Sources of Cervicogenic Headache Among
the Upper Cervical Synovial Joints Subjects with Single HeadachesThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Pain Medicine 2022 (May 30); 23 (6): 10591065 ~ FULL TEXT
OPEN ACCESS Jayantilal Govind MB, ChB, MMed and Nikolai Bogduk MD, PhD, Dsc
Faculty of Health,
University of Newcastle,
New South Wales, Australia.
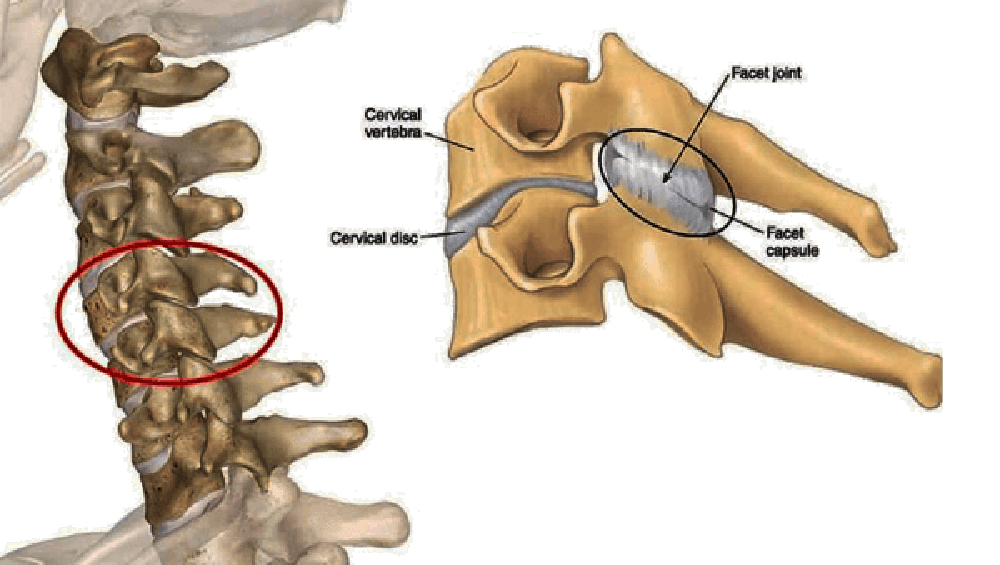
FROM: Cervical Facet Joint SyndromeObjectives: The study sought to assess the utility of controlled diagnostic blocks in patients with probable cervicogenic headache by determining the prevalence of sources of pain among the upper and lower synovial joints of the cervical spine.
Methods: Controlled diagnostic blocks were performed in 166 consecutive patients who clinically exhibited features consistent with a diagnosis of probable cervicogenic headache. Data were collected on how often a particular source of pain could be pinpointed and how often particular diagnostic blocks provided a positive yield.
Results: In patients in whom headache was the dominant complaint, diagnostic blocks succeeded in establishing the source of pain in 75% of patients. The C23 joint was the source of pain in 62%, followed by the C12 (7%) and C34 (6%). In patients in whom headache was less severe than neck pain, blocks were successful in 67%. C23 was the source of pain in 42%, followed by lower cervical joints in 18% and the C34 joint in 7%.
Conclusions: Controlled diagnostic blocks can establish the source of pain in the majority of patients presenting with probable cervicogenic headache, with C23 being the most common source. On the basis of pretest probability, diagnostic algorithms should commence investigations at C23. Second and third steps in the algorithm should differ according to whether headache is the dominant or nondominant complaint.
From the FULL TEXT Article:
Introduction
By definition, cervicogenic headache is pain referred to the head from a source in the cervical spine. [15] Various clinical criteria have been promoted for the diagnosis of cervicogenic headache, but none have been fully validated. On clinical grounds alone, a diagnosis might, at best, be rendered of possible cervicogenic headache or probable cervicogenic headache. [26] A definitive diagnosis requires establishing that the source of pain lies in the neck. At present, the only means for doing so is to relieve the headache by anaesthetizing putative cervical sources by using controlled diagnostic blocks. [15]
In the second edition of its Classification of Headache, the International Headache Society made positive responses to controlled diagnostic blocks an essential criterion for the diagnosis of cervicogenic headache. [1] However, it did not indicate what structures are the most likely sources of pain and which should be targeted for diagnostic blocks.
Some investigators have used diagnostic blocks of the greater occipital nerve and other structures in the cervical spine [7], but they did not use controlled blocks, and few of their patients obtained complete relief of their pain. Controls are essential for diagnostic blocks in order to rule out false-positive responses. [8, 9] Relief of pain must be complete because partial responses to blocks leave the remaining pain unaccounted for and do not exclude some form of placebo response.
Only one study has reported using controlled diagnostic blocks. [10] It found that, in 40 patients with headache after whiplash, the source of pain could be traced to the C23 zygapophysial joint in 21 (53%). However, to date, no study has tested or corroborated this figure. In the absence of further evidence, the prevalence of different sources of cervicogenic headache among the cervical synovial joints remains contentious.
The present study was, therefore, undertaken with three objectives. The first was to determine how often a source of pain could be determined in patients with probable cervicogenic headache. The second was to establish what those sources might be. The third was to assess the utility and efficiency of controlled diagnostic blocks as a diagnostic tool.
Methods
The study was conducted in a tertiary referral center specializing in the diagnosis and treatment of spinal pain, with a particular interest in neck pain and headache. The center saw patients on referral from specialists and general practitioners. The source population was 284 consecutive patients with chronic neck pain, seen between June 2000 and May 2004.
The study sample consisted of 166 consecutive patients who, in addition to their neck pain, reported headache. Clinically, these patients all satisfied the operational criteria for a diagnosis of probable cervicogenic headache. [46] They had pain starting in the neck and at least three of the following features: headache that was constant but non-throbbing, with concomitant pain in the neck or shoulder, triggered by neck movement, with reduced range of motion of the neck, and onset of headache shortly after neck trauma. These patients were further subdivided into 98 whose headache was only an incidental or minor complaint relative to their neck pain and 68 whose headache was their dominant complaint.
The possible sources of pain tested were the lateral atlanto-axial joint (C12), the C23 zygapophysial joint, the C34 zygapophysial joint, and zygapophysial joints at lower segmental levels. Fluoroscopically guided diagnostic blocks were performed according to the standards prescribed by the International Spine Intervention Society. Lateral atlanto-axial joints were tested with intra-articular blocks. [11] The C23 joint was tested with third occipital nerve blocks. [12] The C34 and other zygapophysial joints were tested with cervical medial branch blocks. [13]
For blocks of the lateral atlanto-axial joint, a posterior approach was used. [11] Once the needle appeared to enter the joint, a test dose of about 0.3 mL of contrast medium was injected to confirm intra-articular placement. To anesthetize the joint, between 0.5 mL and 0.8 mL of bupivacaine 0.5% was carefully injected while monitoring the displacement of previously injected contrast medium. Injection was terminated if any contrast medium started to leave the joint or if resistance to injection started to increase, suggesting that the volume injected had reached the capacity of the joint space.
For blocks of the third occipital nerve, aliquots of 0.3 mL of local anesthetic were injected into each of the three target points for this nerve. [12] For C3 and C4 medial branch blocks, a test dose of 0.3 mL of contrast medium was injected to check for vascular uptake, and then 0.5 mL of local anesthetic was injected. [13]
For third occipital nerve blocks and medial branch blocks, physiological controls were used in the form of comparative local anesthetic blocks. [1214] On the first occasion that a nerve was blocked, either 0.5% bupivacaine or 2% lignocaine was used to block the nerve. If the response was positive, a second block with the other agent was performed not sooner than 1 week later. For a response to be deemed positive, the patient had to obtain complete relief of pain on each occasion that the nerve was blocked and obtain longer-lasting relief when bupivacaine was used than when lignocaine was used. All other responses were deemed not positive.
For lateral atlanto-axial joint blocks, anatomic controls were used. On a single-blind basis, the lateral atlanto-axial joint was blocked only if previously the patient had no response to third occipital nerve blocks. For an atlanto-axial joint block to be deemed positive, the patient had to report complete relief of headache.
For the investigation of headache, blocks were initiated at the C23 level. If an initial block of the third occipital nerve relieved the patients headache, we proceeded to a second block of the third occipital nerve to test the response. If this proved positive, investigations were terminated. If either the first or second block was negative and the patient wished to continue investigations, joints at adjacent levels were investigated. Early in the period of study, C34 was typically the second segment studied. However, later in the study, when evidence became available that lateral atlanto-axial joint pain could be treated surgically [15], C12 became the second choice. If blocks at C12 or C34 proved negative and the patient wished to continue investigations, then blocks at the C34 or C12 segment, respectively, were investigated. If blocks at C12, C23, and C34 proved negative, pursuit of the source of headache, per se, was abandoned, but the source of the patients neck pain was investigated with medial branch blocks at C56 or adjacent levels. Nonetheless, relief of headache, as well as neck pain, was monitored in these patients.
In patients with bilateral pain, blocks were performed on one side at a time, following the protocols outlined above. In those cases, the index pain was the pain on the side on which blocks were undertaken. If and once a source for that pain was identified, the other side was tested.
Data were collected to estimate the prevalence of particular sources of headache, the utility of individual diagnostic blocks, and the efficiency of the algorithm followed. Prevalence was defined as the number of patients who had a positive response to blocks of a particular source, divided by the total number of patients in the sample. Confidence intervals of that prevalence estimate were calculated as for the 95% confidence intervals of a proportion. The utility of each diagnostic block was calculated as the number of patients in whom a positive diagnosis was established when a particular block was used, divided by the number of patients who underwent that block. The efficiency of the algorithm followed was calculated as the number of patients in whom a positive diagnosis was eventually established, divided by the total number of blocks required to establish that diagnosis.
Ethics approval for this study was not required because no experimental procedures were performed, and the data were gathered in the course of conventional practice and reported in a deidentified manner. Exemption from ethics approval was obtained retrospectively from the Human Research Ethics Committee of the Hunter New England Area Health Service.
Results
The 166 patients studied were 91 males and 75 females, with a mean age of 46 years (standard deviation: 13.8; range: 18 to 84). On a 100mm visual analog scale, the mean intensity of the patients headache was 64 (standard deviation: 16.3; range: 40 to 100).
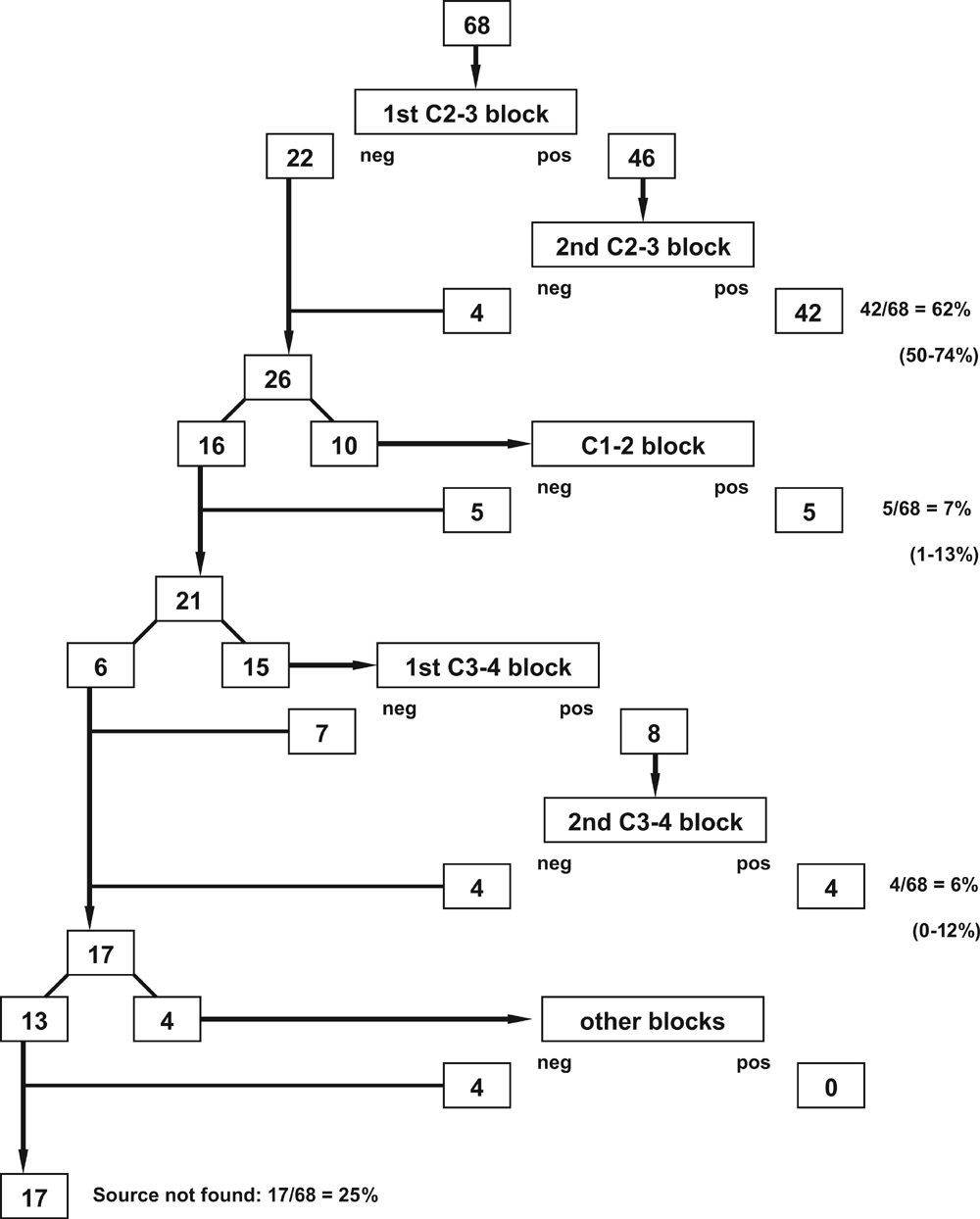
Figure 1
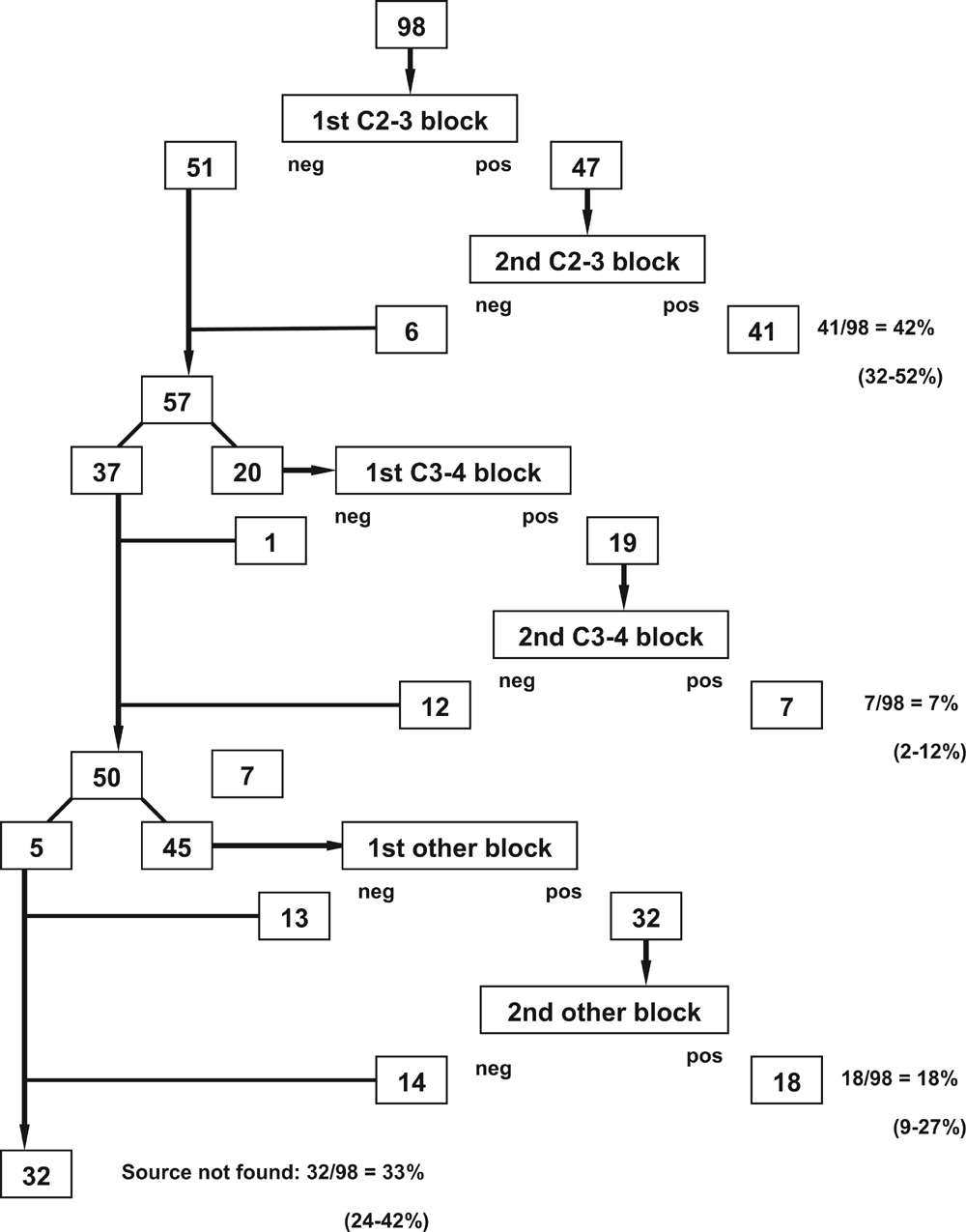
Figure 2 Figures 1 and 2 illustrate the clinical pathways followed by the patients and the diagnostic yield of each step. The numbers in the figures show the number of patients who underwent each type of block and the number who were found negative or positive. The proportions shown in these figures indicate the prevalence of the various possible sources of headache.
In the 68 patients in whom headache was the dominant symptom, blocks failed to identify a source in only 17 patients (25%). These included patients who elected not to pursue further investigations after various steps in the pathway (Figure 1). In the other 51 patients (75% of the initial sample), blocks were positive, most often at C23, followed by C12 and C34 (Figure 1). In this group of patients, blocks were positive only at these upper cervical levels. Forty-two had unilateral responses, and nine had bilateral responses.
In the 98 patients in whom headache was only an incidental symptom and neck pain predominated, blocks failed to identify a source of headache in 32 patients (33%) (Figure 2). In the other 66 patients, blocks were positive most often at C23, followed by lower cervical segments (Figure 2). All 66 had unilateral pain; none had bilateral pain. Lateral atlanto-axial joint blocks were not performed in this group of patients because their pain predominantly gravitated caudally into the neck, inviting pursuit of a source of pain lower than C12.
With respect to prevalence (95% confidence intervals), the C23 joint was the source of headache in 62% (5074%) of patients in whom headache was the dominant complaint and in 42% (3252%) of patients in whom headache was incidental to a predominant complaint of neck pain. Among the remaining patients with headache as the dominant complaint, the source of pain was C12 in 7% (113%) and C34 in 6% (012%). Among the remaining patients in whom headache was less severe than neck pain, the source of pain could be traced to the C34 joint in 7% (212%) and lower cervical joints in 18% (912%).
With respect to utility, in patients whose dominant complaint was headache, third occipital nerve blocks were positive in 62% (5074%) of patients in whom they were performed, C12 blocks were positive in 50% (1981%) of applications, and C34 blocks were positive in 27% (549%). In patients in whom neck pain was the dominant complaint, the utility of third occipital nerve blocks was 42% (3252%), the utility of C34 medial branch blocks was 35% (1456%), and that of lower cervical medial branch blocks was 40% (2664%).
With respect to efficiency, in the 68 patients in whom headache was the dominant symptom, 68 initial third occipital nerve blocks were required to identify 22 patients with negative responses and 46 patients with possible positive responses (Figure 1). A further 46 blocks were required to find 4 patients with false-positive responses and 42 patients with true-positive responses. This amounts to an efficiency of 114 blocks to find a source of pain in 42 patients, or 62% of inception cohort. Subsequently, an additional 7% of patients were found positive after a total of 10 lateral atlanto-axial blocks, and a further 6% were found positive after a total of 23 C34 medial branch blocks. This amounts to a final efficiency of 55 of 68 patients (75%) diagnosed for a cost of 147 blocks or an average of 2.7 blocks per patient diagnosed. Blocks at lower cervical levels proved ineffective in this sample, but very few patients were investigated at these levels (Figure 1).
In patients with predominantly neck pain, 98 initial third occipital blocks and 47 control blocks were required to find 41 patients whose headache was relieved. After 39 additional C34 blocks, a further 7 patients were found positive, and 77 medial branch blocks at lower cervical levels were required to find an additional 18 patients with positive response. This amounts to a total efficiency of 66 of 98 patients diagnosed for the cost of 265 blocks or an average of 4 blocks per patient diagnosed.
Discussion
In an ideal study of prevalence, all patients would undergo diagnostic blocks at each and every target spinal segment to determine exactly what the rates were of true-positive, false-positive, true-negative, and false-negative responses for each block and for each segment. This is neither humanely nor logistically possible. Patients for whom a diagnosis was established early could not be expected to undergo superfluous or redundant extra procedures at other segmental levels simply to provide negative results for statistical purposes. For that reason, the protocol followed in the present study was pragmatic. Blocks were performed in a sequence based on the pretest probability of the target segments being the source of pain, according to the published evidence at the time that the study was conducted.
The present study did not focus on patients with negative responses in order to find out why their responses were negative or whether there might be some other source of pain that was not tested. The choice of patients to no longer pursue diagnosis was respected. Under those conditions, a diagnosis could not be established in some 30% of patients and remains unknown. However, lack of attention to negative responses does not compromise the positive findings.
The results of the present study show that the C23 zygapophysial joint is the most common source of headache, both in patients with headache as a dominant complaint (62%; 5074%) and in patients with headache less intense than neck pain (42%; 3252%). Although notionally different, these prevalence rates are not significantly different statistically. In both instances, these figures are consonant with the original prevalence estimate of 53% (3867%) [10] and thereby corroborate it.
Second, the results show that the prevalence of a source of headache at C12 or C34 is low but not zero. In each case, the actual prevalence might be greater than those encountered in the present study because not all patients underwent investigations at these segmental levels. Some of the patients who declined further investigation might have responded had they been investigated.
The prevalence estimates, derived in the present study, for headache stemming from C12, C34, or lower levels are likely to be reasonably valid, for their confidence intervals are tight (±6%). However, future studies might be able to find more valid prevalence estimates if larger numbers of patients are investigated. However, any such study would need to take into account that most patients with probable cervicogenic headache will be positive at C23, and, therefore, to provide larger samples of patients with pain from C12 and C34, an inception cohort much larger than that of the present study would need to be recruited.
The utility data from the present study are liable to be misinterpreted. Yields of only 35% or 27% might seem unimpressive, but these need to be interpreted in context. There is no other diagnostic test for cervicogenic headache. So, the default position is that no diagnosis can be made beyond probable cervicogenic headache. In that context, a yield even as low as 27% is a substantial improvement. Moreover, the collective yield of diagnostic blocks is massive, raising the rate of a positive diagnosis from zero to 66% or 75%, depending on whether headache is the dominant complaint or not.
The foremost determinant of the utility of a diagnostic block is the prevalence of the condition being tested. Consequently, third occipital nerve blocks have a high utility because pain from the C23 joint is common. Lateral atlanto-axial joint blocks and C34 medial branch blocks have lower utility because the conditions that they test are less common. Nonetheless, low yields are not inconsequential when they allow a diagnosis to be made in a further 6% and 7% of patients. These properties also have a bearing on the efficiency of diagnostic algorithms for cervicogenic headache.
The data of the present study vindicate and refine previously published algorithms for the investigation of cervicogenic headache. [4, 16] To maximize efficiency, these algorithms were based on pretest probability and the principle that common conditions should be investigated first. Doing so reduces the number of blocks eventually required to diagnose those patients in whom a first block does not provide a diagnosis.
Investigations are best initiated at C23, with third occipital nerve blocks. Doing so identifies the majority of patients in whom a diagnosis is possible. It also increases the utility of subsequent blocks in the remaining patients because patients with pain from C12 or C34 will be concentrated among these remaining patients, rather than diluted by the large numbers of patients in the initial sample with pain from C23. Commencing investigations arbitrarily at C12 or C34, i.e., before investigating C23, is inefficient. The low prevalence of pain from these segments means that most blocks at these levels would be negative if they were performed as the first investigation. The yields of blocks at both C12 and C34 increase if blocks at these segments are performed only in patients previously negative to third occipital nerve blocks.
The present data show that, in patients with headache as a dominant symptom, if third occipital nerve blocks are negative, either C12 or C34 should be the next target because the prevalence of pain from these sources is essentially equal. The converse applies to patients with headache as an incidental feature to neck pain. In these patients, C23 is the most common source, but the next most common source is among the joints at C56 and C67. Therefore, lower cervical blocks should be the second step. Blocks at C34 become the third step.
The figures derived in the present study are subject to certain limitations and, therefore, possible errors. Comparative local anesthetic blocks are not a perfect test. They have a specificity of only 0.88 [17], which means that 12% might be false-positive, despite two blocks providing complete relief of pain. Meanwhile, no form of control for lateral atlanto-axial joint blocks has been validated. [11] Therefore, the prevalence estimates reported in the present study might be adjusted downward by future studies that use more rigorous controls, should they become available. However, in that event, the adjustments in prevalence would not materially compromise the principles promoted by the present data.
The results of the present study constitute a proof of principle that, in the majority of patients with probable cervicogenic headache, a source of pain can be pinpointed if controlled diagnostic blocks are used, as required by the International Headache Society. [1] The source of pain will most likely lie in the upper three cervical synovial joints, with C23 being the most common source. With varying degrees of likelihood and certainty, alternative sources lie in the C12 joint, the C34 joint, or lower cervical joints.
Finding sources of headache in the C12, C23, and C34 joints is consonant with the current paradigm of cervicogenic headache, which maintains that the headache constitutes referred pain from the upper cervical spine, the mechanism of which lies in the convergence, in the spinal nucleus of the trigeminal nerve, of trigeminal afferents and afferents from the C1, C2, and C3 spinal nerves. [5] Harder to explain is the mechanism in that small proportion patients with nondominant headache that can be relieved by blocks at lower cervical levels. The fact that the headache in these patients is less of a complaint than their neck pain suggests that the headache is secondary to their lower cervical pain. A now old study showed that patients with predominantly lower cervical pain commonly exhibited biomechanical abnormalities in the upper cervical spine [18], ostensibly caused by excessive muscle activity that was stimulated by lower cervical pain but exerted across upper cervical segments. In such cases, secondary headache may be due to muscle pain, which was not targeted by any of the upper cervical blocks used in the present study. Nor was there a need to develop such blocks, because the secondary headache could be relieved by treating the lower cervical pain.
Acknowledgements
This article is based on data collected by the late Dr. Jay Govind in his clinical work at the Royal Newcastle Hospital and later the Royal Newcastle Centre. Dr. Govind passed away in 2009 before publishing this work [19]. The present article was developed by using the data collected by Dr. Govind, as well as notes and drafts exchanged by the two authors when preparing the manuscript. The work was presented at the annual scientific meeting of the Spine Society of Australia in 2008, where it was awarded a prize for best presentation.
Disclosure statement
Authors have no disclosures to report.
References:
International Headache Society.
The International Classification of Headache Disorders, 2nd edition.
Cephalalgia 2004;24(24 Supp 1):1156.Bogduk N.
Distinguishing primary headache disorders from cervicogenic headache:
Clinical and therapeutic implications.
Headache Curr 2005;2(2):2736.Bogduk N, Bartsch T.
Headaches of cervical origin: Focus on anatomy and physiology.
In: Goadsby PJ, Silberstein SD, Dodick DW, eds.
Chronic Daily Headache for Clinicians.
London: BC Decker; 2005:36981.Bogduk N, Bartsch T.
Cervicogenic headache.
In: Silberstein SD, Lipton RB, Dodick DW, eds.
Wolffs Headache, 8th edition.
New York: Oxford University Press; 2008:55170.Bogduk, N and Govind, J.
Cervicogenic Headache: An Assessment of the Evidence on
Clinical Diagnosis, Invasive Tests, and Treatment
Lancet Neurol. 2009 (Oct); 8 (10): 959968Antonaci F, Ghirmai S, Bono S, Sandrini G, Nappi G.
Cervicogenic headache: Evaluation of the original diagnostic criteria.
Cephalalgia 2001;21(5):57383.Bovim G, Berg R, Dale LG.
Cervicogenic headache: Anaesthetic blockades of cervical
nerves (C2-C5) and facet joint (C2/C3).
Pain 1992;49(3):31520.Bogduk N.
Role of anesthesiologic blockade in headache management.
Curr Pain Headache Rep 2004;8(5):399403.Bogduk N.
Diagnostic nerve blocks in chronic pain.
In: Breivik H, Shipley M, eds.
Pain: Best Practice & Research Compendium.
Edinburgh: Elsevier; 2007:4755.Lord S, Barnsley L, Wallis B, Bogduk N.
Third occipital headache: A prevalence study.
J Neurol Neurosurg Psychiat 1994;57(10):118790.International Spine Intervention Society.
Lateral atlanto-axial joint blocks.
In: Bogduk N, ed.
Practice Guidelines for Spinal Diagnostic and Treatment Procedures, 2nd edition.
San Francisco, CA: International Spinal Intervention Society; 2013:3562.International Spine Intervention Society.
Third occipital nerve blocks.
In: Bogduk N, ed.
Practice Guidelines for Spinal Diagnostic and Treatment Procedures, 2nd edition.
San Francisco, CA: International Spinal Intervention Society; 2013:14163.International Spine Intervention Society.
Cervical medial branch blocks.
In: Bogduk N, ed.
Practice Guidelines for Spinal Diagnostic and Treatment Procedures, 2nd edition.
San Francisco, CA: International Spinal Intervention Society; 2013:10139.Barnsley L, Lord S, Bogduk N.
Comparative local anaesthetic blocks in the diagnosis
of cervical zygapophysial joints pain.
Pain 1993;55:99106.Schaeren S, Jeanneret B.
Atlantoaxial osteoarthritis: Case series and review of the literature.
Eur Spine J 2005;14(5):5016.International Spine Intervention Society.
An algorithm for the conduct of cervical synovial joint blocks.
In: Bogduk N, ed.
Practice Guidelines for Spinal Diagnostic and Treatment Procedures, 2nd edition.
San Francisco, CA: International Spinal Intervention Society; 2013:30312.Lord SM, Barnsley L, Bogduk N.
The utility of comparative local anaesthetic blocks versus placebo-controlled
blocks for the diagnosis of cervical zygapophysial joint pain.
Clin J Pain 1995;11:20813.Amevo B, Aprill C, Bogduk N.
Abnormal instantaneous axes of rotation in patients with neck pain.
Spine 1992;17(7):74856.Bogduk N.
In Memoriam. Jayantilal Govind MB, ChB, DPH, MMed(Pain Med), FAFOM, FAFMM.
Pain Med 2009;10(6):115960
Return to HEADACHE
Since 4-06-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |