

Conservative Spine Care: Opportunities to
Improve the Quality and Value of CareThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Popul Health Manag. 2013 (Dec); 16 (6): 390–396 ~ FULL TEXT
OPEN ACCESS Thomas M. Kosloff, DC, David Elton, DC, Stephanie A. Shulman, DVM, MPH,
Janice L. Clarke, RN, Alexis Skoufalos, EdD, and Amanda Solis, MS
Physical Health, Optum Health,
Kingston, New York.
Low back pain (LBP) has received considerable attention from researchers and health care systems because of its substantial personal, social, work-related, and economic consequences. A narrative review was conducted summarizing data about the epidemiology, care seeking, and utilization patterns for LBP in the adult US population. Recommendations from a consensus of clinical practice guidelines were compared to findings about the current state of clinical practice for LBP. The impact of the first provider consulted on the quality and value of care was analyzed longitudinally across the continuum of episodes of care. The review concludes with a description of recently published evidence that has demonstrated that favorable health and economic outcomes can be achieved by incorporating evidence-informed decision criteria and guidance about entry into conservative low back care pathways.
From the FULL TEXT Article:
Introduction
The united states has the most expensive and complex health care system in the world, [1] yet the magnitude of funds spent on the system has failed to provide commensurate benefits in terms of quality, access, and cost performance. [2]
To achieve value for the current levels of investment in care, the factors that contribute to variation in costs and quality must be addressed. In fact, experts have concluded that the quality and efficiency of the US health care system could be improved by approaches that address overuse, and inappropriate or ineffective use of care — the chief factors contributing to the current high levels of expenditures, inefficiency, and waste. [3]
A previous article analyzed current practices regarding the use of coronary stents in the chronic stable angina patient. [4] Musculoskeletal disorders represent another diagnostic class that, while usually not life threatening, results in a high prevalence of morbidity and significant societal burden. [5] Low back pain (LBP) management in particular has been linked to inefficiency and waste. [6] This is likely related, in part, to the growing list of treatment approaches recommended for conservative care (pharmacologic and non-pharmaceutical options) and the difficulty in determining the best option for each patient. [7]
Although useful in assisting practitioner and patient decisions about appropriate health care for specific clinical circumstances, [8] clinical practice guidelines (CPGs) are not sufficient to maximize effectiveness and cost-effectiveness at the individual level (ie, targeting specific care). [9] The clinical appropriateness of health care services at the individual level can be assessed by considering the patient's clinical characteristics, the relevant risk factors, the setting or health care provider type, the severity of the illness, and the specific requirements for a procedure (eg, availability of the service). [9]
The purpose of this article is to discuss the challenges associated with management of LBP and describe an evidence-informed process to effectively and cost-effectively integrate individual patient conservative care for LBP with appropriate population-based recommendations found in high-quality CPGs.
Back Pain—An Overview
Pain affects millions of Americans; contributes greatly to national rates of morbidity, mortality, and disability; and is rising in prevalence. [10] Back pain is the most common physical condition for which patients visit their doctor, [6] and surveys reveal that over one quarter of adults (26%) report LBP in the past 3 months. [11] The lifetime prevalence of LBP is approximately 85% (probably closer to 100% of adults). [12]
A substantial majority of those who suddenly develop LBP improve quickly with or without professional care. However, recurrences and flare-ups are common, and individuals with chronic LBP tend to show a more persistent course. [13] Thus, LBP is best viewed as a recurrent disorder that can occur anytime in a person's life and fluctuates between no/mild pain to debilitating pain. [12] Important prognostic factors are related to the back pain episode, individual and psychological characteristics, as well as the work and social environment. [13]

Figure 1 About 1 in 2 people who experience LBP seek health care during an episode. [14] Care seekers tend to be those who have high levels of disability, [15] and/or who are experiencing more severe pain, more distal pain, work-related pain, and those who are more fearful about what the pain might mean. [14] Clinicians most commonly consulted for back pain in North America are chiropractors, general medical practitioners, and orthopedists. [14] When initial care seeking is calculated on an episodic basis, chiropractors and primary care physicians (PCPs) are by far the provider types most commonly consulted (D. Elton, unpublished data, 2010) (Figure 1). About 85% to 90% of individuals who seek care are assessed as having nonspecific or ordinary LBP (ie, not associated with a specific cause including serious pathology). [16]
Increasingly, back pain has become a financial concern because of the high associated direct and indirect costs of testing and treatment. Cost estimates vary, but the most recent estimates (2008) put care related to back pain at $86 billion in incremental health care costs. [17] A 49% increase in the number of patients seeking spine-related care (from 12.2 million in 1997 to 18.2 million in 2006) was the largest contributing factor to increased outpatient expenditures. [18] Adding to the problem is a sharp increase in the number of investigations and interventions performed related to back pain, including imaging, injections, surgical procedures, implantable devices, and medications. These services have value for some patients, but it appears that they are being used in areas beyond those for which data support an improvement in outcomes. [19]
Despite the fact that the proportion of office visits has changed little since 1990, there has been remarkable (307%) growth in the use of lumbar magnetic resonance imaging (MRI) in the Medicare population from 1994 to 2004. [21] Using current guidelines as a baseline, one third to two thirds of spinal computed tomography (CT) imaging and MRI may be inappropriate. [19]
Use of opioid prescriptions also has increased by 108% from 1997 to 2004 resulting in a 423% inflation-adjusted increase in expenditures. [19] The number of spinal injections grew more than 200% over the same time period, and spine surgery rates have risen over 200% from 1997–2004. Spine imaging rates vary across geographic regions, and the rate of surgery is highest where imaging rates are highest. Moreover, the evidence shows that despite newer technologies, higher spine surgery rates can be associated with worse outcomes. [19]
The Challenge of Low Back Pain
Patient “care-seeking” decisions for LBP initiate a cascade of management services and processes representing clinical pathways that may or may not equate to the most appropriate intervention for individuals. [20] Treatment choices can be influenced by patients depending on the types of health care providers they choose to consult, which in turn influences the types of treatments received. [21] In many instances, circumstances require that patients navigate LBP management on their own. [22]
Fundamental challenges include:
Provider Type — People who develop LBP and wish to seek care are first required to select a health provider. To a large degree, the tests and services provided to individuals are dependent upon the health care professional type from whom a patient first seeks care. [21, 23] More than 20 different health care provider types (eg, physicians, allied health, complementary and alternative medicine) may be considered when seeking treatment for LBP. [7]
Treatment Options — The challenge of weighing alternate treatment options for LBP does not end once the choice of a specific type of health provider is made. A partial list of treatment options available to a person with LBP includes more than 200 different medications, therapies, injections, products, or procedures. [7] It is difficult for any health care provider involved in the management of LBP to understand the relative benefits and harms of each intervention at a level that is sufficient to advise his or her patients.
Individual Patient Variations — The selection of the correct intervention for LBP is further complicated by differences in baseline prognoses among patients seeking care. [24] An important consideration when commencing an episode of care is the “targeting” of interventions that address individual risk factors. [25]
Review of Clinical Practice Guidelines for Low Back Pain
A number of CPGs have been published recently that focus on the management of acute and/or persistent (chronic) common (nonspecific) LBP. [26–35] Typically, these guidelines commence with patient decisions to enter primary care management. They describe recommendations for diagnostic assessment, treatment options (eg, self-care, pharmacotherapy, non-pharmacologic interventions), and indications for referral for testing and specialist care.
Synthesized recommendations from these CPGs provide a consistent set of “quality” recommendations concerning processes of care. [36-38] Specifically, 10 CPGs sponsored by 10 different international organizations during the past decade were compared and summarized in a recent text. [13] Both acute and chronic LBP complaints were represented, providing an overview of the best available evidence to inform clinical judgment. Although each new CPG may emphasize a distinct aspect of care or a specific subgroup, the collective recommendations have been largely consistent, with only minor changes throughout the years based on new evidence. [17, 30]
Among these guidance documents, there was general agreement on 5 main sequential goals when conducting an assessment of LBP:
Ruling out potential serious pathology (eg, infection).
Ruling out specific causes of LBP (eg, spinal stenosis).
Ruling out substantial neurological involvement.
Evaluating the severity of symptoms and functional limitations.
Identifying risk factors for chronicity. [13]
For the 85%–90% of individuals assessed as having nonspecific or ordinary LBP, CPGs recommend against routine imaging (eg, radiography, CT scan, MRI), stronger opioid analgesics, and injection procedures (eg, epidural, facet, soft tissue).
Instead, the consensus of the guidelines suggests that patients with acute, nonspecific LBP should:
be reassured of a good prognosis,
be educated in self-care,
remain active,
use over-the-counter medications (eg, acetaminophen, nonsteroidal anti-inflammatory drugs) or spinal manipulation, or both as a first line of symptom control. [30]
Other physical modalities (eg, traction, ultrasound, transcutaneous electrical nerve stimulation) and supports/braces are not recommended by CPG developers. Supervised exercise and, to a lesser degree, behavioral modification and/or acupuncture therapies also are recommended for individuals who have chronic or persistent LBP. [38]
In summary, the goal of CPGs is to provide algorithms whereby busy clinicians can quickly determine/identify “best practice” alternatives for their patients that are based on careful evaluation of the evidence. [39] Ideally, CPGs focus on common problems with significant morbidity or mortality. Back pain fits this ideal. Whether CPGs are worth the resources that continue to be dedicated to them remains a matter of speculation. [40]
Current Clinical Practices
When followed by providers and patients, evidence-based guidelines for the clinical management of LBP have been associated with better functional outcomes, reduced health care utilization, and lower health care costs. [41, 42] Yet there is a strong body of evidence suggesting a low level of adherence to guidelines in daily clinical practice. [43, 44] Overall adherence to guideline-based care by PCPs has been recorded at 65%, a rate that has remained unchanged despite attempts to increase implementation of evidence-based care. [43] For acute nonspecific LBP, 65% of the cases receive recommendations for imaging studies despite clear guidance that this is not routinely indicated. [45] Only half of LBP patients who see a PCP receive a recommendation to remain active. [45] Manipulation, which is supported by most guidelines, is recommended by PCPs in only 2% of the acute nonspecific LBP cases. This gap in adherence to evidence-based practice recommendations by clinicians has become popularly known as the “know-do gap” — the gap between what is known and what is done in practice. [46, 47]
These national trends are contextualized by data that describe the timing of services received by patients seeking care for spinal pain in the “real world” of clinical practice. A recently published analysis of nationwide private insurer claims covering more than 8 million lives revealed the front-loading of treatment expenditures, even among patients with nonspecific LBP. [17] “Contrary to clinical guidelines, many patients with low back pain start incurring significant resource use and associated expenses soon after the index [initial] diagnosis.” [17] p.623
The analysis showed:
Diagnostic and treatment interventions were common in the first month.
More than 32% of patients with LBP received X-rays, with at least 50% receiving them on the same day as the initial diagnosis.
Second-line medication was prescribed for 69.4% of patients, with at least 50% of those patients filling the prescription within 8 days of the initial diagnosis.
Opioids were prescribed for 41.6% of patients, and more than half of the prescriptions were filled within 25 days of the initial visit.
The median number of days to surgery was 90 for all those having surgery. Surgery was performed within 54 days (median) of the initial diagnosis for those individuals not classified as having chronic LBP (>3 months duration).

Table 1 The impact of non-adherence to evidence-based CPGs has been measured by analyzing episodes of care — a method that provides longitudinal data across the entire pathway of care (eg, total number of health care providers seen by the individual throughout the episode of care, the diagnostic tests performed, the medication prescribed). [48] As demonstrated by data synthesized by Elton (Figure 1), individuals with similar risk profiles who begin their care pathway with a chiropractor or PCP see fewer total health care providers throughout the overall episode of care than do individuals who initially consult an orthopedic specialist, physical medicine/rehabilitation specialist, or physical/occupational therapist (Table 1). Individuals who commence an episode of care with a chiropractor or PCP are less likely to undergo imaging and are prescribed fewer medications. Also, they are more likely to receive first-line management options as recommended by CPGs.
These findings are similar to recently published data. A 2-year retrospective claims analysis of BlueCross BlueShield TN members presenting with LBP employed a similar episode treatment grouping methodology. “Paid costs for episodes of care initiated with a DC [chiropractor] were almost 40% less than episodes initiated with an MD [physician]. Even after risk adjusting each patient's costs, we found that episodes of care initiated with a DC were 20% less expensive than episodes initiated with an MD.” [49]
The current management of back pain has led to increased resource usage without a corresponding improvement in outcomes. In a nationally representative population sample (Medical Expenditure Panel Survey), trends in health care expenditures from 1997 to 2005 were calculated for adults who self-reported spine problems (neck pain and LBP). [50] Spine-related expenditures were found to have increased substantially from 1997 to 2005 without evidence of corresponding improvement in self-assessed health status, functional disability, work limitations, or social functioning.
These findings about the current state of clinical practice for spine-related disorders provide substance to the assertion that we need to rethink frontline care for back pain. [23]
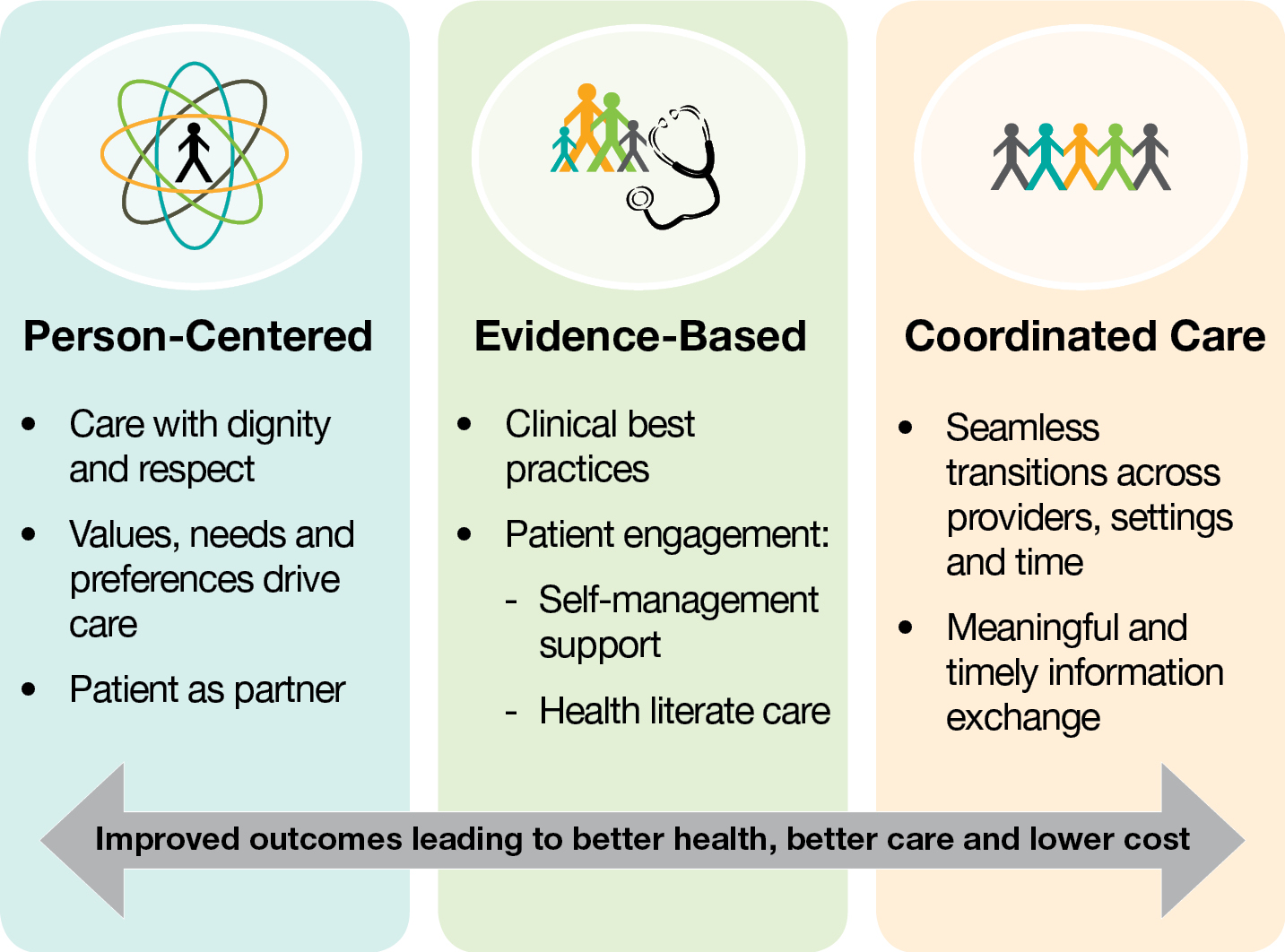
Patient-Centered Conservative Care
Decision criteria and guidance about entry into conservative LBP care pathways represent an opportunity to advance the quality and delivery of health services. The choice of initial health care provider matters when it comes to spine-related disorders. The variable impact of “first provider seen” is greatest for the 85%–90% of health care consulters who have “nonspecific” spine-related pain. [24] For these patients, guidelines highlight the importance of assessing a broad range of potential influences on prognosis including fears and anxieties about pain, physical limitations related to pain, mood, motivation, and work situation. [29, 32, 35]

Figure 2 Previous authors have postulated that targeting specific back pain interventions for particular subgroups of patients holds great potential for boosting their effectiveness. [51, 52] “However, this is often difficult to do in practice and, until recently, no validated tool has existed to inform clinicians or others about the risk status of individual patients.” [53] The STarT Back Screening Tool (SBST), developed by researchers at Keele University (United Kingdom) with funding from Arthritis Research UK, can be administered prior to initiating treatment. This tool presents an opportunity to fill a serious knowledge gap in the delivery of health services by incorporating evidence-informed decision criteria and guidance about entry into conservative low back care pathways (Figure 2).
This classification-based model for the management of LBP has been shown to improve clinical outcomes and address the inappropriate utilization of services. [25] It is predicated on the understanding that not all patients entering a care pathway for nonspecific LBP are the same. Primary care data suggest that, for first contact settings such as general practitioner consultations, approximately 55% of patients with nonspecific LBP are at low risk of poor outcome (ie, patients who are likely to do well irrespective of treatment); 33% are at medium risk; and 12% are at high risk. [24]
Appropriate individualized care management may be facilitated when the first health care provider seen is best equipped to administer the treatment most likely to benefit a particular patient. [23] Using the SBST approach, individuals at “low risk” usually benefit most from receiving reassurance and advice, which can be rendered by PCPs, nurses, or health coaches (Table 2). The treatment options recommended for persons at “medium risk” — manual therapy (eg, manipulation) and specific exercises—are most typically provided by chiropractors and physical therapists. Optimally, the management of patients at “high risk” should be overseen by physical therapists or chiropractors, who are skilled in providing behavioral therapy in addition to the same strategies targeted for patients at medium risk. [54]
This framework has demonstrated “proof of principle” in a recently published clinical trial. [25] “The results showed the SBST approach changes the pattern of management and referral in a way that is more appropriate for patients' needs.” [53] When compared to current best practice, use of the SBST tool along with targeted treatments increased efficiency, improved clinical outcomes, and reduced health care costs.
Almost half of the “low-risk” patients in the usual care group, who typically respond well to self-care management, were referred for supervised physical therapy. In contrast, more than 90% of those allocated to the SBST group were provided with advice and education to support self-care management. Conversely, more than a third of patients likely to benefit from supervised therapy (medium- and high-risk categories) in the usual care group did not receive referrals. Virtually all those patients in the SBST group, who were similarly categorized, were referred for therapy.
Overall, 75% of the SBST group were referred for physical therapy vs. 60% of controls. Despite this greater rate of referral, the costs over 12 months were about 13% less for the SBST group. Savings were attributed in large part to more efficient utilization. The SBST referral group averaged 4.2 visits, while the usual care group received a mean of 5.1 visits.
At 4 and 12 months, the SBST group demonstrated superior patient-important outcomes compared to the “usual care” control group at both 4 and 12 months. Adjusted mean changes in disability scores were significantly better in the SBST group than in the control group at 4 months and at 12 months. The patients in the SBST group were significantly more likely to be satisfied with treatment and lost fewer days of work. Importantly, those individuals in the low-risk category who did not receive referral for therapy did as well or slightly better than those in the same risk category who did receive a course of physical therapy.
Conclusion
The current state of the conservative management of LBP is summarized in this narrative review. Current clinical practice has been ineffective in meeting the challenge of consistently adhering to the recommendations of modern evidence-based guidelines. It is not surprising that patient “care-seeking” decisions for LBP initiate a cascade of interventions that may or may not represent the most appropriate management for individuals.
One opportunity to facilitate compliance with clinical guidelines is to assure that the first health care provider seen is best able to administer the treatment likely to benefit a particular patient. This can be achieved, in part, by implementing a triage approach for the early referral of well-defined subgroups of patients into appropriate clinical pathways. Recently published evidence supports this premise. The STarT Back subgrouping and targeted treatment approach has been shown to significantly improve patient outcomes (effectiveness) and is associated with substantial economic benefits (efficiency) compared with current usual practice. [24]
Author Disclosure Statement
Drs. Kosloff, Elton, and Shulman are employees of Optum Health Care Solutions. Optum Health Care Solutions is currently contracted with the Jefferson School of Population Health to develop programs around over-utilization in health care. Ms. Clarke, Dr. Skoufalos, and Ms. Solis are employees of the Jefferson School of Population Health, which has been contracted to collaborate with Optum Health Care Solutions on programs regarding health care over-utilization.
The authors received no financial support for the research, authorship, and/or publication of this article.
References:
Sarpel U, Vladeck BC, Divino CM, Klotman PE.
Fact and fiction: Debunking myths in the US healthcare system.
Ann Surg. 2008;247(4):563–569Institute of Medicine Committee on Quality of Health Care in America.
Crossing the Quality Chasm: A New Health System for the 21st Century
Washington, DC: National Academies Press; 2001Davis K, Schoen C, Guterman S, Shih T, Schoenbaum SC, Weinbaum I.
Slowing the growth of U.S. health care expenditures: What are the options?
Available at:
http://www.commonwealthfund.org/Publications/Fund-Reports/2007/Jan/
Slowing-the-Growth-of-U-S–Health-Care-Expenditures–What-Are-the-Options.aspx
Accessed October11, 2012Behnke LM, Solis A, Shulman SA, Skoufalos A.
A targeted approach to reducing overutilization: Use of percutaneous coronary intervention in stable coronary artery disease.
Popul Health Manag. Epub ahead of print October31, 2012Woolf AD, Erwin J, March L.
The need to address the burden of musculoskeletal conditions.
Best Pract Res Clin Rheumatol. 2012;26:183–224American Academy of Orthopaedic Surgeons Spine:
Low back and neck pain.
In: The Burden of Musculoskeletal Diseases in the United States. Available at:
http://www.boneandjointburden.org/pdfs/BMUS_chpt2_spine.pdf
Accessed October11, 2012Haldeman S, Dagenais S.
A Supermarket Approach to the Evidence-informed Management of Chronic Low Back Pain
Spine Journal 2008 (Jan); 8 (1): 1–7Field MJ, editor; , Lohr KN, editor. , eds.
Clinical Practice Guidelines: Directions for a New Program.
Washington, DC: National Academy Press; 1990;38Lavis JN, Anderson GM.
Appropriateness in health care delivery: Definitions, measurement and policy implications.
CMAJ. 1996;154:321–328Schiller JS, Lucas JW, Ward BW, Peregoy JA.
Summary health statistics for U.S. adults: National Health Interview Survey, 2010.
Vital Health Stat 10. 2012;10(252):1–207Paulose R, Hertz RP.
The Burden of Pain Among Adults in the United States PDF
2008 Pfizer Inc.Dagenais S, Haldeman S.
Evidence-Based Management of Low Back Pain.
St Louis, MO: Mosby, Inc. (Elsevier); 2012:1–2Hayden JA, Dunn KM, van der Windt DA, Shaw WS.
What is the prognosis of back pain?
Best Pract Res Clin Rheumatol. 2010;24:167–179Kent PM, Keating JL.
The epidemiology of low back pain in primary care.
Chiropr Osteopat. 2005;13:13.Ferreira ML, Machado G, Latimer J, Maher C, Ferreira PH, Smeets RJ.
Factors defining care-seeking in low back pain—a meta-analysis of population based surveys.
Eur J Pain. 2010;14:747.e1–7Deyo RA, Weinstein JN.
Low back pain.
N Engl J Med. 2001;344:363–370Ivanova JI, Birnbaum HG, Schiller M, Kantor E, Johnstone BM, Swindle RW.
Real-world practice patterns, health-care utilization, and costs in patients with low back pain: the long road to guideline-concordant care.
Spine J. 2011;11:622–632Martin BI, Turner JA, Mirza SK, Lee MJ, Comstock BA, Deyo RA.
Trends in Health Care Expenditures, Utilization, and Health Status Among US Adults
With Spine Problems, 1997-2006.
Spine (Phila Pa 1976). 2009 (Sep 1); 34 (19): 2077–2084Deyo RA, Mirza SK, Turner JA, Martin BI.
Overtreating Chronic Back Pain: Time to Back Off?
J Am Board Fam Med. 2009 (Jan); 22 (1): 62–68Fourney DR, Dettori JR, Hall H, Härtl R, McGrit MJ, Daubs MD.
A systematic review of clinical pathways for lower back pain and introduction of the Saskatchewan spine pathway.
Spine (Phila Pa 1976). 2011;36(21 suppl):S164–S171Carey TS, Freburger JK, Holmes GM, et al.
A long way to go: Practice patterns and evidence in chronic low back pain care.
Spine (Phila Pa 1976). 2009;34:718–724Weisel SW, editor. , ed.
Has there been any progress in the management of low back pain?
The BackLetter. 2011;26:109–116Hartvigsen J, Foster N, Croft PR.
We need to rethink front line care for back pain.
BMJ. 2011;342:d3260.Hill JC, Dunn KM, Lewis M, et al.
A Primary Care Back Pain Screening Tool: Identifying Patient Subgroups For Initial Treatment
(The STarT Back Screening Tool)
Arthritis Rheum. 2008 (May 15); 59 (5): 632–641Hill JC, Whitehurst DGT, Lewis M, et al.
Comparison of Stratified Primary Care Management For Low Back Pain With
Current Best Practice (STarT Back): A Randomised Controlled Trial
Lancet. 2011 (Oct 29); 378 (9802): 1560–1571Accident Compensation Corporation, New Zealand Guidelines Group
New Zealand Acute Low Back Pain Guide PDF
Wellington, NZ: Accident Compensation Corporation (ACC); 2004Airaksinen O, Brox JI, Cedraschi C, et al.
COST B13 Working Group on Guidelines for Chronic Low Back Pain Chapter 4.
European Guidelines for the Management of Chronic Nonspecific Low Back Pain
European Spine Journal 2006 (Mar); 15 Suppl 2: S192–300Australian Acute Musculoskeletal Pain Guidelines Group
Evidence-Based Management of Acute Musculoskeletal Pain PDF
Brisbane, Australia: Australian Academic Press Pty. Ltd.; 2003Chou R, Qaseem A, Snow V, Casey D, Cross JT Jr., Shekelle P, Owens DK:
Diagnosis and Treatment of Low Back Pain: A Joint Clinical Practice Guideline
from the American College of Physicians and the American Pain Society
Annals of Internal Medicine 2007 (Oct 2); 147 (7): 478–491Negrini S, Giovannoni S, Minozzi S, et al.
Diagnostic therapeutic flow-charts for low back pain patients: The Italian clinical guidelines.
Eura Medicophys. 2006;42:151–170Nielens H, Van Zundert J, Mairiaux P, et al.
Chronic Low Back Pain PDF
Report No. 48C. Brussels, Belgium:
Belgian Health Care Knowledge Centre (KCE); 2006National Institute for Health and Clinical Excellence (NICE).
Low Back Pain: Early Management of Persistent Nonspecific Low Back Pain PDF
London: National Institute for Health and Care Excellence; 2009.
[Report No.: Clinical guideline 88].The Norwegian Back Pain Network
Acute Low Back Pain: Interdisciplinary Clinical Guidelines PDF
Oslo, UK: The Norwegian Back Pain Network; 2002Institute of Health Economics Alberta Canada.
Evidence-Informed Primary Care Management of Low Back Pain
February 2017van Tulder M, Becker A, Bekkering T, Breen A, Carter T, Gil del Real MT.
European Guidelines for the Management of Acute Nonspecific Low Back Pain in Primary Care
European Spine Journal 2006 (Mar); 15 Suppl 2: S169–191Dagenais S, Tricco AC, Haldeman S.
Synthesis of Recommendations for the Assessment and Management of Low Back Pain
From Recent Clinical Practice Guidelines
Spine J. 2010 (Jun); 10 (6): 514–529Koes BW, van Tulder M, Lin CW, Macedo LG, McAuley J, Maher C.
An Updated Overview of Clinical Guidelines for the Management of Non-specific Low Back Pain
in Primary Care
European Spine Journal 2010 (Dec); 19 (12): 2075–2094Pillastrini P, Gardenghi I, Bonetti F, et al.
An Updated Overview of Clinical Guidelines for Chronic Low Back Pain
Management in Primary Care
Joint Bone Spine 2012 (Mar); 79 (2): 176–185Hayward RS, Wilson MC, Tunis SR, Bass EB, Guyatt G.
Users' guides to the medical literature. VIII:
How to use clinical practice guidelines.
A. Are the recommendations valid?
The Evidence-Based Medicine Working Group. JAMA. 1995;274:570–574Jackson JL, Browning R.
Impact of national low back pain guidelines on clinical practice.
South Med J. 2005;98:139–143Feuerstein M, Hartzell M, Rogers HL, Marcus SC.
Evidence-based practice for acute low back pain in primary care: Patient outcomes and cost of care.
Pain. 2006;124(1–2):140–149Fritz JM, Cleland JA, Brennan GP.
Does adherence to the guideline recommendation for active treatments improve the quality of care for patients with acute low back pain delivered by physical therapists?
Med Care. 2007;45:973–980Finestone AS, Raveh A, Mirovsky Y, Lahad A, Milgrom C.
Orthopaedists' and family practitioners' knowledge of simple low back pain management.
Spine (Phila Pa 1976). 2009;34:1600–1603Williams CM, Maher CG, Hancock MJ et al.
Low Back Pain and Best Practice Care: A Survey of General Practice Physicians
Archives of Internal Medicine 2010 (Feb 8); 170 (3): 271–277Weiner SS, Weiser SR, Carragee EJ, Nordin M.
Managing nonspecific low back pain: do nonclinical patient characteristics matter?
Spine (Phila Pa 1976). 2011;36:1987–1994Pablos-Mendez A, Shademani R.
Knowledge translation in global health.
J Contin Educ Health Prof. 2006;26:81–86Scott NA, Moga C, Harstall C.
Managing low back pain in the primary care setting: The know-do gap.
Pain Res Manag. 2010;15:392–400Hornbrook MC, Hurtado A, Johnson RE.
Health care episodes: Definition, measurement, and use.
Med Care Rev. 1985;42:163–218Liliedahl RL, Finch MD, Axene DV, Goertz CM.
Cost of Care for Common Back Pain Conditions Initiated With Chiropractic
Doctor vs Medical Doctor/Doctor of Osteopathy as First Physician:
Experience of One Tennessee-Based General Health Insurer
J Manipulative Physiol Ther 2010 (Nov); 33 (9): 640–643Martin BI, Deyo RA, Mirza SK, Turner JA, Comstock BA, Hollingworth W, et al.
Expenditures and Health Status Among Adults With Back and Neck Problems
JAMA 2008 (Feb 13); 299 (6): 656–664Fritz JM, Cleland JA, Childs JD.
Subgrouping patients with low back pain: evolution of a classification approach to physical therapy.
J Orthop Sports Phys Ther. 2007;37(6):290–302Waddell G.
Subgroups within “nonspecific” low back pain.
J Rheumatol. 2005;32:395–396Overview of the STarT Back approach
https://www.keele.ac.uk/sbst/Sowden G, Hill JC, Konstantinou K, et al.
Targeted treatment in primary care for low back pain: the treatment system and clinical training programmes used in the IMPaCT Back study (ISRCTN 55174281).
Fam Pract. 2012;29:50–62
Return to COST-EFFECTIVENESS
Return to ALL ABOUT CHIROPRACTIC
Return to INITIAL PROVIDER/FIRST CONTACT
Since 8-20-2004


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |