Welcome to the Cost-Effectiveness of Chiropractic section @ Chiro.Org
This section details the long history of the cost-effectiveness of chiropractic care.




The Cost-Effectiveness of Chiropractic This section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org
If there are terms in these articles you don't understand, you can get a definition from the Merriam Webster Medical Dictionary. If you want information about a specific disease, you can access the Merck Manual. You can also search Pub Med for more abstracts on this, or any other health topic.
| Jump to: | Newest Studies | Older Studies | Reference Materials |




|
|
Conditions That Respond | Alternative Medicine Approaches to Disease |




Newest Cost-Effectiveness Studies




The Cost-Effectiveness Triumvirate 
Variations in Patterns of Utilization and Charges
for the Care of Headache in North Carolina,
2000-2009: A Statewide Claims' Data Analysis
J Manipulative Physiol Ther. 2016 (May); 39 (4): 229-239 ~ FULL TEXT
Overall utilization and average charges for the treatment of headache increased considerably from 2000 to 2005 and then decreased in each subsequent year. Policy changes that took place between 2005 and 2007 may have affected utilization rates of certain providers and their associated charges. MD care accounted for the majority of total allowed charges throughout the decade. In general, patterns of care involving multiple providers and referral care incurred the largest charges, whereas patterns of care involving single or nonreferral providers incurred the least charges. MD-only, DC-only, and MD-DC care were the least expensive patterns of headache care; however, risk-adjusted charges (available 2006-2009) were significantly lower for DC-only care compared with MD-only care.

Variations in Patterns of Utilization and Charges
for the Care of Neck Pain in North Carolina,
2000 to 2009: A Statewide Claims'
Data Analysis
J Manipulative Physiol Ther. 2016 (May); 39 (4): 240-251 ~ FULL TEXT
Increases in utilization and charges were the highest among patterns involving MDs, PTs and referral providers. These findings are consistent with previous studies showing that medical specialty, diagnostic imaging, and invasive procedures (eg, spine injections, surgery) [17, 19, 20, 21] are significant drivers of increasing spine care costs. When costs are viewed vertically as if in “silos” (eg, DC-only costs, MD-only costs), increasing utilization of one particular provider is seen as a net cost increase. However, when costs are viewed across the silos, as this study has done, an increase in utilization of one provider group can result in a net cost decrease given its effect on the patient population. This is an opportunity to view costs laterally versus a confined, vertical analysis.

Variations in Patterns of Utilization and Charges
for the Care of Low Back Pain in North Carolina,
2000 to 2009: A Statewide Claims'
Data Analysis
J Manipulative Physiol Ther. 2016 (May); 39 (4): 252-262 ~ FULL TEXT
A major strength of the study was the large amount of low back pain claims made available to us for analysis. The data were from 3,159,362 claims generated by approximately 66,0000 persons over the 2000-2009 decade in North Carolina, in several different pathways of healthcare services. This study and the series of papers it has generated on the treatment of low back pain, neck pain [25] and headache, [26] provides unique economic examination for healthcare policy makers and legislators. When costs are viewed vertically as if in “silos” (eg, DC-only costs, MD-only costs), increasing utilization of one particular provider is seen as a net cost increase. However, when costs are viewed across the silos, as this study has done, an increase in utilization of one provider group can result in a net cost decrease given its effect on the patient population. This is an opportunity to view costs laterally versus a confined, vertical analysis.
The Cost-Effectiveness of Chiropractic
From: Testimony to the Department of Veterans Affairs' Chiropractic Advisory Committee
George B. McClelland, D.C., Foundation for Chiropractic Education and Research ~ March 25, 2003
In the treatment of musculoskeletal disorders, despite the fact that most studies have not properly factored in such patient characteristics as severity and chronicity and lack the complete assessment of all direct costs and most indirect costs, the bulk of articles reviewed demonstrate lower costs for chiropractic. [9] This pattern is consistently observed from the perspectives of workers' compensation studies, [10], [11], [12], [13], [14], [15] databases from insurers, [16], [17], [18], or the analysis of a health economist employed by the provincial government of Ontario. [19], [20].
Other studies have suggested the opposite [that chiropractic services are more expensive than medical], [5], [21], [22] but these contain significant flaws which have been refuted. [23]
The cost advantages for chiropractic for matched conditions appear to be so dramatic that Pran Manga, the aforementioned Canadian health economist, has concluded that doubling the utilization of chiropractic services from 10% to 20% may realize savings as much as $770 million in direct costs and $3.8 billion in indirect costs. [20] When iatrogenic effects [yet to be discussed] are factored in, the cost advantages of spinal manipulation as a treatment alternative become even more prominent. In one study, for instance, it was shown that for managing disc herniations, the cost of treatment failures following a medical course of treatment [chymopapain injections] averaged 300 British pounds per patient, while there were no such costs following spinal manipulation. [24], Imagine how failed back surgery might compare. Finally, in no cost studies to date have legal burdens been calculated, which one would expect should be heavily advantageous for chiropractic health management.
From: Testimony to the Department of Veterans Affairs' Chiropractic Advisory Committee

A Comparison of Chiropractic, Medical and
Osteopathic Care for Work-related Sprains and Strains
J Manipulative Physiol Ther 1989 (Oct); 12 (5): 335-344
For those who received care from DCs (n = 266), the mean number of compensated days lost from work was at least 2.3 days less than for those who were treated by MDs (n = 494; p less than 0.025) and at least 3.8 days less than for those who were treated by DOs (n = 102; p less than 0.025). Consequently, much less money in employment compensation was paid, on the average, to those who saw DCs.

An Analysis of Florida Workers' Compensation
Medical Claims for Back-related Injuries
Journal of the American Chiro Association 1988; 25 (7): 50-59
This study of 10,652 Florida Workers' Compensation cases was conducted by Steve Wolk, Ph.D., and reported by the Foundation for Chiropractic Education and Research. It was concluded that claimant with a back-related injury, when initially treated by a chiropractor versus a medical doctor, is less likely to become temporarily disabled, or if disabled, remains disabled for a shorter period of time; and claimants treated by medical doctors were hospitalized at a much higher rate than claimants treated by chiropractors.” The analysis focused on the cost of treatment, frequency of compensable injuries (an injury which disables an individual for more than seven days, resulting in wage compensation benefits), and frequency of hospitalization for workers' compensation claim patient (end of reference).
Editorial:
End Medical Mis-Management of Musculoskeletal Complaints
Q. Are medical doctors well-trained to diagnose or treat musculoskeletal complaints?
A. Read the unsettling answer in this series of articles
Educational Deficiencies in Musculoskeletal Medicine
Journal of Bone and Joint Surgery 2002 (Apr); 84-A (4): 604-608
According to the standard suggested by the program directors of internal medicine residency departments, a large majority of the examinees once again failed to demonstrate basic competency in musculoskeletal medicine on the examination. It is therefore reasonable to conclude that medical school preparation in musculoskeletal medicine is inadequate. NOTE: This is a follow-up article to the study cited below, which demonstrated that medical students were inadequately trained to diagnose and treat musculoskeletal complaints.
Ask yourself: What would the headlines scream if, after 4 years, chiropractors had failed to improve their skills in musculoskeletal assessment and management? Why is medicine is shown more slack?
The Adequacy of Medical School Education
in Musculoskeletal Medicine
Journal of Bone and Joint Surgery 1998 (Oct); 80-A (10): 1421-1427
This is the original article, which found that 82 per cent of medical school graduates failed a valid musculoskeletal competency examination. They concluded that "we therefore believe that medical school preparation in musculoskeletal medicine is inadequate" and that medical students were inadequately trained to diagnose and treat musculoskeletal complaints.
Educating Medical Students About Musculoskeletal
Problems: Are Community Needs Reflected in
the Curricula of Canadian Medical Schools?
Journal of Bone and Joint Surgery 2001 (Sept); 83-A (9): 1317-1320
Musculoskeletal problems are a common reason why patients present for medical treatment. The purpose of the present study was to review the curricula of Canadian medical schools to determine whether they prepare their students for the demands of practice with respect to musculoskeletal problems. The curriculum analysis revealed that, on the average, medical schools in Canada devoted 2.26% (range, 0.61% to 4.81%) of their curriculum time to musculoskeletal education. Our literature review and survey of local family physicians revealed that between 13.7% and 27.8% of North American patients presenting to a primary care physician have a chief symptom that is directly related to the musculoskeletal system. (So they conclude:) There is a marked discrepancy between the musculoskeletal knowledge and skill requirements of a primary care physician and the time devoted to musculoskeletal education in Canadian medical schools.A Comparison of Chiropractic Student Knowledge
Versus Medical Residents
Proceedings of the World Federation of Chiropractic Congress 2001 Pgs. 255
A previously published knowledge questionnaire designed by chief orthopedic residents was given to a Chiropractic student group for comparison to the results of the medical resident group. Based on the marking scale determined by the chief residents, the Chiropractic group (n = 51) showed statistically significant higher average grade than the orthopedic residents. Expressed in other terms, 70% of chiropractic students passed the knowledge questionnaire, compared to an 80% failure rate for the orthopedic residents.Musculoskeletal Knowledge: How Do You Stack Up?
Physician and Sportsmedicine 2002; 30 (8) August
One of every 4 or 5 primary care visits is for a musculoskeletal problem. Yet undergraduate and graduate training for this burden of illness continues to constitute typically less than 5% of the medical curriculum. This is an area of clear concern, but also one in which sports medicine practitioners can assume leadership.Musculoskeletal Curricula in Medical Education
Physician and Sportsmedicine 2004 (Nov); 32 (11)
It's 8:00 pm on a Monday night. Just as you're getting ready to put your 5-year-old son to bed, he falls from a chair, landing on his wrist. It quickly swells, requiring a visit to a nearby urgent care clinic. At the clinic, a pleasant young resident takes a history, performs a physical exam, and orders an x-ray to evaluate the injury. You are told that nothing is broken, and a wrist splint is placed. The following day, however, you receive a phone call from the clinic informing you that upon further review of the radiographs, a fracture was detected, and your son will need a cast for definitive treatment. This scenario, while fictitious, is not unusual. According to some studies, up to 10% of wrist fractures are missed at the initial evaluation.1 While pediatric fractures are often difficult to detect, this example highlights a problem that continues to plague medical education: inadequate instruction in musculoskeletal medicine in both medical school and residency training.Adequacy of Education in Musculoskeletal Medicine
J Bone Joint Surg Am 2005 (Feb); 87 (2): 310-314
In this study, 334 medical students, residents and staff physicians, specializing in various fields of medicine, were asked to take a basic cognitive examination consisting of 25 short-answer questions - the same type of test administered in the original JBJS 1998 study. The average score among medical doctors, students and residents who took the exam in 2005 was 2.7 points lower than those who took the exam in 1998. Just over half of the staff physicians (52%) scored a passing grade or higher on the 2005 exam. Only 21% of the residents registered a passing grade, and only 5% of the medical students passed the exam. Overall, Seventy-nine percent of the participants failed the basic musculoskeletal cognitive examination.More Evidence of Educational Inadequacies
in Musculoskeletal Medicine
Clin Orthop Relat Res 2005 (Aug); (437): 251-259
A modified version of an exam used to assess the competency of incoming interns at the University of Pennsylvania was used to assess the competency of medical students during various stages of their training at the University of Washington. Despite generally improved levels of competency with each year at medical school, less than 50% of fourth-year students showed competency. These results suggested that the curricular approach toward teaching musculoskeletal medicine at this medical school was insufficient and that competency increased when learning was reinforced during the clinical years.




Additional (Older) Cost-Effectiveness Studies




Thanks to the NBCE for access to this information!
Practice Analysis of Chiropractic 2020 PDF
Practice Analysis of Chiropractic 2015
Practice Analysis of Chiropractic 2010
Job Analysis of Chiropractic 2005
Job Analysis of Chiropractic 2000
Job Analysis of Chiropractic 1993
NBCE's Practice Analysis Archive (See 2 other files)
The National Board of Chiropractic Examiners published reports based on a four-year study of chiropractic. These reports focused on three surveys including full-time, licensed U.S., Canadian and registered Australian and New Zealand chiropractic practitioners. The surveys and their resulting reports are titled Job Analysis of Chiropractic.
Following publication of the Job Analysis of Chiropractic, the NBCE began to receive requests for permission to reproduce certain portions of the reports. In response to those requests, the NBCE has condensed relevant portions and reprinted them in this brochure.
In recent years, numerous independent researchers and various government agencies have conducted studies which focus on the efficacy, appropriateness and cost-effectiveness of chiropractic treatment. Several of these important studies are listed below.
U.S. GOVERNMENT AGENCY REPORT
A 1994 study published by the U.S. Agency for Health Care Policy and Research (AHCPR) and the U.S. Department of Health and Human Services endorses spinal manipulation for acute low back pain in adults in its Clinical Practice Guideline # 14. An independent multidisciplinary panel of private-sector clinicians and other experts convened and developed specific statements on appropriate health care of acute low back problems in adults. One statement cited, relief of discomfort (low back pain) can be accomplished most safely with spinal manipulation, and/or nonprescription medication.
Acute Low Back Problems in Adults ~ AHCPR Clinical Practice Guidelines, No. 14
Clinical Practice Guideline 14
AHCPR Publication No. 95-0642:
December 1994
THE MANGA REPORT
A major study to assess the most appropriate use of available health care resources was reported in 1993. This was an outcomes study funded by the Ontario Ministry of Health and conducted in hopes of sharing information about ways to reduce the incidence of work-related injuries and to address cost-effective ways to rehabilitate disabled and injured workers. The study was conducted by three health economists led by University of Ottawa Professor Pran Manga, Ph.D. The report of the study is commonly called the Manga Report. The Manga Report overwhelmingly supported the efficacy, safety, scientific validity, and cost-effectiveness of chiropractic for low-back pain. Additionally, it found that higher patient satisfaction levels were associated with chiropractic care than with medical treatment alternatives.
"Evidence from Canada and other countries suggests potential savings of hundreds of millions annually,"
the Manga Report states.
"The literature clearly and consistently shows that the major savings from chiropractic management come from fewer and lower costs of auxiliary services, fewer hospitalizations, and a highly significant reduction in chronic problems, as well as in levels and duration of disability."
Ontario Ministry of Health
RAND STUDY ON LOW-BACK PAIN
A four-phase study conducted in the early 1990s by RAND, one of America's most prestigious centers for research in public policy, science and technology, explored many indications of low-back pain. In the RAND studies, an expert panel of researchers, including medical doctors and doctors of chiropractic, found that:
chiropractors deliver a substantial amount of health care to the U.S. population.
spinal manipulation is of benefit to some patients with acute low-back pain.
The RAND reports marked the first time that representatives of the medical community went on record stating that spinal manipulation is an appropriate treatment for certain low-back pain conditions.
The Appropriateness of Spinal Manipulation for Low-Back Pain.
Project Overview and Literature Review
RAND Corp., Santa Monica, CA; 1991
THE NEW ZEALAND COMMISSION REPORT
A particularly significant study of chiropractic was conducted between 1978-1980 by the New Zealand Commission of Inquiry. In its 377-page report to the House of Representatives, the Commission called its study "probably the most comprehensive and detailed independent examination of chiropractic ever undertaken in any country." The Commission entered the inquiry with "the general impression ... shared by many in the community: that chiropractic was an unscientific cult, not to be compared with orthodox medical or paramedical services."
By the end of the inquiry, the commission reported itself "irresistibly and with complete unanimity drawn to the conclusion that modern chiropractic is a soundly-based and valuable branch of health care in a specialized area...: Conclusions of the Commission's report, based on investigations in New Zealand, the U.S., Canada, the United Kingdom, and Australia, stated:
Spinal manual therapy in the hands of a registered chiropractor is safe.
Spinal manual therapy can be effective in relieving musculo-skeletal symptoms such as back pain, and other symptoms known to respond to such therapy, such as migraine.
Chiropractors are the only health practitioners who are necessarily equipped by their education and training to carry out spinal manual therapy.
In the public interest and in the interests of patients, there must be no impediment to full professional cooperation between chiropractors and medical practitioners.
STATE OF TEXAS WORKERS' COMPENSATION STUDY OF 2003
In 2002, the Texas Chiropractic Association (TCA) commissioned an independent study to determine the use and effectiveness of chiropractic with regard to workers' compensation, the results of which were published in February. According to the report, Chiropractic Treatment of Workers' Compensation Claimants in the State of Texas, chiropractic care was associated with significantly lower costs and more rapid recovery in treating workers with low-back injuries. They found: Lower back and neck injuries accounted for 38 percent of all claims costs. Chiropractors treated about 30 percent of workers with lower back injuries, but were responsible for only 17.5 percent of the medical costs and 9.1 percent of the total costs.
These findings were even more intertesting: The average claim for a worker with a low-back injury was $15,884. However, if a worker received at least 75 percent of his or her care from a chiropractor, the total cost per claimant decreased by nearly one-fourth to $12,202. If the chiropractor provided at least 90 percent of the care, the average cost declined by more than 50 percent, to $7,632.
Chiropractic Treatment of Workers' Compensation
Claimants in the State of Texas
MGT of America, Austin, Texas ~ February 2003
FLORIDA WORKERS' COMPENSATION STUDY
A 1988 study of 10,652 Florida workers' compensation cases was conducted by Steve Wolk, Ph.D. , and reported by the Foundation for Chiropractic Education and Research (FCER). It was concluded that "a claimant with a back-related injury, when initially treated by a chiropractor versus a medical doctor, is less likely to become temporarily disabled, or if disabled, remains disabled for a shorter period of time; and claimants treated by medical doctors were hospitalized at a much higher rate than claimants treated by chiropractors." Some of the study results were:
51.3 percent shorter temporary total disability duration with chiropractic care
lower treatment cost by 58.8 percent ($558 vs. $1,100 per case) in the chiropractic group, and
20.3 percent hospitalization rate in the chiropractic care group vs. 52.2 percent rate in the medical care group
An Analysis of Florida Workers' Compensation
Medical Claims for Back-related Injuries
J American Chiro Association 1988; 25 (7): 50-59
WASHINGTON HMO STUDY
In 1989, a survey administered by Daniel C. Cherkin, Ph.D., and Frederick A. MacCornack, Ph.D., concluded that patients receiving care from health maintenance organizations (HMOs) within the state of Washington were three times as likely to report satisfaction with care from chiropractors as they were with care from other physicians. The patients were also more likely to believe that their chiropractor was concerned about them.
Patient Evaluations of Low Back Pain Care
From Family Physicians and Chiropractors
Western Journal of Medicine 1989 (Mar); 150 (3): 351-355
UTAH WORKERS' COMPENSATION STUDY
A workers' compensation study conducted in Utah by Kelly B. Jarvis, D.C., Reed B. Phillips, D.C., Ph.D., and Elliot K. Morris, JD, MBA, compared the cost of chiropractic care to the costs of medical care for conditions with identical diagnostic codes. Results were reported in the August 1991 Journal of Occupational Medicine. The study indicated that costs were significantly higher for medical claims than for chiropractic claims; in addition, the number of work days lost was nearly ten times higher for those who received medical care instead of chiropractic care.
This Compensation Board study found the total treatment costs for back-related injuries cost an average of $775.30 per case when treated by a doctor of chiropractic. When injured workers received standard medical treatment as opposed to chiropractic treatment, the average cost per case was $1,665.43. They also found the mean compensation cost paid out by the Utah Worker's Compensation Board for patients treated by medical doctors was $668.39, while the mean compensation cost paid for patients treated by chiropractic doctors was only $68.38.
Cost Per Case Comparison of Back Injury Claims of
Chiropractic Versus Medical Management for
Conditions With Identical Diagnostic Codes
J Occup Med 1991 (Aug); 33 (8): 847-852
PATIENT DISABILITY COMPARISON
A 1992 article in the Journal of Family Practice reported a study by DC Cherkin, Ph.D., which compared patients of family physicians and of chiropractors. The article stated "the number of days of disability for patients seen by family physicians was significantly higher (mean 39.7) than for patients managed by chiropractors (mean 10.8)." A related editorial in the same issue referred to risks of complications from lumbar manipulation as being "very low."
Family Physicians and Chiropractors:
What's Best for the Patient?
J Family Practice 1992; 35 (5): 505-506
OREGON WORKERS' COMPENSATION STUDY
A 1991 report on a workers' compensation study conducted in Oregon by Joanne Nyiendo, Ph.D., concluded that the median time loss days (per case) for comparable injuries was 9.0 for patients receiving treatment by a doctor of chiropractic and 11.5 for treatment by a medical doctor.
Disabling Low Back Oregon Workers'
Compensation Claims Part II: Time Loss
J Manipulative Physiol Ther. 1991 (May); 14 (4): 231-239
STANO COST COMPARISON STUDY
Miron Stano, PhD, a health care economist at Oakland University, conducted a study comparing the health-care costs for chiropractic and medical patients with neuromusculoskeletal conditions. The database he used came from the records of MEDSTAT Systems, Inc., a health benefits management consulting firm which processes insurance claims for many of the country's largest corporations. This June 1993 Journal of Manipulative and Physiological Therapeutics study involved 395,641 patients, drawn from statistical information on more than two million beneficiaries. Results over a two-year period showed that patients who received chiropractic care incurred significantly lower health care costs than did patients treated solely by medical or osteopathic physicians.
DISTRIBUTION OF TOTAL COST PER CASE FOR SELECTED ICD-9 CODES (MEAN VALUES)
ICD-9 CODE DIAGNOSIS TOTAL COST
(MEDICAL)TOTAL COST
(CHIROPRACTIC)722.10 Lumbar Disc $ 8,175 $ 1,065 724.40 Neuritis/Radiculitis $ 2,154 $ 531 846.00 Sprain/Sacroiliac $ 813 $ 537 847.00 Sprain/Strain Cervical $ 968 $ 586 847.10 Sprain/Strain Thoracic $ 487 $ 474 847.20 Sprain/Strain Lumbar $ 969 $ 523 Total Cost of Selected Cases $ 13,556 $ 3,716 Average Cost Per Case $ 2,259 $ 619
Also of interest, for those patients receiving both medical and chiropractic care, the Stano/MEDSTAT results revealed:
31 percent lower hospital admissions rates;
43 percent lower inpatient payments; and
23 percent lower total health care costs.
A Comparison of Health Care Costs
for Chiropractic and Medical Patients
J Manipulative Physiol Ther 1993 (Jun); 16 (5): 291-299
SASKATCHEWAN CLINICAL RESEARCH
Following a 1993 study, researchers J. David Cassidy, D.C., Haymo Thiel, D.C., M.S., and W. Kirkaldy-Willis, M.D., of the Back Pain Clinic at the Royal University Hospital in Saskatchewan concluded that "the treatment of lumbar intervertebral disk herniation by side posture manipulation is both safe and effective."
Side Posture Manipulation for Lumbar
Intervertebral Disk Herniation
J Manipulative Physiol Ther 1993 (Feb); 16 (2): 96-103
UNIVERSITY OF SASKATCHEWAN STUDY OF 1985
In 1985 the University of Saskatchewan conducted a study of 283 patients "who had not responded to previous conservative or operative treatment" and who were initially classified as totally disabled. The study revealed that "81% ... became symptom free or achieved a state of mild intermittent pain with no work restrictions" after daily spinal manipulations were administered.
WIGHT STUDY ON RECURRING HEADACHES
A 1978 study conducted by J.S. Wight, D.C. , and reported in the ACA Journal of Chiropractic, indicated that 74.6% of patients with recurring headaches, including migraines, were either cured or experienced reduced headache symptomatology after receiving chiropractic manipulation.
1991 GALLUP POLL
A 1991 demographic poll conducted by the Gallup Organization revealed that 90% of chiropractic patients felt their treatment was effective; more than 80% were satisfied with that treatment; and nearly 73% felt most of their expectations had been met during their chiropractic visits.
1990 BRITISH MEDICAL JOURNAL REPORT
A study conducted by T.W. Meade, a medical doctor, and reported in the June 2, 1990, British Medical Journal concluded after two years of patient monitoring, "for patients with low-back pain in whom manipulation is not contraindicated, chiropractic almost certainly confers worthwhile, long-term benefit in comparison with hospital outpatient management."
More importantly, this article contradicts other articles which maintained that spinal adjusting (manipulation) was only effective for "acute" low back pain. This article found: The benefit is seen mainly in those with chronic or severe pain. It also suggested that "introducing chiropractic into NHS practice should be considered."
Low Back Pain of Mechanical Origin: Randomised
Comparison of Chiropractic and
Hospital Outpatient Treatment
British Medical Journal 1990 (Jun 2); 300 (6737): 1431-1437
VIRGINIA COMPARATIVE STUDY
A 1992 study conducted by L.G. Schifrin, Ph.D., provided an economic assessment of mandated health insurance coverage for chiropractic treatment within the Commonwealth of Virginia. This economic analysis found chiropractic care to be a lower cost option for back-related ailments. The researchers concluded that if chiropractic care was insured to the extent of other medical specialties, it would likely emerge as a first option for many patients with certain medical conditions. They also believed this could result in a decrease in the overall treatment costs for these conditions. The study reported that:
The low cost of chiropractic is due not to its low rate of use, but to its apparently offsetting impacts on costs in the face of high rates of utilization. Chiropractic is a growing component of the health care sector, and it is widely used by the population.
Formal studies of the cost, effectiveness, or both of chiropractic, usually measured against other forms of treatment, show it to compare favorably with them.
By every test of cost and effectiveness, the general weight of evidence shows chiropractic to provide important therapeutic benefits, at economical costs. Additionally, these benefits are achieved with apparently minimal, even negligible, impacts on the costs of health insurance.
The conclusion of this analysis is that chiropractic mandates help make available health care that is widely used by the American public and has proven to be cost-effective.
Mandated Health Insurance Coverage for Chiropractic Treatment:
An Economic Assessment, with Implications for the Commonwealth of Virginia
The College of William and Mary, Williamsburg, Virginia, and Medical College of Virginia, Richmond, Virginia - January 1992.
Return to the Top
1992 AMERICA HEALTH POLICY REPORT
A 1992 review of data from over 2,000,000 users of chiropractic care in the U.S., reported in the Journal of American Health Policy, stated that "chiropractic users tend to have substantially lower total health care costs," and that "chiropractic care reduces the use of both physician and hospital care."
1985 UNIVERSITY OF SASKATCHEWAN STUDY
In 1985 the University of Saskatchewan conducted a study of 283 patients "who had not responded to previous conservative or operative treatment" and who were initially classified as totally disabled. The study revealed that "81% ... became symptom free or achieved a state of mild intermittent pain with no work restrictions" after daily spinal manipulations were administered.
Further validation of chiropractic care evolved from an antitrust suit which was filed by four members of the chiropractic profession against the American Medical Association (AMA) and a number of other health care organizations in the U.S. (Wilk et al v. AMA et al, 1990). Following 11 years of litigation, a federal appellate court judge upheld a ruling by U.S. District Court Judge Susan Getzendanner that the AMA had engaged in a "lengthy, systematic, successful and unlawful boycott" designed to restrict cooperation between MDs and chiropractors in order to eliminate the profession of chiropractic as a competitor in the U.S. health care system.
Judge Getzendanner rejected the AMA's patient care defense, and cited scientific studies which implied that "chiropractic care was twice as effective as medical care in relieving many painful conditions of the neck and back as well as related musculo-skeletal problems." Since the court's findings and conclusions were released, an increasing number of medical doctors, hospitals, and health care organizations in the U.S. have begun to include the services of chiropractors.
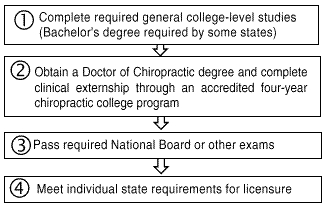
In order to become a licensed doctor of chiropractic, an individual must meet stringent testing, academic and professional requirements. Currently, an individual must complete the four major steps shown below in order to become a chiropractic practitioner:
.
CHIROPRACTIC TRAINING
Government inquiries (some of which are described in this brochure), as well as independent investigations by medical practitioners, have affirmed that today's chiropractic academic training is of equivalent standard to medical training in all pre-clinical subjects. High standards in chiropractic education are maintained by the Council on Chiropractic Education (CCE) and its Commission on Accreditation, as recognized by the U.S. Department of Education.
Some Chiropractic colleges require a Bachelor's degree before enrollment. A doctor of chiropractic's training generally requires a minimum of six years of college study (two years of which are undergraduate course work) and an internship prior to entering practice. Post-doctoral training in a variety of clinical disciplines and specialties is also available through accredited colleges and specialty councils.
CHIROPRACTIC LICENSING
Chiropractic is one of many occupations which are regulated by state licensing agencies. The requirements for chiropractic licensure vary from state to state (and country to country). Some states require a Bachelor's degree as a prerequisite for licensure. To assist the various regulatory agencies in assessing candidates for licensure, the National Board administers examinations to individuals currently in the chiropractic educational system or who have completed a chiropractic educational program. The National Board also offers an examination designed for previously licensed individuals.
A candidate for chiropractic licensure may request that transcripts of scores from National Board examinations be forwarded to licensing agencies which assess eligibility for licensure. Scores from National Board examinations are made available to licensing agencies throughout the U.S. and in some foreign countries including Canada, the United Kingdom, France and Australia.




Reference Materials





Initial Provider/First Contact and Chiropractic
A Chiro.Org article collection
Although the Cost Effectiveness page has always painted a rosey picture for patients and Insurers, recent studies have zeroed in on the extent of that savings when chiropractors are the first provider of care. As you will see, when we are the first and only provider, the savings are the greatest. In 1993 Pran Manga, Ph.D. recommended that placing DCs as the gatekeepers in Hospitals and for Work-related MSK injuries would save Ontario. Canada a fortune, and that has been bourne out in the studies that followed.

Non-pharmacologic Therapy and Chiropractic
A Chiro.Org article collection
Onc of the few silver linings in the Opioid Epidemic storm cloud was the studies looking at which patients ended up being swallowed by opioid addiction. Chiropractic is an effective approach for managing musculoskeletal pain, and that has saved many of them from starting down that dark path.

Chiropractic: A Safe and Cost Effective Approach to Health
Cleveland College of Chiropractic (2017) ~ FULL TEXT
Manipulation, which chiropractors usually refer to as an “adjustment,” continues to meet the threshold of scientific scrutiny for many neurological and musculoskeletal conditions. In addition to the adjustment, chiropractors often advise and instruct on posture, stretching, exercise, rehabilitation, nutrition, hydration, and stress management as part of their care. While often assisting in repair and recovery of patient health, a chiropractor’s focus is primarily on healthy living (now commonly referred to as wellness by the rest of the population) and optimization (helping a patient get the best outcome from their body). I have personally sought their treatment for my own musculoskeletal complaints ranging from operative fatigue, overuse, degenerative disease and to enhance my athletic performance.

The Cost-Effectiveness of Chiropractic
Chapter 2 from: Practice Analysis of Chiropractic 2015
Provided by the National Board of Chiropractic Examiners (NBCE)
From Page 23: A recent study of 12,036 records in the Medical Expenditure Panel Survey (MEPS) investigated the costs of treating patients with low back and neck pain (Martin et al., 2012). The study estimated the expenditures for care among complementary and alternative medicine (chiropractic, homeopathy, herbalism, acupuncture, and massage) users relative to non-users. This study included a chiropractic-specific analysis of expenditures for chiropractic users versus non-users, as approximately 75% of all complementary and alternative medicine services were rendered by doctors of chiropractic. Survey data were analyzed for the years 2002-2008. The analysis demonstrated that seeing a CAM/chiropractic provider did not add to overall medical spending. In fact, adjusted annual healthcare costs among chiropractic users were $424 lower for spine-related costs when compared to non-CAM users. Additionally, those who used complementary and alternative providers, including doctors of chiropractic, had significantly lower hospitalization expenditures.

Chiropractic Cost-Effectiveness
Health Insights Today (2011) ~ FULL TEXT
In the current economic and political climate, one of the most important arguments to be made for any health care method is that it is cost-effective. As a result, researchers are redoubling their efforts to identify cost-effective approaches. This includes a growing number of studies addressing the cost-effectiveness of chiropractic services. Chiropractors and chiropractic students need to understand this information and to share it with others.

Chiropractic Cost-Effectiveness Supplement
Provided by a Joint Task Force of the ACA, ICA, CAS and the ACC (2009)
The following is a collection of studies relating to the cost effectiveness and efficacy associated with chiropractic care and the procedures that doctors of chiropractic provide. The American Chiropractic Association, The International Chiropractic Association, The Congress of State Associations, and the Association of Chiropractic Colleges appreciate the opportunity to provide these materials for your review. This presentation is divided into several parts:
- Background studies, detailing that LBP is much more complex than the literature leads us to believe;
- Cost-Effectiveness Studies;
- Worker's Compensation Studies (National studies) and
- Worker's Compensation Studies (State specific studies)
- Additional Research Studies

Chiropractic Cost-Effectiveness Review (2009)
Anthony L. Rosner, Ph.D., LL.D.[Hon.], LLC ~ FULL TEXT
Enjoy this review of reduced Healthcare expenditures, Chiropractic and medical expenditures and Workers' Compensation costs when chiropractic is moved to the top slot.
Return to ChiroZINE
Return to LINKS Table of Contents
Return to SAFETY OF CHIROPRACTIC
Return to TELL ME ABOUT CHIROPRACTIC
Since 6–26–1998
Updated 10-07-2024


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |