

The Association of Complementary and Alternative
Medicine Use and Health Care Expenditures
for Back and Neck ProblemsThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Medical Care 2012 (Dec); 50 (12): 1029–1036 ~ FULL TEXT
OPEN ACCESS Martin, Brook I. PhD MPH; Gerkovich, Mary M. PhD; Deyo, Richard A. MD, MPH;
Sherman, Karen J. PhD, MPH; Cherkin, Daniel C. PhD; Lind, Bonnie K. PhD;
Goertz, Christine M. DC, PhD; Lafferty, William E. MD
The Geisel School of Medicine at Dartmouth &
Dartmouth-Hitchcock Medical Center,
Department of Orthopaedics,
Lebanon, NH
FROM: Weeks ~ JMPT 2016 (Feb)BACKGROUND: Health care costs associated with use of complementary and alternative medicine (CAM) by patients with spine problems have not been studied in a national sample.
OBJECTIVES: To estimate the total and spine-specific medical expenditures among CAM and non-CAM users with spine problems.
RESEARCH DESIGN: Analysis of the 2002-2008 Medical Expenditure Panel Survey.
SUBJECTS: Adults (above 17 y) with self-reported neck and back problems who did or did not use CAM services.
MEASURES: Survey-weighted generalized linear regression and propensity matching to examine expenditure differences between CAM users and non-CAM users while controlling for patient, socioeconomic, and health characteristics.
RESULTS: A total of 12,036 respondents with spine problems were included, including 4306 (35.8%) CAM users (40.8% in weighted sample). CAM users had significantly better self-reported health, education, and comorbidity compared with non-CAM users. Adjusted annual medical costs among CAM users was $424 lower (95% confidence interval: $240, $609; P<0.001) for spine-related costs, and $796 lower (95% confidence interval: $121, $1470; P=0.021) for total health care cost than among non-CAM users. Average expenditure for CAM users, based on propensity matching, was $526 lower for spine-specific costs (P<0.001) and $298 lower for total health costs (P=0.403). Expenditure differences were primarily due to lower inpatient expenditures among CAM users.
CONCLUSIONS: CAM users did not add to the overall medical spending in a nationally representative sample with neck and back problems. As the causal associations remain unclear in these cross-sectional data, future research exploring these cost differences might benefit from research designs that minimize confounding.
From the FULL TEXT Article:
Introduction
Complementary and alternative medicine (CAM) includes professional services provided by chiropractic, homeopathic and naturopathic physicians, herbalists, acupuncturists and massage therapists.(Kaptchuk and Eisenberg 2001) As insurance coverage has become more widespread, CAM use among patients with spine problems has increased.(Eisenberg, Davis et al. 1998; Pelletier and Astin 2002; Nahin, Barnes et al. 2009) For example, the number of adults in the United States who sought chiropractic care, the most common type of CAM used by people with spine problems, increased 57% from 1997 to 2006.(Davis, Sirovich et al. 2010)
The financial impact of increased CAM use has been hotly debated. Some have argued that increased use of CAM services reduces the need for more expensive medical care; but others believe that CAM use increases costs because it supplements medical care rather than replacing it. (Metz, Nelson et al. 2004) Concerns that CAM coverage increases health care costs for the general population are not supported by claims data from large insurers or cost-effectiveness studies. (Legorreta, Metz et al. 2004; Sarnat and Winterstein 2004; Haas, Sharma et al. 2005; Nelson, Metz et al. 2005; Grieves, Menke et al. 2009; Liliedahl, Finch et al. 2010; Lind, Lafferty et al. 2010) However, such findings have not been examined using a national sample to estimate the impact of CAM use on total health care costs or for specific types of services (e.g., inpatient, outpatient, prescriptions, and emergency services).
Although a finding of lower expenditures among CAM users with back pain would be consistent with the hypothesis that it obviates the need for more expensive medical care, it might also reflect differences in demographic, clinical and treatment preferences between CAM and non-CAM users. For example, CAM-users are younger, more physically active, less likely to be obese, and have higher educational status and income compared to non-CAM users.(Eisenberg, Davis et al. 1998; Ndetan, Bae et al. 2009) Using data from a nationally representative survey of health care utilization and cost, we estimated differences in the total and spine-specific annual expenditures among CAM and non-CAM users with self-reported spine problems. Two methods (linear regression and propensity score matching) were used to adjust these estimates for observed demographic, clinical, socioeconomic, and health status differences between CAM and non-CAM users.
Methods
Data Source
We examined data from 2002 to 2008 using the Medical Expenditure Panel Survey (MEPS), an annual cross-sectional survey of non-institutionalized U.S. household health care utilization that is supplemented by provider and employer records.(AHRQ 2010) Participants in MEPS are a subsample of participants in the previous year’s National Health Interview Survey. The MEPS data include sampling weights and survey design variables that allow researchers to produce unbiased national estimates of expenditures, utilization and self-reported health status.
We linked unique respondent identifiers in the demographic files to their separate “event” files containing medical encounter details for the following service categories: outpatient care, inpatient care, prescription medication files, and emergency department visits. We performed separate analyses for each type of service category. Many patients have multiple types of events (e.g. both prescription medication and outpatient visits), so these subgroups of service categories are not mutually exclusive.
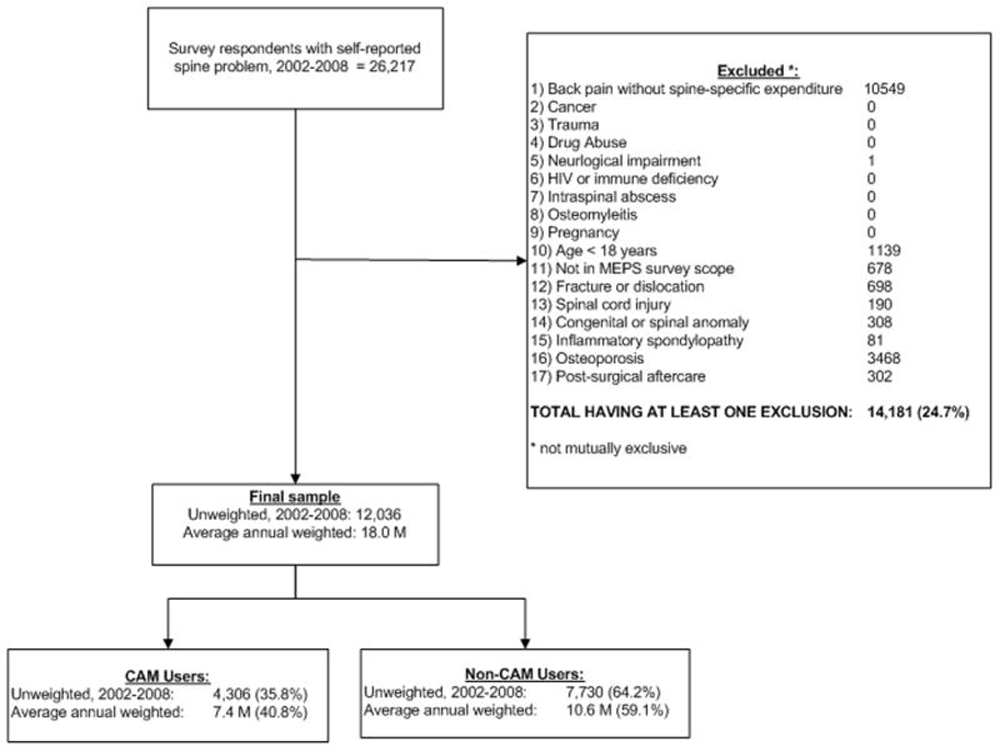
Figure 1 Average annual national estimates of utilization and expenditures were obtained by dividing the weighting variable by seven, since we combined data from seven years. Figure 1 describes the case selection, the number of survey respondents, as well as the proportion of our sample who were CAM-users.
Sample Selection
We used the International Classification of Disease, 9th revision, Clinical Modification (ICD-9-CM) to identify survey respondents with back and neck problems. We performed this analysis at the Agency for Healthcare Research and Quality’s Data Center in order to have access to fully-specified ICD-9 codes. Publicly available MEPS files are truncated at the 3-digit level to protect respondent confidentiality. Previous studies have used ICD-9-CM codes for capturing spine conditions.(Cherkin, Deyo et al. 1992; Martin, Deyo et al. 2008) Patient-reported medical conditions are translated into ICD-9-CM codes by MEPS survey administrators and provider surveys. We searched all available diagnosis codes for each respondent to identify those who had at least one medical encounter for a back or neck problem. We then identified all inpatient, outpatient, emergency and prescription events for these respondents. We searched all three diagnosis fields for each event record to identify those that were specifically related to a spine problem. The order that diagnosis codes were entered into the diagnosis fields did not matter.
Respondents were grouped into their most severe spinal diagnosis using a mutually-exclusive hierarchy of spinal pathology that we developed with our clinical colleagues. In order of decreasing severity, this hierarchy included codes for scoliosis, spondylolisthesis, stenosis, herniated disc (with or without myelopathy), degeneration (e.g. spondylosis), and spinal sprains or strains.
Exclusions We excluded patients with non-degenerative spinal pathologies such as spinal fracture, vertebral dislocation, spinal cord injury, inflammatory spondylopathy, myelopathy, osteoporosis, neurological impairment, osteomylitis, or who had post-operative spinal care. We further excluded patients who had cancer, trauma, fractures, drug abuse, HIV or immune deficiencies, or were pregnant. Finally, we limited our analysis to those over age 17. Classifying CAM users
In 2002, MEPS introduced a new variable to describe 16 types of medical providers. Using this information, we defined a “CAM user” as someone having at least one visit to a doctor of chiropractic, massage therapist, homeopathic provider, acupuncturist, or “other CAM provider” (without further information). Our primary analysis focused on differences between CAM and non-CAM users. “Non-CAM” users were patients who had at least one conventional medical care visit for a spine-related problem (patients who self-reported back pain, but did not have any spine-specific medical visits were excluded). Categorizing a person as a CAM user was based on visits for all reasons, and was not necessarily related to the spine problem. We performed additional analyses focused on expenditure differences between users and non-users of chiropractic care exclusively, while excluding those who used other types of CAM (whether it was in addition to chiropractic care or not), because chiropractic care constituted approximately 75% of all CAM use.
Expenditures
Medical expenditures included all payments made by private insurance, Medicaid, Medicare, patient out-of-pocket costs and other recorded payment sources for office-based or hospital-based outpatient visits, inpatient stays, prescription medications, and emergency department visits. All services incurred during a hospital stay, including direct hospital care, diagnostic tests and procedures, imaging studies, and laboratory work were included as inpatient expenditures. Over-the-counter medications, services provided by free-standing radiology clinics, medical supplies or equipment and dental expenditure were not included in the analysis.
Two costing methods, a direct and an incremental method, were used to estimate expenditures. These methods have different underlying assumptions about how expenditures are related to spine problems. The direct method includes only those costs specifically identified as being spine related (i.e. the event is recorded with a spine-related diagnosis code). The incremental approach includes differences in cost for all care, whether or not they are specifically spine-related (e.g. medical visits for treatment of depression). The difference in mean expenditure between CAM and non-CAM users for all medical care is “attributed” to differences due to CAM use. The incremental method is therefore a more holistic approach that includes potential excesses (or reductions) in expenditures among CAM users whether or not these differences are coded as being spine related. Both methods have been commonly reported in the literature for musculoskeletal and spinal conditions.(AAOS 2008)
Health Status
Multiple self-reported measures of health and functional status are collected from MEPS respondents. These include: the Short Form-12 Physical Component Summary (PCS) and Mental Component Summary (MCS); perceived physical and mental health (dichotomized as “fair-poor” versus “good-excellent”); any social, work and physical functioning limitations (coded as “any” versus “none”); and needed help for Instrumental Activities of Daily Living (IADL). Specifically, IADL asks respondents whether they need help with tasks such as taking medications, preparing meals, doing laundry, or going shopping. We dichotomized IADL to report the effect of having any limitation on function.
Covariates
Patient characteristics in MEPS include age, sex, race, ethnicity, education, marital status, US census region, health insurance status, family income, and whether the respondent was unemployed at any time during the year. Health insurance was coded as “Medicare”, “Medicaid”, “Private insurance only”, and “Uninsured”. Family income was defined relative to the federal poverty level (“poor”, “near poor”, “low”, “middle”, “high”). Finally, we used Quan’s version of the Charlson Index to account for comorbidity. (D’Hoore, Bouckaert et al. 1996)
Analysis
We identified the total number of survey respondents with spine problems, and grouped them based on whether or not they reported any health care utilization delivered by a CAM provider. Differences in the distribution of both patient characteristics and health status measures between CAM and non-CAM users were compared using chi-square comparisons on the weighted data (or by using t-test for age, a continuous variable). Within each service category we examined differences in the overall and spine-specific number of events between CAM and non-CAM users.
We then compared the unadjusted mean annual medical expenditures between CAM and non-CAM users for overall medical care (incremental methods), as well as spine-specific care (direct method). We estimated costs using a generalized linear regression model with a gamma distribution and log link function to account for the skewed nature of cost data. The selection of this distributional family was informed by the Modified Park Test.(Glick HA 2007) To the unadjusted model we then sequentially added the variables for 1) patient and disease characteristics (age group, sex, insurance, comorbidity, and spinal diagnosis); 2) socioeconomic factors (income relative to the federal poverty level, education, work status, and U.S. census region), and 3) self-reported health status (activity limitation and perceived health). The fully adjusted model included all potential covariates except when evidence of multicolinearity was found among health measures.
To present the average differences in adjusted costs between CAM and non-CAM users, we weighted each observation using beta-coefficients associated with the corresponding variables from our regression models. This produced the normative cost for each patient based on the experience of patients with similar characteristics. We then reported the difference in these average costs between CAM and non-CAM users.
Because of selection bias concerns, we conducted additional analyses using propensity score matching to estimate differences in costs. Propensity score matching is a non-experimental sampling method that produces a non-CAM group whose distribution on observed covariates is similar to that of CAM users. We calculated a propensity score through an iterative process of balancing the properties among those with the same predicted probability for using CAM, based on the variables that were included in our fully adjusted regression model.(Guo S. 2010) To create this balance, only CAM and non-CAM users whose distributions of the propensity score overlapped were used as a basis for inferences (known as the “region of common support”). Each CAM user was then matched to a single non-CAM user with the most similar propensity score (known as “nearest-neighbor” matching.) Matching on propensity score is more efficient than including a propensity score in a regression model, results in the least amount of selection bias, and is a common approach when test and control groups vary in size.(Austin 2011) The average treatment effect of CAM use on expenditure was then estimated using 1000 bootstrap samples from the matched sample.
All analyses were performed using StataMP, version 11.0 (Stata Corp, College Station, TX) and incorporated weighting and design variables to account for multistage sampling methods. Hypothesis testing was conducted using an alpha level set at 0.05 based on the survey design degree of freedom. The study received a minimal risk approval from the University of Missouri-Kansas City Institutional review board.
Methods
Population
Data were analyzed for 12,036 survey respondents for the years 2002 through 2008 who met our criteria, representing an estimated 18.0 million people annually (figure 1). Of these, 40.8% were CAM users. Chiropractic care was used by 75% of CAM users, followed by 18.8% who used massage, 6.9% using acupuncture, 4.5% for unspecified CAM providers, and 3.4% using homeopathic physicians.

Table 1 CAM users were significantly younger, and most prevalent in the Midwest and least prevalent in the South. They were more likely to be white, non-Hispanic, privately insured, and employed, while less likely to be widowed, divorced, or separated (Table 1). CAM users also had higher family incomes, less comorbidity, and were more likely to be college-educated compared to non-CAM users.
The majority (60.9%) of patients had spine degenerative conditions, followed by herniated disc (23.8%), sprains and strains (10.7%), scoliosis (2.7%), stenosis (2.5%), and spondylolisthesis (0.4%). Degenerative disc disease and scoliosis were more common diagnoses among CAM than non-CAM users. A diagnosis of disc herniation was less common among CAM users.
Health Status

Table 2 Table 2 presents differences in self-reported health status between CAM and non-CAM respondents with spine problems. CAM users reported significantly better levels of perceived physical and mental health, as well as fewer physical, functional, social and disabling limitations. The greatest differences were for physical functioning and perceived health status. For example, 17.8% of CAM users compared to 32.6% of non-CAM users reported physical functioning limitations (p<0.001). Norm-based SF-12 physical and mental component scores were lower (worse) among non-CAM users. These differences in the SF-12 summary scores were statistically significant but not clinically meaningful. Moreover, their scores were not substantially lower than those of the general population.
Expenditures

Table 3

Table 4 Among respondents in our study, the mean unadjusted annual medical cost among CAM users was $2,495 (95% CI $1,774 – 3,216) lower than that of non-CAM users (p<0.001) for total health care costs (Table 3), and $685 (95%CI $497 –$872) lower for spine-specific health care services (p<0.001; Table 4). After adjusting for patient characteristics, socioeconomic differences, and health status, the average annual medical cost for all health care was $796 lower (95% CI $121 – $1470) for CAM users than for non-CAM users (p=0.021), and $424 (95% CI $240 – $609) lower for spine-specific health care services (p<0.001).
Among CAM users, the proportion of outpatient expenditures that were specifically for CAM services was 21.7% (95%CI 20.2, 23.4) for total health care, and 63.5% (95%CI 59.3, 67.8) for spine-specific care.
Differences in both total and spine-specific expenditures were primarily attributed to significantly lower inpatient expenditures among CAM users. After excluding the inpatient service category, we found no difference in total or spine-specific medical expenditures between CAM and non-CAM users.
All but 60 of the 12,036 survey respondents were included in the region of common support (see Methods), and were included in the propensity score matching analyses. In contrast to the regression analysis, the average treatment effect for CAM use on total expenditures was not statistically significant. The total annual expenditures among CAM users were $298 lower than non-CAM users for total care (p = 0.403). However, even with the propensity-matching method, CAM users had significantly lower spine-specific expenditures ($526 lower than non-CAM users; p < 0.001).
Similar patterns of utilization and costs were observed when we considered only patients who did or did not use chiropractic care, while excluding all other types of CAM use from the analysis.
Conclusions
We observed significantly lower overall and spine-specific medical costs among CAM users compared to non-CAM users in a regression model adjusted for patient characteristics, diagnosis, socioeconomic factors, and health status. The lower total costs among CAM users was primarily attributable to their lower expenditures for inpatient services. After excluding inpatient expenditures, there was no difference in spine-specific or overall medical expenditures between CAM and non-CAM users.
As with any non-randomized study, selection bias is a concern when comparing costs of CAM users to non-users. We found that CAM users had significantly better self-reported measures of health status, lower comorbidity, more private insurance, and higher socioeconomic status compared to non-CAM users. These factors are also likely to be related to expenditures. Thus, the observed cost differences associated with CAM use may differ from those that would be observed in a randomized comparison. Indeed, we found that adjusting our analysis for observed differences largely attenuated the cost differences between CAM and non-CAM users. And, by further matching CAM users to non-CAM users who had a similar propensity scores, we found that the magnitude of the effect for CAM use on total health care expenditures was largely attenuated compared to the effects found in the regression models, and that this difference was no longer statistically significant. Nevertheless, even with propensity matching, spine-specific expenditures were significantly lower among CAM users compared to non-users.
A major strength of our study is that it is based on a large and nationally-representative sample, rather than on data from a select clinical study or from a specific health network. However, there are some limitations. Although the use of ICD-9-CM codes is common in spine research, the codes lack specific clinical detail such as disease severity and duration. Even with multiple adjustments for observed group differences, unobserved factors may exist that could explain the remaining differences in costs. It is uncertain whether unmeasured confounding factors could explain the observed difference in costs between CAM and non-CAM users. Finally, differences in healthcare utilization and expenditures between CAM and non-CAM users may be the cause or consequence of differences in health status. Cross-sectional data preclude causal inferences regarding CAM use and health status, but allow us to examine the association of CAM use with expenditures after adjusting for differences in health status. The self-reported health status measures in this study may not reflect baseline values as these data may have been collected either before or after spine-related visits. Future research exploring these differences might benefit from randomized designs or statistical methods (e.g. instrumental variable analysis) that further seek to identify and minimize unmeasured confounding.
Our findings are generally consistent with other studies that have reported that CAM use does not significantly increase overall medical spending.(Haas, Sharma et al. 2005; Nelson, Metz et al. 2005; Grieves, Menke et al. 2009; Lind, Lafferty et al. 2010) Our study is the first to generalize this findings to a nationally representative sample. Whether expanding CAM coverage will retain a budget neutral impact is unclear. On the basis of cost-effectiveness, the UK’s National Institute for Health and Clinical Excellence (NICE) has recommended expanded use of early conservative treatments in response to back pain, and a recent study has shown reduced rates of surgery among those receiving early physical therapy for common acute back pain.(Mayor 2009; Gellhorn, Chan et al. 2010) On the other hand, a Medicare demonstration project recently reported that expanding chiropractic services to include payment for physical examinations, imaging and additional manual services significantly increased costs.(Federal Register 2009) However, concerns exist regard the generalizability of this finding. Costs for all users with neuromuskuloskeletal complaints were significantly higher in demonstration sites when compared to control sites, both before and during the demonstration period. Furthermore, the majority of additional expenditures occurred at one site (Illinois, primarily Chicago and its suburbs). Costs in other demonstration areas either decreased or increased only slightly when compared to control sites.
Our findings are consistent with the hypothesis that, after accounting for clear differences between CAM and non-CAM users, expenditures for CAM users are not higher than those of non-CAM users, and even suggest possible cost savings. Discretionary clinician decisions are the predominant driver of medical spending for back pain; and, despite evidence-based clinical guidelines that recommend conservative treatment approaches, trends suggest increases in the use of advanced imaging, epidural steroid injections, opioid analgesics, and surgical treatments for those with back pain.(Deyo, Mirza et al. 2009) These services are often provided with the expectation that they will obviate the need for more invasive and longer duration therapies. As the health care costs for spine-related pain continue to grow in the absence of evidence of corresponding improvements in population-based outcomes, there is a major need for research that clarifies how the timing, frequency, and effectiveness of CAM services affect subsequent rates of spinal surgery, opioid prescription, epidural steroid injections, and other expensive and invasive treatments for patients with back pain.
Acknowledgments
Funding for this project was provided by grant #R01AT005061 from the National Center for Complementary and Alternative Medicine (NCCAM). The findings and conclusions expressed are solely those of the author(s) and do not necessarily represent the views of the NCCAM, or any agency of the Federal Government.
Contributor Information
Brook I. Martin, The Geisel School of Medicine at Dartmouth, Dartmouth-Hitchcock Medical Center, Department of Orthopaedics, HB7541, One Medical Center Drive, Lebanon, NH 03756, Phone (603) 653-9167, Fax (603) 653-3554.
Mary M. Gerkovich, Office of Health Services & Public Health Outcomes Research, Department of Biomedical and Health Informatics, University of Missouri-Kansas City, School of Medicine, 5E-100 Center for Behavioral Medicine, Kansas City, Missouri 64108-2792, 816-235-1322 (office), 816-283-8563 (fax)
Richard A. Deyo, Kaiser Center for Health Research, Departments of Family Medicine, Medicine, Public Health and Preventive Medicine, and the Center for Research on Occupational and Environmental Toxicology, Oregon Health and Science University; and the Kaiser Permanente Center for Health Research. 3181 SW Sam Jackson Park Rd, Mail code FM, Portland, OR 97239, Phone (503) 494-1694, Fax (503) 494-2746.
Karen J. Sherman, Group Health Research Institute; Group Health Cooperative, 1730 Minor Ave, Ste 1600, Seattle, WA 98101, Phone (206) 287-2426, Fax (206) 287-2871.
Daniel C. Cherkin, Group Health Research Institute; Group Health Cooperative, 1730 Minor Ave, Ste 1600, Seattle, WA 98101, Phone: (206) 287-2875, Fax: (206) 287-2871.
Bonnie K. Lind, Saint Luke’s Health System, 190 East Bannock St., Boise, ID 83712, Phone (208) 381-5378, Fax (208) 381-8711, University of Washington.
Christine M. Goertz, Vice Chancellor for Research and Health Policy, Palmer Center for Chiropractic Research, Palmer College of Chiropractic, 1000 Brady Street, Davenport, IA 52803, Phone: (563) 884-5159, Fax: (563) 884-5227.
William E. Lafferty, Department of Internal Medicine, Hicklin Endowed Chair, Office of Health Services and Public Health Outcomes Research, University of Missouri-Kansas City, 1000 E. 24th Street, 5th Floor, Kansas City, Missouri, Phone (816) 235-1074, Fax (816) 283-8563.
References
T.J. Kaptchuk, D.M. Eisenberg
Varieties of Healing 2: A Taxonomy of Unconventional Healing Practices
Annals of Internal Medicine 2001 (Aug 7); 135 (3): 196–204Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, Kessler RC.
Trends in Alternative Medicine Use in the United States, 1990 to 1997:
Results of a Follow-up National Survey
JAMA 1998 (Nov 11); 280 (18): 1569–1575Nahin RL. Barnes PM. Stussman BJ. Bloom B.
Costs of Complementary and Alternative Medicine (CAM)
and Frequency of Visits to CAM Practitioners:
United States, 2007
National Health Statistics Reports 2009 (Jul 30); (18): 1–14Pelletier KR, Astin JA.
Integration and reimbursement of complementary and alternative medicine by managed care and insurance providers: 2000 update and cohort analysis.
Altern Ther Health Med. 2002;8(1):38–9. 42, 44Davis, MA, Sirovich, BE, and Weeks, WB.
Utilization and Expenditures on Chiropractic Care
in the United States from 1997 to 2006
Health Serv Res. 2010 (Jun); 45 (3): 748-761Metz, RD, Nelson, CF, LeBrot, T, and Pelletier, KR.
Chiropractic Care: Is It Substitution Care or Add-on Care in Corporate Medical Plans?
J Occup Environ Med 2004 (Aug); 46 (8): 847–855Legorreta, AP, Metz, RD, Nelson, CF, Ray, S, Chernicoff, HO, and Dinubile, NA.
Comparative Analysis of Individuals With and Without Chiropractic Coverage:
Patient Characteristics, Utilization, and Costs
Archives of Internal Medicine 2004 (Oct 11); 164 (18): 1985–1892Sarnat, RL and Winterstein, J.
Clinical and Cost Outcomes of an Integrative Medicine IPA
J Manipulative Physiol Ther 2004 (Jun) ; 27 (5): 336–347Lind BK, et al.
Comparison of health care expenditures among insured users and nonusers of complementary and alternative medicine in Washington State: a cost minimization analysis.
J Altern Complement Med. 2010;16(4):411–7.Nelson CF, Metz RD, LaBrot T.
Effects of a Managed Chiropractic Benefit on the Use of Specific Diagnostic
and Therapeutic Procedures in the Treatment of Low Back and Neck Pain
Journal of Manipulative and Physiological Therapeutics 2005 (Oct); 28 (8): 564–569Grieves B, Menke JM, Pursel KJ.
Cost Minimization Analysis of Low Back Pain Claims Data for
Chiropractic vs Medicine in a Managed Care Organization
J Manipulative Physiol Ther 2009 (Nov); 32 (9): 734–739Haas M, Sharma R, Stano M.
Cost-effectiveness of Medical and Chiropractic Care for Acute and Chronic Low Back Pain
J Manipulative Physiol Ther 2005 (Oct); 28 (8): 555–563Liliedahl RL, Finch MD, Axene DV, Goertz CM.
Cost of Care for Common Back Pain Conditions Initiated With Chiropractic
Doctor vs Medical Doctor/Doctor of Osteopathy as First Physician:
Experience of One Tennessee-Based General Health Insurer
J Manipulative Physiol Ther 2010 (Nov); 33 (9): 640–643Ndetan HT, et al.
Characterization of health status and modifiable risk behavior among United States adults using chiropractic care as compared with general medical care.
J Manipulative Physiol Ther. 2009;32(6):414–22.AHRQ. Medical Expenduture Panel Survey. 2010
Available from: http://www.meps.ahrq.gov/mepsweb/Martin BI, Deyo RA, Mirza SK, Turner JA, Comstock BA, Hollingworth W, et al.
Expenditures and Health Status Among Adults With Back and Neck Problems
JAMA 2008 (Feb 13); 299 (6): 656–664Cherkin DC, et al.
Use of the International Classification of Diseases (ICD-9-CM) to identify hospitalizations for mechanical low back problems in administrative databases.
Spine (Phila Pa 1976) 1992;17(7):817–25.AAOS.
The Burden of Musculoskeletal Diseases in the United States.
American Academy of Orthopaedic Surgeons; Rosemont, IL: 2008.D’Hoore W, Bouckaert A, Tilquin C.
Practical considerations on the use of the Charlson comorbidity index with administrative data bases.
J Clin Epidemiol. 1996;49(12):1429–33.Glick HA, DJ, Sonnad SS, Polsky D.
In: Economic Evaluation in Clinical Trials.
Gray BA, editor. Oxford: Oxford University Press; 2007.Guo S, FM .
Advanced Quantitative Techniques in the Social Sciences.
Washington D.C: Sage Publications; 2010.
Propensity Score Analysis: Statistical Methods and Applications.Austin PC.
Comparing paired vs non-paired statistical methods of analyses when making inferences about absolute risk reductions in propensity-score matched samples.
Stat Med. 2011;30(11):1292–301.Federal Register.
Discussion on Chiropractic Services Demonstration Project.
Federal Register. 2009;74(226):61926–61928.Mayor S.
NICE recommends early intensive management of persistent low back pain.
BMJ. 2009;338:b2115.Gellhorn AC, et al.
Management Patterns in Acute Low Back Pain: The Role of Physical Therapy.
Spine (Phila Pa 1976) 2010Deyo RA, et al.
Overtreating Chronic Back Pain: Time to Back Off?
J Am Board Fam Med. 2009 (Jan); 22 (1): 62–68
Return to CHRONIC NECK PAIN
Return to COST-EFFECTIVENESS
Return to the ALT-MED/CAM ABSTRACTS Page
Since 11-16-2012


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |