

Three Patterns of Spinal Manipulative Therapy for Back Pain
and Their Association With Imaging Studies, Injection
Procedures, and Surgery: A Cohort Study
of Insurance ClaimsThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Manipulative Physiol Ther 2021 (Nov); 44 (9): 683689 ~ FULL TEXT
OPEN ACCESS Brian R. Anderson, DC, MPH, MS, PhD, Steve W. McClellan, MS
Palmer Center for Chiropractic Research,
Palmer College of Chiropractic,
Davenport, IA.
FROM: Houweling, JMPT 2015 Liliedahl, JMPT 2010Objective: The purpose of this study was to evaluate the relationship between procedures and care patterns in back pain episodes by analyzing health insurance claims.
Methods: We performed a retrospective cohort study of insurance claims data from a single Fortune 500 company. The 3 care patterns we analyzed were initial spinal manipulative therapy, delayed spinal manipulative therapy, and no spinal manipulative therapy. The 3 procedures analyzed were imaging studies, injection procedures, and back surgery. We considered "escalated care" to be any claims with diagnostic imaging, injection procedures, or back surgery. Modified-Poisson regression modeling was used to determine relative risk of escalated care.
Results: There were 83,025 claims that were categorized into 10 372 unique patient first episodes. Spinal manipulative therapy was present in 2,943 episodes (28%). Initial spinal manipulation was present in 2,519 episodes (24%), delayed spinal manipulation was present in 424 episodes (4%), and 7,429 (72%) had no evidence of spinal manipulative therapy. The estimated relative risk, adjusted for age, sex, and risk score, for care escalation (eg, imaging, injections, or surgery) was 0.70 (95% confidence interval 0.650.75, P < .001) for initial spinal manipulation and 1.22 (95% confidence interval 1.101.35, P < .001) for delayed spinal manipulation with no spinal manipulation used as the reference group.
Conclusion: For claims associated with initial episodes of back pain, initial spinal manipulative therapy was associated with an approximately 30% decrease in the risk of imaging studies, injection procedures, or back surgery compared with no spinal manipulative therapy. The risk of imaging studies, injection procedures, or back surgery in episodes in the delayed spinal manipulative therapy group was higher than those without spinal manipulative therapy.
Keywords: Chiropractic; Injections; Low Back Pain; Orthopedic Surgery; Radiology; Spinal Manipulation; Therapeutics.
From the FULL TEXT Article:
Introduction
Back pain has been the leading cause of disability since 1990. [1] The lifetime prevalence of this condition is estimated at 60% to 70% in industrialized countries. [2] In the United States, back pain treatment costs are estimated at $8000 per person per year, totaling approximately $87 billion per year, or 2.5% of the gross domestic product. [3]
Approximately 18% of Americans report visiting a healthcare practitioner in the previous 12 months for a back pain related complaint, with general practitioners and chiropractors accounting for the greatest number of visits. [4] The American College of Physicians treatment guidelines for the management of acute, subacute and chronic back pain advocate for nonpharmaceutical treatments first. [5] However, the use of opioid medications, injection procedures, and surgeries for back pain have increased exponentially since 2000. [69] A recent study [10] found that primary care referrals for nonpharmaceutical care were relatively common for chronic back pain, but nonexistent for acute back pain, suggesting that recommended treatments are being underutilized. It has been suggested that escalating costs may be associated with overuse of low-value care (eg, imaging, injections, and back surgery) and underuse of high-value care. [2]
Given the extreme and growing costs associated the management of back pain, treatment strategies that avoid care escalation are increasingly relevant. Using imaging as an example, it has been estimated in the United States that 60% of lumbar MRI studies and 40% of lumbar radiography studies are inappropriate, which represents nearly $1 billion that could be saved. [11] Lower rates of low back surgery and advanced imaging procedures have been associated with chiropractic users as compared with other provider types. [12]
Therefore, the primary aim of this project was to evaluate the relationship between patients receiving imaging studies, injection procedures, and back surgery (ie, care escalation) and 3 distinct care patterns in back pain episodes by analyzing health insurance claims from a large Fortune 500 company. It was hypothesized that episodes initiated with spinal manipulative therapy (SMT) as a treatment would have a lower risk of care escalation when compared with delayed SMT or no SMT.
Methodology
We conducted a retrospective study of a deidentified health insurance claims dataset spanning the years 2012 to 2018 from a single, self-insured, Fortune 500 company. The Institutional Review Board of Northern Illinois University determined this project was exempt from review according to federal guidelines.
Our cohort included only claims with complete data, age ≥18, and the presence of a specific primary diagnosis code related to back pain (Supplemental File). Our unit of analysis was an episode of back pain, defined by a 90day claim-free window after the index visit. Only claims associated with the first episode of back pain were included. Depending on duration, these episodes may include acute, subacute, or chronic classifications.
Following the inclusion of claims related to back pain, we identified SMT via the presence of current procedural terminology (CPT) codes 9894098942. The 3 treatment groups were generated as follows: Initial SMT included an episode with SMT present as the initial treatment; Delayed SMT included an episode where SMT was provided subsequent to some other care; No SMT included an episode without evidence of SMT. All SMT was provided in outpatient, community-based clinics. We then identified back pain episodes with CPT codes for imaging studies, injection procedures, and back surgery (Supplemental File).
Additional variables included age, sex, claim count, allowed cost, diagnosis category, and retrospective risk score. The risk score is derived from a proprietary tool applied to the dataset by a third-party administrator known as Symmetry Episode Risk Groups. [13] Scores (0100) in the year before (retrospective risk) the claim are calculated based on characteristics such as demographics, medical claims, and pharmacy claims. The resulting score is used to predict expected health care costs and use of health care services. [13] We used age at first claim and mean risk score over the entire episode, because risk score has the potential to change with each additional claim. Claim count included the number of dates with a claim during episode one. Allowed cost included the amount allowed by the insurer during episode one, which was log-transformed to account for skewed data. The supplemental file includes additional detail on our methodology following the Strengthening the Reporting of Observational studies in Epidemiology and Reporting of Studies Conducted using Observational Routinely collected Data (STROBE/RECORD) guidelines. [14, 15]
Data Analysis
Data were cleaned and organized via R, [16] Microsoft SQL server, and Microsoft Excel. We used SPSS (v26, IBM Corp, Armonk, NY) to conduct data analysis. Descriptive statistics were calculated for each care group based on presence or absence of care escalation, along with care group by individual procedures (ie, imaging studies, injection procedures, and back surgery). We estimated relative risk of all procedures combined (ie, care escalation), along with relative risk of each individual procedures for each care group with a modified Poisson regression model [17] fit through generalized estimating equations using an unstructured covariance matrix, adjusting for sex, age, claim count, and risk score. Allowed cost was not included in our model, as cost and presence of the 3 procedures are strongly correlated. A subgroup analysis was performed evaluating the interaction of sex with treatment group, which was an exploratory analysis, as we did not have an a priori hypothesis regarding the directionality of this interaction.
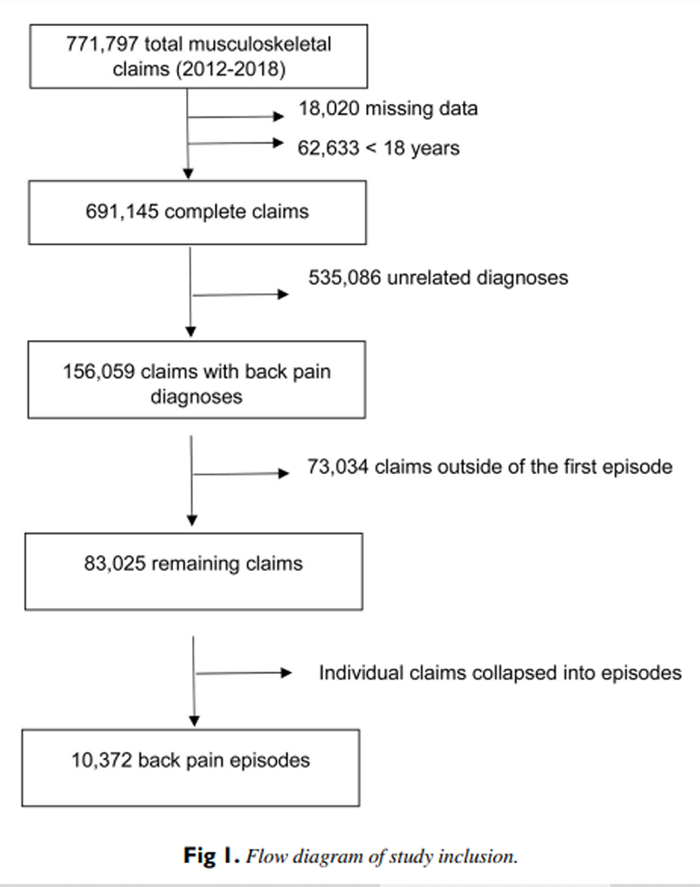
Figure 1
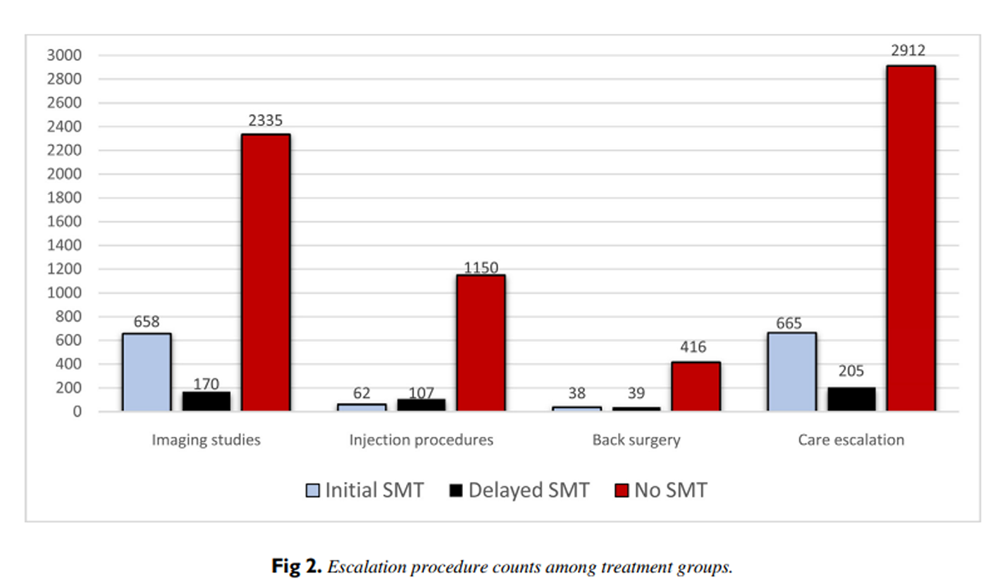
Figure 2

Table 1
page 4

Table 2

Table 3 Results
The initial dataset consisted of 771,797 claims, spanning the years 2012 to 2018. After eliminating claims with missing data, those associated with individuals <18 years of age, and anatomically unrelated diagnoses, 83,025 claims were categorized into 10,372 unique back pain initial episodes (Figure 1). SMT CPT codes were present in 2,943 episodes (28%), whereas 7,468 (72%) had no evidence of SMT codes. The overall rate of care escalation in our cohort was 36% (n = 3,782), with imaging being the most common procedure (83%) and surgery being the least common (13%) (Figure 2). Risk score was lowest among the initial SMT cohort absent care escalation and highest in the no SMT cohort with care escalation present. Allowed reimbursement was highest in the delayed SMT, care escalation present cohort. Men were more likely in the initial SMT cohort regardless of escalation status (Table 1).
Adjusted relative risk of care escalation overall, along with escalation to each procedure level, was significantly lower in the initial SMT group as compared with the delayed SMT and no SMT groups (Table 2). This relative risk (RR) ranged from 0.17 (95% confidence interval [CI] 0.130.22, P < .001) for injection procedures to 0.86 (CI 0.800.93, P < .001) for imaging studies. Conversely, adjusted RR of escalated care overall, along with escalation to each procedure level was significantly higher in the delayed SMT group as compared with initial SMT and no SMT groups. Initial SMT was associated with a 30% reduction in risk of care escalation (RR 0.70 [CI 0.650.75], P <.001), and delayed SMT was associated with a 22% increase in risk of care escalation (RR 1.22 [CI 1.101.35], P < .001).
Because sex was not a significant contributor in the model described earlier, the interaction between sex and SMT group was evaluated for its association with care escalation. The female Initial SMT and female Delayed SMT cohorts were less likely to experience care escalation, as well as individual procedures (imaging, injection, and surgery), when compared with the men in these cohorts (using male No SMT cohort as a reference; Table 3).
Discussion
Our results indicate that treatment initiated with SMT for episodes of back pain resulted in a significant decrease in the risk of having imaging studies, injection procedures, or back surgery as compared with care patterns with delayed SMT or no SMT. Conversely, the delayed SMT group was associated with a significant increased risk of imaging studies, injection procedures, or back surgery when compared with the other 2 groups. The interaction between sex and SMT group was a significant contributor to the risk of care escalation.
Although several studies have evaluated the relationship between provider type and future healthcare use for episodes of back pain, only a single study evaluated this relationship among chiropractic users. Fritz et al [12] found that initiating back pain care with a chiropractor (vs primary care) decreased the odds for future advanced imaging (odds ratio [OR] = 0.21, P = .001) and surgeon visits (OR = 0.13, P = .005), but increased care duration. Although they did not investigate the use of chiropractic services per se, Nelson et al [18] measured the effects of insurance plans including vs excluding chiropractic coverage on use of advanced imaging, surgery, and plain-film radiographs in the management of neck and low back pain. The group including (vs excluding) chiropractic benefits had a statistically significant decrease in use of surgery (23%), advanced imaging (23%), and plain film radiography (8%).
We found the risk of escalated care was highest in the delayed SMT group. As indicated by a higher median risk score, this group is more medically complex, which may lead to increased care seeking behavior. Our finding of lower risk score in the initial SMT group is consistent with other literature documenting fewer comorbid conditions, more moderate disability, and better overall self-rated physical and mental health in patients seeking chiropractic vs medical care. [1923]
The prevalence of chiropractic use in back pain populations ranges from 14% to 39%, [2427] which is consistent with the 28% prevalence reported here. Our population had a slightly higher use of injection procedures and surgery than others have reported. [24, 26] Regarding allowed log-transformed cost, a similar pattern was seen in both escalated and nonescalated episodes; initial SMT was slightly higher than no SMT with the latter showing a larger range. Other authors [28, 29] have found a reduction in cost of back pain care initiated with a chiropractor vs medical doctor.
Except for the delayed SMTinjection interaction, women with any exposure to SMT were less likely to experience imaging studies, injection procedures, or back surgery procedures when compared with men. We are likely the first to report such an association. Others have reported no significant difference in sex-specific responses to spinal manipulation for low back pain. [30, 31]
Our findings suggest that the delayed SMT group was at increased risk for imaging studies, injection procedures, or back surgery, increased claim count, and allowed reimbursement. We suggest that patients at high risk for poor prognosis should be identified as early as possible; assessment tools such as STarT Back have been successful in this regard. [32]
Limitations
Our dataset did not include a provider identifier; therefore, we cannot be certain of the type of provider associated with each service (eg, chiropractor, osteopath, and physical therapist). It has been established in a Medicare population that chiropractors administer 97% to 98% of all SMT services in the United States. [33] There is a high likelihood this finding would translate to other patient populations. Without additional clinical information, the distinction between high vs low value care cannot be determined. There are inherent limitations when analyzing administrative data, including unknown accuracy of billing codes, risk of unmeasured confounding variables, inclusion/exclusion errors, and the influence of health insurance coverage on the use of certain services. [34]
Conclusions
The hypothesis that initial SMT (vs delayed SMT or no SMT) for episodes of back pain would result in decreased risk of imaging studies, injection procedures, or back surgery was confirmed. This risk reduction remained after adjusting for age, sex, risk score, and episode count. The availability of additional clinical variables would help confirm the necessity of escalated care at the individual level.
Appendix. Supplementary materials
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): B.A., S.M.
Design (planned the methods to generate the results): B.A., S.M.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): B.A.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): S.M., B.A.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): B.A.
Literature search (performed the literature search): B.A.
Writing (responsible for writing a substantive part of the manuscript): B.A.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): B.A., S.M.
References:
US Burden of Disease Collaborators.
The state of US health, 1990-2016:
burden of diseases, injuries, and risk factors among US states.
JAMA. 2018;319:1444-1414.Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, Ferreira PH, Fritz JM.
Prevention and Treatment of Low Back Pain:
Evidence, Challenges, and Promising Directions
Lancet. 2018 (Jun 9); 391 (10137): 23682383
This is the third of 4 articles in the remarkable Lancet Series on Low Back PainMacKay C, Canizares M, Davis AM, Badley EM.
Health care utilization for musculoskeletal disorders.
Arthritis Care Res. 2010;62:161-169.Managing Neck and Back Pain in America
Gallup-Palmer College of Chiropractic Annual Report (2018)Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514530Beckworth WJ, Jiang M, Hemingway J, Hughes D, Staggs D.
Facet injection trends in the Medicare population and
the impact of bundling codes.
Spine J. 2016;16:1037-1041.Mafi JN, McCarthy EP, Davis RB, Landon BE.
Worsening Trends in the Management and Treatment of Back Pain
JAMA Internal Medicine 2013 (Sep 23); 173 (17): 15731581Stokes A, Berry KM, Hempstead K, Lundberg DJ, Neogi T.
Trends in prescription analgesic use among adults with
musculoskeletal conditions in the United States, 1999-2016.
JAMA Netw Open. 2019;2:e1917228-ee191722.Yoshihara H, Yoneoka D.
National trends in the surgical treatment for lumbar
degenerative disc disease: United States, 2000 to 2009.
Spine J Off J North Am Spine Soc. 2015;15:265-271.Roseen EJ, Conyers FG, Atlas SJ, Mehta DH.
Initial Management of Acute and Chronic Low Back Pain:
Responses from Brief Interviews of Primary Care Providers
J Altern Complement Med 2021 (Mar); 27 (S1): S106S114Flaherty S, Zepeda ED, Mortele K, Young GJ.
Magnitude and financial implications of inappropriate diagnostic
imaging for three common clinical conditions.
Int J Qual Health Care J Int Soc Qual Health Care. 2019;31:691-697.Fritz JM, Kim J, Dorius J.
Importance of the Type of Provider Seen to Begin Health Care for a New Episode
Low Back Pain: Associations with Future Utilization and Costs
J Eval Clin Pract. 2016 (Apr); 22 (2): 247252OPTUMInsight.
Symmetry Episode Risk Groups
A successful approach to cost risk assessmentThe REporting of studies Conducted using Observational
Routinely-collected health Data (RECORD) Statement.
https://journals.plos.org/plosmedicine/article?id=
10.1371/journal.pmed.1001885von Elm E, Altman DG, Egger M, et al.
The Strengthening the Reporting of Observational Studies in
Epidemiology (STROBE) statement: guidelines for
reporting observational studies.
Ann Intern Med. 2007;147:573-577.R:
A language and environment for statistical computing.
Foundation for Statistical Computing; 2017.Zou G.
A modified poisson regression approach to prospective studies with binary data.
Am J Epidemiol. 2004;159:702-706.Nelson CF, Metz RD, LaBrot T.
Effects of a Managed Chiropractic Benefit on the Use of
Specific Diagnostic and Therapeutic Procedures in the
Treatment of Low Back and Neck Pain
J Manipulative Physiol Ther 2005 (Oct); 28 (8): 564569Bath B, Lawson J, Ma D, Trask C.
Self-reported Use of Family Physician, Chiropractor and
Physiotherapy Services Among Adult Canadians with
Chronic Back Disorders: An Observational Study
BMC Health Serv Res 2018 (Dec 17); 18 (1): 970Broom AF, Kirby ER, Sibbritt DW, Adams J, Refshauge KM.
Back pain amongst mid-age Australian women: a longitudinal
analysis of provider use and self-prescribed treatments.
Complement Ther Med. 2012;20:275-282.Cote P, Cassidy JD, Carroll L.
The Treatment of Neck and Low Back Pain:
Seeks Care? Who Goes Where?
Med Care. 2001 (Sep); 39 (9): 956967de Luca KE, Parkinson L, Haldeman S, Byles JE, Blyth F.
The relationship between spinal pain and comorbidity:
a cross-sectional analysis of 579 community-dwelling,
older Australian women.
J Manipulative Physiol Ther. 2017;40 (7):459-466.Sibbritt D, Lauche R, Sundberg T, et al.
Severity of back pain may influence choice and order of practitioner
consultations across conventional, allied and complementary health care:
a cross-sectional study of 1851 mid-age Australian women.
BMC Musculoskelet Disord. 2016;17:393.Azad T, Vail D, Bentley J, et al.
Initial provider specialty is associated with long-term opiate use
in patients with newly diagnosed low back and lower extremity pain.
Spine. 2019;44(3):211-218.Weigel, P.A., Hockenberry, J., Bentler, S.E., Wolinsky, F.D., 2014.
The Comparative Effect of Episodes of Chiropractic and
Medical Treatment on the Health of Older Adults
J Manipulative Physiol Ther 2014 (Mar); 37 (3): 143154Ivanova JI, Birnbaum H, Schiller M, et al.
Real-world practice patterns, health-care utilization, and costs
in patients with low back pain: the long road to
guideline-concordant care.
Spine J. 2011;11:622-632.Kazis LE, Ameli O, Rothendler J, et al.
Observational Retrospective Study of the Association of Initial
Healthcare Provider for New-onset Low Back Pain
with Early and Long-term Opioid Use
BMJ Open. 2019 (Sep 20); 9 (9): e028633Liliedahl RL, Finch MD, Axene DV, Goertz CM.
Cost of Care for Common Back Pain Conditions Initiated with
Chiropractic Doctor vs Medical Doctor/Doctor of Osteopathy
as First Physician: Experience of One Tennessee-Based
General Health Insurer
J Manipulative Physiol Ther 2010 (Nov); 33 (9): 640643Houweling TAW, Braga AV, Hausheer T, et al.
First-Contact Care With a Medical vs Chiropractic Provider After Consultation
With a Swiss Telemedicine Provider: Comparison of Outcomes,
Patient Satisfaction, and Health Care Costs in Spinal,
Hip, and Shoulder Pain Patients
J Manipulative Physiol Ther. 2015 (Sep); 38 (7): 477483George SZ, Fritz JM, Childs JD, Brennan GP.
Sex differences in predictors of outcome in selected physical
therapy interventions for acute low back pain.
J Orthop Sports Phys Ther. 2006;36:354-363.Peterson CK, Humphreys BK, Hodler J, Pfirrmann CW.
Gender differences in pain levels before and after treatment:
a prospective outcomes study on 3,900 Swiss patients
with musculoskeletal complaints.
BMC Musculoskelet Disord. 2012;13:1-8.Stevans JM, Delitto A, Khoja SS, et al.
Risk Factors Associated With Transition From Acute to Chronic
Low Back Pain in US Patients Seeking Primary Care
JAMA Netw Open 2021 (Feb 1); 4 (2): e2037371Whedon JM, Haldeman S, Peterson C, et al.
Temporal trends and geographic variations in the supply of clinicians
who provide spinal manipulation to medicare beneficiaries:
a serial cross-sectional study.
J Manipulative Physiol Ther. 2021;44 (3):177-185. https://doi.org/10.1016/j.jmpt.2021.02.002Johnson EK, Nelson CP.
Utility and pitfalls in the use of administrative databases
for outcomes assessment.
J Urol. 2013;190:17-18.
Return to LOW BACK PAIN
Return to INITIAL PROVIDER/FIRST CONTACT
Since 4-28-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |
