|
Chiropractors as the Spinal Health Care Experts
A Chiro.Org article collection
Enjoy these learned articles about chiropractors as first-contact Spinal Health Care Experts.
|

|
The Chiropractic And Spinal Allignment
and Cervical Curve Page
A Chiro.Org article collection
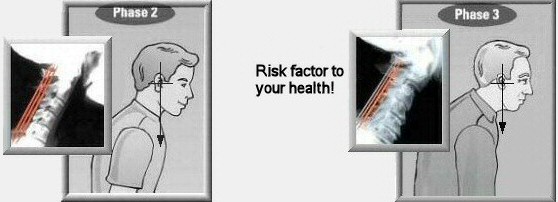
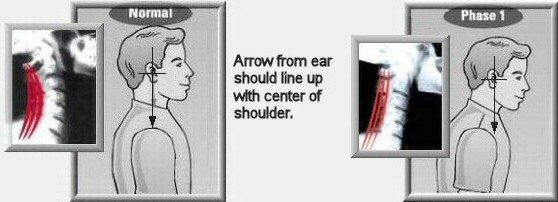
This page reviews how loss of function in the spine, and the loss of structural integrity (hypolordosis) can lead to degenerative changes and the neurological abnormalities associated with the
Vertebral Subluxation Complex.
|

|
Posture and Your Health
Our thanks to TonalBalance.Com for access to this interesting (and perhaps controversial) Adobe Acrobat document!
|

|
Two Methods of Forward Head Posture Assessment:
Radiography vs. Posture and Their Clinical Comparison
J Clinical Medicine 2024 (Apr 8); 13 (7): 2149 ~ FULL TEXT
While the CVA and radiographic C2–C7 SVA are weakly correlated in an individual, they seem to represent different aspects of sagittal cervical balance. The CVA cannot replace radiographically measured cervical lordosis. We recommend that more emphasis be given to radiographic measures of sagittal cervical alignment than the CVA when considering patient interventions.
|

|
Relationships Between Forward Head Posture and
Lumbopelvic Sagittal Alignment in Older Adults
with Chronic Low Back Pain
J Bodywork & Movement Therapies 2021 (Oct); 28: 150-156 ~ FULL TEXT
This study has provided objective evidence that dysfunction
such as faulty posture and not just lumbosacral pathoanatomy relates to low back pain. Significant associations have been established among pain intensity, FHP and lumbopelvic sagittal
alignment parameters in patients with CMLBP. Back pain may be
increased in patients with FHP and in patients with increased LL or SS and/or decreased PT.
|

|
Demonstration of Autonomic Nervous Function and Cervical
Sensorimotor Control After Cervical Lordosis Rehabilitation:
A Randomized Controlled Trial
J Athl Train 2021 (Apr 1); 56 (4): 427–436
Neck pain is among the most common musculoskeletal disorders requiring intervention, with an annual prevalence ranging from 30% to 50%. [1] Chronic nonspecific neck pain (CNSNP) contributes a substantial proportion of the rising health care costs and workplace absenteeism for musculoskeletal disorders. [1] Although the prevalence of neck pain among athletes is similar to that in the general population, sport-specific activities may put athletes at a higher risk of neck pain in some situations. [2] Regardless of the origin of their symptoms, athletes with neck pain may have deficits in muscle recruitment, strength and endurance, repositioning acuity, postural stability, and oculomotor control. [2].
|

|
Influence of Forward Head Posture on Cervicocephalic
Kinesthesia and Electromyographic Activity of Neck
Musculature in Asymptomatic Individuals
J Chiropractic Medicine 2020 (Dec); 19 (4): 230–240 ~ FULL TEXT
The findings of the present study suggest that cervicocephalic kinesthesia and activation patterns of neck muscles are significantly altered in individuals with FHP. Head repositioning accuracy, which measures cervicocephalic kinesthesia, is significantly reduced for all directions in individuals with FHP, and EMG activity of neck muscles — that is, the UT and SCM — is significantly elevated at rest and during activity. Also, cervicocephalic kinesthesia is significantly associated with the severity of FHP. These observations indicate that HRA and muscular activity are areas which should be focused on for individuals with FHP for better prognosis.
|

|
Plausible Impact of Forward Head Posture
on Upper Cervical Spine Stability
J Family Med Prim Care 2020 (May 31); 9 (5): 2517–2520 ~ FULL TEXT
The cervical spine is responsible for allowing mobility and stability to the head and neck. Any deviation to the center of gravity of the head results in an increase in cantilever loads, which can be particularly damaging to the upper cervical joints. Excessive neck bending also exaggerates stretching through the cervical spine and all of the spinal structures below. It has been reported that forward head posture (FHP) can cause a multitude of disorders including cervical radiculopathy, cervicogenic headaches and cervicogenic dizziness. Most of these conditions manifest with clusters of painful symptoms and spine dysfunctions. The purpose of this case study is to describe the radiographic imaging considerations and to illustrate the potential impacts in symptomatic adults with FHP. We randomly selected radiographs of three individuals with FHP who had undergone cervical adjustment for cervical pain. The occipito-axial (C0-C2) and atlanto-axial (C1-C2) joints were assessed via the C0-2 distance from the C2 base to the McGregor line (Redlund-Johnell criterion) and the Ranawat C1-2 index, in addition to subjective radiographic parameters. By comparing the radiographs of before-and-after intervention of each patient, a regressive joint spacing was observed from both indices. Such a long-lasting stretching concordant with FHP was assumed to be hazardous to joint stability. A definite conclusion, however, cannot be drawn due to the small sample size and a lack of convincing measurements.
|

|
Association Between Forward Head, Rounded Shoulders,
and Increased Thoracic Kyphosis:
A Review of the Literature
J Chiropractic Medicine 2017 (Sep); 16 (3): 220–229 ~ FULL TEXT
According to Kendall et al, [6] there should be vertical alignment between the midline of the shoulder and the mastoid process. If the acromion processes are more anteriorly positioned compared with the mastoid processes, a condition known as forward shoulder posture (FSP) or rounded shoulders or protracted shoulders [11, 15] occurs (Fig 3); this condition is characterized by protracted, internally rotated, anteriorly tilted, elevated, and abducted scapula along with winging of scapula. [15, 18, 19] This poor alignment of the shoulders leads to greater torque production by gravitational forces, which is being offset by greater internal forces generated by muscles and other soft tissues around the shoulder.
|

|
Cervical Spine Muscle-Tendon Unit Length Differences Between
Neutral and Forward Head Postures: Biomechanical Study
Using Human Cadaveric Specimens
Phys Ther. 2017 (Apr 21) [Epub ahead of print] ~ FULL TEXT
Forward Head Posture (FHP) was associated with flexion of the mid-lower cervical spine and extension of the upper cervical (sub-occipital) spine. Muscles that insert on the cervical spine and function as flexors (termed "cervical flexors") as well as muscles that insert on the cranium and function as extensors ("occipital extensors") shortened in FHP when compared to neutral posture. In contrast, muscles that insert on the cervical spine and function as extensors ("cervical extensors") as well as muscles that insert on the cranium and function as flexors ("occipital flexors") lengthened. The greatest shortening was seen in the Rectus Capitis Posterior Major and Minor muscles crossing the Occiput-C2 segments, which extended to maintain horizontal gaze in FHP. The greatest lengthening was seen in posterior muscles crossing the C4-C6 segments, which exhibited the most flexion.
|

|
The Effect of Adding Forward Head Posture Corrective Exercises
in the Management of Lumbosacral Radiculopathy:
A Randomized Controlled Study
J Manipulative Physiol Ther. 2015 (Mar); 38 (3): 167–178 ~ FULL TEXT
The addition of forward head posture correction to a functional restoration program seemed to positively affect disability, 3-dimensional spinal posture parameters, back and leg pain, and S1 nerve root function of patients with chronic discogenic lumbosacral radiculopathy.
|

|
Is There a Difference in Head Posture and Cervical Spine Movement
in Children With and Without Pediatric Headache?
European Journal of Pediatrics 2013 (Oct); 172 (10): 1349–1356 ~ FULL TEXT
Cervical range of motion (ROM) in each cardinal plane was significantly less in the children with purported cervicogenic headache (CGH) compared to those without headache (Table 1). ROM values recorded in the asymptomatic group are comparable with a previous report for children. [3] While no previous studies have reported ROM values for children with CGH, these results are consistent with reports in adult populations. [23, 51, 52] Interestingly, ROM does not appear to be restricted in all directions in adults with headache [23, 51, 52], but the explanation for this is not clear. This study finding of reduced ROM in children with purported CGH supports the current criteria for CGH diagnosis. [20, 44]
|

|
Effects of Thoracic Kyphosis and Forward Head Posture
on Cervical Range of Motion in Older Adults
Manual Therapy 2013 (Feb); 18 (1): 65—71 ~ FULL TEXT
Greater thoracic kyphosis was significantly associated with lesser CVA (Spearman ρ = -0.48) whereas greater CVA was significantly associated with greater cervical flexion (Spearman ρ = 0.30) and general rotation ROM (ρ = 0.33), but not with upper cervical rotation ROM (ρ = 0.15). Bootstrap mediational analyses, adjusted for age, gender, weight and NDI, revealed significant indirect effects of thoracic kyphosis on cervical flexion and general rotation ROM through a FHP. Our results show that FHP mediated the relationship between thoracic kyphosis and cervical ROM, specifically general cervical rotation and flexion.
|

|
The Role of Forward Head Correction in Management of
Adolescent Idiopathic Scoliotic Patients:
A Randomized Controlled Trial
Clin Rehabil. 2012 (Dec); 26 (12): 1123–1132 ~ FULL TEXT
A forward head corrective exercise programme combined with conventional rehabilitation improved three-dimensional scoliotic posture and functional status in patients with adolescent idiopathic scoliosis.
|

|
Effect of Backpack Load Carriage on Cervical Posture
in Primary Schoolchildren
Work. 2012 (Jan 1); 41 (1): 99–108
Subjects demonstrated immediate and statistically significant changes in craniovertebral angle (CVA), indicating increased forward head positions upon donning the backpacks containing 15% and 20% body weight. Following the walking of 6 minutes, the CVA demonstrated further statistically significant changes for all backpack loads indicating increased forward head postures. For the 15 & 20% of body weight conditions, more than 50% of the subjects reported discomfort after walking, with the neck as the primary location of reported pain.
|

|
The Efficacy of Forward Head Correction on Nerve Root Function and
Pain in Cervical Spondylotic Radiculopathy: A Randomized Trial
Clin Rehabil. 2012 (Apr); 26 (4): 351–361 ~ FULL TEXT
Forward head posture correction using a posture corrective exercise programme in addition to ultrasound and infrared radiation decreased pain and craniovertebral angle and increased the peak-to-peak amplitude of dermatomal somatosensory evoked potentials for C6 and C7 in cases of lower cervical spondylotic radiculopathy.
|

|
Musculoskeletal Dysfunction and Pain in Adults with Asthma
J Asthma. 2011 (Feb); 48 (1): 105–110
This cross-sectional and controlled study enrolled 30 patients with mild (n = 17) and severe (n = 13) persistent asthma. Fifteen non-asthmatic volunteers were also assessed. Postural alignment and muscle shortening were evaluated by head and shoulder positions, chest wall mobility, and posterior (trunk and lower limb) muscle flexibility. In comparison with non-asthmatic subjects, patients with mild or severe persistent asthma held their head and shoulders more forward and had lower chest wall expansion, decreased shoulder internal rotation, and decreased thoracic spine flexibility. Chronic lower thoracic, cervical, and shoulder pain was significantly increased in patients with mild or severe asthma compared with non-asthmatic subjects.
|

|
Influence of Forward Head Posture on Scapular Upward Rotators
During Isometric Shoulder Flexion
J Bodyw Mov Ther. 2010 (Oct); 14 (4): 367–374
Significantly increased EMG activity in the upper trapezius and lower trapezius and significantly decreased EMG activity in the serratus anterior were found during loaded isometric shoulder flexion with FHP. Thus, FHP may contribute to work-related neck and shoulder pain during loaded shoulder flexion while sitting. These results suggest that maintaining NHP is advantageous in reducing sustained upper and lower trapezius activity and enhancing serratus anterior activity as compared with FHP during loaded shoulder flexion.
|

|
Head and Shoulder Alignment Among Patients with
Unilateral Vestibular Hypofunction
Rev Bras Fisioter. 2010 (Aug); 14 (4): 330–336 ~ FULL TEXT
This was a cross-sectional study. Thirty individuals with unilateral vestibular hypofunction (UVH) and 30 with normal vestibular function and without complaints of dizziness underwent CB in the anterior, right and left and posterior views, in an upright standing position. Alcimage™ 2.0 was used to evaluate three angles in order to verify the anterior deviation and inclination of the head, and the alignment of the shoulders. The patients with UVH had greater forward (55.44 ± 16.33) and lateral (2.03 ± 1.37) head deviation angles than did the normal individuals (34.34 ± 4.60 and 1.34 ± 1.05 respectively), with a statistically significant difference (p<0.001).
|

|
Managing Forward Head Posture in the Elderly
The American Chiropractor 2010 (Jul); 32 (7) ~ FULL TEXT
I recently got some great questions from a doctor in south Florida who frequently encounters aging patients with large forward head translations, yet have pronounced, sometimes even hyperlordotic, cervical curves. We've all observed this posture, common among elderly patients, but many doctors aren't aware it needs to be managed differently than the typical case of FHP associated with cervical hypolordosis.
|

|
Recurrent Neck Pain and Headaches in Preadolescents Associated
with Mechanical Dysfunction of the Cervical Spine:
A Cross-Sectional Observational Study With 131 Students
J Manipulative Physiol Ther 2009 (Oct); 32 (8): 625–634 ~ FULL TEXT
Forty percent of the children (n = 52) reported neck pain and/or recurrent headache. Neck pain and/or headache were not associated with forward head posture, impaired functioning in cervical paraspinal muscles, and joint dysfunction in the upper and middle cervical spine in these subjects. However, joint dysfunction in the lower cervical spine was significantly associated with neck pain and/or headache in these preadolescents. Most of the students had nonsymptomatic biomechanical dysfunction of the upper cervical spine. There was a wide variation between parental report and the child's self-report of trauma history and neck pain and/or headache prevalence.
|

|
Increased Forward Head Posture and Restricted Cervical
Range of Motion in Patients with Carpal Tunnel Syndrome
Journal of Orthopaedic & Sports Physical Therapy 2009 (Sep); 39 (9): 658–664 ~ FULL TEXT
Patients with mild/moderate CTS exhibited a greater FHP and less cervical range of motion, as compared to healthy controls. Additionally, a greater FHP was associated with a reduction in cervical range of motion. However, a cause-and-effect relationship cannot be inferred from this study.
|

|
Respiratory Dysfunction in Chronic Neck Pain Patients.
A Pilot Study
Cephalalgia 2009 (Jul); 29 (7): 701–710
According to the results, chronic neck patients presented with a statistically significant decreased maximal voluntary ventilation (P = 0.042) and respiratory muscle strength (Pimax and Pemax), (P = 0.001 and P = 0.002, respectively). Furthermore, the current study demonstrated a strong association between an increased forward head posture and decreased respiratory muscle strength in neck patients. The connection of neck pain and respiratory function could be an important consideration in relation to patient assessment, rehabilitation and consumption of pharmacological agents.
|

|
The Relationship Between Head Posture and Severity and
Disability of Patients With Neck Pain
Manual Therapy 2008 (May); 13 (2): 148–154 ~ FULL TEXT
The CV angle in subjects with neck pain is significantly smaller than that in normal subjects. There is moderate negative correlation between CV angle and neck disability. Patients with small CV angle have a greater forward head posture, and the greater the forward head posture, the greater the disability.
|

|
Myofascial Trigger Points, Neck Mobility, and Forward Head Posture
in Episodic Tension-Type Headache
Headache 2007 (May); 47 (5): 662–672 ~ FULL TEXT
Active TrPs in the upper trapezius, sternocleidomastoid, and temporalis muscles were more common in ETTH (Episodic Tension-Type Headache) subjects than in healthy controls, although TrP activity was not related to any clinical variable concerning the intensity and the temporal profile of headache. ETTH patients showed greater FHP and lesser neck mobility than healthy controls, although both disorders were not correlated with headache parameters.
|

|
Hyperkyphotic Posture and Risk of Future Osteoporotic Fractures:
The Rancho Bernardo Study
J Bone Miner Res 2006 (Mar); 21 (3): 419–423 ~ FULL TEXT
In logistic regression analyses, older women with hyperkyphotic posture had a 1.7-fold increased risk of having a future fracture independent of age, prior fracture, and spine or hip BMD (bone mineral density). There was a significant trend of increasing fracture risk with increasing kyphosis of the spine. Whereas hyperkyphosis may often result from vertebral fractures, our study findings suggest that hyperkyphotic posture itself may be an important risk factor for future fractures, independent of low BMD or fracture history.
|

|
Trigger Points in the Suboccipital Muscles and
Forward Head Posture in Tension-Type Headache
Headache: The Journal of Head and Face Pain 2006 (Mar); 46 (3): 454–460
Twenty chronic tension-type headache (CTTH) subjects and 20 matched controls without headache participated. Trigger points (TrPs) were identified by eliciting referred pain with palpation, and increased referred pain with muscle contraction. Side-view pictures of each subject were taken in sitting and standing positions, in order to assess forward head posture (FHP) by measuring the craniovertebral angle. Suboccipital active TrPs and FHP were associated with CTTH. CCTH subjects with active TrPs reported a greater headache intensity and frequency than those with latent TrPs. The degree of FHP correlated positively with headache duration, headache frequency, and the presence of suboccipital active TrPs.
|

|
Reflex Control of the Spine and Posture: A Review
of the Literature From a Chiropractic Perspective
Chiropractic & Osteopathy 2005 (Aug 9); 13: 16 ~ FULL TEXT
Visual and vestibular input, as well as joint and soft tissue mechanoreceptors, are major players in the regulation of static upright posture. Each of these input sources detects and responds to specific types of postural stimulus and perturbations, and each region has specific pathways by which it communicates with other postural reflexes, as well as higher central nervous system structures. This review of the postural reflex structures and mechanisms adds to the growing body of posture rehabilitation literature relating specifically to chiropractic treatment.
|

|
Hyperkyphotic Posture and Poor Physical Functional Ability
in Older Community-dwelling Men and Women:
The Rancho Bernardo Study
J Gerontol A Biol Sci Med Sci 2005 (May); 60 (5): 633–637 ~ FULL TEXT
Physical functional decline is often the determining factor that leads to loss of independence in older persons. Identifying risk factors for physical disability may lead to interventions that may prevent or delay the onset of functional decline. Our study objective was to determine the association between hyperkyphotic posture (Forward Head Posture) and physical functional limitations. In multiply adjusted comparisons, there was a graded stepwise increase in difficulty in bending, walking and climbing, measured grip strength, and ability to rise from a chair (with increased kyphosis of the spine).
|

|
Hyperkyphotic Posture Predicts Mortality in Older
Community-dwelling Men and Women:
A Prospective Study
J Am Geriatr Soc 2004 (Oct); 52 (10): 1662–1667
To determine the association between hyperkyphotic posture and rate of mortality, the authors tracked 1,353 participants from the Rancho Bernardo Study who had measurements of kyphotic posture made at an osteoporosis visit. Participants were followed for an average of 4.2 years, with mortality and cause of death confirmed using review of death certificates. This study found that persons with hyperkyphotic posture had a 1.44 greater rate of mortality.
|

|
Upper Crossed Syndrome and Its Relationship
to Cervicogenic Headache
J Manipulative Physiol Ther 2004 (Jul); 27 (6): 414–420 ~ FULL TEXT
The principles of upper crossed syndrome and the use of exercise, chiropractic care, and myofascial release in the treatment of cervicogenic headache are discussed. A review of the literature indicates that analyzing muscle imbalance as well as vertebral subluxation may increase the effectiveness of chiropractic treatment for cervicogenic headache.
There are more articles on this topic at our
Rehabilitation Diplomate Information Page.
|

|
Vertical Posture and Head Stability in Patients
With Chronic Neck Pain
J Rehabil Med. 2003 (Sep); 35 (5): 229–235 ~ FULL TEXT
Our experiments have confirmed earlier reports on increased postural sway and decreased ability to maintain more demanding standing posture in patients with chronic neck pain, and, in addition, showed major differences in vertical postural and head stability to perturbations. The differences between the patients with whiplash associated disorders (WAD) and those suffering from work-related pain (WRP) suggest that deficits in proprioception and motor control, rather than the chronic pain itself, may be the main factors defining the clinical picture in different chronic neck pain conditions. Consequently, qualitative and quantitative measures of postural performance and head stabilization could be used to increase the precision and efficiency of diagnosis and rehabilitation of chronic neck pain of different aetiology.
|

|
A Study on the Prevalence of and Risk Factors for Neck Pain
Among University Academic Staff in Hong Kong
J Occup Rehabil 2002 (Jun); 12 (2): 77–91
Among those with neck pain during computer processing, 60.3% had a forward head posture. However, a low correlation between psychosocial factors and neck pain was demonstrated (r = 0.343). Academic staff in tertiary institutions could be considered as a high-risk group of job-related neck pain.
|

|
Forward Head Posture is the Cause of
'Straight Spine Syndrome' in Many Professionals
Indian J Occupat and Environmental Med 2000 (Jul); 4 (3): 122–124
Our results show that forward head posture is the commonest defect found in variety of professionals. This leads to SSS, an early functional stage, and can lead to serious compression of cervical nerve roots. Education programmes on right posture, ergonomics, regular corrective exercises may prevent SSS.
|

|
Forward Head Posture
Dynamic Chiropractic (April 3, 2000)
Forward head posture is a clinical entity that has been identified by multiple authors as a significant factor in a variety of musculoskeletal pain syndromes. [2–7] Although some reports are essentially anecdotal, [2–4] several reports use sophisticated statistical analyses and healthy ontrols versus painful subjects to establish forward head posture as a real clinical entity with significant musculoskeletal consequences. [5–7]
|

|
The Associations Between Adolescent Head-on-neck Posture,
Backpack Weight, and Anthropometric Features
Spine 1999 (Nov 1); 24 (21): 2262–2267
A significant change in craniovertebral angle was found at every year level, when comparing standing posture with no backpack with posture when carrying a backpack. The change was greatest for the youngest students. There are more articles like this in the Backpack Page
|

|
Forward Head / Forward Shoulders
Dynamic Chiropractic (August 23, 1999)
Probably one of the most common postural distortions we see is the forward head, forward shoulders posture. This distortion often appears in teenagers and progresses to old age. Porterfield and DeRosa1 have provided some important information regarding this problem. They state1 that while lengthening or weakness of the scapular retractors is often blamed, a major cause is weakness and lengthening of the abdominal muscles, allowing the chest to descend and shifting the weight of the upper trunk anteriorly. This causes the chest to descend with the scapula shifting forward around the rib cage, pressing the clavicle to the first rib. In this position, the humerus internally rotates and the head and neck are brought forward.
|

|
Neck Posture a Key to Pain Relief
Seattle Fibromyalgia International Team Conference (2–13–1997)
Head and neck posture may be a major factor in the pain experienced by many fibromyalgia (FMS) and chronic fatigue and immune dysfunction syndrome(CFIDS) patients. Case studies presented last week showed that successful treatment of neck and jaw pain made significant improvements in FMS and CFIDS patients. Herbert P. Gordon, D.D.S., Ph.D., P.S., attributed a major portion of head, neck, jaw, and shoulder pain to the posture of the sufferer. Dr. Gordon, an assistant professor of oral medicine at the University of Washington, Seattle, presented his theories and techniques for pain relief to the conference, which was attended by 200 FMS and CFIDS survivors.
|

|
The Relationship Between Forward Head Posture
and Temporomandibular Disorders
J Orofac Pain 1995 (Spring); 9 (2): 161–167
This study investigated the relationship between forward head posture and temporomandibular disorder symptoms. Thirty-three temporomandibular disorder patients with predominant complaints of masticatory muscle pain were compared with an age- and gender-matched control group. In other words, when evaluating the ear position with respect to the seventh cervical vertebra, the head was positioned more forward in the group with temporomandibular disorders than in the control group (P < .05).
|

|
Cervical Headache: An Investigation of Natural Head Posture
and Upper Cervical Flexor Muscle Performance
Cephalalgia 1993 (Aug); 13 (4): 272–284
In this study, 60 female subjects, aged between 25 and 40 years, were divided into two equal groups on the basis of absence or presence of headache. A passive accessory intervertebral mobility (PAIVM) examination was performed to confirm an upper cervical articular cause of the subjects' headache and a questionnaire was used to establish a profile of the headache population. Measurements of cranio-cervical posture and isometric strength and endurance of the upper cervical flexor muscles were compared between the two groups of subjects. The headache group was found to be significantly different from the non-headache group in respect to forward head posture (FHP) (t = -5.98, p < 0.00005), less isometric strength (t = 3.43, p < 0.001) and less endurance (t = 8.71, p < 0.0005) of the upper cervical flexors.
|

|
Incidence of Common Postural Abnormalities in the Cervical,
Shoulder, and Thoracic Regions and their Association with
Pain in Two Age Groups of Healthy Subjects
Phys Ther 1992 (Jun); 72 (6): 425–431
Subjects with kyphosis and rounded shoulders had an increased incidence of interscapular pain, and those with a forward-head posture had an increased incidence of cervical, interscapular, and headache pain.
|