/NEJM200102013440508.Docking RE, Fleming J, Brayne C, Zhao J, Macfarlane GJ, Jones GT;
Cambridge City Over-75s Cohort Study Collaboration.
Epidemiology of back pain in older adults: prevalence and risk factors for back pain onset.
Rheumatology (Oxford). 2011;50(9):1645-1653. doi: 10.1093/rheumatology/ker175.Dunn KM, Hestbaek L, Cassidy JD.
Low back pain across the life course.
Best Pract Res Clin Rheumatol. 2013;27(5):591-600. doi: 10.1016/j.berh.2013.09.007.Hart LG, Deyo RA, Cherkin DC.
Physician office visits for low back pain: frequency, clinical evaluation, and treatment patterns
from a U.S. national survey.
Spine (Phila Pa 1976). 1995;20(1):11-19.Whedon JM, Song Y, Davis MA.
Trends in the Use and Cost of Chiropractic Spinal Manipulation Under Medicare Part B
Spine J. 2013 (Nov); 13 (11): 1449–1454Davis, MA, Sirovich, BE, and Weeks, WB.
Utilization and Expenditures on Chiropractic Care
in the United States from 1997 to 2006
Health Serv Res. 2010 (Jun); 45 (3): 748-761Allareddy V, Greene BR, Smith M, Haas M, Liao J.
Facilitators and barriers to improving interprofessional referral relationships between
primary care physicians and chiropractors.
J Ambul Care Manage. 2007;30(4):347-354. doi: 10.1097/01.JAC.0000290404.96907.e3.Greene BR, Smith M, Haas M, Allareddy V.
How often are physicians and chiropractors provided with patient information when accepting referrals?
J Ambul Care Manage. 2007;30(4):344-346. doi: 10.1097/01.JAC.0000290403.89284.e0.Meeker, W., & Haldeman, S. (2002).
Chiropractic: A Profession at the Crossroads of Mainstream and Alternative Medicine
Annals of Internal Medicine 2002 (Feb 5); 136 (3): 216–227Whedon JM, Goertz CM, Lurie JD, Stason WB.
Beyond Spinal Manipulation: Should Medicare Expand Coverage for Chiropractic Services?
A Review and Commentary on the Challenges for Policy Makers
Journal of Chiropractic Humanities 2013 (Aug 28); 20 (1): 9–18Martin, BI, Gerkovich, MM, Deyo, RA et al.
The Association of Complementary and Alternative Medicine Use and Health Care Expenditures
for Back and Neck Problems
Medical Care 2012 (Dec); 50 (12): 1029–1036Stano M, Smith M:
Chiropractic and Medical Costs of Low Back Care
Medical Care 1996 (Mar); 34 (3): 191–204Luo W, Wang F.
Measures of spatial accessibility to health care in a GIS environment:
synthesis and a case study in the Chicago region.
Environ Plann B Plann Des. 2003;30(6):865-884. doi: 10.1068/b29120.McGrail MR.
Spatial accessibility of primary health care utilising the two step floating catchment area method:
an assessment of recent improvements.
Int J Health Geogr. 2012;11:50. doi: 10.1186/1476-072X-11-50.Cherkin DC, Deyo RA, Volinn E, Loeser JD.
Use of the International Classification of Diseases (ICD-9-CM) to identify hospitalizations
for mechanical low back problems in administrative databases.
Spine (Phila Pa 1976). 1992;17(7):817-825.Crosswalk: Medicare provider/supplier to healthcare provider taxonomy.
CMS website.
cms.gov/Medicare/Provider-Enrollment-and-Certification/MedicareProviderSupEnroll/Downloads/TaxonomyCrosswalk.pdf
Published November 30, 2017. Accessed November 15, 2018.Consumer Price Index.
Bureau of Labor Statistics website.
bls.gov/cpi/. Accessed July 9, 2019.Deyo RA, Cherkin DC, Ciol MA.
Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases.
J Clin Epidemiol. 1992;45(6):613-619. doi: 10.1016/0895-4356(92)90133-8.Davis MA, Mackenzie TA, Coulter ID, Whedon JM, Weeks WB.
The United States chiropractic workforce: an alternative or complement to primary care?
Chiropr Man Therap. 2012;20(1):35. doi: 10.1186/2045-709X-20-35.Cheng SH, Lee TT, Chen CC.
A longitudinal examination of a pay-for-performance program for diabetes care:
evidence from a natural experiment.
Med Care. 2012;50(2):109-116. doi: 10.1097/MLR.0b013e31822d5d36.Costello EJ, Compton SN, Keeler G, Angold A.
Relationships between poverty and psychopathology: a natural experiment.
JAMA. 2003;290(15):2023-2029. doi: 10.1001/jama.290.15.2023.Song Y, Skinner J, Bynum J, Sutherland J, Wennberg JE, Fisher ES.
Regional variations in diagnostic practices [erratum in N Engl J Med. 2010;363(2):198. doi: 10.1056/NEJMx100034].
N Engl J Med. 2010;363(1):45-53. doi: 10.1056/NEJMsa0910881.Finkelstein A, Gentzkow M, Williams H.
Sources of geographic variation in health care: evidence from patient migration.
Q J Econ. 2016;131(4):1681-1726. doi: 10.1093/qje/qjw023.Hill AB.
The environment and disease: association or causation?
Proc R Soc Med. 1965;58:295-300.Davis MA, Anthopolos R, Tootoo J, Titler M, Bynum JPW, Shipman SA.
Supply of healthcare providers in relation to county socioeconomic and health status.
J Gen Intern Med. 2018;33(4):412-414. doi: 10.1007/s11606-017-4287-4.Deyo RA, Jarvik JG, Chou R.
Low back pain in primary care.
BMJ. 2014;349:g4266. doi: 10.1136/bmj.g4266.Srinivas SV, Deyo RA, Berger ZD.
Application of “less is more” to low back pain.
Arch Intern Med. 2012;172(13):1016-1020. doi: 10.1001/archinternmed.2012.1838.Mafi JN, McCarthy EP, Davis RB, Landon BE.
Worsening trends in the management and treatment of back pain
[erratum in JAMA Intern Med. 2015;175(5):869. doi: 10.1001/jamainternmed.2015.1589].
JAMA Intern Med. 2013;173(17):1573-1581. doi: 10.1001/jamainternmed.2013.8992.Davis MA, Onega T, Weeks WB, Lurie JD.
Where the United States Spends its Spine Dollars: Expenditures on Different Ambulatory Services
for the Management of Back and Neck Conditions
Spine (Phila Pa 1976). 2012 (Sep 1); 37 (19): 1693–1701Vogt MT, Kwoh CK, Cope DK, Osial TA, Culyba M, Starz TW.
Analgesic usage for low back pain: impact on health care costs and service use.
Spine (Phila Pa 1976). 2005;30(9):1075-1081. doi: 10.1097/01.brs.0000160843.77091.07.Weinstein JN, Lurie JD, Olson PR, Bronner KK, Fisher ES.
United States’ trends and regional variations in lumbar spine surgery: 1992-2003.
Spine (Phila Pa 1976). 2006;31(23):2707-2714. doi: 10.1097/01.brs.0000248132.15231.fe.Lurie JD, Birkmeyer NJ, Weinstein JN.
Rates of advanced spinal imaging and spine surgery.
Spine (Phila Pa 1976). 2003;28(6):616-620. doi: 10.1097/01.BRS.0000049927.37696.DC.Webster BS, Cifuentes M, Verma S, Pransky G.
Geographic variation in opioid prescribing for acute, work-related, low back pain and associated factors:
a multilevel analysis.
Am J Ind Med. 2009;52(2):162-171. doi: 10.1002/ajim.20655.Chiropractic services in the Medicare program:
payment vulnerability analysis. HHS Office of Inspector General website.
oig.hhs.gov/oei/reports/oei-09-02-00530.pdf
Published March 2005. Accessed November 15, 2018.Inappropriate Medicare payments for chiropractic services.
HHS Office of Inspector General website.
oig.hhs.gov/oei/reports/oei-07-07-00390.pdf
Published May 2009. Accessed November 15, 2018.Hundreds of millions in Medicare payments for chiropractic services
did not comply with Medicare requirements.
HHS Office of Inspector General website.
oig.hhs.gov/oas/reports/region9/91402033.pdf
Published 2016. Accessed November 15, 2018.Davis, MA, Yakusheva, O, Gottlieb, DJ, and Bynum, JP.
Regional Supply of Chiropractic Care and Visits to
Primary Care Physicians for Back and Neck Pain
J American Board of Family Medicine. 2015 (Jul); 28 (4): 481–490
Return to OPIOID EPIDEMIC
Return to COST-EFFECTIVENESS
Since 8-16-2019


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |