

Deconstructing Chronic Low Back Pain in the Older Adult -
Step by Step Evidence and Expert-Based Recommendations
for Evaluation and Treatment.
Part IV: DepressionThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Pain Medicine 2015 (Nov); 16 (11): 20982108 ~ FULL TEXT
OPEN ACCESS Joseph A. Carley, Jordan F. Karp, Angela Gentili, Zachary A. Marcum,
M. Carrington Reid, Eric Rodriguez, Michelle I. Rossi, Joseph Shega,
Stephen Thielke, Debra K. Weiner
Departments of Psychiatry,
University of Pittsburgh,
Pittsburgh, PA, USA.OBJECTIVE: To present the fourth in a series of articles designed to deconstruct chronic low back pain (CLBP) in older adults. The series presents CLBP as a syndrome, a final common pathway for the expression of multiple contributors rather than a disease localized exclusively to the lumbosacral spine. Each article addresses one of twelve important contributors to pain and disability in older adults with CLBP. This article focuses on depression.
METHODS: The evaluation and treatment algorithm, a table articulating the rationale for the individual algorithm components, and stepped-care drug recommendations were developed using a modified Delphi approach. The Principal Investigator, a three-member content expert panel, and a nine-member primary care panel were involved in the iterative development of these materials. The algorithm was developed keeping in mind medications and other resources available within Veterans Health Administration (VHA) facilities. As panelists were not exclusive to the VHA, the materials can be applied in both VHA and civilian settings. The illustrative clinical case was taken from one of the contributor's clinical practice.
RESULTS: We present an algorithm and supportive materials to help guide the care of older adults with depression, an important contributor to CLBP. The case illustrates an example of a complex clinical presentation in which depression was an important contributor to symptoms and disability in an older adult with CLBP.
CONCLUSIONS: Depression is common and should be evaluated routinely in the older adult with CLBP so that appropriately targeted treatments can be planned and implemented.
KEYWORDS: Aged; Assessment; Chronic Pain; Depression; Elderly; Low Back Pain; Primary Care
From the FULL TEXT Article:
Introduction
Major depressive disorder (MDD) has a reported 1-year prevalence of 612% in older adults in both Veterans Affairs and civilian settings. In addition to MDD, the prevalence of clinically significant subsyndromal depressive symptoms in late-life (generally defined as ≥65 years) is estimated to be even higher. This may be due to under-recognition in the context of complex comorbidities. [1, 2] Depression is often a recurrent illness, triggered, and exacerbated by both psychological stress and medical illnesses. High medical burden in older adults contributes to treatment response variability such as delayed response to antidepressant pharmacotherapy and increased likelihood of recurrence. [3]
Numerous studies suggest that depression worsens both the severity of and disability caused by chronic low back pain (CLBP). [48] A large survey of community dwelling older adults found that mild to severe depressive symptoms increased the odds of disabling low back pain over a period of 2 years by 3060%. [8] Similarly, baseline disabling low back pain ranging from a little of the time to all of the time increased the odds of depressive symptoms by 27.984.2%, respectively. [8] As depression is a treatable illness, a rational approach to reducing the burden of CLBP is to diagnose and treat comorbid depression. To date, there is little research published about how to assess and treat these conditions simultaneously.
There are several challenges related to identifying depressive symptoms. Depressed older adults frequently communicate emotional distress by focusing on somatic complaints and describing nonspecific symptoms. Rather than spontaneously reporting depressive symptoms, the older adult may describe feeling helpless due to unrelenting back pain, joint pain, or gastrointestinal distress. [9, 10] Instead of reporting the cardinal symptoms of depression (i.e., depressed mood or anhedonia), many older adults with CLBP and other chronic pain conditions who are in a depressive episode often report non-specific symptoms such as irritability, insomnia, decreased energy, difficulty concentrating, and memory problems. [10, 11]
Reasons for this overlap in clinical presentation may be due to shared neurobiology and psychology between depression and CLBP [12] as well as genetic influences. [13] Areas of the brain which modulate mood also process pain and include the dorsolateral prefrontal cortex, anterior cingulate cortex, periaqueductal gray, insular cortex, and hypothalamus. [1416] Psychological similarities between patients with depression and patients with CLBP include diminished self-efficacy and subsequent learned helplessness. [1721] Older adults who have become disabled by either depression or CLBP often have a sense that they are unable to manage these and other chronic conditions. Both conditions frequently wax and wane, are exacerbated by environmental stressors, and may be responsive to similar pharmacologic (e.g., antidepressants) and behavioral treatments (e.g., cognitive behavioral therapy [CBT], mindfulness techniques). [12, 22] This overlapping neurobiology and psychology support the need for a shared approach to treatment.
Disability and loss of function are among the most feared consequences of medical problems and pain in late-life. [23] Pain-related disability is worse in patients with depression, further supporting the importance of its diagnosis and treatment. [7, 8] Thus, to increase the likelihood that CLBP and associated disability will respond to treatment, it is vital to systematically screen for and treat clinically significant depressive symptoms in the older adult who presents with CLBP. We present a patient who has CLBP with depression being at least one contributor to his pain and difficulty functioning. This case demonstrates the clinical complexity of older patients with CLBP, depression, and a multidisciplinary approach to his clinical care.
Methods
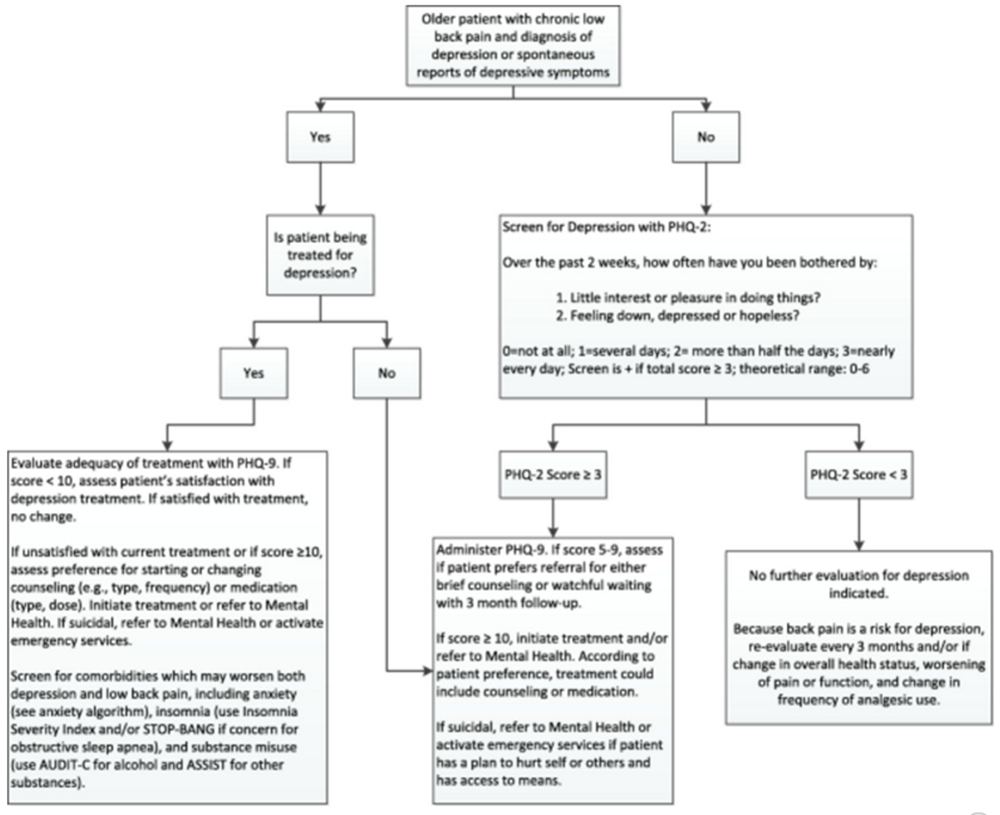
Figure 1 A modified Delphi technique was used to create an algorithm for assessing and treating CLBP and depression (Figure 1), as well as a table providing the rationale for the various components of the algorithm (Table 1), and the stepped-care medication table (Table 2). This iterative approach to the development of the algorithm is described in detail in the first article of this series. [45] Expertise represented among the Delphi expert panel for the depression algorithm included geriatric psychiatry, geriatric medicine, and geriatric psychopharmacology.
Table 1.
Depression and back pain: Theoretical and pragmatic underpinnings of algorithm recommendations
Algorithm component Comments Depression screening with PHQ-2 and PHQ-9 The Patient Health Questionnaire (PHQ) is a self-administered version of the PRIME-MD diagnostic instrument for common mental disorders. A PHQ-2 score > or =3 had a sensitivity of 83% and a specificity of 92% for major depression. Likelihood ratio and receiver operator characteristic analysis identified a PHQ-2 score of 3 as the optimal cutpoint for screening purposes.
The PHQ-9 is the depression module, which scores each of the 9 DSM-5 criteria as 0 (not at all) to 3 (nearly every day). PHQ-9 score ≥10 had a sensitivity of 88% and a specificity of 88% for major depression. PHQ-9 scores of 5, 10, 15, and 20 represented mild, moderate, moderately severe, and severe depression, respectively.Screening for psychiatric comorbidities and insomnia Late-life depression rarely occurs in isolation. Thus, screening for and assessment of late-life depression should always involve screening for other psychiatric disorders, including anxiety, alcohol, and drug abuse. As comorbid psychiatric disorders affect clinical course and prognosis, and may worsen long-term disability and pain management, treatment is critical to optimize both psychiatric and pain outcomes.
Untreated insomnia is associated with worse depression and low back pain treatment outcomes. We recommend screening for insomnia with the Insomnia Severity Index (available on myhealthevet.gov) and treating insomnia along with depression and low back pain to optimize outcomes.
If the patient is at high risk for obstructive sleep apnea (obese, male, African American, prescribed opioids, smoker, cardiovascular disease), consider administering the STOP-BANG questionnaire to assess whether referral for diagnostic polysomnography is indicatedCognitive Behavioral Therapy (CBT) Dissemination and implementation of cognitive behavioral therapy for depression in the VA system resulted in mean improvement in depression scores by about 40% from initial to later treatment phase. The effect size for improvement in quality of life ranged from d = 0.39 to d = 0.74. However, while a meta-analysis of trials using cognitive behavioral therapy [CBT] for late-life depression found it to be more effective than waiting list or treatment as usual, greater efficacy than active controls was not observed.
Despite the findings of this meta-analysis, CBT for pain has been shown to ameliorate pain-related symptoms for chronic back pain patients treated in an outpatient setting. CBT for pain provided in a group setting is associated with up to 5-year improved health and economic benefits compared with an information comparison group. Although CBT for depression in older adults may not be superior to other active controls, given the efficacy of CBT for pain and the superiority of CBT to treatment as usual, we recommend this as the psychosocial intervention of choice for older adults with low back pain and depression.Stepped care antidepressant treatment According to expert consensus guidelines for unipolar nonpsychotic major depression, the preferred strategy is an antidepressant (selective serotonin reuptake inhibitors or Venlafaxine XR are the preferred agents) plus psychotherapy. As these guidelines were prepared before the release of Duloxetine, and given that duloxetine is approved for the treatment of chronic pain in addition to depression, we include duloxetine as recommended for these patients. These guidelines also suggest that if the patient has a comorbid medical condition (e.g., chronic low back pain) that is contributing to the depression, both the depression and medical condition should be treated from the outset. The majority of experts would continue treatment with antidepressant medication for at least 1 year if a patient has had a single episode of severe unipolar major depression, for 13 years for a patient who has had two such episodes, and for longer than 3 years if there is a history of three or more episodes.
Beer's Criteria suggests monitoring for hyponatremia when starting an antidepressant in older adults. Second line antidepressant pharmacotherapy may include Bupropion SR, Mirtazapine, and Nortriptyline (with appropriate cardiac monitoring).
While not specific for older adults, the Sequenced Treatment Alternatives to Relieve Depression Study (STAR*D) showed that about half of participants are symptom-free after two treatment levels. Over the course of all four treatment levels, almost 70% of those who did not withdraw from the study became symptom-free.
The table included in the algorithm reflects best practice for the first three steps of depression pharmacotherapy that may be offered in primary care.Serial monitoring of progress Monitor improvement in depression with the PHQ-9. As antidepressant pharmacotherapy may reduce both pain severity and pain interference, routinely assess these clinical outcomes with a numeric rating scale for both pain severity and pain interference. The use of the 24-item Roland Morris Back Pain Disability Questionnaire may also be used to assess improvement in functioning.
Serial monitoring of adherence to both pharmacological and psychosocial treatment plans and management of barriers to compliance should be addressed.
Table 2.
Recommended early sequence of antidepressant pharmacotherapy
This stepped care approach for the pharmacotherapy of depression and low back pain in older adults is blended from both the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) and Prevention of Suicide in Primary care Elderly-Collaborative Trial (PROSPECT). Duloxetine has been added to this updated algorithm given its dual approval from the FDA for both major depression and chronic pain. This algorithm is truncated at level 3 because beyond this level, primary care physicians should consider referring the patient for evaluation by mental health.
Level
(all levels
are 6 weeks)Medication Target/Maintenance Dose Notes Level 1 SSRI:
Citalopram
Sertraline20 mg (for patients >60 y.o.) 100200 mg May consider first line treatment with sertraline if there are concerns about prolonged QTc. Level 2
Non-response to Level 1Taper and stop SSRI
Start Duloxetine
Or
Start Venlafaxine60 mg
Target dose 150300 mgDuloxetine is U.S. Food and Drug Administration (FDA)-approved for both major depression and chronic pain.
Duloxetine is not recommended for patients with end-stage renal disease or severe renal impairment (estimated creatinine clearance <30 mL/minutes)Level 2
Partial response to Level 1Continue SSRI
Augment with Bupropion SR200 mg bid Confirm patient has no history of seizure disorder and is not at increased risk of seizure (i.e., taking Tramadol) Level 2A
Partial response to Level 1Continue SSRI
Consider low dose Nortriptyline to help with pain and sleep (if no contraindication, per below).1025 mg po qhs While low dose nortriptyline may reduce pain and help with sleep, (and, therefore, benefit mood), these low doses are unlikely to have specific antidepressant effects. Level 3
Non-response to Level 2Taper and stop all Level 2 medications
Start NortriptylinePlasma concentration 80120 ng/mL
Steady state achieved in approximately 56 days.
If possible, plasma levels should be trough, drawn immediately before next dose.Nortriptyline may have analgesic effects.
Obtain Electrocardiogram (EKG) prior to use.
Limit supply of medication if patient at high suicide risk.
Monitor for anticholinergic side effects.Level 3
Partial response to Level 2Continue SSRI
Taper and stop bupropion SR
Augment with either:
Nortriptyline or LithiumPlasma concentration 80120 ng/mL
Plasma concentration 0.60.8 mEq/LCaution use of lithium in older adults with renal insufficiency (or using concomitant Nonsteroidal Anti-inflammatory Drugs (NSAIDs), Angiotensin Converting Enzyme (ACE) inhibitors, thiazide diuretics, or loop diuretics).
Obtain Thyroid Stimulating-hormone (TSH) level before using lithium.
Note lower plasma levels than used in younger adults and/or with bipolar disorder. Refer for psychiatric co-management if desired.
Nonresponse may be defined as <30% improvement in a depression rating scale after 6 weeks of treatment with a score still in the symptomatic range. Partial response may be defined as >50% response on a depression rating scale, with a score still in the symptomatic range.
At all levels of this sequenced care, referral for cognitive behavioral therapy should be offered. This is, especially important given the significant proportion of older adults who will refuse or stop antidepressant pharmacotherapy. Given the added stress of chronic low back pain on depression, patients may benefit from learning more adaptive approaches to coping with these challenges, improving problem solving skills, planning pleasurable activities, increasing activity, and improving restorative sleep.
The FDA has recommended that citalopram should no longer be used at doses greater than 40 mg/day because it could cause potentially dangerous abnormalities in the electrical activity of the heart, in particular prolonged QTc. The maximum recommended dose for patients older than 60 is 20 mg/day. [3841]
Case Presentation
Relevant Pain and Functioning History
The patient is an 88year-old widowed Caucasian man residing in an assisted living facility (ALF) who presented to his primary care physician complaining of a flare of his CLBP. He described having low back pain as long as I can remember. The pain is worse with walking but does not radiate into either leg. He states the pain can hit me at any time, including while sitting and at times while supine. He describes the pain as aching and heavy and at a 6/10 severity on average. However, over the past 2 weeks, he describes the pain as 10/10 severity more than 50% of the time.
He has had two spine surgeries. These included lumbar decompression (20 years ago) and laminectomy and fusion (8 years ago). Each of these surgeries improved his back pain for about 2 months, but the pain then returned at the same level of severity. In addition to these surgeries, he has had three epidural steroid injections, physical therapy, chiropractic manipulation, massage therapy, heat therapy, opioid, and nonopioid oral analgesics, topical analgesics, and been episodically compliant with a home-based stretching and core-strengthening program. He is currently prescribed oxycodone extended release 10 mg bid and oxycodone immediate release 5 mg every 4 hours as needed for pain. He has been taking additional oxycodone immediate release over the past 2 weeks. He has a TENS unit at home, and although it helps, he has trouble motivating himself to use it. He is unable to walk or stand for more than 15 minutes because of the pain. He has also curtailed attending church and reduced the number of community dinners he attends each week at the ALF. Although he has not fallen, he is fearful that he will.
Relevant Physical and Psychiatric Examination, and Review of Systems
He is alert and oriented Χ 5 with good fund of knowledge and no language deficits. His gait is notable for short step length and relatively slow gait velocity. He carries a standard straight cane in his left hand for balance. On physical exam there was no evidence of leg length discrepancy, scoliosis, sacroiliac joint pain, vertebral body pain, or pain and restricted motion of the hip with internal rotation. On palpation, there was mild myofascial pain of the paralumbar musculature. The Mini Mental State Examination score was 27 (theoretical range 030). [46] As his wife died and his move to the ALF, he describes feeling lonely and does not see much reason for living as most of his friends and all of his siblings have died. He scores 20 on the Patient Health Questionnaire (PHQ)9 (theoretical range 027), endorsing daily depressed mood, insomnia (with sleep continuity disturbance and early morning awakening), self-critical thinking, low appetite, trouble concentrating, and a passive death wish. [25] He denies active suicidal ideation or plan. He does not own any firearms and is not stockpiling opioids. Upon further questioning, he states he spends most of his day sitting in a chair watching television or staring out the window as he feels sapped of energy. Associated symptoms he describes include chronic nausea and constipation, feeling cold, blurry vision, pain in other joints, urinary frequency, and dry mouth. He denies any weight change, fever, chills, or night sweats.
Clinical Course
The patient revealed that in addition to analgesia, he also used the oxycodone extended release for its calming and numbing effect, and was counseled that there were better and safer treatments available. The evening dose of oxycodone extended release was discontinued, and the oxycodone immediate release was reduced to 5 mg every 6 hours. To treat both the depression and back pain, pharmacotherapy with duloxetine was initiated at 30 mg for 1 week and increased to 60 mg starting week 2. The clinic social worker began to see the patient every other week to deliver supportive psychotherapy informed by Cognitive Behavioral Therapy (CBT) and Problem Solving Therapy techniques. [47] Their work together also focused on sleep consolidation techniques and increasing his participation in pleasurable activities. [48] With his permission, the social worker engaged both his daughter and the social coordinator from the ALF into treatment planning.
Approach to Management
Upon further history taking, it became clear that depression and bereavement were playing roles in this flare of CLBP. As he spontaneously reported some depressive symptoms after the passing of his wife, he was appropriately screened with the PHQ-9. If this patient had not spontaneously mentioned loneliness and some hopelessness, he could have been screened with the PHQ-2 which is shorter yet still has robust psychometric properties. [49]
The algorithm presented in the Figure 1 provides guidance for the clinician as to when to use the PHQ-2 vs the PHQ-9. The PHQ-2 is best utilized when the older patient with CLBP has no prior diagnosis of depression and no spontaneous report of depressive symptoms. The PHQ-2 score of greater than or equal to 3 has a sensitivity of 83% and a specificity of 92% for major depression [24] (Table 1). Patients who screen positive with the PHQ-2 should be administered the PHQ-9. If clinical resources are available and the PCP feels a referral is indicated (i.e., because of high depression severity, history of treatment nonresponse, or complex psychiatric and psychosocial comorbidity) a referral to Psychiatry may be warranted. Because patients with CLBP are at increased risk of new onset depression, those who screen negative on the PHQ-2 should be reevaluated at 3-month intervals or sooner in the setting of worsening health status, pain, or increased analgesic use.
For older patients with CLBP who already carry a diagnosis of depression or are spontaneously reporting depressive symptoms, we recommend using the PHQ-9. The PHQ-9 scores each of the nine DSM-5 criteria for depression from 0 being not at all to 3 being nearly every day. A score of 10 or higher has a sensitivity of 88% and a specificity of 88% for major depression. [25] PHQ-9 scores also provide a range of depression severity with mild, moderate, moderately severe, and severe, corresponding to scores of 5, 10, 15, and 20, respectively. [25] Based both on whether the patient is already receiving treatment for depression and the current PHQ-9 score, the algorithm provides directions for further evaluation and treatment including screening for psychiatric and sleep comorbidities, counseling, and medication management.
Once clinically significant depression is diagnosed, screening for comorbid psychiatric conditions should be undertaken, as comorbidity is the norm, not the exception. [26] Common comorbid conditions in older depressed patients include anxiety, cognitive impairment, and alcohol misuse [27] , and in VA settings, PTSD is frequently comorbid. While data are limited, there is evidence of improved outcomes for depression with comorbid anxiety or alcohol use disorders when treated using CBT or substance use counseling, respectively. [26] Another common comorbid condition, which worsens both depression and CLBP, is insomnia. [28] A detailed algorithm guiding evaluation and treatment of insomnia will be published later in this series on CLBP in the older adult. The Insomnia Severity Index is a brief screen for insomnia and can be easily incorporated into routine assessments. [50] Sleep apnea is especially prevalent in patients who are obese, living with cardiovascular disease, and is worsened by the use of opioids and benzodiazepines. If sleep apnea is suspected, the STOP-BANG questionnaire can be used to assess the need for referral to sleep medicine and possibly diagnostic polysomnography. [30] Important other risks for poor response to treatment for both depression and CLBP include prolonged and/or use of high-dose opioids [51] and history of multiple spine surgeries. [52] Tailoring treatment based on an individual's psychiatric and medical comorbidities provides the best chance of improving both depression and CLBP.
Cognitive Behavioral Therapy (CBT) has demonstrated clinical benefit for both depression and CLBP. [3134] The efficacy of CBT for depressed older adults is well established [53] with average effect sizes above 0.80. [54] CBT is an established intervention for CLBP [55], and there is evidence for its use in older adults with pain syndromes. In general, studies of CBT in older adults with chronic pain support its efficacy for significantly reducing pain (with small to medium effect sizes) [56], with meaningful improvements in indices of adapting to and coping with pain, such as measures of depression, anxiety, pain catastrophizing, self-efficacy, and level of activity. [57] CBT for CLBP and MDD utilizes similar techniques such as learning to pace activities, involvement of spouses/caregivers, reinforcement of adaptive responses, reframing affective and cognitive responses, learning active coping skills and relaxation techniques, and problem solving skills training. [56, 58] Using a personalized approach, CBT may be individualized for these complex patients. To our knowledge, there have not been randomized controlled trials of CBT for patients with both MDD and CLBP. In the context of coexisting CLBP and depression, CBT is our consensus recommendation. CBT targets the diminished self-efficacy and learned helplessness, which often occur in both depression and CLBP, particularly in older adults. CBT can be delivered by psychologists, social workers, and psychiatrically trained nurses. Computerized CBT programs are becoming increasingly available, may be equivalent to therapist-delivered CBT [59], and should be considered for patients who are computer savvy and/or have limited access to mental health care. There is also evidence supporting goal attainment as a measurable focus of treatment for older adults living with chronic conditions. [60] This practical approach enhances patient-centered care and may align well with the processes of CBT. In addition to CBT and pharmacotherapy, increased physical activity may improve outcomes for both CLBP and depression [61, 62] Increasing physical activity is consistent with the behavioral activation focus of CBT and may be a patient-centered goal of treatment.
In addition to Cognitive Behavioral Therapy (CBT), our expert consensus guidelines for depression recommend pharmacotherapy with selective serotonin reuptake inhibitors (SSRI's) or serotonin norepinephrine reuptake inhibitors (SNRI's) [35, 36, 39] (Table 2). In addition to venlafaxine, duloxetine has been shown to be effective as both an SNRI antidepressant and for chronic musculoskeletal pain. [40, 41] When prescribing serotonergic and noradrenergic reuptake inhibitor treatment in older adults, monitoring for hyponatremia is recommended. [37] An accepted approach for duration of treatment is continuation of antidepressant pharmacotherapy for at least a year if this is the first episode of depression and at least 3 years if the patient has a history of recurrent episodes. [63] Patient and caregiver education is important when antidepressants are administered for depression and/or analgesia. Instructing patients on both the importance of taking the medication every day as prescribed and that the medication is being prescribed for both conditions may improve adherence and reduce stigma.
Approximately 50% of older adults do not respond to first line pharmacotherapy and require subsequent treatment trials. While not specific to older adults, the Sequenced Treatment Alternatives to Relieve Depression Study (STAR*D) showed that about half of participants are symptom-free after two treatment levels. [36] Second line treatments include bupropion, mirtazapine, or nortriptyline (see Table 2). While amitriptyline has been studied for use in certain pain conditions and in depression, its severe anticholinergic side effect profile has led to its inclusion on the Beers list [37], and so is not recommended in older adults. Nortriptyline has a somewhat less severe side effect profile but this should be monitored.
Using a measurement-based approach, pharmacotherapy focused on both depression and CLBP may result in superior outcomes than focusing on only one condition. [12] Indeed, serial monitoring of progress has been shown to improve outcomes for both depression treatment and chronic pain management by allowing appropriate adjustments to treatment plans. [42, 43] In addition to the PHQ-9 for serial measurement of depression, the 24-item Roland Morris Back Pain Disability Questionnaire is recommended for use to monitor change in functioning related to low back pain. [44] Alternatively, periodic monitoring of pain severity using a numeric rating scale may also inform measurement-guided treatment.
Resolution of Case
After titrating the duloxetine up to 60 mg, the patient began to gradually show improvement first in low back pain and then depression severity. [64] Screening for psychiatric comorbidities including alcohol use was negative, as was screening for sleep apnea with the STOP-BANG questionnaire. He engaged in eight sessions of supportive therapy informed by CBT (with a focus on increasing pleasurable activities, strategies to increase physical activity while pacing himself to avoid precipitating a pain flare, and reducing insomnia). Additional benefit was gained through treatment planning with his daughter and the social coordinator from the ALF. They successfully supported him in becoming gradually more engaged in community activities. It is worth noting that social workers can be trained to deliver CBT in primary care settings. This is significant, as a major barrier to the delivery of evidence based depression and pain interventions is limited access to psychologists. Serial monitoring of progress and gradual reductions in use of opioids over time further contributed to his overall improvement.
Summary
Because of the increased prevalence of mood symptoms in patients living with chronic pain, screening for depression should be routine in older adults with CLBP. As depression worsens both pain severity and pain-associated disability, treating this modifiable contributor to CLBP can improve analgesia and functioning as well as other health and disability related outcomes. [65] Step-wise screening with the PHQ-2 and PHQ-9 is a highly sensitive and specific approach for detecting clinically actionable depression. If depression is detected, screening for and treating common comorbidities such as anxiety, substance misuse, insomnia, and sleep disordered breathing is indicated and may result in a more durable treatment response.
Depression and CLBP in older adults are mutually exacerbating conditions that both contribute to patient and family suffering, increased disability, cognitive impairment [66], polypharmacy, and hastened mortality. [67] Because of an overlapping neurobiology and psychology, treating these disorders as linked conditions may spare use of opioids and encourage a parsimonious approach to prescribing. Using a shared decision to account for patient preference and an interdisciplinary approach, initiating treatment with a SSRI or SNRI is first line treatment and may improve outcomes for both conditions. CBT is the behavioral intervention with the greatest evidence base for both depression and CLBP. Social workers and chronic disease care managers are increasingly colocated in primary care practices and may be trained in the reliable delivery of CBT. These clinicians also play a key role in monitoring symptom change and medication adherence, information which can then be communicated to the prescribing PCP. Educating patients that these interventions target both mood and pain symptoms may enhance compliance, resulting in better outcomes for both conditions.
Key Points
Older adults with CLBP should be screened for depression, and treated if depression is present.
Effective treatment of depression in older adults with CLBP will reduce pain-related activities interference and overall disability.
Older adults with depression also should be screened for important psychiatric comorbidities that also may worsen CLBP including alcohol use, anxiety disorders, cognitive impairment, insomnia, and sleep disordered breathing.
Depression comorbid with CLBP should be treated for at least 1 year to avoid recurrence. Behavioral interventions and pharmacotherapy such as SSRIs and SNRIs, chosen based on symptom severity and shared decision making, may improve long-term outcomes.
Acknowledgments
This material is based on work supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Rehabilitation Research and Development Service. Dr. Karp would like to acknowledge grant AG033575 (the ADAPT Project: Addressing Depression and Pain Together), which provided support for his work on this article. The contents of this report do not represent the views of the Department of Veterans Affairs or the US government. The authors thank Dave Newman for his thoughtful review of the manuscript.
Conflict of interest:
Dr. Karp has received medication supplies for investigator initiated studies from Pfizer and Invidior. The other authors have no potential conflicts to report.
References:
Mulsant B, Ganguli M. Epidemiology and diagnosis of depression in late life. J Clin Psychiatry 1999;60(Suppl 20):915
Burnett-Zeigler I, Zivin K, Ilgen M, et al. Depression treatment in older adult veterans. Am J Geriatr Psychiatry 2012;20(3):22838
Lenze EJ, Sheffrin M, Driscoll HC, et al. Incomplete response in late-life depression: Getting to remission. Dialogues Clin Neurosci 2008;10(4):41930
Cecchi F, Debolini P, Lova RM, et al. Epidemiology of back pain in a representative cohort of Italian persons 65 years of age and older: The InCHIANTI study. Spine 2006;31(10):114955
Linton SJ. A review of psychological risk factors in back and neck pain. Spine 2000;25(9):114856
Pincus T, Burton AK, Vogel S, Field AP. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine 2002;27(5):10920
Reid MC, Williams CS, Concato J, Tinetti ME, Gill TM. Depressive symptoms as a risk factor for disabling back pain in community-dwelling older persons. J Am Geriatr Soc 2003;51(12):17107
Meyer T, Cooper J, Raspe H. Disabling low back pain and depressive symptoms in the community-dwelling elderly: A prospective study. Spine 2007;32(21):23806
Wang SJ, Liu HC, Fuh JL, Wang PN, Lu SR. Comorbidity of headaches and depression in the elderly. Pain 1999;82(3):23943
Hein S, Bonsignore M, Barkow K, Giltay EJ. Lifetime depressive and somatic symptoms as preclinical markers of late-onset depression. [erratum appears in Eur Arch Psychiatry Clin Neurosci 2003;253(2):110]. Eur Arch Psychiatry Clin Neurosci 2003;253(1):1621
Hegeman JM, Kok RM, van der Mast RC, et al. Phenomenology of depression in older compared with younger adults: Meta-analysis. Br J Psychiatry 2012;200(4):27581
Karp J, Reynolds C. Depression, pain, and aging. Focus 2009;7:1727
Pinheiro MB, Ferreira ML, Refshauge K, et al. Genetics and the environment affect the relationship between depression and low back pain: A co-twin control study of Spanish twins. Pain 2015;156(3):496503
Hadjipavlou G, Dunckley P, Behrens TE, Tracey I. Determining anatomical connectivities between cortical and brainstem pain processing regions in humans: A diffusion tensor imaging study in healthy controls. Pain 2006;123(12):16978
Aziz Q, Thompson DG, Ng VW, et al. Cortical processing of human somatic and visceral sensation. J Neurosci 2000;20(7):265763
Tracey I, Mantyh PW. The cerebral signature for pain perception and its modulation. Neuron 2007;55(3):37791
Blazer DG. Depression in late life: Review and commentary. J Gerontol Biol Med Sci 2003;58(3):24965
Barry LC, Guo Z, Kerns RD, et al. Functional self-efficacy and pain-related disability among older veterans with chronic pain in a primary care setting. Pain 2003;104(12):1317
Rudy T, Weiner D, Lieber S, Slaboada J, Boston J. The impact of chronic low back pain on older adults: A comparative study of patients and controls. Pain 2007;131:293301
Rowe JW, Kahn RL. Successful aging. Aging Clin Exp Res 1998;10(2):1424
Seligman ME. Learned helplessness. Annu Rev Med 1972;23:40712
Sullivan MJ, Reesor K, Mikail S, Fisher R. The treatment of depression in chronic low back pain: Review and recommendations. Pain 1992;50(1):513
Herr KA, Garand L. Assessment and measurement of pain in older adults. Clin Geriatr Med 2001;17(3):45778
Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Med Care 2003;41(11):128492
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med 2001;16(9):60613
Gum AM, Cheavens JS. Psychiatric comorbidity and depression in older adults. Curr Psychiatry Rep 2008;10(1):239
Devanand DP. Comorbid psychiatric disorders in late life depression. Biol Psychiatry 2002;52(3):23642
Buysse DJ. Insomnia, depression and aging. Assessing sleep and mood interactions in older adults. Geriatrics 2004;59(2):4751
Karp JF, Yu L, Friedly J, et al. Negative affect and sleep disturbance may be associated with response to epidural steroid injections for spine-related pain. Arch Phys Med Rehabil 2014;95(2):30915
Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire: A tool to screen patients for obstructive sleep apnea. Anesthesiology 2008;108(5):81221
Karlin BE, Brown GK, Trockel M, et al. National dissemination of cognitive behavioral therapy for depression in the Department of Veterans Affairs health care system: Therapist and patient-level outcomes. J Consult Clin Psychol 2012;80(5):70718
Gould RL, Coulson MC, Howard RJ. Cognitive behavioral therapy for depression in older people: A meta-analysis and meta-regression of randomized controlled trials. J Am Geriatr Soc 2012;60(10):181730
Linton SJ, Nordin E. A 5-year follow-up evaluation of the health and economic consequences of an early cognitive behavioral intervention for back pain: A randomized, controlled trial. Spine 2006;31(8):8538
Glombiewski JA, Hartwich-Tersek J, Rief W. Two psychological interventions are effective in severely disabled, chronic back pain patients: A randomised controlled trial. Int J Behav Med 2010;17(2):97107
Alexopoulos G, Katz IR, Reynolds CF III., et al. The expert consensus guideline series: Pharmacotherapy of depressive disorders in older patients. Postgrad Med 2001;186
Rush AJ, Trivedi MH, Wisniewski SR, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: A STAR*D report. Am J Psychiatry 2006;163(11):190517
American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc 2012;60(4):61631
Gaynes BN, Rush AJ, Trivedi MH, et al. The STAR*D study: Treating depression in the real world. Cleve Clin J Med 2008;75(1):5766
Mulsant BH, Alexopoulos GS, Reynolds CF 3rd., et al. Pharmacological treatment of depression in older primary care patients: The PROSPECT algorithm. Int J Geriatr Psychiatry 2001;16(6):58592
Raskin J, Wiltse CG, Siegal A, et al. Efficacy of duloxetine on cognition, depression, and pain in elderly patients with major depressive disorder: An 8-week, double-blind, placebo-controlled trial. Am J Psychiatry 2007;164(6):9009
Smith HS, Smith EJ, Smith BR. Duloxetine in the management of chronic musculoskeletal pain. Ther Clin Risk Manag 2012;8:26777
Yeung AS, Jing Y, Brenneman SK, et al. Clinical Outcomes in Measurement-based Treatment (Comet): A trial of depression monitoring and feedback to primary care physicians. Depress Anxiety 2012;29(10):86573
Hadjistavropoulos T, Herr K, Turk DC, et al. An interdisciplinary expert consensus statement on assessment of pain in older persons. Clin J Pain 2007;23(1 Suppl):S143
Roland M, Morris R. A study of the natural history of back pain. Part I: Development of a reliable and sensitive measure of disability in low-back pain. Spine 1983;8(2):1414
Weiner DK.
Deconstructing Chronic Low Back Pain in the Older Adult -
Shifting the Paradigm from the Spine to the Person
Pain Med 2015; 16 (5): 881885Folstein MF, Folstein SE, McHugh PR. Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12(3):18998
Arean P, Hegel M, Vannoy S, Fan MY, Unuzter J. Effectiveness of problem-solving therapy for older, primary care patients with depression: Results from the IMPACT project. Gerontologist 2008;48(3):31123
Troxel WM, Germain A, Buysse DJ. Clinical management of insomnia with brief behavioral treatment (BBTI). Behav Sleep Med 2012;10(4):26679
Arroll B, Goodyear-Smith F, Crengle S, et al. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann Fam Med 2010;8(4):34853
Morin CM, Belleville G, Bιlanger L, Ivers H. The insomnia severity index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep 2011;34(5):6018
Kobus AM, Smith DH, Morasco BJ, et al. Correlates of higher-dose opioid medication use for low back pain in primary care. J Pain 2012;13(11):11318
Long DM. Failed back surgery syndrome. Neurosurg Clin N Am 1991;2(4):899919
Kiosses DN, Leon AC, Arean PA. Psychosocial interventions for late-life major depression: Evidence-based treatments, predictors of treatment outcomes, and moderators of treatment effects. Psychiatr Clin North Am 2011;34(2):377401
Pinquart M, Duberstein PR, Lyness JM. Effects of psychotherapy and other behavioral interventions on clinically depressed older adults: A meta-analysis. Aging Ment Health 2007;11(6):64557
Turner JA, Jensen MP. Efficacy of cognitive therapy for chronic low back pain. Pain 1993;52(2):16977
Williams AC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev 2012;11:Cd007407
Keefe FJ, Porter L, Somers T, Shelby R, Wren AV. Psychosocial interventions for managing pain in older adults: Outcomes and clinical implications. Br J Anaesth 2013;111(1):8994
Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: A review of meta-analyses. Clin Psychol Rev 2006;26(1):1731
Proudfoot J, Clarke J, Birch MR, et al. Impact of a mobile phone and web program on symptom and functional outcomes for people with mild-to-moderate depression, anxiety and stress: A randomised controlled trial. BMC Psychiatry 2013;13:312
Toto PE, Skidmore ER, Terhorst L, Rosen J, Weiner DK. Goal Attainment Scaling (GAS) in geriatric primary care: A feasibility study. Arch Gerontol Geriatr 2015;60(1):1621
van Tulder MW, Malmivaara A, Esmail R, Koes BW. Exercise therapy for low back pain. Cochrane Database Syst Rev 2000;(2):CD000335
Cooney GM, Dwan K, Greig CA, et al. Exercise for depression. Cochrane Database Syst Rev 2013;9:CD004366
Reynolds CF 3rd., Frank E, Perel JM, et al. Nortriptyline and interpersonal psychotherapy as maintenance therapies for recurrent major depression: A randomized controlled trial in patients older than 59 years. JAMA 1999;281(1):3945
Karp JF, Weiner DK, Dew MA, et al. Duloxetine and care management treatment of older adults with comorbid major depressive disorder and chronic low back pain: Results of an open-label pilot study. Int J Geriatr Psychiatry 2010;25(6):63342
Ormel J, VonKorff M, Ustun TB, et al. Common mental disorders and disability across cultures. Results from the WHO collaborative study on psychological problems in general health care. JAMA 1994;272(22):17418
Karp JF, Reynolds CF 3rd., Butters MA, et al. The relationship between pain and mental flexibility in older adult pain clinic patients. Pain Med 2006;7(5):44452
Andersson HI. Increased mortality among individuals with chronic widespread pain relates to lifestyle factors: A prospective population-based study. Disabil Rehabil 2009;31(24):19807

Return to LOW BACK PAIN
Since 1-22-2016


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |