Effects of a Physician-supervised, Structured Meal
Replacement Program on Body Composition and Weight LossThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: American College of Nutrition Proceedings (2015) ~ FULL TEXT
Francis C. Lau, PhD, FACN; Bruce P. Daggy, PhD, FACN,
and Jamie F. McManus, MD, FAAFP.
Shaklee Research Center,
Pleasanton, CA
Why was this study done?
Previous Shaklee studies demonstrated the effectiveness of a meal replacement program for weight loss. This study of employees was designed to further understand the reason for the success of the program by looking at body composition (percent of body protein and fat) and the role of lean body mass in weight loss and maintenance.
What This Study Found
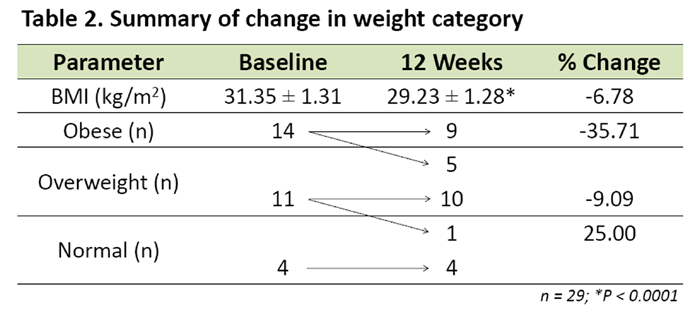
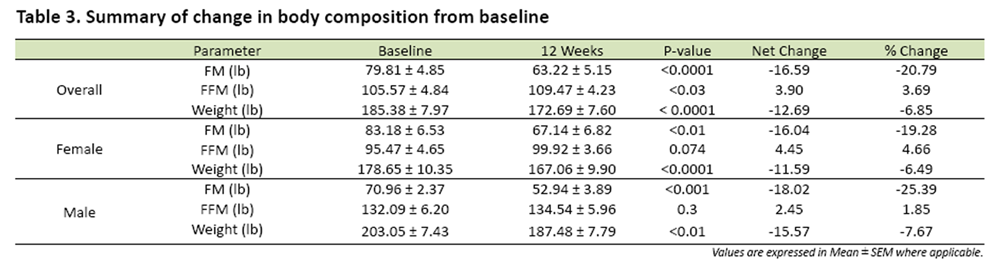
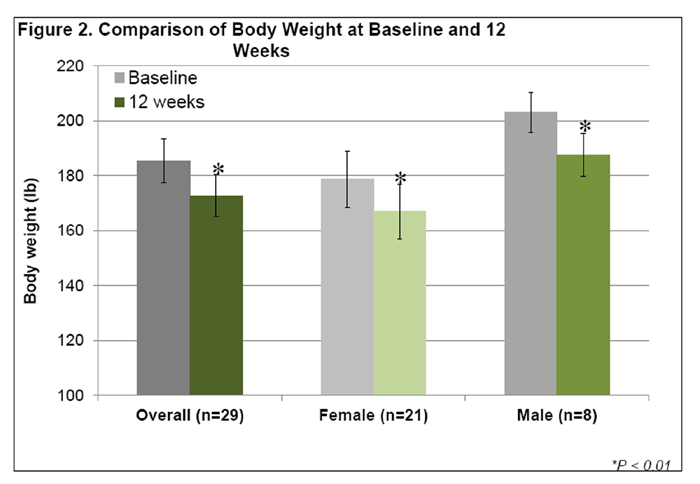
After 12 weeks, participants lost an average of 12.7 lb (or 6.9%) of their initial body weight (p<0.0001). Fat mass was significantly reduced by 16.6 lb (p<0.001) with a concomitant increase of 3.9 lb in fat-free mass (p<0.03). Body Mass Index (BMI) was significantly reduced from 31.4 to 29.2 kg/m2 (p<0.0001). Categorical shift in weight classification was observed in 5 out of 14 subjects who were obese at baseline.
Previously we showed that a physician-supervised, structured meal replacement program was effective in facilitating weight loss. The current study was designed to evaluate whether such a program may promote weight loss through alteration in body composition.
The study was conducted as an employee wellness weight loss challenge in a workplace setting. Participants received free physician consultations and were advised to use a customizable 3-meal-a-day structured meal plan featuring 2 meal replacements daily. Meal replacement products were designed to deliver high levels of protein with added leucine. Participants were given the meal replacement products free of charge and were incentivized with prizes at the end of the challenge based on percent of initial body weight lost. There were 7 brief physician-supervised consultations and weigh-ins: at baseline and at two-week intervals thereafter for 12 weeks. Body composition was assessed at baseline and at 12 weeks by bioimpedance analysis (BIA). To be included in the analysis, participants were required to complete baseline and 12-week bioimpedance measurements. Missing data for bi-weekly weigh-ins were imputed using last-observation-carried-forward method. Student’s t-test was used for comparisons between two time points. For comparison of reduction in body weight at different time points, ANOVA was used. Pvalues less than 0.05 were considered to be statistically significant.
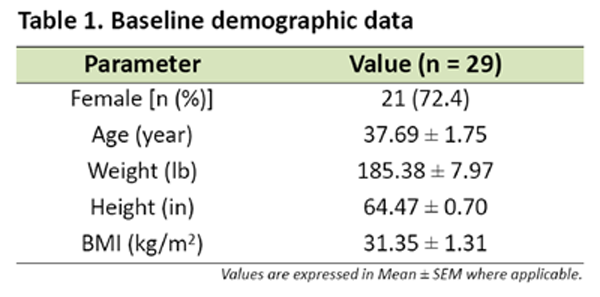
One out of 30 participants who completed baseline bioimpedance measurements dropped out at the end of 12 weeks. Baseline characteristics for the completers (n = 29) were as follows: average age = 37.7 years, average body weight = 185.4 lb, average BMI = 31.4 kg/m2 , average fat mass = 79.8 lb, and percent of female participants = 72.4%. After 12 weeks the completers lost an average of 12.7 lb or 6.9% of their initial body weight (p<0.0001). Fat mass was significantly reduced by 16.6 lb (p<0.001) with a concomitant increase of 3.9 lb in fat free mass (p<0.03). BMI was significantly reduced from 31.4 to 29.2 kg/m2 (p<0.0001). Categorical shift in weight classification was observed in 5 out of 14 subjects who were obese at baseline.
The results indicate that combined with physician supervision this structured meal replacement program promoted significant and clinically meaningful weight loss in 12 weeks. Bioimpedance analysis suggests that the observed weight loss was associated with a significant reduction in fat mass. Additional BIA studies are warranted to evaluate the effects of this program on body fat loss and muscle sparing for weight management
From the Full-Text Article:
BACKGROUND AND OBJECTIVES
Structured meal replacement plans consisting of optimized micro- and macronutrient composition combined with physician supervision have been shown to promote weight loss by providing convenient alternatives to the typical high fat, hyperglycemic, and supersized American diets.
The current study examined the effects of a structured meal replacement, physician supervised diet program on weight loss and body composition in a work place setting. The diet plan consisted of two hypocaloric, high protein, low glycemic meal replacements and one self-prepared meal based on recipes provided. Low caloric snacks were available between meals.
METHODS
Design: The study was conducted in a workplace setting. Participants were advised by a physician to use a customizable 3-meal-a-day structured meal plan: two meal replacements and one balanced dinner daily.
Diet Plan: Meal replacements include low-glycemic shakes and bars each providing approximately 20–24 g of protein, 3 -7 g of fat, 30–37 g carbohydrate, 6–7 g of fiber, and 23 vitamins and minerals for a total of 260–270 Calories per serving. Snacks contain 6–10 g of protein, 2–3 g of fiber, and 100–140 Calories per serving. Dinner recipes typically consist of 4 oz. protein from skinless chicken, pork tenderloin or lean beef; 1 cup of steamed vegetables; a small serving of carbohydrate such as a small baked potato, 1/3 cup of brown rice or a 6” tortilla; a small salad of healthy leafy greens with low-calorie dressing.
Data Collection: There were 7 brief physician-supervised consultations and weigh-ins: at baseline and at two-week intervals thereafter for 12 weeks. Bioimpedance data were collected at baseline and week 12. To be included in the statistical analysis, participants were required to complete baseline and week 12 bioimpedance measurements.
Statistics: Missing biweekly weigh-in data were imputed using last-observation-carried-forward method. Student’s t-test was used for comparisons between two data points. For comparison of multiple data points, ANOVA was used. P-values less than 0.05 were considered to be statistically significant.
SUMMARY
Significant loss in fat mass (-16.6 lb) with a concomitant increase in fat free mass
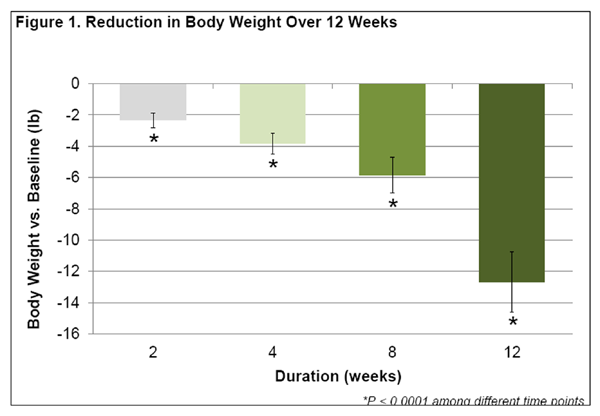
(+3.9 lb) was observed after 12 weeks (Table 3).Net body weight reduction of 12.7 lb (6.9% of initial body weight) occurred after
12 weeks (Table 3); significant reduction was observed after 2 weeks (Figure 1).In general, men lost significantly more weight than women (-15.6 vs. -11.6 lb)
after 12 weeks (Figure 2).Significant decrease in BMI by 2.2 kg/m2 was seen after 12 weeks, shifting the
average BMI from 31.4 (obese category) to 29.2 (overweight category) (Table 2).Categorical shift in weight classification was observed such that 5 out of 14 obese
participants shifted to overweight category. Out of the 11 overweight participants,
1 shifted to normal weight category. No categorical change was observed in the
normal weight cohort (Table 2).
CONCLUSIONS
This structured meal replacement program combined with physician supervision resulted in significant and clinically meaningful weight loss in 12 weeks. Bioimpedance analysis suggests that the observed weight loss was associated with a significant reduction in fat mass. Additional BIA studies are warranted to evaluate the effects of this program on body fat loss and muscle sparing for weight management.
Return to SHAKLEE STUDIES
Since 9-10-2017


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |