

Early Predictors of Lumbar Spine Surgery After Occupational
Back Injury: Results From a Prospective Study
of Workers in Washington StateThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Spine (Phila Pa 1976). 2013 (May 15); 38 (11): 953–964 ~ FULL TEXT
OPEN ACCESS Benjamin J. Keeney, PhD, Deborah Fulton-Kehoe, PhD, MPH, Judith A. Turner, PhD,
Thomas M. Wickizer, PhD, Kwun Chuen Gary Chan, PhD, and Gary M. Franklin, MD, MPH
Department of Orthopaedics,
Geisel School of Medicine at Dartmouth College,
Lebanon, NH 03756, USA.
Benjamin.J.Keeney@Dartmouth.edu
FROM: Keeney Spine 2013 (May 15)STUDY DESIGN: Prospective population-based cohort study.
OBJECTIVE: To identify early predictors of lumbar spine surgery within 3 years after occupational back injury.
SUMMARY OF BACKGROUND DATA: Back injuries are the most prevalent occupational injury in the United States. Few prospective studies have examined early predictors of spine surgery after work-related back injury.
METHODS: Using Disability Risk Identification Study Cohort (D-RISC) data, we examined the early predictors of lumbar spine surgery within 3 years among Washington State workers, with new workers compensation temporary total disability claims for back injuries. Baseline measures included worker-reported measures obtained approximately 3 weeks after claim submission. We used medical bill data to determine whether participants underwent surgery, covered by the claim, within 3 years. Baseline predictors (P < 0.10) of surgery in bivariate analyses were included in a multivariate logistic regression model predicting lumbar spine surgery. The area under the receiver operating characteristic curve of the model was used to determine the model's ability to identify correctly workers who underwent surgery.
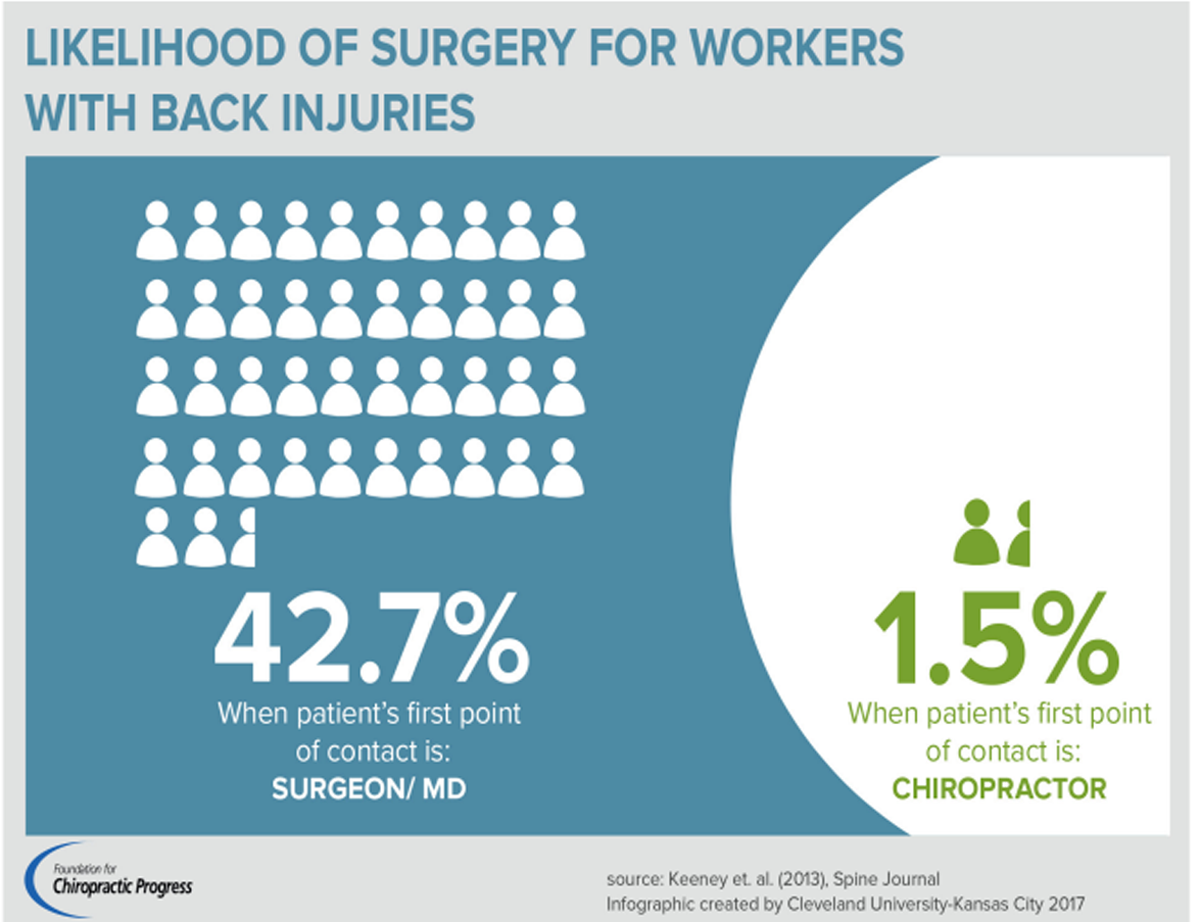
RESULTS: In the D-RISC sample of 1,885 workers, 174 (9.2%) had a lumbar spine surgery within 3 years. Baseline variables associated with surgery (P < 0.05) in the multivariate model included higher Roland-Morris Disability Questionnaire scores, greater injury severity, and surgeon as first provider seen for the injury. Reduced odds of surgery were observed for those younger than 35 years, females, Hispanics, and those whose first provider was a chiropractor. Approximately 42.7% of workers who first saw a surgeon had surgery, in contrast to only 1.5% of those who saw a chiropractor. The area under the receiver operating characteristic curve of the multivariate model was 0.93 (95% confidence interval, 0.92-0.95), indicating excellent ability to discriminate between workers who would versus would not have surgery.
CONCLUSION: Baseline variables in multiple domains predicted lumbar spine surgery. There was a very strong association between surgery and first provider seen for the injury even after adjustment for other important variables.
Keywords: Lumbar spine surgery, back injury, worker’s compensation, predictors, prospective study
From the FULL TEXT Article:
Introduction
Back pain is the most costly and prevalent occupational health condition among the U.S. working population. [1, 2] Costs relating to occupational back pain increased over 65% from 1996 through 2002, after adjustment for medical and general inflation. [3] Spine surgeries, including those after occupational back injury, represent a significant proportion of these costs and have faced increasing scrutiny regarding effectiveness and efficacy. [4, 5] Spine surgeries are associated with little evidence for improved population outcomes, [4] yet rates have increased dramatically since the 1990s. [6–9] Reducing unnecessary spine surgeries is important for improving patient safety and outcomes and reducing surgery complications and health care costs. [10, 11] Although previous studies have investigated predictors of outcomes following lumbar spine surgery, [12–16] little research has focused on identifying early (after injury) factors associated with receipt of surgery. [17, 18] Knowledge of early predictors of lumbar spine surgery following occupational back injury may help identify workers likely to undergo surgery, which in turn has potential to improve patient outcomes by targeting evidence-based care to such workers. Furthermore, such information is essential for comparative effectiveness studies so that factors associated with receipt of surgery can be assessed and included in adjustment or matching techniques to increase comparability of treatment groups.
We used data from the Washington State Worker’s Compensation Disability Risk Identification Study Cohort (D-RISC), a sample of workers with early wage replacement for temporary total disability due to a back injury, to examine the incidence of lumbar fusion and decompression spine surgeries by 3 years after claim submission, identify early predictors of surgery, develop a multivariate predictive model of surgery, and evaluate the model’s ability to predict surgery. We used previous occupational injury, back injury, chronic back pain-related disability, and lumbar spine surgery literature to identify potential early predictors available in the D-RISC baseline data, which include measures in seven domains (sociodemographic, employment-related, pain and function, clinical status, health care, health behavior, and psychological). [19–22]
We hypothesized that the following baseline variables would be associated with subsequent lumbar spine surgery:older age, [8, 9]
higher pain ratings, [16, 19, 23, 24]
prescription of opioid medication within 6 weeks from the first medical visit for the injury, [17, 25]
worker perception that the job is “hectic”, [19]
no employer offer of job accommodation after the injury, [19]
worse psychological factors, [15, 16, 21, 22]
worse injury severity, [4–5, 17, 19] and
rural residence. [8, 26]We also hypothesized that Hispanic, [9, 16, 27, 28] non-white, [8, 9, 16, 28] and female [8, 9, 28] workers would have reduced odds of surgery. Finally, we explored whether other variables predicted subsequent surgery.
Materials and Methods
Setting and Participants
The D-RISC study has been described previously. [19–22, 25, 29] In brief, workers with back injuries were identified prospectively through weekly claims review from the Washington State Department of Labor and Industries (DLI) State Fund, which covers approximately two-thirds of the state’s non-federal workforce. Workers who received some wage-replacement compensation for temporary total disability (four days off work) due to the injury were potentially eligible for the study.
In the D-RISC study, 4,354 potential participants were identified from the DLI claims database between June 2002 and April 2004. As previously reported, [19] 1,178 (27.1%) could not be contacted successfully soon after the injury, 909 (20.9%) declined enrollment into the study, and 120 (2.8%) were ineligible. The remaining 2,147 (49.3%) enrolled in D-RISC and completed a telephone interview, which was conducted a median of 18 days after claim receipt. Study participants were excluded from the D-RISC analysis sample if they were not eligible for compensation in the claim’s first year (n=240), were hospitalized for the initial injury (n=16), were missing data on age (n=3), or did not have a back injury according to medical record review (n=3). Thus, 1,885 (43.3%) were included in the D-RISC analysis sample. As previously reported, [19] this sample, as compared to workers who received wage-replacement compensation for a back injury but were not in D-RISC, was slightly older [mean age (SD) = 39.4 (11.2) vs. 38.2 (11.1) years, P = 0.001]; contained more women (32% vs. 26%, P <0.001); and had more workers receiving wage-replacement compensation 1 year after claim submission (13.8% vs. 11.3%, P =0.02).
Baseline variables

Table 1

Appendix 1

Appendix 2 The D-RISC baseline data came from three sources: administrative claims and medical bill data, medical record review, and worker self-report in telephone interviews. [19–22, 25, 29] A measure of injury severity was developed for D-RISC and trained occupational health nurses reviewed medical records of visits for the injury and rated injury severity. [22] See Table 1 and Appendix 1 for additional information about the baseline variables. 52 of 111 available D-RISC variables were examined bivariately.
Outcome measures
To determine whether a worker had lumbar spine surgery covered by DLI within 3 years, we used the DLI computerized medical bill database, which includes dates of service and Current Procedural Terminology (CPT) codes for all medical bills paid by DLI in the claim. We identified all lumbar spine surgery bills using the CPT codes shown in Appendix 2. Our CPT codes vary slightly from a previous code list [30] for lumbar spine surgery; there were no differences in counts or types of surgeries when we used that list. The date of surgery was defined as the first date of service for an included CPT code. We identified operations within 3 years (1,095 days) from the date DLI received the claim for the back injury. This period was the longest amount of time surgical data were available for all 1,885 D-RISC participants. We categorized the surgeries into fusion, decompression, or both operations for descriptive purposes, but combined them for analytical purposes.
Statistical Analyses
Initially, we conducted bivariate logistic regression analyses to examine associations between baseline variables of interest and lumbar spine surgery, adjusted for worker age and gender. We then constructed a multivariate model for predicting surgery that included baseline variables bivariately associated (P < 0.10) with lumbar spine surgery. This criterion of P < 0.10 was used because a standard 0.05 P-value level in a bivariate analysis may exclude variables that may be significant in a multivariate model. [31] Analyses were conducted using Stata versions IC10 and MP12. [32] To evaluate the ability of the multivariate model to distinguish between workers who did versus did not undergo surgery by 3 years, we determined the area under the receiver operating characteristic curve (AUC) and used 10-fold cross validation to estimate the AUC in different sub-samples of the D-RISC data. [33] An AUC from 0.70 to 0.80 is considered acceptable and 0.80 to 0.90 is considered excellent. [19, 31]
Results
Sample characteristics
Study participants (N=1,885) were mostly white non-Hispanic (71%; Hispanic 15% and Other 14%) and male (68%). By 3 years after claim receipt, 174 (9.2%) of the workers underwent one or more lumbar spine operations covered by DLI under the same claim as the index back injury. Among the 174 workers with an operation, 137 (78.7%) had decompression only as the first operation in the claim, 6 (3.4%) had fusion only, and 31 (17.8%) had both procedures on the same day.
Bivariate Analyses
Table 1 shows the baseline variables that had bivariate associations with surgery with P < 0.10. Variables that were not significant in bivariate analyses are listed in Appendix 1. All seven domains contained variables associated with lumbar spine surgery. All variables from the pain and function, health care, and psychological domains were associated with lumbar spine surgery in bivariate analyses. In the sociodemographic domain, suburban residence was associated with higher odds of surgery; younger age, female gender, Hispanic ethnicity, and non-white race were associated with reduced odds. Perception of job as fast-paced, working at current job for less than 6 months, not having returned to original work duties, and not receiving a job accommodation offer from the employer were associated with greater odds of surgery. In the clinical status domain, injury severity, pain radiating below the knee, missing at least 1 month of work due to a previous occupational injury (any type), and receipt of an opioid prescription for the injury were associated with surgery. Using tobacco daily (health behavior domain) was also associated with surgery.
Multivariate Model

Table 2 The multivariate model (Table 2) included variables that were associated with surgery in bivariate analyses. Due to concerns about collinearity, we examined correlations among the variables in the pain and function and psychological domains; as a result, we did not include variables for pain interference with daily activities, [49] pain interference with work, [49] SF-36 v2 Physical Function, [35] and SF-36 v2 Role Physical [35] in the multivariate model. We did include number of pain sites, pain intensity, Roland-Morris Disability Questionnaire (RMDQ), [34] and all of the variables in the psychological domain. Finally, we did not include self-report of radiating pain below the knee due to its similarity to radiculopathy in the injury severity measure. [19]
Due to missing data on some variables, the multivariate model included 1,857 (98.5%) workers. These workers, as compared to the 28 who were in the D-RISC sample but not in the multivariate model, were less likely to have some college education (52% vs. 61%, P=0.01) No other differences, including undergoing surgery, were identified.
Six variables from four domains contributed independently (P < 0.05) to the prediction of lumbar spine surgery in the multivariate model. Workers with high baseline RMDQ scores had six times the odds of surgery compared with those with low scores. Those with greater injury severity and those whose first provider seen for the injury was a surgeon also had significantly higher odds of surgery, after adjusting for all other variables.
The surgery provider category includedorthopedic surgeons (n=104 workers seen),
neurosurgeons (34), and
general surgeons (33).Factors associated with significantly reduced odds of surgery included age younger than 35 years, female gender, Hispanic ethnicity, and chiropractor as first provider seen for the injury. No measures in the employment-related, health behavior, or psychological domains were significant.
The AUC value was 0.93 (95% CI 0.92–0.95), indicating a very high ability for the model to distinguish between participants who did and did not undergo lumbar spine surgery. [31] The cross-validation AUC was also 0.93 (95% CI 0.91–0.95). In additional analyses, inclusion of only the RMDQ score, injury severity, and first provider seen for the injury resulted in an AUC value of 0.89 (95% CI 0.87–0.91) and a cross-validation AUC of 0.89 (95% CI 0.86–0.91).
Discussion
In this sample, 9.2% of workers receiving temporary total disability compensation soon after an occupational back injury went on to have lumbar spine surgery in the next three years. This rate is similar to rates of lumbar spine surgery following occupational back injury reported in other studies (9.8% [17] and 10.8% [27]). Measures in four domains predicted surgery: sociodemographic, pain and function, clinical status, and health care.
In an adjusted multivariate model, workers with baseline RMDQ scores of 17 or higher on the 0 – 24 scale had 6 times the odds (adjusted OR=6.12, 95% CI=1.84–20.42) of surgery, as compared with those with scores of 0–8. The RMDQ has also been shown to be predictive of chronic work disability (in a previous study involving the D-RISC sample), [19] longer duration of sick leave, [36] chronic pain, [24] and other measures of function. [37] In a previous D-RISC study of predictors of chronic work disability after back injury, baseline measures in the psychological domain were highly significant in bivariate analyses, but remained significant in a multivariate model only when the RMDQ was excluded from the model. [19] Previous studies noted that participants with lumbar spinal stenosis and discogenic back pain who did versus did not have surgery did not differ prior to surgery on measures of mental health and pain catastrophizing. [18, 38] In the current study, several psychological variables were significant in bivariate analyses, but none were significant in the multivariate model, with or without inclusion of RMDQ scores. There is evidence that psychological measures predict patient pain and function outcomes after spine surgery [39, 40] and research is needed to identify which combination of disease status, psychosocial, and other measures might best guide treatment decision-making for patients with back pain.
The D-RISC injury severity rating also predicted surgery in the multivariate model. This is consistent with previous findings that radiculopathy influences back pain outcomes, including surgeries. [16, 17, 24, 37] Surgeries may be appropriate treatment for radiculopathy. [41] Odds of surgery were highest for workers with reflex, sensory, or motor abnormalities (19 of 58, or 32.8%, received surgery). Odds were also high for workers with symptomatic radiculopathy without such abnormalities (85 of 344, or 24.7%, received surgery). In future studies investigating lumbar spine surgery, it may be informative, if the number of cases is sufficient, to separate these categories.
In Washington State worker’s compensation, injured workers may choose their medical provider. Even after controlling for injury severity and other measures, workers with an initial visit for the injury to a surgeon had almost nine times the odds of receiving lumbar spine surgery compared to those seeing primary care providers, whereas workers whose first visit was to a chiropractor had significantly lower odds of surgery (adjusted OR 0.22, 95% CI=0.10–0.50). Approximately 43% of workers who saw a surgeon had surgery within 3 years, in contrast to only 1.5% of those who saw a chiropractor. It is possible that these findings indicate that “who you see is what you get.” [42] Previous studies have noted similar findings using provider surveys of hypothetical patients. [42, 43] Persons with occupational back injuries who first saw a chiropractor had lower odds of chronic work disability and early receipt of magnetic resonance imaging (MRIs) in previous reports of data from the D-RISC sample, [19, 29] and higher rates of satisfaction with back care. [44] However, patients who see chiropractors may differ from patients who choose other provider types. [19, 45] It may be of interest to worker’s compensation programs to evaluate a gatekeeper approach to help ensure the need for lumbar spine surgery.
As hypothesized, Hispanic participants had lower odds of surgery. Prior research has also observed lower rates of spine surgery among Hispanics. [8, 9, 27, 28, 46] In an earlier study, Spanish-speaking workers had significantly fewer lumbar spine surgeries within two years of work injury compared to non-Hispanic whites (7.4% vs. 11.0%). [27]These lower odds may reflect cultural barriers and less willingness to undergo surgeries; [9, 47] lack of familiarity or understanding of surgery; [9, 48] fewer physician referrals to surgery; [28] and discouragement, lack of information, or bias from employers. [4]
Receipt of a prescription for an opioid medication within 6 weeks of claim receipt was not significant in the multivariate model. A previous study linked early opioid use to receiving lumbar spine surgery for a work-related injury, although the study inclusion criteria and methods differed from those of D-RISC. [17] When we matched our inclusion criteria and methods to that study, an opioid prescription was still not significant. We speculate that the difference may be that in the previous study, a measure of worker-related function was not included, whereas in our study the RMDQ was a highly significant predictor of surgery and opioid prescription was no longer significant after adjusting for RMDQ socres. [17]
The multivariate model had excellent ability to distinguish between workers who did or did not have surgery. A model that included only the RMDQ, injury severity, and first provider seen for the injury also had a very high ability to identify workers who did or did not undergo surgery. These three variables may be of use in future research to predict lumbar spine surgery after occupational back injury; they are relatively simple to obtain, use, and interpret.
Our study has some limitations. We had no ability to capture information on surgery covered outside DLI, although it is reasonable to assume that surgeries for the index back injury would be covered by DLI. Although the D-RISC sample consisted of workers with back injuries, some of the CPT codes are not restricted to lumbar-specific spine surgeries. The extent to which our findings may generalize to other settings is unknown. Nonetheless, the study has notable strengths, including complete data for the entire sample on surgery covered by worker’s compensation and a large prospective sample of workers who provided detailed information shortly after injury on several factors, as well as data from other sources.
Variables from several domains predicted lumbar spine surgery after occupational back injury. Surgeries were predicted by factors beyond aspects of the injury, such as age, gender, ethnicity, and first provider seen for the injury. Knowledge of surgery predictors may inform interventions or studies on care management of workers with occupational back injuries, including comparative effectiveness studies of surgery for back pain.
Key Points
174 (9.2%) of 1,885 workers had one or more lumbar spine surgeries within 3 years of filing a worker’s compensation claim for temporary total disability from an occupational back injury. 137 had a decompression procedure, 6 had a fusion without decompression, and 31 had both as the first surgery in the claim.
Significant worker baseline variables in a multivariate model predicting one or more lumbar spine surgeries within 3 years of claim submission included higher Roland-Morris Disability Questionnaire scores, greater injury severity, and first seeing a surgeon for the injury. Participants younger than 35 years, females, Hispanics, and participants whose first visit for the injury was to a chiropractor had lower odds of surgery.
The multivariate model had excellent ability to distinguish between those who did and did not undergo lumbar spine surgery (area under the receiver operating characteristic curve = 0.93).
Acknowledgments
Federal (CDCP/NIOSH) funds were received in support of this work via grant R01-OH04069. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Footnotes
The manuscript submitted does not contain information about medical devices or drugs.
References:
Courtney TK, Webster JS.
Disabling occupational morbidity in the United States.
J Occup Environ Med. 1999;41:60–9Guo HR, Tanaka S, Halperin WE, et al.
Back pain prevalence in US industry and estimates of lost workdays.
Am J Public Health. 1999;89:1029–35Shuford H, Restrepo T, Beaven N, Leigh JP.
Trends in components of medical spending within workers compensation: Results from 37 states combined.
J Occup Environ Med. 2009;51:232–8Deyo RA, Mirza SK, Turner JA, Martin BI.
Overtreating Chronic Back Pain: Time to Back Off?
J Am Board Fam Med. 2009 (Jan); 22 (1): 62–68Chou R, Baisden J, Carragee EJ, Resnick DK, Shaffer WO, Loeser JD.
Surgery for low back pain: A review of the evidence for an American Pain Society Clinical Practice Guideline.
Spine. 2009;34 (10):1094–9Cherkin DC, Deyo RA, Loeser JD, Bush T, Waddell G.
An international comparison of back surgery rates.
Spine. 1994;19:1201–6Deyo RA, Mirza SK.
Trends and variations in the use of spine surgery.
Clin Orthop Relat Res. 2006;443:139–46Wang MC, Kreuter W, Wolfla CE, Maiman DJ, Deyo RA.
Trends and variations in cervical spine surgery in the United States: Medicare beneficiaries, 1992 – 2005.
Spine. 2009;34 (9):955–61Alosh H, Riley LH, 3rd, Skolasky RL.
Insurance status, geography, race, and ethnicity as predictors of anterior cervical spine surgery rates and in-hospital mortality: An examination of United States trends from 1992 to 2005.
Spine. 2009;34(18):1956–62Deyo RA, Mirza SK.
The case for restraint in spinal surgery: Does quality management have a role to play?
Eur Spine J. 2009;18 (Suppl 3):S331–7Weinstein JN, Lurie JD, Olson PR, Bronner KK, Fisher ES.
United States’ trends and regional variations in lumbar spine surgery.
Spine. 2006;31 (23):2707–14Anderson PA, Schwaegler PE, Cizek D, Leverson G.
Work status as a predictor of surgical outcome of discogenic back pain.
Spine. 2006;31 (21):2510–5DeBerard MS, LaCaille RA, Spielmans G, Colledge A, Parlin MA.
Outcomes and presurgery correlates of lumbar discectomy in Utah Workers’ Compensation patients.
Spine J. 2009;9 (3):193–203LaCaille RA, DeBerard MS, LaCaille LJ, Masters KS, Colledge AL.
Obesity and litigation predict workers’ compensation costs associated with interbody cage lumbar fusion.
Spine J. 2007;7 (3):266–72DeBerard MS, Masters KS, Colledge AL, Holmes EB.
Presurgical biopsychosocial variables predict medical and compensation costs of lumbar fusion in Utah workers’ compensation patients.
Spine J. 2003;3 (6):420–9Weinstein JN, Tosteson TD, Lurie JD, et al.
Surgical versus Nonsurgical Therapy for Lumbar Spinal Stenosis.
N Engl J Med. 2008;358 (8):794–810Webster BS, Verma SK, Gatchel RJ.
Relationship between early opioid prescribing for acute occupational low back pain and disability duration, medical costs, subsequent surgery and late opioid use.
Spine. 2007;32 (19):2127–32Kurd MF, Lurie JD, Zhao W, et al.
Predictors of treatment choice in lumbar spinal stenosis. A SPORT study.
Spine. 2012 Mar 15;Turner JA, Franklin G, Fulton-Kehoe D, et al.
ISSLS Prize Winner: Early Predictors of Chronic Work Disability.
Spine. 2008;33:2809–18Turner JA, Franklin G, Fulton-Kehoe D, et al.
Prediction of chronic disability in work-related musculoskeletal disorders: A prospective, population-based study.
BMC Musculoskeletal Disord. 2004;5:14Turner JA, Franklin G, Fulton-Kehoe D, et al.
Work recovery expectations and fear-avoidance predict work disability: A longitudinal, population-based study of workers’ compensation back injury claimants.
Spine. 2006;31:682–9Stover BD, Turner JA, Franklin G, et al.
Factors associated with early opioid prescription among workers with low back injuries.
J Pain. 2006;7:718–25Gureje O, Simon GE, Von Korff M.
A cross-national study of the course of persistent pain in primary care.
Pain. 2001;92:195–200Fransen M, Woodward M, Norton R, et al.
Risk factors associated with the transition from acute to chronic occupational back pain.
Spine. 2002;27:92–8Franklin GM, Stover BD, Turner JA, Fulton-Kehoe D, Wickizer TM.
Early opioid prescription and subsequent disability among workers with back injuries.
Spine. 2008;33 (2):199–204Francis ML, Scaife SL, Zahnd WE.
Rural-urban differences in surgical procedures for Medicare beneficiaries.
Arch Surg. 2011;146 (5):579–83Bonauto DK, Smith CK, Adams DA, Fan ZJ, Silverstein BA, Foley MP.
Language preference and non-traumatic low back disorders in Washington State workers’ compensation.
Am J Indust Med. 2010;53:204–15Taylor BA, Casas-Ganem J, Vaccaro AR, Hilibrand AS, Hanscom BS, Albert TJ.
Differences in the work-up and treatment of conditions associated with low back pain by patient gender and ethnic background.
Spine. 2005;30:359–64Graves JM, Fulton-Kehoe D, Martin DP, Jarvik JG, Franklin GM.
Factors associated with early MRI utilization for acute occupational low back pain: A population-based study from Washington State workers compensation.
Spine. 2011 Oct 24; e-pub ahead of printGray DT, Deyo RA, Kreuter W, et al.
Population-based trends in volumes and rates of ambulatory lumbar spine surgery.
Spine. 2006;31 (17):1957–63Hosmer DW, Lemeshow S.
Applied Logistic Regression. 2.
New York, NY: John Wiley; 2000.StataCorp.
College Station, TX: StataCorp LP; 2007.
Stata Statistical Software, Version 10.Steyerberg EW, Harrell FE, Jr, Borsboom GJJM, et al.
Internal validation of predictive models: Efficiency of some procedures for logistic regression analysis.
J Clin Epidemiol. 2001;54:774–81Roland M, Morris R.
A study of the natural history of back pain. Part 1: Development of a reliable and sensitive measure of disability in low back pain.
Spine. 1983;8:141–4Ware JE, Kosinski M, Dewey JE.
How to Score Version Two of the SF-36 Health Survey.
Lincoln, RI: Quality Metric; 2000.Steenstra IA, Verbeek JH, Heymans MW, et al.
Prognostic factors for duration of sick leave in patients sick listed with acute low back pain: A systematic review of the literature.
Occup Environ Med. 2005;62:851–60Chapman JR, Norvell DC, Hermsmeyer JT, et al.
Evaluating common outcomes for measuring treatment success for chronic low back pain.
Spine. 2011;36 (21 Suppl):S54–68Mirza SK, Deyo RA, Heagerty PJ, Turner JA, Martin BI, Comstock BA.
One-year outcomes of surgical versus non-surgical treatments for discogenic back pain: A community-based comparative effectiveness study.
Manuscript under reviewDaubs MD, Norvell DC, McGuire R, et al.
Fusion versus nonoperative care for chronic low back pain: Do psychological factors affect outcomes?
Spine. 2011;36 (21 Suppl):S96–109Celestin J, Edwards RR, Jamison RN.
Pretreatment psychosocial variables as predictors of outcomes following lumbar surgery and spinal cord stimulation: A systematic review and literature synthesis.
Pain Med. 2009;10 (4):639–53Voorhies RM, Jiang X, Thoams N.
Predicting outcome in the surgical treatment of lumbar radiculopathy using the Pain Drawing Score, McGill Short Form Pain Questionnaire, and risk factors including psychosocial issues and axial joint pain.
Spine J. 2007;7 (5):516–24Cherkin DC, Deyo RA, Wheeler K, Ciol MA.
Physician variation in diagnostic testing: Who you see is what you get.
Arthritis Rheum. 1994;37 (1):15–22Cherkin DC, Deyo RA, Wheeler K, Ciol MA.
Physician views about treating low back pain: The results of a national survey.
Spine. 1995;20 (1):1–9Butler RJ, Johnson WG.
Satisfaction with low back pain care.
Spine J. 2008;8 (3):510–21Sharma R, Haas M, Stano M.
Patient Attitudes, Insurance, and Other Determinants of
Self-referral to Medical and Chiropractic Physicians
Am J Public Health 2003 (Dec); 93 (12): 2111–2117Dembe A.
Social inequalities in occupational health and health care for work-related injuries and illnesses.
Int J Law Psychiatry. 1999;22:567–79McCann J, Artinian V, Duhaime L, et al.
Evaluation of the causes for racial disparity in surgical treatment of early stage lung cancer.
Chest. 2005;128:3440–6Peterson ED, Shaw LK, DeLong ER, et al.
Racial variation in the use of coronary-revascularization procedures. Are the differences real? Do they matter?
N Engl J Med. 1997;336:480–6Von Korff M, Ormel J, Keefe FJ, et al.
Grading the severity of chronic pain.
Pain. 1992;50:133–49Sullivan MJL, Bishop SR, Pivik J.
The pain catastrophizing scale: Development and validation.
Psychol Assess. 1995;7:524–32.Hazard RG, Haugh LD, Reid S, et al.
Early prediction of chronic disability after occupational low back injury.
Spine. 1996;21:945–51Waddell G, Newton M, Henderson I, et al.
A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability.
Pain. 1993;52:157–68Bush K, Kivlahan DR, McDonell MB, et al.
The AUDIT Alcohol Consumption Questions (AUDIT-C): An effective brief screening test for problem drinking.
Arch Intern Med. 1998;158:1789–95
Return to LOW BACK PAIN
Return to COST-EFFECTIVENESS
Return to INITIAL PROVIDER/FIRST CONTACT
Since 3–06–2017


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |