

Interprofessional Collaboration in Research,
Education, and Clinical Practice:
Working Together for a Better FutureThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Chiropractic Education 2015 (Mar); 29 (1): 1–10 ~ FULL TEXT
OPEN ACCESS Bart N. Green, DC, MSEd and Claire D. Johnson, DC, MSEd
Department of Physical and Occupational Therapy,
Chiropractic Services, and Sports Medicine
at the Naval Medical Center San Diego
Interprofessional collaboration occurs when 2 or more professions work together to achieve common goals and is often used as a means for solving a variety of problems and complex issues. The benefits of collaboration allow participants to achieve together more than they can individually, serve larger groups of people, and grow on individual and organizational levels. This editorial provides an overview of interprofessional collaboration in the areas of clinical practice, education, and research; discusses barriers to collaboration; and suggests potential means to overcome them.
KEYWORDS: Collaboration; Relations, Interprofessional; Role, Professional; Trust
From the Full-Text Article:
INTRODUCTION
Individual commitment to a group effort — that is what makes a team work, a company work, a society work, a civilization work.
—Vince LombardiCollaboration is a term commonly used in research, clinical practice, and health professions education. There are collaborations in almost every aspect of health, such as patient advocacy and health care collaboratives, collaborative learning, interprofessional collaboration in practice and in education, health care value collaborations, business collaborations, collaborative efforts in research and funding. With the increasing use of computers, mobile devices, and social media, collaboration seems to be present more than ever before. At its core, collaboration occurs when 2 or more entities work together to produce a desired and shared outcome. The fields of research, education, and clinical practice are interrelated; research informs education, which in turn influences clinical practice and patient care. In a complementary manner, the needs of practitioners, patients, and educational systems should inform what research may be needed. If we wish to succeed in improving outcomes for students, practitioners, patients, and populations, then we need to consider working together in these environments through collaborations. Therefore, the purpose of this editorial is to discuss interprofessional collaboration in research, education, and practice, particularly with regard to problems to avoid and practices that help to achieve collaboration.
What Is Collaboration?
Collaboration may occur at virtually any level of an organizational structure. People can collaborate within an organization, between organizations, between one another, between countries, and between professions. [1, 2] More commonly referred to as interorganizational collaboration in the business domain, [2, 3] the principles are similar in the health professions and are often referred to as interprofessional collaboration (IPC). There are several key concepts relevant to collaboration, including sharing, partnership, interdependency, and power. [4] Mattessich and Monsey [5](p7) nicely summarize the essence of collaboration:
Collaboration is a mutually beneficial and well-defined relationship
entered into by 2 or more organizations to achieve common goals.The relationship includes a commitment to a definition of mutual
relationships and goals, a jointly developed structure and shared
responsibility, mutual authority and accountability for success,
and sharing of resources and rewards.

Table 1
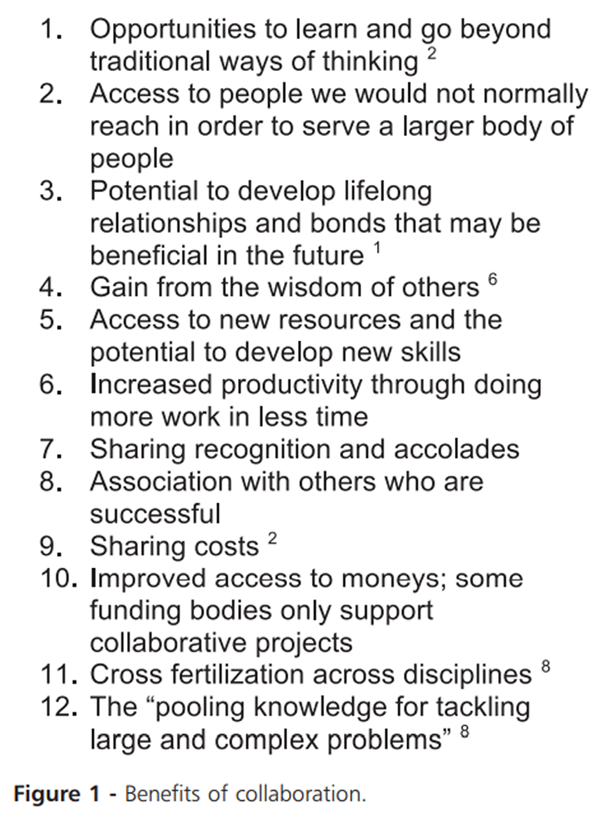
Figure 1 Creating successful collaborations is no mean task, and naysayers may scoff at the idea. However, there are several exemplars of successful large and international collaborations in research, education, and practice to show that it can be done. A sampling is presented in Table 1.
Benefits of Collaboration
Collaborating usually provides a means for organizations, institutions, or professions to achieve more than they can on their own. Business has used collaboration for many years to share costs, spread risk, and reduce supply chain uncertainty while forming strategic economic alliances that also serve as fertile grounds for innovation and learning. [2, 6] Collaboration potentially reduces self-sufficiency in environments demanding great flexibility and innovation. [7] Several benefits of collaboration are listed in Figure 1.
In health care it is generally believed that collaborative efforts yield better health services and outcomes for the populations that are served. [4] Littlechild and Smith [9] state that collaboration leads to improved efficiency, improved skills mix, greater levels of responsiveness, more holistic services, innovation and creativity, and a more user-centered practice. The World Health Organization (WHO) has linked IPC with better outcomes in family health, infectious disease, humanitarian efforts, responses to epidemics, and noncommunicable diseases. [10] Further studies have shown improvements in access to care and coordination of services, appropriate use of specialty care, chronic disease outcomes, and safety. [10, 11] Important indicators of safety, patient care, and environment of care, such as complications and error rates, length of hospital stay, conflict among caregivers, staff turnover, and mortality rates, have all been shown to decrease in collaborative care environments. [10]
Interprofessional Collaboration in Research
Science and knowledge are foundational for a health care profession to exist, and research is one means of achieving these requirements. The problems that must be solved in the modern era are complex, and solutions may not be available if one is working alone. The National Academies suggest that interprofessional or interdisciplinary collaboration may offer solutions when trying to solve multifaceted issues. [12] Interprofessional/interdisciplinary research collaboration occurs when researchers from more than 1 profession/discipline are “working together to achieve the common goal of producing new scientific knowledge.” [13]
The National Academies defines research collaboration as follows [12]:
Interdisciplinary research (IDR) is a mode of research by teams or individuals that integrates information, data, techniques, tools, perspectives, concepts, and/or theories from two or more disciplines or bodies of specialized knowledge to advance fundamental understanding or to solve problems whose solutions are beyond the scope of a single discipline or field of research practice.
Collaborating parties benefit not only in accomplishing research studies, but also in other, less tangible areas. IPC among researchers can help build informational networks, encourage different ways of thinking, and stimulate new solutions to old problems.
Each profession's research community faces various obstacles, such as limited workforce, resources, and expertise. For researchers who work in the isolation of their own profession, there are limitations and risks for not collaborating. On the profession or discipline level, working in a research silo can create a false sense of security because ideas are not likely to be challenged. This can result in a small fish who thinks to be a big fish simply because he is in a small pond. When working in seclusion, work will likely go only so far and will not reach as wide an audience as might be possible as when working with others. As well, there is the possibility that a solution may have already been found elsewhere; thus, isolated research efforts may waste limited resources. Research done in segregation likely can benefit from better infrastructure. Finally, without collaboration, some research may result in poor-quality studies.
Collaboration can be a significant catalyst to positive advancement in research, as it allows access to resources so that more complex, and perhaps more meaningful, investigation may be possible. Research that may not have been possible if done by a single profession may be possible when done in collaboration with others. [14] Resnick [15] states that “while multidisciplinary research brings disciplines together, interdisciplinary research cuts across the disciplines and fosters the integration of ideas.” It has been suggested that there is a correlation between collaborative research and prestige, [16] increased success of publication, [8] and citability (ie, impact). [17, 18] As stated by Frenken et al [19] “Research collaboration enhances the quality of research, which leads papers with more authors to be cited more often.” Results of research may have a better chance of being implemented if there are multiple professions to disseminate the findings. This is especially important if the results have direct application to clinical practice.
Breaking past professional barriers to achieve research collaboration can be challenging. A profession that has few resources and little access to funding may not be invited, or even considered, to participate in larger studies or projects. Some health professions do not have many (or any) experts in particular areas within their profession to perform certain areas of research, especially those in emerging fields. It is also difficult to initiate a collaborative effort when one has few resources to bring to the relationship. Those with few resources are often the professions and disciplines that especially need to collaborate in order to improve and may find that larger organizations are receptive to including them, especially if it helps build more collaborative infrastructure.
Trust is an important factor for collaboration in research. The culture of science has traditionally been secretive. Scientists must compete for funding; sharing novel ideas may risk that a fundable project is “stolen,” either intentionally or unintentionally. Therefore, trust and respect of others in a collaboration are necessary to prevent withholding of ideas and assistance. There may also be a funding advantage to participating in collaborative research. There has been a movement by major funding agencies to reward and value multidisciplinary collaborations. [20] So, if helping humanity is not a big enough motivator for collaboration, then better funding may be a motivating stimulus.
Value continues once the research is done. After a collaborative study is complete, the communications among researchers often will continue. Skills and ways of thinking that were shared among group members across the disciplines can have long-lasting effects. The traditional approaches of 1 discipline are expanded by working with other professions; thus, the problem or the approach will have been seen in a new light. As Lee et al [14] suggest, “There is a general consensus that interdisciplinary collaboration is important in solving large scale, complex biomedical questions.” If we wish to tackle the big problems that we are facing, then we need to consider seeking out and developing better and more interprofessional and interdisciplinary relationships in research.
Interprofessional Collaboration in Practice
We have trained, hired and rewarded people to be cowboys, but it's pit crews that we need.
— Atul Gawande, MD, MPHInterprofessional collaborative practice (IPCP) has emerged in health care over several decades, [21, 22] but has garnered more support, particularly in the past 15 years, as a means to address medical error. [21, 23] Also, the advent of patient-centered medical homes [21] and family home teams [24] and a global shortage of primary care providers in areas with major health disparities [10] have made IPCP an attractive model to, it is hoped, provide better care to populations of health care users.
IPCP has been defined by WHO [10] as follows:
Collaborative practice in health-care occurs when multiple health workers from different professional backgrounds provide comprehensive services by working with patients, their families, careers and communities to deliver the highest quality of care across settings. [10]
IPCP involves more than different health care providers applying their unique skills and knowledge to the management of a patient. Collaboration occurs when individuals have mutual respect for one another and one another's professions and are willing participants in a cooperative atmosphere. [25] It has been suggested that IPCP is different from interdisciplinary, multidisciplinary, and transdisciplinary practice, all terms used within the recent past to denote care provided by more than 1 health care provider for the benefit of a patient. [26-28] While these practices are indeed noteworthy for their contributions to health care, the unit of study is a single patient and the model is focused on the health care provider(s), whereas the unit of study in IPCP is often a community of patients and the model is focused on improving health outcomes. Thus, when we look at IPCP, we must think of the bigger picture and health in populations.
Traditionally, an individual patient has sought care for a disease or disorder from a reputable health care provider. [29] Under such a model, it was conceived that this singular health care provider working in the “silo” of his or her own office could meet the needs of the patient. Today, with chronic and complex diseases requiring multiple specialty providers [30] and the role of primary care increasingly shifting toward the provision of services to populations of people with massive disparities, there is a great need for team-based community care more reminiscent of public health practice than health care. From a social perspective, practices that focus on the skill set and charisma of a singular health care provider are inefficient and costly. As has been noted in the Institute of Medicine's [30] landmark report The Future of the Public's Health, “smaller practices have great difficulty in organizing the array of services and support needed to efficiently manage chronic disease.”
In many countries, health care systems are fragmented and unable to meet the health care needs of the population. [10] A chief force driving the use of IPC is the shortage of primary care providers that is occurring globally. This is a critical barrier to achieving the health-related Millennium Development Goals. [10] Part of the United Nations Millennium Development Declaration, several of these 8 international goals have health-related indicators, such as reducing child mortality rates, improving maternal health, and decreasing common and endemic infectious diseases. [31] Gostin and colleagues [32] poignantly state, “Siloed models centered on temporary fixes are not sufficient to greatly alleviate the overall burden of disease in developing countries.”
Researchers at WHO have found that health care workers who are team players are the ones who succeed in austere situations dealing with extremely complex issues. [10] IPC relies upon the ready integration of people with diverse talents, including those not often associated with health care, who may assist in the improved health care outcomes of the group being served. In a collaborative environment, the input of economists, logisticians, informatics specialists, technology experts, and others may be critical to success. This perspective is something common in public health but foreign to most patient care environments. [23] Collaboration at this level requires participants to work together with open minds and to value what each team member brings to the team. Such collaboration is evident in a proposed interprofessional oath suggested by Brown and colleagues [33]: “We will work with others to provide care, recognizing the unique skills of each, and we will seek to collaborate effectively on the healthcare team.” This environment is perhaps best summarized by Hall, [34] when she says, “The milieu for collaborative practice must foster a status-equal basis between the various team members.”
Interprofessional Collaboration in Education
Interprofessional education (IPE) “occurs when students from 2 or more professions learn about, from, and with each other.” [10] It has been suggested that to be a genuinely interprofessional education experience such interaction requires purposeful integration and collaboration among the disciplines, whether in an educational or practice environment. [23]

Figure 2 IPCP and IPE are related. Advocates state that IPE must be a part of the professional training of health care workers in order to reach the goal of IPCP. In its widely acclaimed and often-cited publication, Framework for Action on Interprofessional Education and Collaborative Practice, [10] WHO clearly outlines the necessary elements and relationships inherent to IPE and IPCP. As shown in Figure 2, the health and education systems exist in a local context and are there to provide the health care needs of the local population. Within this environment, future health care workers ought to be trained to work together as members of a “collaborative, practice-ready workforce” [10] (ie, IPE) that provides collaborative health care to the population. A workforce that is ready for IPC therefore emerges from IPE training experiences. The goal of the IPC health care system is to deliver better health outcomes to the population. [10]
Receiving formal IPE training has benefits. While some people without training in collaborative practice might be able to figure out how to function or thrive in IPCP, it has been shown that training people using IPE leads to “members who show respect and positive attitudes towards each other and work towards improving patient outcomes.” [25] While health care systems have moved toward IPC, teamwork training in health professions education has not kept pace with such changes. [21] IPE and IPCP are linked to what society needs; through IPE, the workforce is trained to work better as a team to deliver better health outcomes to the community being served.
Collaborative work in IPE and IPCP has been done across geographic and political boundaries. Much of the work that has been published related to IPE and IPCP originates from Canada, the United Kingdom, the United States, and Australia. [352] However, attention has been garnered for IPE from around the world since WHO made it an essential component of health professions education. [10] In an international survey of WHO's 193 member states, Rodger and colleagues [36] found evidence of IPE in 41 different countries, with varying levels of complexity noted in collaborative efforts. This makes sense given the shortage of primary care services occurring globally.
Opportunities for involvement in various IPCP and IPE groups are widely distributed, including those inCanada (www.cihc.ca),
Europe (www.eipen.eu),
the United Kingdom (http://caipe.org.uk),
United States (www.aihc-us.org),
Australia and New Zealand (www.aippen.net),
Japan (www.jaipe.jp and http://jipwen.dept.showa.gunma-u.ac.jp),
Scandinavia (www.nipnet.org),
and Eastern and African countries (www.ecipen.org).Furthermore, annual international conferences focus on IPCP and IPE, such as the All Together Better Health conferences that are supported by 8 different organizations with international representation (www.atbh.org). There are also the Collaborating Across Borders conferences, a joint IPCP/IPE effort between Canada and the United States (http://www.aihc-us.org/collaborating-across-borders) and the New Zealand Interprofessional Health Conference (http://www.nziphc.co.nz).
Potential Barriers to Collaboration
The secret is to gang up on the problem, rather than each other.
— Thomas StallkampGiven the core elements of collaboration (participants from different cultures, high level of interaction, mutual authority, sharing of resources), it has its potential problems. What may start out as a well-meaning endeavor can lead to conflict. [3] In fact, due to the very nature of a collaborative environment, conflict should be expected; but with this comes the opportunity for better understanding. IPC is essentially a melting pot of professions, and each profession has its own unique history, culture, attitudes, values, customs, and beliefs. How professionals in collaborations come to understand and appreciate these nuances can pose several challenges. [34] For example, 1 profession may see another profession as an outsider or rival and not want to involve this profession in collaboration. There also may be professional groups that are afraid to interact with other professional groups for various reasons, not the least of which could be historical isolation or low status within the social hierarchy. There are also situations in which a culturally dominant profession may have attitudes that are prejudiced against other professions, as has been stated by Gaboury and colleagues [37]: “It is plausible that practitioners who belong to occupational groups that have obtained, or are in the process of obtaining, legitimacy through licensing, certification, or registration may be seen differently by their biomedical peers.” The aforementioned are all relatively minor obstacles compared to that of bringing together professions that historically have been at odds with one another. In summary, the ideological differences and power relations brought to collaboration from different professions can be potentially problematic. [4, 38]
Boundary disputes, status issues, language barriers, customer service orientations, and reporting structures are all potential challenges. [9, 39–41] Other authors warn of problems with IPC in areas where the physical space is not adequate or appropriate in design, [42] where role overlap and confusion exist, [4, 38] and where there is territorialism. [42, 43] The conclusion is that collaboration [44] will lead to conflict. However, the management of any conflict to arrive at a benefit for the customer is a necessary step in building an effective collaboration. [44, 45] It is recommended that collaborative groups have an agreed-upon method for resolving conflict, starting with resolution at the level of individual participants and working out toward the larger levels of organization. [44]
There are also concerns that IPC can lead to the loss of uniqueness of a profession or professional identity. [23] When participants focus on the team goals and the people that they are serving, then differences between professions can be seen as unique opportunities to bring a valuable and different point of view or skill set to the collaboration. [23] The collaboration may result in overlap, to some degree, of the activities of any 1 profession involved in it, but the collaboration should not duplicate the efforts of any particular profession. [5] As stated by D'Amour and colleagues, [4] working together in this way requires “implementing a logic of collaboration rather than a logic of competition.”
Getting to Collaboration
If everyone is moving forward together, then success takes care of itself.
— Henry FordLike other things that are valued but difficult to attain, such as exalted leadership, fine wine, or an enduring marriage, working collaborations are perhaps as much an art as they are a science. Experts suggest that the process of building a culture of collaboration is not exactly methodical, is somewhat organic, and requires a great deal of practice and nurturing. [2, 46, 47] It is suggested to start small and first learn to work collaboratively at a local level. Examples might be collaborating within an office, department, or group. Once skills in collaboration are developed (not tolerance or just working in the same building, but actually accomplishing a task together), then reaching out to larger circles of influence and other professions may be easier.
Many books and articles have been written on the topic of collaboration, and several are cited in this article; thus, we refer the reader to these sources for comprehensive discussions about attaining quality collaborations. However, there are some cogent points relevant to forging collaborations across disciplines that are expressed by several experts, and we briefly review them here and provide a checklist for assessing readiness for collaboration in Appendix_A.
Know when to use collaboration and when not to. Effective leaders can identify when it is the right time to collaborate. Essentially, collaboration is a tool to employ to achieve a desired outcome and it will not be a good tool to use in all situations. Collaboration tends to work best in diverse groups where the people participating in the collaboration have authority to make final decisions and when innovation and creativity are desired. [45] As stated by Hansen, [1](p15) “The goal of collaboration is not collaboration, but better results.”
Know what the collaborating professions or organizations stand to gain from the alliance and what the costs are to get there. [1, 48] One expert has suggested that collaboration should only be engaged if the net value of the partnership is more than the sum of the return on the venture, minus the costs and the opportunity costs, such as manpower and time spent on the collaboration that could be spent in other endeavors. [1] In short, some effort needs to be expended in advance of the collaboration to determine if the value/benefits outweigh the costs. [48]
Be aware of the factors that drive the strength of collaboration: alignment of mission/values, [47, 48] personal connections, [48] value generation for each collaborating organization or profession, [48] and improved outcomes. [10]
Become familiar with the factors that lead to successful collaborations. [5] Such factors include attitudes, environmental concerns, communication, resources and trust. [2, 7, 46]
Recognize the intangible elements, such as tacit knowledge, social capital, ownership, disclosure, transparency, motivation, and commitment, that strongly influence peoples' decisions. [46, 49]
Identify barriers to the collaboration that you desire to build, and find ways to remove the barriers so that collaborative relationships can evolve. [1]
Create organizational learning objectives and goals to facilitate knowledge creation. [7, 50] Performance goals may stifle knowledge generation when they do more to encourage people to “win” than to learn. [45] If the organization has clear ideas about what it wants to learn from the collaboration, then it is easier to identify when new knowledge is generated by or obtained from the collaboration. Identify the new learning processes, outcomes, and innovations that occur during collaboration as assets and build upon these successes. [6, 7] Inkpen [7] suggests that collaborations should consider both incremental and large gains in knowledge as successes.
Commit to collaboration for the long haul because it is a long-term process and investment. [46, 47] Since collaboration is experiential and based upon relationships, it takes time to develop. If an organization's culture and leadership are not invested and committed to establishing formal relationships, then collaboration is not a good fit. [7, 23, 25] A long-term commitment, both in principle and in resources, is a necessary element of success.
Know when it is time to stop a collaboration. [7] Collaborations are a means to an end, and if the end is reached, it may be time to stop the collaboration or change it to meet a new goal. While ceasing a collaboration can be disappointing for some, it may be prohibitive to continue a collaboration for which the net value of the collaboration is a liability. [1]
A recent expert report from the Josiah Macy Jr Foundation identified 3 important recommendations for establishing interprofessional partnerships, all of which are long-term investments for any institution [51]:
Make changes in the content and conduct of health professions education necessary to graduate practitioners who partner with patients, families, and communities.
Make changes in health professions education organizations and health care organizations necessary to facilitate durable partnerships, both new and existing, with patients, families, and communities.
Build the capacity for partnerships among patients, families, and communities and health professions education and health care organizations.
Suggested Resources
For anyone interested in setting up collaborations in research, education, or clinical practice, seek out existing publications, training centers, and experts who have established collaborations. For example, those interested in research collaboration can seek out funding bodies that require collaboration, become participants in established collaborations (eg, the Cochrane Collaboration or Best Evidence Medical Education Collaboration), or seek new opportunities by identifying gaps in the literature that need interprofessional solutions. Another approach is to inventory current research at one's institution and consider if any of the projects or goals would benefit from team research efforts.
For educators, there are many excellent resources for getting started in IPE, including the WHO framework, which includes suggestions for actions, participants, and outcomes. [10] Those interested in pursuing IPE should consider this document required reading, as it serves as a primer for this topic. The WHO framework also makes the case for placing the community as the unit of concern because of global shortages in health care providers and health workers.
In clinical practice, numerous health professions are currently working on developing policies and educational competencies related to IPC, including physical therapy, [52] nursing, medicine, dentistry, public health, and pharmacy. [21] One excellent resource on IPE and IPCP is a competencies monograph by the Interprofessional Education Collaborative (IPEC) that has application across health professions. [21] In the United States, IPEC is the collaborative that has done the most work in IPE. The chiropractic profession has joined the complementary and alternative health disciplines in developing competencies for interprofessional practice through the Academic Consortium for Complementary and Alternative Health Care (ACCAHC).
This consortium worked independently to develop IPE competencies and then reviewed the IPEC document, [21] which was released simultaneously; it eventually became a supporting organization of IPEC. ACCAHC also created 3 additional elements for IPE, as they relate to the professions represented by ACCAHC. These elements include a value for personal behaviors and self-care practices that reflect optimal health and wellness, a section on evidence-based care, and a section on institutional health care culture and practice. [53]
Canada has been a world leader in IPC for more than 15 years, with government interest and funding of research and educational programs focused on more integrated, team-based approaches to meet the health care and service delivery needs of the Canadian population. [23] A wealth of information and wisdom is available from the Canadian Interprofessional Health Collaborative. Like IPEC, this collaborative has developed competencies for IPE. However, in their document, A National Interprofessional Competency Framework, competencies are unique in the sense that they integrate knowledge, skills, and attitudes to arrive at judgments over 6 competency domains considered to be critical to IPCP. [54]
Faculty development in IPE is critical to the success of IPE programs. [23, 39] Institutions must be willing to invest the resources necessary to develop faculties into communities of collaborators who can model the desired traits and behaviors to students. Faculty members who are legendary for their inability to work well with others are not likely to be good ambassadors for IPC, nor are they likely to appreciate training in the topic. Bridging the gap for these faculty members may be difficult, but 1 successful method is to engage them in team-oriented trainings that show obvious improvements in patient outcomes or safety. [55] Faculty development programs should be developed using the same educational principles required to teach students: team-based learning, active learning, problem solving, utilization of available resources, and feedback mechanisms. [55] Buring and colleagues [56] have published an excellent article on faculty training, including desired attributes of IPE educators, faculty development resources, and a rubric containing selected topics mapped to Institute of Medicine competencies, teaching methods, and learning objectives. Mackenzie and colleagues [57] also offer an informative account of the key elements of success of their IPE program by linking successful organizational structure and actions with the Canadian Interprofessional Health Collaborative competency domains. [57]
CONCLUSION
When discussing collaboration, the key issues include putting the community or client first, the organization second, oneself last, and prejudices aside. Shortages in primary care providers and the challenges of managing chronic, complex diseases, such as musculoskeletal problems, are excellent opportunities for the health professions to bring unique skills to collaborative environments. Times are changing, silos are falling, national health burdens are being shared, and it is going to take much more than a single practitioner or paradigm to solve the serious health care issues confronting humanity today and in the future. Through collaboration, we can work together for a better future.
Appendix A Readiness for collaboration

Funding Sources and Conflicts of Interest
BNG and CDJ receive a stipend for services provided to the Journal of Chiropractic Education and Association of Chiropractic Colleges Research Agenda Conference (ACC-RAC) meeting, respectively. However, this work was performed independent of these relationships, and the authors have no conflicts of interest to declare relevant to this work. The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States Government.
References:
Hansen MT.
Collaboration: How Leaders Avoid the Traps, Create Unity,
and Reap Big Results.
Boston, MA: Harvard Business Press; 2009. xi, 231.Vangen S, Huxham C.
Nurturing collaborative relations: building trust in interorganizational collaboration.
J Appl Behav Sci. 2003;39:5–31.Kumar K, vanDissel HG.
Sustainable collaboration: managing conflict in interorganizational systems.
Manag Inf Syst Q. 1996;20(3):279–300.D'Amour D, Ferrada-Videla M. San Martin Rodriguez L, Beaulieu MD.
The conceptual basis for interprofessional collaboration:
core concepts and theoretical frameworks.
J Interprof Care. 2005;((suppl 1)):116–131Mattessich PW, Monsey BR. 53 St. Paul, MN: Amherst H.
Wilder Foundation; 1992. Collaboration — What Makes It Work:
A Review of Research Literature on Factors Influencing
uccessful Collaboration.
Wilder Research Center.Powell WW, Koput KW, Smith-Doerr L.
Interorganizational collaboration and the locus of innovation:
networks of learning in biotechnology.
Adm Sci Q. 1996;41(1):116–145.Inkpen AC.
Creating knowledge through collaboration.
Calif Manage Rev. 1996;39(1):123–140.vanRijnsoever FJ, Hessels LK.
Factors associated with disciplinary and interdisciplinary
research collaboration.
Res Policy. 2011;40(3):463–472.Littlechild B, Smith R.
A Handbook for Interprofessional Practice in the Human Services:
Learning to Work Together.
New York, NY: Routledge; 2013.World Health Organization.
Framework for Action on Interprofessional Education and Collaborative Practice.
Geneva: World Health Organization; 2010.Lemieux-Charles L, McGuire WL.
What do we know about health care team effectiveness? A review of the literature.
Med Care Res Rev. 2006;63(3):263–300Committee on Facilitating Interdisciplinary Research,
Committee on Science Engineering and Public Policy (US),
National Academy of Sciences (US), National Academy of Engineering,
Institute of Medicine (US) Facilitating Interdisciplinary Research.
Washington, DC: The National Academies Press; 2005. xxv, 306.Katz JS, Martin BR.
What is research collaboration?
Res Policy. 1997;26(1):1–18.Lee ES, McDonald DW, Anderson N, Tarczy-Hornoch P.
Incorporating collaboratory concepts into informatics in support
of translational interdisciplinary biomedical research.
Int J Med Inform. 2009;78(1):10–21Resnick JC.
Increasing opportunity through interdisciplinary research:
climbing down and shattering a tower of babel.
Front Psychiatry. 2011 2:20Bozeman B, Corley E.
Scientists' collaboration strategies:
implications for scientific and technical human capital.
Res Policy. 2004;33(4):599–616.Nomaler Ö, Frenken K, Heimeriks G.
Do more distant collaborations have more citation impact?
J Informetrics. 2013;7(4):966–971.Didegah F, Thelwall M.
Which factors help authors produce the highest impact research?
J Informetrics. 2013;7(4):861–873.Frenken K, Hölzl W, deVor F.
The citation impact of research collaborations:
the case of European biotechnology and applied microbiology
(1988–2002)
J Eng Technol Manage. 2005;22:9–30.Nagarajan R, Kalinka AT, Hogan WR.
Evidence of community structure in biomedical research grant collaborations.
J Biomed Inform. 2013;46(1):40–46Interprofessional Education Collaborative Expert Panel.
Core Competencies for Interprofessional Collaborative Practice:
Report of an Expert Panel.
Washington, DC: Interprofessional Education Collaborative; 2011.WHO Study Group on Multiprofessional Education of Health Personnel.
Learning Together to Work Together for Health:
Report of a WHO Study Group on Multiprofessional Education of Health Personnel:
The Team Approach.
Geneva: World Health Organization; 1988. 72Institute of Medicine (US) Workshop.
Cuff PA: Institute of Medicine (US),
Board on Global Health, National Research Council (US); 2013.
Global Forum on Innovation in Health Professional Education. (2012: Washington DC)Mior S, Gamble B, Barnsley J, Côté P, Côté E.
Changes in Primary Care Physician's Management of Low Back Pain
in a Model of Interprofessional Collaborative Care:
An Uncontrolled Before-After Study
Chiropractic & Manual Therapies 2013 (Feb 1); 21 (1): 6Bridges DR, Davidson RA, Odegard PS, Maki IV, Tomkowiak J.
Interprofessional collaboration: three best practice models
of interprofessional education.
Med Educ Online. 2011 16Boon H, Verhoef M, O'Hara D, Findlay B.
From parallel practice to integrative health care:
a conceptual framework.
BMC Health Serv Res. 2004;4(1):15Johnson, C.
Health Care Transitions: A Review of Integrated, Integrative,
and Integration Concepts
J Manipulative Physiol Ther. 2009 (Nov); 32 (9): 703–713Stone J.
Interprofessional Collaborative Practice: Definitions and Terminology.
Canberra: Australian Capital Territory Health; 2009.Allan J, Barwick TA, Cashman S, et al.
Clinical prevention and population health:
curriculum framework for health professions.
Am J Prev Med. 2004;27(5):471–476Institute of Medicine.
The Future of the Public's Health in the 21st Century.
Washington, DC: National Academies Press; 2003.United Nations.
The Millennium Development Goals Report 2014.
New York, NY: United Nations; 2014.Gostin LO, Boufford JI, Martinez RM.
The future of the public's health: vision, values, and strategies.
Health Aff (Millwood) 2004;23(4):96–107Brown SS, Garber JS, Lash J, Schnurman-Crook A.
A proposed interprofessional oath.
J Interprof Care. 2014;28(5):471–472Hall P.
Interprofessional teamwork: professional cultures as barriers.
J Interprof Care. 2005;19((suppl 1)):188–196Thistlethwaite JE, Forman D, Matthews LR, Rogers GD, Steketee C, Yassine T.
Competencies and frameworks in interprofessional education:
a comparative analysis.
Acad Med. 2014;89(6):869–875Rodger S, Hoffman SJ.
World Health Organization Study Group on Interprofessional
Educational and Collaborative Practice.
Where in the world is interprofessional education?
A global environmental scan.
J Interprof Care. 2010;24(5):479–491Gaboury I, Bujold M, Boon H, Moher D.
Interprofessional collaboration within Canadian integrative
healthcare clinics: key components.
Soc Sci Med. 2009;69(5):707–715Caldwell K, Atwal A.
The problems of interprofessional healthcare practice in hospitals.
Br J Nurs. 2003;12(20):1212–1218Lawlis TR, Anson J, Greenfield D.
Barriers and enablers that influence sustainable interprofessional education:
a literature review.
J Interprof Care. 2014;28(4):305–310Gulati R.
Silo busting: how to execute on the promise of customer focus.
Harv Bus Rev. 2007;85(5):98–108. 45Headrick LA, Wilcock PM, Batalden PB.
Interprofessional working and continuing medical education.
BMJ. 1998;316(7133):771–774Lawn S, Lloyd A, King A, Sweet L, Gum L.
Integration of primary health services:
being put together does not mean they will work together.
BMC Res Notes. 2014 7:66Chung CL, Manga J, McGregor M, Michailidis C, Stavros D, Woodhouse LJ.
Interprofessional collaboration and turf wars: how prevalent are hidden attitudes?
J Chiropr Educ. 2012;26(1):32–39Weiss J, Hughes J.
Want collaboration? Accept—and actively manage—conflict.
Harv Bus Rev. 2005;83(3):92–101. 49Ibarra H, Hansen MT.
Are you a collaborative leader?
Harv Bus Rev. 2011;89((7–8)):68–74. 164Schuman S.
Creating a Culture of Collaboration:
The International Association of Facilitators Handbook.
San Francisco, CA: Jossey-Bass; 2006.
International Association of Facilitators. xxxiv, 498.Adler P, Heckscher C, Prusak L.
Building collaborative enterprise.
Harv Bus Rev. 2011;89((7–8)):94–101. 64Austin JE.
Strategic collaboration between nonprofits and business.
Nonprofit Volunt Sect Q. 2000;29:69–97.Grabher G.
Cool projects, boring institutions:
temporary collaboration in social context.
Regional Studies. 2002;36(3):205–214.McDermott R, Archibald D.
Harnessing your staff's informal networks.
Harv Bus Rev. 2010;88(3):82–89Fulmer T, Gaines M.
Partnering With Patients, Families, and Communities to Link
Interprofessional Practice and Education.
New York, NY: Josiah Macy Jr; 2014. Foundation;Bainbridge L, Nasmith L, Orchard C, Wood V.
Competencies for interprofessional collaboration.
J Phys Ther Educ. 2010;24(1):6–11.Goldblatt E, Wiles M, Schwartz J, Weeks J.
Competencies for optimal practice in integrated environments:
examining attributes of a consensus interprofessional practice
document from the licensed integrative health disciplines.
Explore. 2013;9(5):285–291Canadian Interprofessional Health Collaborative.
A National Interprofessional Competency Framework.
Vancouver, BC: Canadian Interprofessional Health Collaborative; 2010.Silver IL, Leslie K.
Faculty development for continuing interprofessional education and collaborative practice.
J Contin Educ Health Prof. 2009;29(3):172–177Buring SM, Conway S, Hansen L, Westberg S.
Keys to successful implementation of interprofessional education:
learning location, faculty development, and curricular themes.
Am J Pharm Educ. 2009;73(4):60MacKenzie DE, Doucet S, Nasser S, Godden-Webster AL, Andrews C, Kephart G.
Collaboration behind-the-scenes: key to effective interprofessional education.
J Interprof Care. 2014;28(4):381–383
Return to INTEGRATED HEALTH CARE
Return to ALL ABOUT CHIROPRACTIC
Since 12-21-2016


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |