

Overcoming Overuse Part 4:
Small Business SurvivalThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Orthop Sports Phys Ther 2021 (Jan); 51 (1): 1–4 ~ FULL TEXT
Adrian C Traeger, Jason Soon, Mary O'Keeffe, Simon Décary, Zoe A Michaleff, Joshua R Zadro
Institute for Musculoskeletal Health,
The University of Sydney and Sydney Local Health District,
Sydney, Australia.
The challenge of overuse raises important questions for those in the business of musculoskeletal health care. What is the right number of physical therapy visits for a given condition? Can a practice provide "less" but still be profitable? In this, the editorial on overcoming overuse of musculoskeletal health care, we consider the economic drivers of overuse in the private sector. We propose actions that could support small business leaders to overcome overuse and build profitable, high-quality services.
Keywords: medical economics; musculoskeletal; overuse; physical therapy.
From the FULL TEXT Article:
Backgroumd
Clinicians in the private sector are often remunerated according to the number of consultations they provide. It is easy to see how this fee-for-service payment model could drive overuse: it incentivizes service providers to do more, not less. This payment model may also influence the type of care provided by remunerating some providers differently according to the specific services they provide in the consultation.
In the “Overcoming Overuse” series, we have discussed how overuse can happen, [14] what clinicians can do to identify it in practice, [8] and its many and complex drivers. [10] In this editorial, we focus on economic factors that could drive overuse in the private sector. We do not attempt to provide answers for any one health system. Rather, we propose ideas for small business leaders that demand further investigation.
Supplier-Induced Demand, Unwarranted Variation, and Overuse
Supplier-induced demand [9] — a surplus in demand for a health service beyond what would be expected had the consumers of the service (patients) been fully informed — can help explain the economics of overuse.
Patients use more health services than they need because:(1) they have incomplete information about benefits and harms of care options,
(2) they have easy access to clinicians in their region, and
(3) the clinicians in that region need to maintain a target income.In this environment, suppliers of health care can “induce” demand through various means of persuasion, including during consultations or through advertising.
Measures of variation in health care are widely viewed by policy makers as hallmarks of potential waste in the system. The most well-known examples are in surgery: if you break your hip, where you live does not tend to influence the likelihood that you will have hip surgery. [2] In contrast, where a person lives might substantially influence the likelihood of having a spinal fusion operation for low back pain. A person living on Bruny Island, Australia — a regional area that, apart from its exceptional cheese, is similar to other Australian regional areas — is 7 times more likely to have spinal fusion surgery than a person living in the regional area of New South Wales. [1] Supplier-induced demand can explain some of these variations insofar as they cannot be explained by differences in the need for clinical services in different areas.
There is also evidence of geographic variation in physical therapy. A person living in the Northeast region of the United States has a greater number of physical therapy visits per episode of care compared with someone living in the West region of the United States (7.8 visits per episode in the West versus 10.8 visits per episode in the Northeast). [7] In Germany, there was substantial geographic variation in physical therapy utilization even after controlling for patient “need” (eg, the number of people with disabling osteoarthritis in a region). [11] Variation in care is not direct evidence of overuse; lower numbers in a given region could be explained by underuse of appropriate care, for example, due to lack of access.
Economic theory suggests that the number of clinicians in an area should not influence the number of services provided per person, unless people are receiving more services than they need. Ten out of 12 countries had a positive linear relationship between surgeon supply and spine surgery rates. [3] However, a more recent study in the United States found a wide geographic variation in rates of knee and shoulder arthroscopy but no relationship between orthopaedic surgeon supply and geographic variation. [6]
Funding Arrangements to Promote Quality and Support Small Businesses

Table Similar patient outcomes can be achieved with fewer consultations. [8] For a business to be profitable with fewer consultations per episode, the equation appears simple: increase the number of patients a practice services, not the number of visits per episode. The TABLE shows our suggestions for how private physical therapy businesses could foster a culture of quality over quantity. Below, we discuss actions from governments, private health insurers, and consumers that could support the less-is-more approach we advocate.
Action From Governments
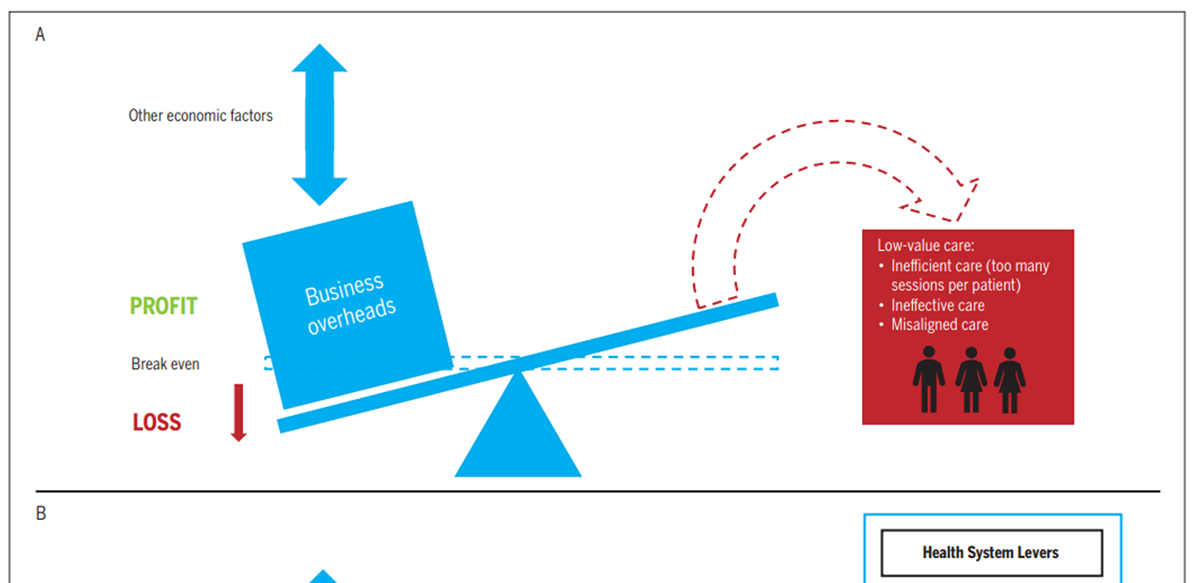
Figure
Page 4Reducing barriers to direct access; increasing primary contact responsibilities of physical therapists, including case management in workers’ compensation; and reorienting the workforce (eg, the ratio of physical therapists to general practitioners to specialists) based on need are examples of government actions that could help the private sector compensate for reducing low-value care (FIGURE). The net effect would be more episodes of care diverted to the private physical therapy sector to meet clinically appropriate needs and less incentive to bill for visits per patient.
Governments could shift funds currently spent on ineffective therapies to packages of evidence-based physical care that include quality indicators. [13] In Australia, the government currently pays for ineffective spine surgeries (at up to A$53,700 per operation), but not for an evidence-based exercise program provided by a physical therapist (the government pays for a maximum of 5 physical therapy visits annually, for selected patients, at a cost of A$311). [12] Clearly, this needs to change.
Action From Insurers
Systems based on fee for service have higher visit numbers than those where clinicians are paid a fixed salary (socalled “capitation” models). [5] The capitation model has worked well in the United Kingdom, where the quantity and costs of care for a given health condition are substantially lower than in countries with fee-for-service payment systems. To move away from fee for service, insurers could fund packages of evidence-based physical therapy care (eg, progressive resistance training and education for knee osteoarthritis).
Moving away from fee-for-service models could remove the incentive to overservice, because payment for an episode is fixed. Of course, there is potential to exploit package-based funding; some patients and clinicians may feel that they need to use all allotted sessions, which leads to more care rather than less. Other limitations of package-based care include third-party payers having strong influence on the number of sessions a physical therapist can provide, irrespective of a patient’s progress. A focus on outcomes and quality indicators is therefore essential, as is ongoing evaluation of any new funding scheme. Action From Consumers Consumers play an important role in addressing overuse by demanding care that is evidence based. Shared decision making will be important but is unlikely to solve such a complex problem. It may, however, empower consumers to look critically at the care they are paying for. Physical therapy is often associated with substantial out-of-pocket costs. As more consumers become aware of the concept of value in health care, clinicians and their patients should be asking themselves, “Do the benefits of this care justify its cost?” The answer becomes difficult when care is discretionary, in the “gray zone,” [8] or when the payer is not an individual but a faceless insurance company.
Conclusion
Efforts to address overuse in the private sector need not destroy small businesses. In theory, the solution is simple: replace low-value services with high-value services. This requires a substantial redesign of systems: funding arrangements, clinical responsibilities, referral patterns, and access to physical therapy. Rigorous and ongoing evaluation of any policy to address theoretical drivers of overuse would ensure that physical therapy in the private sector may remain as valuable as possible. We hope this editorial serves as a call to better understand and overcome the economic drivers of overuse.
References:
Australian Commission on Safety and Quality in Health Care.
The Second Australian Atlas of Healthcare Variation.
Sydney, Australia: Australian Commission on Safety
and Quality in Health Care; 2017.Birkmeyer JD, Reames BN, McCulloch P, Carr AJ, Campbell WB, Wennberg JE.
Understanding of regional variation in the use of surgery.
Lancet. 2013;382:1121-1129.
https://doi.org/10.1016/S0140-6736(13)61215-5Cherkin DC, Deyo RA, Loeser JD, Bush T, Waddell G.
An international comparison of back surgery rates.
Spine (Phila Pa 1976). 1994;19:1201-1206.
https://doi.org/10.1097/00007632-199405310-00001Gawande A.
The cost conundrum.
The New Yorker. June 1, 2009. Available at:
https://www.newyorker.com/magazine/2009/06/01/the-cost-conundrumGosden T, Forland F, Kristiansen IS, et al.
Capitation, salary, fee-for-service and mixed systems of payment:
effects on the behaviour of primary care physicians.
Cochrane Database Syst Rev. 2000:CD002215.
https://doi. org/10.1002/14651858.CD002215Jain NB, Peterson E, Ayers GD, Song A, Kuhn JE.
US geographical variation in rates of shoulder and knee
arthroscopy and association with orthopedist density.
JAMA Netw Open. 2019;2:e1917315.
https://doi.org/10.1001/jamanetworkopen.2019.17315Machlin SR, Chevan J, Yu WW, Zodet MW.
Determinants of utilization and expenditures for episodes
of ambulatory physical therapy among adults.
Phys Ther. 2011;91:1018-1029.
https://doi.org/10.2522/ptj.20100343Michaleff ZA, Zadro JR, Traeger AC, O’Keeffe M, Décary S.
Overcoming Overuse Part 2: Defining and Quantifying
Health Care Overuse for Musculoskeletal Conditions
J Orthop Sports Phys Ther 2020 (Nov); 50 (11): 588-591Mulley AG.
Inconvenient truths about supplier induced demand
and unwarranted variation in medical practice.
BMJ. 2009;339:b4073.
https://doi.org/10.1136/bmj.b4073O’Keeffe M, Traeger AC, Michaleff ZA, Décary S, Garcia AN, Zadro JR.
Overcoming Overuse Part 3: Mapping the Drivers
of Overuse in Musculoskeletal Health Care
J Orthop Sports Phys Ther 2020 (Dec); 50 (12): 657-660Rommel A, Kroll LE.
Individual and regional determinants for physical therapy utilization
in Germany: multilevel analysis of national survey data.
Phys Ther. 2017;97:512-523.
https://doi.org/10.1093/ptj/pzx022Traeger AC, Buchbinder R, Elshaug AG, Croft PR, Maher CG.
Care for Low Back Pain: Can Health Systems Deliver?
Bulletin of the World Health Organization 2019 (Jun 1); 97 (6): 423–433Westby MD, Klemm A, Li LC, Jones CA.
Emerging role of quality indicators in physical therapist practice
and health service delivery.
Phys Ther. 2016;96:90-100. https://doi.org/10.2522/ptj.20150106Zadro JR, Décary S, O’Keeffe M, Michaleff ZA, Traeger AC.
Overcoming Overuse: Improving Musculoskeletal Health Care
J Orthop Sports Phys Ther 2020 (Mar); 50 (3): 113–115
Return NON-PHARMACOLOGIC THERAPY
Since 9-26-2021


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |