

Outcomes of a 3-Month Employee Wellness Weight Loss Challenge:
A Physician-Supervised, Structured Meal Replacement ProgramThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: American College of Nutrition's 55th Annual Conference (2014) ~ FULL TEXT
Jamie F. McManus, MD, FAAFP; Francis C. Lau, PhD, FACN; Bruce P. Daggy, PhD, FACN
Shaklee Research Center,
Pleasanton, CA
Why was this study done?
Obesity may be one of the largest threats to overall individual health that we face. A number of conditions are associated with increasing weight gain, including diabetes, heart disease, stroke, and even certain cancers. This study was designed to understand the impact of a structured meal plan on participant’s weight loss efforts.
What This Study Found
Participants following a structured meal program for three months and lost an average of 9.6 pounds (5.1%). Seven out of twenty-nine obese participants (24%) were able to lower their BMI enough to change their classification (from “obese” to “overweight”).
The current study evaluated the effect of a physician-guided weight loss program in a workplace setting. Participants received free physician consultations and were advised to use a customizable 3–meal-a-day structured meal plan featuring 2 meal replacements daily. Participants were able to purchase the program at a discounted price and were incentivized with cash prizes at the end of the challenge based on percent of initial body weight lost.
There were 7 physician-supervised consultations and weigh-ins: at baseline and at 15–day intervals thereafter for 3 months. To be included in the analysis, participants were required to complete the baseline plus 3 additional weigh-ins. Missing data were imputed using last-observationcarried-forward method. Student’s t-test was used for comparisons between two time points. For comparison of reduction in body weight at different time points, ANOVA was used. P-values less than 0.05 were considered to be statistically significant.
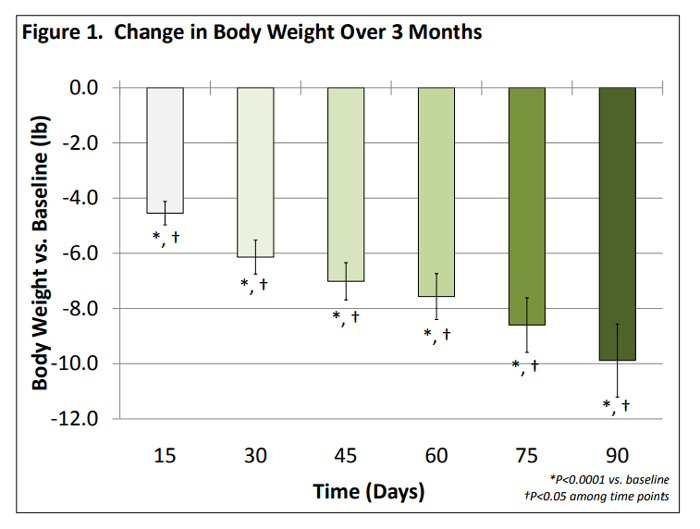
Of 106 participants who enrolled in the challenge, 76 (72%) were completers, with a mean body weight 190 lb and mean BMI of 30 kg/m2 at baseline; 65% of completers were female. Completers lost an average of 9.6 lb or 5.1% of initial body weight (p<0.0001) after 3 months. A categorical shift in weight classification was observed, with 7 of 29 obese participants at baseline shifting to BMI<30 after 3 months. The effect of this program was seen in the first 2 weeks, with a significant weight loss of 4.3 lb (p<0.0001). Sub-analysis indicated that men lost significantly more weight than women after two weeks (5.7 lb vs. 3.9 lb; p<0.05).
The 3 month results indicate that this structured meal replacement program combined with physician supervision exhibited a good completion rate and significant & clinically meaningful weight loss. Longterm studies are warranted to evaluate the effects of this program on weight loss and weight loss maintenance over an extended period of usage.
From the Full-Text Article:
BACKGROUND AND OBJECTIVES
The prevalence of overweight and obesity has grown into a global health concern. According to the Centers for Disease Control and Prevention, more than 69% of U.S. adults age 20 years and above are either overweight or obese. Obesity increases the risk of developing a number of conditions including diabetes, cardiovascular disease, osteoarthritis and some cancers. As a result, obesity and its related comorbidities cost U.S. healthcare system more than $190 billion annually. In order to combat the obesity epidemic, an increased effort has been devoted to developing commercial products, diets, services, and programs to support weight loss and prevent weight gain.
Structured meal plans that are hypocaloric, low in glycemic index, convenient and compatible with nutrition guidelines have been shown to be effective in weight management. This study was designed to evaluate the effect of a structured meal replacement program combined with physician-supervision on weight loss in a workplace setting.
METHODS
The study was conducted in a workplace setting. Participants were advised by a physician to use a customizable 3–meal-a-day structured meal plan: two meal replacements and one balanced dinner daily.
Meal replacements include low-glycemic shakes and bars each providing approximately 20–24 g of protein, 3–7 g of fat, 30–37 g carbohydrate, 6–7 g of fiber, and 23 vitamins and minerals for a total of 260–270 Calories per serving. Snacks contain 6–10 g of protein, 2–3 g of fiber, and 100–140 Calories per serving.
Dinner recipes typically consist of 4 oz. protein from skinless chicken, pork tenderloin or lean beef; 1 cup of steamed vegetables; a small serving of carbohydrate such as a small baked potato, 1/3 cup of brown rice or a 6” tortilla; a small salad of healthy leafy greens with lowcalorie dressing.
Online tools and mobile app providing information on daily caloric intake, recipes, exercise programs, etc. were readily available to motivate participants.
There were 7 brief physician-supervised consultations and weigh-ins: at baseline and at 15–day intervals thereafter for 3 months. To be included in the analysis, participants were required to complete the baseline plus 3 additional weigh-ins.
Missing data were imputed using lastobservation-carried-forward method. Student’s t-test was used for comparisons between two time points. For comparison of reduction in body weight at different time points, ANOVA was used. P-values less than 0.05 were considered to be statistically significant.
RESULTS


SUMMARY
Significant reduction in body weight by 9.6 lb (5.1% of initial body weight) after 3 months; significant results were observed after 2 weeks (Figure 1)
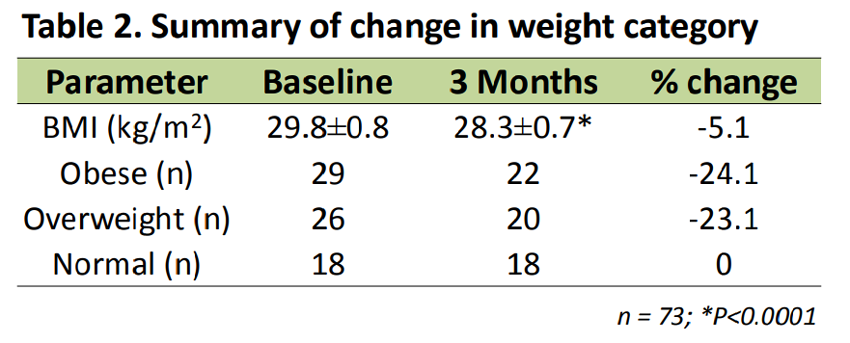
Significant decrease in BMI by 1.5 kg/m2 after 3 months (Table 2)
In general, men lost significantly more weight than women (–13.0 vs. –7.7 lb) after 3 months (Figure 2)
Categorical shift in weight classification was observed such that 7 out of 29 obese participants shifted to overweight (n=6) or normal weight (n=1) category (Table 2) resulting in significant weight loss of 15.0 lb at the end of 3 months
Out of the 26 overweight participants, 6 shifted to normal weight category
No categorical change was observed in the normal weight cohort
CONCLUSIONS
Shaklee 180 structured meal replacement program combined with physician supervision resulted in significant and clinically meaningful weight loss.

Return to SHAKLEE STUDIES
Since 7-28-2017


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |