

Comparative Effectiveness of Usual Care With or Without
Chiropractic Care in Patients with Recurrent
Musculoskeletal Back and Neck PainThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Gen Intern Med. 2018 (Sep); 33 (9): 1469–1477 ~ FULL TEXT
OPEN ACCESS Charles Elder, MD MPH, Lynn DeBar, PhD MPH, Cheryl Ritenbaugh, PhD MPH, John Dickerson, PhD, William M. Vollmer, PhD, Richard A. Deyo, MD MPH, Eric S. Johnson, PhD, and Mitchell Haas, DC MA
Kaiser Permanente Center for Health Research,
Portland, OR, USA.
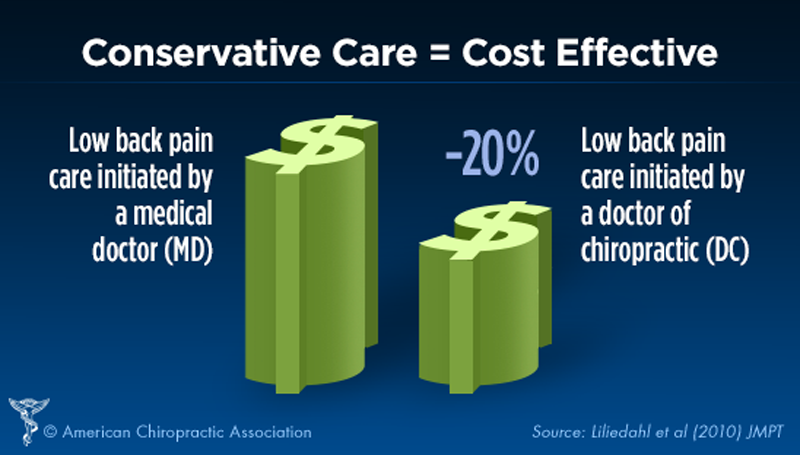
FROM: Liliedahl ~ JMPT 2010 (Nov)BACKGROUND: Chiropractic care is a popular alternative for back and neck pain, with efficacy comparable to usual care in randomized trials. However, the effectiveness of chiropractic care as delivered through conventional care settings remains largely unexplored.
OBJECTIVE: To evaluate the comparative effectiveness of usual care with or without chiropractic care for patients with chronic recurrent musculoskeletal back and neck pain.
STUDY DESIGN: Prospective cohort study using propensity score-matched controls.
PARTICIPANTS: Using retrospective electronic health record data, we developed a propensity score model predicting likelihood of chiropractic referral. Eligible patients with back or neck pain were then contacted upon referral for chiropractic care and enrolled in a prospective study. For each referred patient, two propensity score-matched non-referred patients were contacted and enrolled. We followed the participants prospectively for 6 months.
MAIN MEASURES: Main outcomes included pain severity, interference, and symptom bothersomeness. Secondary outcomes included expenditures for pain-related health care.
KEY RESULTS: Both groups' (N = 70 referred, 139 non-referred) pain scores improved significantly over the first 3 months, with less change between months 3 and 6. No significant between-group difference was observed. (severity – 0.10 (95% CI – 0.30, 0.10), interference – 0.07 (– 0.31, 0.16), bothersomeness – 0.1 (– 0.39, 0.19)). After controlling for variances in baseline costs, total costs during the 6–month post-enrollment follow-up were significantly higher on average in the non-referred versus referred group ($1,996 [SD = 3874] vs $1,086 [SD = 1212], p = .034). Adjusting for differences in age, gender, and Charlson comorbidity index attenuated this finding, which was no longer statistically significant (p = .072).
There are more articles like this @ our: Cost-Effectiveness of Chiropractic Page CONCLUSIONS: We found no statistically significant difference between the two groups in either patient-reported or economic outcomes. As clinical outcomes were similar, and the provision of chiropractic care did not increase costs, making chiropractic services available provided an additional viable option for patients who prefer this type of care, at no additional expense.
KEYWORDS: alternative medicine; back pain; chiropractic; chronic musculoskeletal pain; comparative effectiveness; complementary and integrative medicine; managed care; neck pain; primary care; propensity scoring; spinal manipulation
From the FULL TEXT Article:
INTRODUCTION
Chronic musculoskeletal pain remains a substantial clinical and public health challenge. [1, 2] In 2008, the total financial cost of pain to society, including both health care costs and lost productivity, was estimated at $560 to $635 billion. [3] Spinal disorders are the fourth most common primary diagnosis for office visits in the USA, [4] and are reported by over a third of patients presenting with musculoskeletal complaints. [5] Conventional management commonly includes nonsteroidal antiinflammatory drugs, skeletal muscle relaxants, and opioids, which are of modest benefit and are associated with serious toxicities. [6, 7]
Chiropractic care is popular among patients, [8, 9] with efficacy for treating back and neck pain comparable to usual care in experimental randomized controlled trial (RCT) settings. [10–12] However, the effectiveness of chiropractic care as actually delivered in routine conventional and integrative medicine practice remains largely unexplored. Rigorous evaluation of such routine care is complicated by numerous methodological challenges. In comparative effectiveness research of this type, RCT study designs may be logistically difficult or even infeasible, where the requirements for informed consent, the mechanics of the randomization process, the protocols for blinding, and other experimental constraints often directly conflict with the flow of routine office care. Further, even if feasible, imposing these research constraints is likely to alter care as actually delivered in everyday clinical settings. Prospective cohort studies provide a compelling alternative, but introduce challenges in identifying an appropriate control group that minimizes confounding or bias.
Propensity scores represent one viable approach to controlling for confounding in observational studies. However, propensity scores are typically applied in retrospective analyses and, to our knowledge, have not been previously used to recruit and match subjects on an ongoing basis in prospective cohort studies requiring the collection of patient-reported outcomes. [13] We sought to evaluate the comparative effectiveness of usual care with or without chiropractic care as provided to patients in an established health maintenance organization (HMO), using novel and scientifically rigorous methods. Specifically, we used data from retrospective electronic health record (EHR) and administrative databases to develop a propensity score model describing the likelihood of a patient’s being referred for chiropractic care, [13] and then implemented a prospective cohort study comparing patients with chronic musculoskeletal pain who were referred for chiropractic care with propensity score-matched controls who were not.
METHODS
Design
The Relief project is a multi-phased study evaluating acupuncture and chiropractic care for patients with chronic musculoskeletal pain in an HMO setting. Full descriptions of our study design and propensity score methodology have been previously published. [13, 14] In brief, the project featured two prospective cohort studies evaluating the effectiveness of usual care with or without acupuncture, and usual care with or without chiropractic care. This paper presents data from the chiropractic study; results of the acupuncture study will be published separately.
Setting
The study was conducted at Kaiser Permanente Northwest (KPNW), an HMO serving approximately 550,000 members in the metropolitan Portland area. KPNW provides chiropractic care to patients through a contracted network of chiropractors at Complementary Health Plans (CHP). Most KPNW members are eligible for referral to a CHP chiropractor by a KPNW clinician for a limited number of visits. Over the period of this project, KPNW policy allowed patient referral for chiropractic care in the setting of acute (3 months or less) non-radicular back or neck pain. Importantly, those with an acute exacerbation of a chronic back or neck pain syndrome were eligible for referral.
Participants
We developed a study-specific chronic pain registry employing a comprehensive International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code list to identify patients whose pattern of clinical diagnoses in the EHR suggested chronic musculoskeletal pain. [14] (Appendix 1) The sample was operationally defined as including members at least 18 years old with ≥ 3 outpatient pain-related encounters evident in the EHR, spanning at least 180 days but no more than 18 months.
During the course of the study (August 1, 2013 to August 31, 2015), we used the EHR to electronically monitor the routine care delivered at KPNW to registry patients. We contacted and invited patients to enroll in the study immediately upon chiropractic referral. As this was an observational study, the decision to initiate chiropractic referral, or not, was made between physician and patient in the context of the delivery of routine care in the clinics. Exclusion criteria included a baseline score of < 4 on the (0–10) scale for pain bothersomeness, non-persistent pain, current or recent (last 6 months) chiropractic care, pregnancy, or plans to move out of the area. Given both the study sample definition and the KPNW medical necessity criteria for chiropractic care, most eligible patients had chronic pain with acute exacerbations of back or neck pain. The patients were screened and provided written consent, and baseline measures were collected.
For each referred patient enrolled, we targeted enrollment of two control patients with chronic musculoskeletal pain who had a recent (previous 10 days) office visit for back or neck pain but were not referred for chiropractic care. These patients were likewise identified through EHR monitoring, contacted, and invited to enroll.We matched patients in the control arm to referred patients based upon gender, pain bothersomeness (difference within ± 2 points), and propensity to be referred for chiropractic care. The latter was based upon a propensity score model developed using retrospective EHR data from 2010, and then validated on 2011 data, before implementation for matching in the 2013 prospective cohort study. The rationale andmethodology for development of the propensity score model were identical to those for the Relief acupuncture cohort, and are described elsewhere.13 Baseline predictive factors ultimately included in the calculation of the propensity score were age; opioid and pain medication use; number of outpatient visits; physical therapy utilization; diagnoses of nonspecific chronic pain, sleep disorders, substance abuse, and anxiety; tobacco abuse; procedures for diagnosing and treating pain; ambulatory Charlson score; andmonths since cohort entry (Appendix 2). Over the course of their study participation, both referred and non-referred patients continued to receive usual care as deemed appropriate by their primary care physicians.
Outcomes
We collected patient-reported measures at baseline and at months 1, 3, and 6.Main Outcome Measures. Two subscales (the four-item pain severity and the seven-item pain interference subscales) from the short form of the Brief Pain Inventory (BPI-SF) [15–17] were used to assess pain and related disability. The BPI has sound psychometrics and has been widely adopted. We also included a measure of how bothered the participants were by their pain. This instrument uses a 0 to 10 scale of Bsymptom bothersomeness,^ where 0 represents Bnot at all bothersome^ and 10 is Bextremely bothersome.^ This question has been frequently used in studies of back pain [18, 19] and shown to have adequate construct validity. [20]
Secondary Outcome Measures, Clinical/Patient Reported. Quality of sleep was measured using the five-item Insomnia Severity Index (ISI) [21–23] We used the Personal Health Questionnaire (PHQ-8) [24] to evaluate depression severity. The PHQ-8 is established as a valid severity measure for depressive disorders in large clinical studies. [24–26] We used the sevenitem Generalized Anxiety Disorder Scale (GAD-7) [27] to screen for anxiety disorders. Health-related quality of life (QOL) was assessed using the five-level EuroQol instrument (EQ-5D). [28] Secondary Outcome Measures, Health Care Costs. We monitored the cost of pain-related outpatient visits (including both conventional and chiropractic care), inpatient hospitalizations, and drugs dispensed for the 6 months prior to and following study entry. We estimated health plan costs (in 2014 US dollars) by applying internal unit costs (developed and tested in previous studies) [29–31] to patient-level utilization measures, with the final cost variable acting as a proxy for HMO resource cost.
Adverse Events. On each of the assessment surveys, we asked the participants to report any adverse events associated with pain treatments.
Data Sources
We collected patient-reported outcomes and adverse events over the phone or online. (Appendix 3) [32]
We used EHR data to determine pain-related and comorbid diagnoses, estimate pain-related health care costs, and calculate Charlson comorbidity index scores. [33] We obtained patient data for the 180 days before and after patient enrollment. The data included ICD-9-CM diagnostic codes and Current Procedural Terminology (CPT) codes for procedures and filled prescription data associated with chronic pain.
Finally, we mailed a questionnaire to chiropractors who cared for study participants to collect information on the treatments they provided (session frequency, reason for referral, and use of specific treatment approaches including joint manipulative procedures, soft tissue manipulative procedures, physical modalities, prescriptions/devices, rehabilitative exercises, and self-care/lifestyle recommendations).
Sample Size
Sample size calculations demonstrated that 100 study participants per group would yield statistical power of approximately 0.90 to detect standardized effect sizes of 0.50 or greater. [14] Using an alpha of 0.025, and given the number of participants actually enrolled, we have statistical power of 0.72 and 0.61 to detect standardized effect sizes of 0.50 or greater for BPI pain interference and severity, respectively. Using a 0.05 alpha, the power calculations are 0.81 for pain interference and 0.71 for pain severity, respectively.
Statistical AnalysisPatient-Reported Outcomes. For pain scores, our primary analytic model was a piecewise continuous, segmented regression model that allowed us to estimate shorter-term (first 3 months, which, given the benefit structure, was the expected maximum duration of chiropractic treatment) and longer-term (second 3 months) changes in pain scores. The model was fit using the mixed procedure in Stata (version 13.1) in order to account for clustering of observations within patients and propensity score deciles, and adjusted for age, gender, and baseline Charlson comorbidity index (dichotomized as 0, Charlson = 0, and 1, Charlson = 1+). We included this parsimonious set of additional control variables because they were considered the factors most likely to confound the relationship between chiropractic referrals and patient outcomes. Similar models were used to analyze the secondary clinical outcomes. We also conducted analyses using only the baseline and 6– month data to assess the net impact of the chiropractic referrals 6 months after enrollment. Here, we used simple linear regression models to predict 6–month outcomes as a function of referral status, again adjusting for the baseline level of the outcome measure and age, gender, and baseline Charlson comorbidity index. Finally, we performed sensitivity analyses which retained only referred patients who actually received chiropractic care and non-referred patients who actually did not receive such care.
Costs. We modeled health care costs using generalized linear models with gamma specification and log link to accommodate the distributional properties of cost data and to avoid interpretation issues associated with backtransformation from transformation models. Model-based cost estimates were presented for the Btypical^ study participant where relevant, [34] and models were adjusted for age, gender, baseline Charlson comorbidity index, and baseline costs.
Missing Data. Each analysis was performed on participants with available data. Multilevel estimation procedures allowed all participants to contribute to estimates if they had at least one observation for primary and secondary outcomes. Models estimating the net impact of the chiropractic referrals 6 months after enrollment required completion of the 6–month follow-up assessment. Costs analyses extracted data from the EHR and thus required continuous health plan enrollment during the 6–month follow- up. Results using multiple imputation with chained equations yielded similar results.
RESULTS
Participants

Figure 1

Table 1 Among potential referred participants, 264 completed screening, 94 screened eligible, and 70 consented and were enrolled (Figure 1). The most common reason for screening ineligibility was undocumented chiropractic care within the preceding 6 months (N = 127). Among potential controls, 717 completed screening, 422 screened eligible, and 139 consented and were enrolled. The most common reasons for screening ineligibility were similarly undocumented chiropractic care within the preceding 6 months (N = 162) and low baseline pain scores (N = 151).
Baseline patient characteristicsThe participants were predominantly Caucasian (90.7%) and female (66.0%), with a mean age of 48.0 years (Table 1). Nearly all had back and/or neck pain. Despite propensity score matching, the patients referred for chiropractic care were less likely than non-referred patients to be involved with litigation, to have depressive symptoms, or to have received physical therapy, spinal injections, or pain clinic specialty care. At 6 months, 89% of the referred patients and 86% of the controls provided follow-up data.
Chiropractic services
Among the referred patients, the mean number of visits with the chiropractor, based upon EHR data, was 4.0 (SD 4.4; median = 3, IQR= 0–7).
Based upon both EHR data and participant self-report, 73% of those referred for chiropractic care actually received such care, while in the non-referred group, 16% sought and received chiropractic care on their own.
Forty chiropractors returned questionnaire responses describing the care for 43 referred patients. Regarding spinal care, 80% of responses reported providing thrust adjustment, 51% segmental mobilization, 31% instrument adjustment, and 21% traction/distraction. For soft tissue manipulative procedures, 52% of responses reported using massage, 42% muscle stretching, 39% point-pressure techniques, and 13% the Graston technique (a method using metal instruments to rub patient muscles). Regarding physical modalities, 60% reported electrical stimulation, 60% hot/cold packs, and 24% ultrasound. For home care, 81% of the responses recommended stretching, 41% core stabilization, 33% resistance strengthening, 11% McKenzie exercises, and 11% proprioceptive drills. Regarding lifestyle recommendations, 61% provided exercise handouts, 33% advised stress reduction, 24% coached regarding injury prevention, and 12%provided dietary and nutritional counseling.
Main Results

Table 2

Table 3

Table 4

Table 5 Patient-Reported Outcomes. For bothersomeness, pain severity, and pain interference, both groups improved significantly over the first 3 months, with much less change between months 3 and 6. None of these changes differed significantly between the referred and non-referred groups in either adjusted (Table 2), unadjusted, or sensitivity analyses. Table 3 presents mean pain scores at the 6–month visit. Although these tended to be lower for the referred than for the non-referred groups, again none of the differences were statistically significant.
We likewise found no significant difference between groups for any secondary clinical outcome measure (Table 2). Similarly, there was no significant difference between groups for any of these outcome measures in terms of the percentage of patients showing clinically significant improvement at 6 months.
Economic Outcomes. As shown in Tables 4 and 5, total costs during the 6–month post-enrollment follow-up were significantly higher on average in the non-referred versus referred group ($1,996 [SD = 3,874] vs $1,086 [SD = 1,212], p = .034) after controlling for differences in baseline costs. Sensitivity analyses demonstrated similar results during the 6–month follow-up, with non-referred patients having higher costs than referred patients ($2,272 [SD = 4,545] vs $819 [SD = 882], p = .020). However, adjusting for differences in age, gender, and Charlson comorbidity index attenuated these differences, which were no longer statistically significant.
Adverse Events
A total of 20 participants reported an adverse event: 14, or 10%, of the participants from the non-referred group and six, or 8.5%, of those referred for chiropractic care. Among the non-referred patients, four (3%) reported an adverse event attributable to medications, four (3%) to physical activity, one (< 1%) to acupuncture treatments, and five (4%) to other factors. Among those referred for chiropractic care, three (4%) reported an adverse event attributable to physical activity and three (4%) potentially to chiropractic care. Of these, one participant noted at 6–month follow-up that although neck pain improved with chiropractic care, hip pain worsened. A second participant indicated worsening pain at 3–month follow-up, but expressed uncertainty as to whether this was attributable to chiropractic treatments or to their discontinuation. A third participant specified chiropractic care as a cause of worsening symptoms at 1–month follow-up, without further details. No serious study-related adverse events were reported.
DISCUSSION
In this prospective cohort study, the patients referred for chiropractic care showed statistically significant improvement comparable to the propensity score-matched non-referred patients for clinical pain-related outcomes. After adjusting for differences in baseline costs, total pain-related health care expenditures during the 6–month post-enrollment follow-up were significantly higher on average in the non-referred versus referred group. Although this result persisted in a sensitivity analysis, and is consistent with previously published retrospective analyses, [35] it did not maintain statistical significance after adjustment for differences in age, gender, and Charlson comorbidity index. As clinical outcomes were generally similar, however, and the provision of chiropractic care clearly did not increase costs, chiropractic care may have to some degree substituted for conventional care, rather than just adding to it. Chiropractic care thus provided an additional clinically viable option for patients who prefer this type of care, at no additional expense.
There were no serious adverse events associated with chiropractic care. Chiropractors reported considerable heterogeneity in the types of modalities offered to patients, and chiropractic care commonly included a substantial component of self-care instruction.
Strengths of this study include the prospective cohort design, incorporating patient-reported outcomes, and employing a novel approach to matching referred patients with controls at baseline using propensity score modeling. The study setting provided a unique opportunity to describe and evaluate chiropractic benefits as actually provided in a conventional HMO setting. Study limitations include a relatively small sample size, as we did not achieve our targeted enrollment. This was largely due to many patients having recently used chiropractic care undetected by the EHR, thus rendering them ineligible for the study. Excluding such individuals from the study may have removed those most likely to use chiropractic care routinely from consideration, thereby limiting generalizability of our findings. Further, our analyses do not distinguish between those with neck pain and back pain, which may likewise limit generalizability. In addition, not everyone who was referred actually sought chiropractic care, while some participants in the non-referred group did receive such care. This would generally blunt real differences that might exist, likely biasing our results toward the null.
Even so, the study provides important insight. We found that referred and non-referred participants had comparable clinical outcomes and that chiropractic referral neither added to health care costs nor introduced significant safety concerns. Data suggest that although two thirds of primary care physicians have recommended chiropractic care to their patients, [36] lack of communication remains a major barrier to care coordination. [37, 38] Better integration of chiropractors into conventional care spine management algorithms could represent a sensible approach to enhancing patient-centered care for patients with chronic musculoskeletal pain. Finally, the project establishes the feasibility of a methodologic alternative for prospectively evaluating the comparative effectiveness of clinical interventions in routine settings for chronic musculoskeletal pain.
Supplementary material
Sources of Funding:
This project was funded by a grant from the National Institutes of Health, Center for Complementary and Integrative Health (R01 AT005896). An earlier version of these data were presented as part of a poster presentation at the International Congress on Integrative Medicine and Health in Las Vegas, in 2016.
Compliance with Ethical Standards:
The Institutional Review Board at Kaiser Permanente Northwest approved all study procedures.
Conflict of Interest:
Dr. Deyo reports royalties from UpToDate for authoring topics on low back pain, an endowment from Kaiser Permanente to Oregon Health and Science University, and a financial gift from NuVasive as part of a lifetime achievement award from the International Society for Study of the Lumbar Spine. For the remaining authors, no conflicts of interest were declared.
References:
Hoy, D., L. March, P. Brooks, F. Blyth, A. Woolf, et al.
The Global Burden of Low Back Pain: Estimates from the Global Burden of Disease 2010 study
Ann Rheum Dis. 2014 (Jun); 73 (6): 968–974Hoy D, March L, Woolf A, et al.
The Global Burden of Neck Pain: Estimates From the Global Burden of Disease 2010 Study
Ann Rheum Dis. 2014 (Jul); 73 (7): 1309–1315Institute of Medicine (IOM)
Relieving Pain in America: A Blueprint for Transforming Prevention,
Care, Education, and Research
Washington, DC: The National Academies Press, 2011.Centers for Disease Control and Prevention.
National Ambulatory Medical Care Survey: 2010 Summary Tables.
www.cdc.gov/nchs/data/ahcd/namcs_summary/2010_namcs_web_tables.pdf
Accessed 05/25/2018.Wiitavaara B, Fahlstrom M, Djupsjobacka M.
Prevalence, diagnostics and management of musculoskeletal disorders in primary health care in Sweden—an investigation of 2000 randomly selected patient records.
J Eval Clin Pract 2017;23(2):325-332.Beebe FA, Barkin RL, Barkin S.
A clinical and pharmacologic review of skeletal muscle relaxants for musculoskeletal conditions.
Am J Ther 2005;12(2):151-171.Von Korff M, Kolodny A, Deyo RA, Chou R.
Long-term opioid therapy reconsidered.
Ann Intern Med 2011;155(5):325-328.Barnes PM , Bloom B , Nahin RL:
Complementary and Alternative Medicine Use Among Adults and Children:
United States, 2007
US Department of Health and Human Services,
Centers for Disease Control and Prevention,
National Center for Health Statistics, Hyattsville, MD, 2008.Elder C, DeBar L, Ritenbaugh C, et al.
Acupuncture and Chiropractic Care: Utilization and Electronic Medical Record Capture
American J Managed Care 2015 (Jul 1); 21 (7): e414–421Bronfort G, Haas M, Evans R, Leininger B, Triano J.
Effectiveness of Manual Therapies: The UK Evidence Report
Chiropractic & Osteopathy 2010 (Feb 25); 18 (1): 3Deyo RA.
The Role of Spinal Manipulation in the Treatment of Low Back Pain
JAMA. 2017 (Apr 11); 317 (14): 1418–1419Paige NM, Myiake-Lye IM, Booth MS, et al.
Association of Spinal Manipulative Therapy with Clinical Benefit and Harm
for Acute Low Back Pain: Systematic Review and Meta-analysis
JAMA. 2017 (Apr 11); 317 (14): 1451–1460Johnson ES, Dickerson JF, Vollmer WM, et al.
The feasibility of matching on a propensity score for acupuncture in a prospective cohort study of patients with chronic pain.
BMC Med Res Methodol 2017;17(1):42.DeBar LL, Elder C, Ritenbaugh C, et al.
Acupuncture and chiropractic care for chronic pain in an integrated health plan: a mixed methods study.
BMC Complement Altern Med 2011;11:118.Cleeland CS, Ryan KM.
Pain assessment: global use of the Brief Pain Inventory.
Ann Acad Med Singap 1994;23(2):129-138.Keller S, Bann CM, Dodd SL, Schein J, Mendoza TR, Cleeland CS.
Validity of the brief pain inventory for use in documenting the outcomes of patients with noncancer pain.
Clin J Pain 2004;20(5):309-318.Tan G, Jensen MP, Thornby JI, Shanti BF.
Validation of the brief pain inventory for chronic nonmalignant pain.
J Pain 2004;5(2):133-137.Cherkin, DC, Deyo, RA, Battie, M, Street, J, and Barlow, W.
A Comparison of Physical Therapy, Chiropractic Manipulation, and Provision of an Educational Booklet
for the Treatment of Patients with Low Back Pain
New England Journal of Medicine 1998 (Oct 8); 339 (15): 1021-1029Patrick DL, Deyo RA, Atlas SJ, Singer DE, Chapin A, Keller RB.
Assessing health-related quality of life in patients with sciatica.
Spine 1995;20(17):1899-1908; discussion 1909.Dunn KM. Croft PR.
Classification of Low Back Pain in Primary Care: Using "Bothersomeness"
to Identify the Most Severe Cases
Spine (Phila Pa 1976). 2005 (Aug 15); 30 (16): 1887–1892Bastien CH, Vallieres A, Morin CM.
Validation of the Insomnia Severity Index as an outcome measure for insomnia research.
Sleep Med 2001;2(4):297-307.Morin CM, Belleville G, Belanger L, Ivers H.
The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response.
Sleep 2011;34(5):601-608.Thorndike FP, Ritterband LM, Saylor DK, Magee JC, Gonder-Frederick LA.
Validation of the insomnia severity index as a web-based measure.
Behav Sleep Med 2011;9(4):216-223.Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH.
The PHQ-8 as a measure of current depression in the general population.
J Affect Disord 2009;114(1-3):163-173.Lowe B, Unutzer J, Callahan CM, Perkins AJ, Kroenke K.
Monitoring depression treatment outcomes with the patient health questionnaire-9.
Med Care 2004;42(12):1194-1201.Lowe B, Kroenke K, Herzog W, Grafe K.
Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9).
J Affect Disord 2004;81(1):61-66.Kroenke K, Spitzer RL, Williams JB, Monahan PO, Lowe B.
Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection.
Ann Intern Med 2007;146(5):317-325.Brooks R.
EuroQol: the current state of play.
Health Policy 1996;37(1):53-72.Hornbrook MC, Goodman MJ.
Chronic disease, functional health status, and demographics: a multi-dimensional approach to risk adjustment.
Health Serv Res 1996;31(3):283-307.Lynch FL, Hornbrook M, Clarke GN, et al.
Cost-effectiveness of an intervention to prevent depression in at-risk teens.
Arch Gen Psychiatry 2005;62(11):1241-1248.Smith DH, O'Keeffe-Rosetti M, Owen-Smith AA, et al.
Improving adherence to cardiovascular therapies: an economic evaluation of a randomized pragmatic trial.
Value Health 2016;19(2):176-184.Rutherford C, Costa D, Mercieca-Bebber R, Rice H, Gabb L, King M.
Mode of administration does not cause bias in patient-reported outcome results: a meta-analysis.
Qual Life Res 2016;25(3):559-574.Charlson ME, Pompei P, Ales KL, MacKenzie CR.
A new method of classifying prognostic comorbidity in longitudinal studies: development and validation.
J Chronic Dis 1987;40(5):373-383.Mihaylova B, Briggs A, O'Hagan A, Thompson SG.
Review of statistical methods for analysing healthcare resources and costs.
Health Econ 2011;20(8):897-916.Martin, BI, Gerkovich, MM, Deyo, RA et al.
The Association of Complementary and Alternative Medicine Use and Health Care Expenditures
for Back and Neck Problems
Medical Care 2012 (Dec); 50 (12): 1029–1036Greene BR, Smith M, Allareddy V, Haas M.
Referral patterns and attitudes of primary care physicians towards chiropractors.
BMC Complement Altern Med 2006;6:5.Allareddy V, Greene BR, Smith M, Haas M, Liao J.
Facilitators and barriers to improving interprofessional referral relationships between primary care physicians and chiropractors.
J Ambul Care Manage 2007;30(4):347-354.Penney LS, Ritenbaugh C, Elder C, Schneider J, Deyo RA, DeBar LL.
Primary Care Physicians, Acupuncture and Chiropractic Clinicians, and Chronic
Pain Patients: A Qualitative Analysis of Communication and Care Coordination Patterns
BMC Complement Altern Med. 2016 (Jan 25); 16: 30
Return to COST-EFFECTIVENESS
Since 11-10-2016


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |