

Manual Interventions for Musculoskeletal Factors in
Infants With Suboptimal Breastfeeding: A Scoping ReviewThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Evidence-Based Integrative Medicine 2018 (Dec 12); 23: 1–12 ~ FULL TEXT
OPEN ACCESS Cheryl Hawk, DC, PhD, Amy Minkalis, DC, MS, Carol Webb, MA, MLIS, Olivia Hogan, and Sharon Vallone, DC
Texas Chiropractic College,
Pasadena, TX, USAExclusive breastfeeding for the first 6 months, and continuing for at least the first year of life, is strongly recommended. Suboptimal breastfeeding, which is breastfeeding that does not meet these recommendations, is a multifactorial issue. Some authorities, particularly in the nursing and lactation counseling professions, have identified musculoskeletal issues that may interfere with successful breastfeeding. The purpose of this project was to survey the literature on manual treatments to correct musculoskeletal dysfunctions in infants with suboptimal breastfeeding. Our research question was, “Have manual interventions been used to correct infants’ musculoskeletal dysfunctions thought to be linked to suboptimal breastfeeding?” We searched PubMed and Index to Chiropractic Literature, from inception through July 2018, as well as relevant gray literature. We assessed quality of randomized controlled trials (RCTs) and cohort studies using modified SIGN checklists, and the overall strength of evidence using GRADE. The search yielded 461 articles, with a final inclusion of 27 articles: 7 expert commentaries, 1 high-quality RCT, 1 low-quality cohort, 1 pilot study, 2 cross-sectional surveys, 5 narrative reviews, and 10 case series or case reports. Combining the 10 case series and reports in our search with 18 discussed in narrative reviews included in our review yielded 201 infants who received manual therapy for nursing dysfunction. No serious adverse events were reported and improvement in nursing ability was observed using various outcome measures, usually maternal report. Based on the GRADE criteria, there is moderate positive evidence for the effect of manual therapy on suboptimal breastfeeding.
Keywords: spinal manipulation, breastfeeding, manual therapy, infants
From the FULL TEXT Article:
Breastfeeding Is an Important Public Health Issue
Exclusive breastfeeding for the first 6 months, and continuing for at least the first year of life, is strongly recommended by authorities. [1] These include the American Academy of Pediatrics, [2] the American College of Obstetricians and Gynecologists, [3] the Association of Women’s Health, Obstetric and Neonatal Nurses, [4] the US Preventive Services Task Force (USPSTF), [5] and the World Health Organization. [6] The term suboptimal breastfeeding is used to describe breastfeeding that falls short of these recommendations. [1, 7]
By this definition, suboptimal breastfeeding is currently highly prevalent globally, with only 40% of infants being exclusively breastfed for the first 6 months. [6] This applies to high-income countries like the United States, where only 25% of infants were exclusively breastfed at 6 months as of 2015. [8, 9] However, similar prevalence is seen not only in other high-income countries, but in middle- and low-income countries as well. [10] In fact, “despite its established benefits, breastfeeding is no longer a norm in many communities.” [11](p491)
This has health consequences for mothers and their babies as well as economic consequences for families and the nation in general. Nine serious pediatric conditions (which may extend beyond childhood) have been linked to suboptimal breastfeeding: acute lymphoblastic leukemia, acute otitis media, Crohn’s disease, ulcerative colitis, gastrointestinal infection, lower respiratory tract infection requiring hospitalization, obesity, necrotizing enterocolitis, and sudden infant death syndrome. [1] Five serious maternal conditions are associated with suboptimal breastfeeding: breast cancer, premenopausal ovarian cancer, diabetes, hypertension, and myocardial infarction. [1] Based only on outcomes for these conditions, a 2017 economic analysis found that suboptimal breastfeeding costs the United States $3.0 billion in medical costs, $1.3 billion in nonmedical costs, and $14 billion in the cost of premature deaths (which were mostly maternal). [1]
Contributing Factors to Suboptimal Breastfeeding
Suboptimal breastfeeding is of course a multifactorial issue, best addressed by broad health behavioral theories such as the ecological model. [12] The ecological model posits that behavior is influenced at multiple levels: intrapersonal, interpersonal, community, institutional, and public policy. A model proposed by Rollins et al [11] is congruent with this approach, applied to the issues of breastfeeding. It suggests that interventions be applied at each level (structural, setting and individual). [11]
Generally, public health agencies emphasize the broader levels of community, institutional and policy. [13] Health care providers tend to work at the intra- and interpersonal levels with patients/clients. The USPSTF, which serves as the gold standard for clinical preventive services, strongly recommends that providers counsel new mothers on breastfeeding. [5] All groups can contribute to solving the problem, and in fact, it is essential that all groups work together in order to provide an environment supportive of optimal breastfeeding. Medical physicians, both family practice and specialties (obstetrics and gynecology and pediatrics), nurses and International Board-Certified Lactation Consultants (IBCLCs) have established recommendations and/or guidelines to operationalize the USPSTF recommendation on breastfeeding counseling. [1, 4, 14]
Musculoskeletal Dysfunction and Suboptimal Breastfeeding
Breastfeeding recommendations often focus on interpersonal, community, institutional and policy levels of intervention. [4, 6, 8] However, it is important to build individual mother-infant dyad issues into the intervention model as well, as proposed by Rollins and colleagues. [11] On this level, some authorities, particularly in the nursing and lactation counseling professions, discuss musculoskeletal issues that may interfere with breastfeeding at the intra- as well as interpersonal level, such as the effects of positioning the infant at the breast. [15, 16] Soft tissue dysfunctions, for example, ankyloglossia (tongue-tie) [17] and congenital torticollis, [18] have also been addressed in the biomedical literature. Ankyloglossia is often treated surgically and has been found to improve the infant’s ability to nurse successfully. [17, 19, 20] The physiology and biomechanics of infants’ nursing movements have been investigated and explicated. [21–24]
However, manual interventions that might improve infants’ ability to nurse effectively are not included in current guidelines, other than an acknowledgement of a possible role for ankyloglossia, which is often surgically addressed. Since clinical practice guidelines are based on evidence, it is important to evaluate the current evidence base for manual procedures which may contribute to successful breastfeeding. We chose a scoping review as the most appropriate design for this purpose, because it is “a form of knowledge synthesis that addresses an exploratory research question aimed at mapping key concepts, types of evidence, and gaps in research related to a defined area or field by systematically searching, selecting, and synthesizing existing knowledge.” [25](pp1292,1294) The purpose of this scoping review is to comprehensively survey the existing literature on manual interventions for musculoskeletal dysfunctions in infants with suboptimal breastfeeding.
Methods
We followed Arksey’s and O’Malley’s methodology for scoping reviews,26 as follows.
Stage 1: Identify the Research Question
Our research question was, “Have manual treatments been used to correct infants’ musculoskeletal dysfunctions thought to be linked to suboptimal breastfeeding?”
Stage 2: Identify Relevant Articles
Because this is an emergent field, we included a variety of resources. A topic expert (SV) identified the most relevant books and organizations. A health sciences librarian (CW) conducted the literature searches.
Electronic databases: PubMed and Index to Chiropractic Literature. The search strategy was:
((“breast feeding” OR breastfeeding OR “sucking behavior” OR “sucking difficulty” OR “sucking difficulties” OR “dysfunctional suck” OR “sucking dysfunction”) AND Humans[Mesh] AND English[lang] AND infant[MeSH])) AND (((((chiropract* OR osteopath* OR manipulati* OR “manual therapy” OR “manual therapies” OR massage) AND Humans[Mesh] AND English[lang] AND infant[MeSH])) OR (“Complementary Therapies”[Mesh] AND Humans[Mesh] AND English[lang] AND infant[MeSH])) AND Humans[Mesh] AND English[lang] AND infant[MeSH])Books on breastfeeding15,27 were used primarily for background information and reference tracking.
Reference Tracking from Relevant Texts15,27
Relevant organizations and networks were used for their reference listings:
- International Chiropractors Association Pediatrics Council:
http://icapediatrics.com/resources/articles/tongue-tie-and-chiropractic/
- Ankyloglossia Bodyworkers Facebook page:
http://www.ankyloglossiabodyworkers.com/professional-resources.html
- International Association of Tongue Tie Professionals:
https://tonguetieprofessionals.org/resources/research/
Stage 3: Select Sources of Information
Both peer-reviewed and non–peer-reviewed literature and other resources were eligible, including gray literature such as conference proceedings and theses. At least 2 investigators (CH, CW, or AM) screened the articles and other resources for eligibility, resolving disagreements by discussion.Inclusion:
English language
Human participants
Publications in peer-reviewed journals
Publications in non–peer-reviewed journals
Books and book chapters
Webpages
Conference proceedings
Exclusion:
Case series and case reports cited in an included systematic review
Nonrelevant (did not address manual approaches and/or musculoskeletal conditions)
Video or PowerPoint presentations
Websites used for advertising purposes
Stage 4: Charting the Data

Table 1

Table 2

Table 3 We categorized the included articles in terms of study design. For those with a higher level of design—randomized controlled trials (RCTs) and cohort studies—we evaluated their quality using modified SIGN (Scottish Intercollegiate Guideline Network) checklists. [28, 29] Studies were rated in the SIGN checklists as “high quality, low risk of bias,” “acceptable quality, moderate risk of bias,” “low quality, high risk of bias,” or “unacceptable” quality. Tables 1 and 2 list the items in in each checklist and explain the scoring system we used to determine the quality rating. We did not assess the quality of lower level studies (narrative reviews, cross-sectional descriptive surveys, case report/series, preliminary and pilot studies, commentaries). Two investigators (CH and AM) rated the studies separately and resolved disagreements through discussion.
We made conclusions about the overall level of evidence using the GRADE (Grading of Recommendations Assessment, Development and Evaluation) system [30]:
http://www.essentialevidenceplus.com/product/ebm_loe.cfm?show=grade.
Table 3 summarizes the GRADE system of assessing the quality of evidence. [30] Two investigators (CH and AM) performed the GRADE assessment independently.
Stage 5: Collating, Summarizing, and Reporting the Results
At least 2 investigators (CH, AM, OH) extracted data from the selected articles. Disagreements were resolved by discussion. We summarized the results of the search in figures, tables, and text.
Results
Identification of Relevant Articles
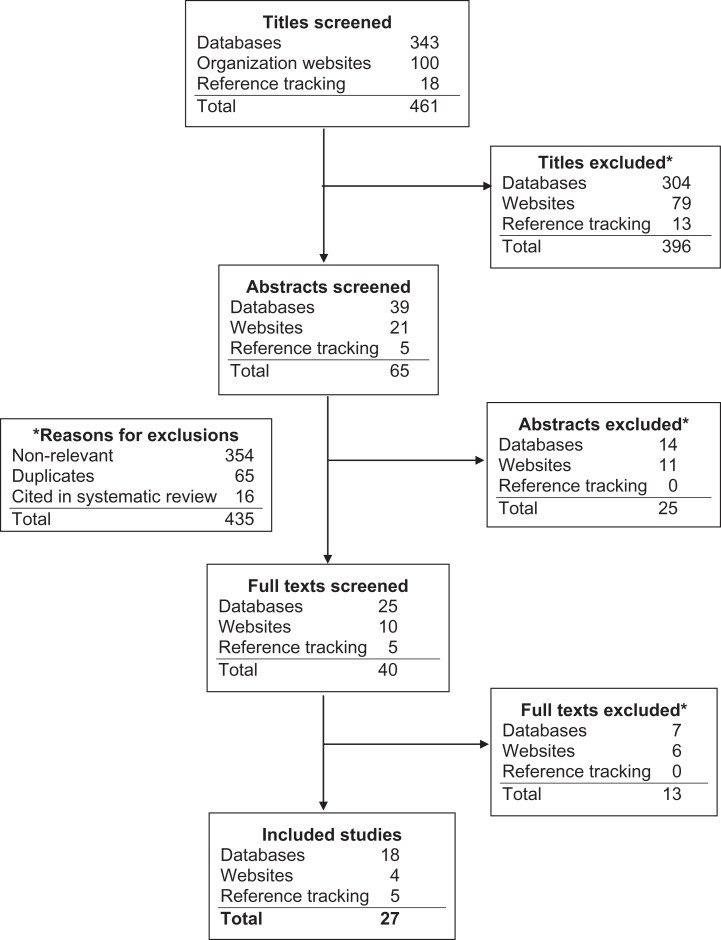
Figure 1 Figure 1 shows the results of the search and reasons for exclusions. The search yielded 461 articles, with a final inclusion of 27 articles for the review. Most of the exclusions made during screening (434 of 461) were made for nonrelevance to the research question. The types of studies represented in the final 27 were:
7 expert commentaries, [18, 31–36]
1 RCT, [37]
1 pilot study, [38]
1 cohort study, [39]
2 cross-sectional studies (surveys), [40, 41]
5 narrative reviews, [42–46] and
10 case reports/series. [47–56]Quality and Strength of Evidence

Table 4 Table 4 summarizes the level of evidence for the included studies. We identified 1 RCT; it was a high-quality, fully powered placebo-controlled study. [37] It had positive outcomes in terms of infants improving their ability to latch when compared with the sham (placebo) manipulation group. One low-quality cohort study [39] found that 25 infants with nursing dysfunction had more musculoskeletal issues, on physical examination, than 10 asymptomatic infants who successfully nursed. A proof-of-concept pilot study [38] with 6 infants found that chemical analysis of breast milk pre- and postosteopathic manual therapy showed improved fat content so that it closely resembled the composition of breast milk from successful mother-infant breastfeeding dyads.
Combining the 7 case reports [48–51, 53, 55, 56] and 3 case series [47, 52, 54] we identified with the 13 case reports and 5 case series described in the 3 included narrative reviews [42–44] on manual therapy for suboptimal breastfeeding, there were a total of 201 infants who received manual therapy for nursing dysfunctions. No serious adverse events were reported and improvement in nursing ability was observed using various outcome measures, usually maternal report.
Based on the GRADE criteria, the level of evidence is moderate, in a favorable direction, for the effect of manual therapy on suboptimal breastfeeding.
Clinical StudiesRandomized controlled trial The only RCT we identified was a high-quality, low risk of bias study. It investigated the efficacy of osteopathic treatment combined with lactation consultations for infants with biomechanical sucking difficulties. [37] Although the authors referred to it as a single-blind study, not only were the patients’ mothers successfully blinded to group status, but the lactation consultant who administered the primary outcome measure was also blinded. The primary outcome measure was the LATCH (Latch, Audible swallowing, Type of nipple, Comfort, Hold) tool, which is used by an expert observer to measure the biomechanical aspects of breastfeeding, including some factors related to the mother (see Table 4). Its interrater reliability is high, and it has been used to identify infants with sucking difficulties since 1994. A visual analog scale (VAS) for pain was used with the mothers to assess nipple pain. [37]
LATCH and the VAS were administered at baseline, prior to randomization and treatment, immediately after treatment, and 2 days later. The treatment consisted of a consultation by the lactation consultant and 1 osteopathic treatment (intervention group) or sham treatment (control group). At the conclusion of treatment, 60% of mothers of control group infants thought they were allocated to the intervention group, while 71% of mothers of infants in the intervention group thought they were allocated to the intervention group (P = .303).
LATCH improved significantly for infants in the intervention group, compared with the sham (control) group. Mothers’ nipple pain did not improve significantly, but this may have been due to the short time frame for measurement. [37]
Cohort study The only cohort study we identified was a retrospective cohort of low quality with high risk of bias. [39] It investigated the association of musculoskeletal dysfunction with suckling dysfunction by comparing the findings on a musculoskeletal examination of neonates with established nursing difficulties with those of neonates who successfully breastfed. Twenty-five infants aged 1 day to 3 months were referred for chiropractic care by health professionals because of suboptimal breastfeeding that had not responded to lactation consultation. Ten infants with successful breastfeeding skills presenting for “well baby” chiropractic care were given the same musculoskeletal examination. The same DC (Doctor of Chiropractic) did all the examinations and was not blinded to the infants’ nursing status.
Comparing the examination findings, the cohort with nursing difficulties had many more observed musculoskeletal irregularities of movement compared with the successful nursing group. These dysfunctions included restriction and/or deviation in mandibular excursion; hypertonicity of muscles involved in suckling and in turning the head; and movement restriction at the cervicocranial junction. [39]
Clinical pilot study We identified 1 pilot study investigating the change in fat content in breast milk after osteopathic treatment of 6 infants. [38] This small pilot study might be considered a proof-of-concept study. The fat content of breast milk can be measured reliably and simply through a centrifuge method; it is called the “creamatocrit.” [57] Because the hind milk (milk produced at the end of each nursing session) is much higher in fat content, the fat content of milk measured with normally feeding infants who completely drain the breast is considered the “gold standard.” [38] This pilot study found that the fat content of breast milk was low before osteopathic manual therapy, but increased so that it was comparable to the level considered normal after the treatment.

Table 5 Case Series and Case Reports We identified 10 case reports/series (7 case reports and 3 case series) which were not included in the narrative reviews identified in our search. Seven described chiropractic approaches, 2 osteopathic and 1 a lactation consultation. There were 2 case series with 2 patients in each (both twins). [47, 52] One of these described hospitalized premature twins who were unable to nurse. To avoid having to surgically place gastrostomy tubes for feeding, osteopathic physicians were consulted. Manual therapy consisting of soft tissue, balanced ligamentous tension, myofascial release, inhibition pressure, and osteopathy in the cranial field was applied. The twins’ nursing skills progressed until they were able to be discharged without gastrostomy tubes. The third case series described 11 infants with nursing dysfunction in whom the lactation consultant also noted musculoskeletal issues, particularly mandibular asymmetry; however, no treatment was administered. [54] Table 5 details both the 3 case series [47, 52, 54] and 7 case reports. [48–51, 53, 55, 56]
Narrative Reviews
Two narrative reviews discussed the literature addressing chiropractic care for nursing dysfunction [42, 44] and 1 narrative review, which was a thesis, covered general manual therapy and both chiropractic and osteopathic care for nursing dysfunction. [43] In all these reviews, the emphasis was on the effect of musculoskeletal/biomechanical factors on infants’ ability to suckle successfully. Two additional narrative reviews specifically addressed safety issues in manual treatment of infants. [45, 46]General Manual Therapy Approach In her 2015 thesis, Cornall summarized the basic theoretical approach of manual therapists, chiefly Beidermann, in Germany. [43, 58] This model is referred to as “kinematic imbalances due to suboccipital stress” (KISS) and is based on the developmental biomechanics of the infant’s spine, supporting musculature and associated neurological structures. It has been observed to be associated with “unsettled babies” as well as colic and nursing dysfunction. [43]
Osteopathic Approach The osteopathic literature summarized in 2015 by Cornall [43] was sparse and primarily descriptive and anecdotal. Three case reports and 1 clinical pilot study specifically addressing nursing difficulties were cited. “Osteopathy in the Cranial Field,” also called craniosacral therapy, is the primary osteopathic approach used in all the cited studies, although its basis is theoretical and anecdotal. [43]
Chiropractic Approach Two reviews, published by Alcantara et al [42] in 2015 and Fry [44] in 2014, included most of the same studies, for a combined total of 13 case reports and 5 case series. The cases included only chiropractic treatment of infants with nursing difficulties. Combined, the 5 case series had a total of 166 patients (sum of 2, [59] 6, [60] 19, [64] 25, [39] 114 [64]). Consequently, a total of 179 infants were treated with chiropractic care. In all the case reports and most of the case series, the patients’ suckling ability was observed to improve. A wide variety of commonly used manual procedures were applied, not only to the cervical spine and cranium (using cranial manipulation as developed and taught within the chiropractic profession by DeJarnette and Upledger63) but also to the entire spine, and to the supporting soft tissue structures as well. [42, 44]
Biomechanical Forces Used in Manual Therapies for Infants A review by Todd et al [45] summarized studies of the amount of biomechanical force used in chiropractic manual therapy of infants in terms of appropriateness and safety. European guidelines for chiropractic spinal manipulation of infants recommend low-force, low-speed manipulation that is 10% of the force (equivalent to 11.2 N of force) for infants up to 3 months of age and 30% of the force used for adults for infants and toddlers aged 3 to 23 months (equivalent to 33.6 N). Similar guidelines for different age groups were developed by Marchand et al, [64] based on(a) a study of tensile strength and osteoligamentous failure rates in pediatric spines and
(b) a report of transient bradycardia and apnea occurring in infants aged 3 months and younger, related to manual application of high-velocity, low-amplitude manipulation of 50-70 to 70 N. [65]To prevent possible adverse physiological effects — even if transient — Marchand et al [64] recommend that the maximum application of force for spinal manipulation should be 20 N for neonates and 50 N for children 2 to 23 months of age, compared with 155 N for adults.
Todd et al [45] state that many manual techniques used by DCs are similar to the manual therapies used by other providers. This includes osteopathic craniosacral therapy, which has been measured at a force of 1 N and spinal manipulation/mobilization performed by physical therapists, measured at a force of 22 N in adults. Medical manual therapists have been found to apply manual therapy to children using forces of 50 to 70 N. [45]
Adverse Events Related to Manual Therapy for Infants and Children Todd et al, [46] in another review, summarized the literature on adverse events in children related to use of manual therapy by any type of provider. Of the 12 articles yielded by their extensive search, an all-time total of 15 serious adverse events was reported. This included 3 deaths. In 1 of these 3 cases, a physical therapist applied electrical current therapy and spinal manipulation to a 3-month-old. In another case, a craniosacral therapist applied craniosacral therapy incorrectly. In the third case, an unspecified provider used spinal manipulation in a child with pneumonia, dislocating the first cervical vertebra. Twelve serious nonfatal injuries were reported to be caused by manual procedures delivered by 7 DCs, 2 physical therapists, 1 each by a medical, osteopathic and an unspecified practitioner. In most cases, high-velocity manipulation using extension and rotation of the spine was used. Preexisting pathology was present in most cases. The authors concluded that published cases of serious adverse events in infants and children due to manual therapies are rare. [46]
Cross-Sectional Descriptive SurveysPrevalence of Ankyloglossia in an Infant Population With Suboptimal Breastfeeding The mothers of 131 infants with suboptimal breastfeeding presenting to a chiropractic college teaching clinic were surveyed. Thirty-nine percent of the infants had been previously diagnosed with ankyloglossia and of these, 77% had had a frenulotomy. However, feeding difficulties had persisted. The study concluded that the diagnostic criteria for ankyloglossia may need clarification and that more research on sustained breastfeeding following frenulotomy is needed. [41]
Lactation Consultants’ Perceptions of Musculoskeletal Disorders Affecting Breastfeeding and Their Referrals for Manual Therapy IBCLCs were surveyed in the United States and Canada. Of 13,017 invited, 2,457 (18.9%) responded. Most (73.9%) reported referral of infants for musculoskeletal treatment. Pediatricians were the most common referral (47%), followed by craniosacral therapists (16%) and chiropractors (14%). Latch issues were the main reason for referral; tongue-tie (27%), painful latch (24%), neck problems (18%), and nonlatching (9%). Congenital torticollis (25%) and neck tension (14%) were the main musculoskeletal problems that the IBCLCs identified. About half the respondents felt they were able to recognize infant musculoskeletal problems. Ninety-one percent noted that breastfeeding improved after manual treatment. [40]
Expert Opinion/Commentaries
One expert commentary by an orthopedic medical physician who practices manual therapy [36] discussed the KISS theory in the context of infants’ sleeping and feeding problems. He explained that the occipitocervical junction (the joint between the occipital bone and the first cervical vertebra) is more vulnerable to excessive mobility in infants and young children due to the structural angle and less developed musculature. His clinical experience has demonstrated that realignment of the cervical joints is associated in improvement in a number of symptoms common in infants and young children. [36]
Three expert commentaries focused on chiropractic care for infants with musculoskeletal dysfunctions contributing to nursing dysfunction. [31–33] These detailed the examination of an infant for dysfunctional movement of the joints and muscles involved in latching and suckling, particularly related to the cervical spine, mandible and other cranial bones, and muscles of the neck and face. The importance of the cervicocranial junction was emphasized. They also emphasized the importance of interprofessional collaboration, particularly between the DC and the lactation consultant.
Two expert commentaries focused on osteopathic craniosacral therapy, also called “cranial osteopathy.” [34, 35] The commentary by Westcott [35] recounted the history of cranial osteopathy, which began in 1900, and was based on Sutherland’s observation of subtle movement of the cranial bones. Although his resultant theory on which cranial osteopathy is based has not been scientifically documented, Upledger [66] later argued that clinical results justify its use. Cranial manipulation for infants specifically was discussed by Upledger [66] as well as Sullivan, [67] with reference to the fact that the cranial bones are not fused in infants. [35] Westcott [35] explains that craniosacral therapy, another term for cranial osteopathy, is practiced by doctors of osteopathy (DOs), DCs, and other health care providers. In her commentary, Gray, [34] a midwife who practices craniosacral therapy, advocates this therapeutic approach “should be in every midwife and lactation consultant’s tool bag.” She also makes the connection between various musculoskeletal dysfunctions and tongue-tie, and echoed previously mentioned points that the condition is usually surgically corrected but may be associated with musculoskeletal issues which may prevent the infant from successful nursing even after the surgical repair. [34]
One expert commentary specifically addressed the issue of breastfeeding in infants with congenital torticollis. [18] This topic has broader implications, however, because torticollis is often (50% of cases) associated with intrauterine constraint and difficult births and may also result in craniofacial, hip and spinal asymmetries. The author recommends that the physical therapy to correct these asymmetries is most effective when applied in infants under four months of age, with fastest resolution occurring when applied at less than 1 month of age. [18] She states that although lactation consultants may recommend various types of bodywork for infants with torticollis, research on approaches other than physical or occupational therapy, such as chiropractic, are limited, and that such research is needed. [18] She has, in fact, included a chapter by a DC in the latest edition of her book, Supporting Sucking Skills in Breastfeeding Infants. [15, 63]
Discussion
This scoping review adds to the evidence base on one aspect of manual therapy for infants, a controversial topic that has even received attention on network television (http://www.abc.net.au/news/health/2016-06-20/newborn-chiropractic-care:where-is-the-evidence/7526116).
Previous literature reviews of the topic of manual therapy for infant musculoskeletal problems linked to suboptimal breastfeeding have been discipline specific and focused on using spinal manipulation as the primary treatment. [42, 44] Relevant information about similar procedures and assessments used by other manual therapy professions remains unshared and unknown. Therefore, we searched literature that was oriented toward both chiropractic and osteopathic medicine because the two professions are most closely associated with spinal manipulation and use other manual therapies. We also searched websites of organizations that focus on infants with breastfeeding issues associated with the compensatory musculoskeletal problems resulting from congenital anomalies like ankyloglossia. Casting this wide net resulted in a surprisingly large number of articles and a higher quality of evidence than we anticipated.
Limitations of the Study
Because scoping reviews are often used to explore an emergent topic, the quality and quantity of the evidence tends to be lower than it is for well-researched topics, making definitive conclusions inappropriate. Often, scoping reviews do not assess the quality of the included literature, for this reason. However, we decided to offset this limitation by evaluating any randomized controlled trials, cohort studies or systematic reviews identified. Another limitation is that we may have missed some studies, particularly because our search covered several different disciplines. We attempted to mitigate this through using reference tracking in key articles. Another inherent limitation in the broad approach is that there was diversity in the procedures and terminology used, making comparisons difficult or impossible.
Key FindingsRelationship of Musculoskeletal Dysfunction to Suboptimal Breastfeeding Although the procedures for conducting musculoskeletal examinations were often unspecified in the articles, several general sites of musculoskeletal dysfunction were pervasive throughout: the cervicocranial junction, cranial bones, mandible, upper cervical spine and neck muscles, especially the sternocleidomastoid. However, the effect of any of these dysfunctions on breastfeeding success remains theoretical, based on the biomechanics of suckling. Correlation between resolution of musculoskeletal dysfunction and improved nursing was seldom attempted, with the exception of the single cohort study included. [39] Developing general protocols for these examinations, and assessment of intra- and interrater reliability would facilitate future controlled studies.
Measures of Successful and Unsuccessful Breastfeeding Most of the case reports and series relied on mothers’ report and/or doctors’ observation. A few studies attempted to develop standardized mother-reported questionnaires, [61, 62] but these have yet to be fully validated. In one of these, [62] exclusive breastfeeding was one of the recorded outcomes. Although this is, in fact, the ultimate goal of the musculoskeletal interventions investigated, breastfeeding is a complex activity that includes both maternal and infant factors. Thus, a measurement that isolates the musculoskeletal factor is necessary in order to assess the effect of these interventions. The single RCT in our review used what is considered to be a reliable and valid outcome measure, the LATCH tool. [37] However, even LATCH has been found by others to lack sensitivity to change, [68] and it also measures maternal factors as well as infant factors, which decreases its utility in measuring only infant factors. One 1998 pilot study identified the “creamatocrit” as a way to accurately measure fat content of breast milk, which can be used as a surrogate measure of successful latching/suckling. [38] However, although a more user-friendly instrument than the original centrifuge method has been developed, [69] it does not appear that this method has been used in other studies of suboptimal breastfeeding. Further testing of this method may be warranted.
Blinded Assessment Only one of all the articles, the RCT, blinded the person conducting the measure to the infants’ treatment status. [37] Without this crucial feature, it will be very difficult, if not impossible, to rule out placebo effects related to the doctor’s attention, the hands-on treatment, and possible rater bias.
Common Terminology Among Disciplines As the importance of interprofessional practice and collaboration continues to grow, discipline-specific terminology must give way to common terminology understood by all related disciplines. [70] Collaborative research among various types of manual therapists as well as with any providers who work with pregnant women and infants could greatly enhance research productivity rather than remaining in their respective research silos.
Safety Issues Related to Manual Interventions A 2015 review concluded that adverse events caused by manual interventions with children are rare. [46] A 2018 systematic review of manual interventions for infants in particular found that the risk of nonserious adverse events was low. [71] It is nevertheless important to maximize the safety of infants receiving manual care. In most of the articles in this review, authors did not state whether or not there were any adverse effects. It would be helpful if future studies and case reports would explicitly state whether there were any adverse effects, even minor ones. Currently, a surveillance system is being developed by chiropractors to gather data on adverse events among pediatric chiropractic patients. [72]
The 2016 review of biomechanical forces used in manual interventions with infants and children made recommendations based on international consensus among DCs, and included some information about forces used by other manual therapists. [45] A more recent study went further into this topic by measuring biomechanical forces with the aid of sophisticated force-sensing technology and manikins, delivered by a highly experienced DC who specializes in treating infants. [73]
The authors found that the DC was in fact capable of modifying biomechanical forces to accommodate an individual patient’s needs, and that the forces were similar to those recommended by the international consensus of DCs. [45, 64] Currently, most chiropractic educational institutions in North America have instituted the use of “force-sensing table technology” — the equipment used in the 2017 study cited above — to train students in spinal manipulation. [74, 75] Additionally, the chiropractic profession has developed a set of “best practices” recommendations for the chiropractic treatment of children, which recommends additional examination, treatment, and referral practices to safeguard pediatric patients. [76]
Conclusion
Because breastfeeding is a significant public health issue, exploring ways to increase its prevalence and success is important. This scoping review found that there is a moderate level of favorable evidence supporting the use of manual interventions for infants with musculoskeletal dysfunctions and suboptimal breastfeeding. Coupled with the rarity of adverse events noted for manual treatment of infants and children, additional controlled studies of this topic are warranted.
Author Contributions:
CH contributed toward design, data collection and analysis, writing, and review.
AM was involved with data analysis, writing, and review.
CW performed the literature search and as involved with writing and review.
OH contributed toward data analysis, writing, and review.
SV contributed toward design, writing, and review.
Declaration of Conflicting Interests:
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding:
The authors received no financial support for the research, authorship, and/or publication of this article.
REFERENCES:
Bartick MC, Schwarz EB, Green BD, et al.
Suboptimal breastfeeding in the United States:
maternal and pediatric health outcomes and costs.
Matern Child Nutr. 2017;13Section on Breastfeeding, American Academy of Pediatrics.
Breastfeeding and the use of human milk.
Pediatrics. 2012;129:e827–e841ACOG Committee Opinion No. 756:
optimizing support for breastfeeding as part of obstetric practice.
Obstet Gynecol. 2018;132:e187–e196Association of Women’s Health, Obstetric and Neonatal Nurses.
AWHONN Position Statement: Breastfeeding. Washington DC:
Association of Women’s Health, Obstetric and Neonatal Nurses; 2015US Preventive Services Task Force.
2014 Guide to Clinical Preventive Services.
Washington, DC: Agency for Healthcare Research and Quality; 2014World Health Organization;
UNICEF Tracking Progress for Breastfeeding Policies and Programmes:
Global Breastfeeding Scorecard 2017.
Geneva, Switzerland: World Health Organization; 2017Bartick M, Reinhold A.
The burden of suboptimal breastfeeding in the United States: a pediatric cost analysis.
Pediatrics. 2010;125:e1048–e1056Centers for Disease Control and Prevention.
Breastfeeding Report Card, United States 2016
Atlanta, GA: Centers for Disease Control and Prevention; 2016Centers for Disease Control and Prevention.
National immunization surveys (NIS).
https://www.cdc.gov/vaccines/imz-managers/nis/index.html
Accessed November 15, 2018.Victora CG, Bahl R, Barros AJ, et al.
Lancet Breastfeeding Series Group. Breastfeeding in the 21st century:
epidemiology, mechanisms, and lifelong effect.
Lancet. 2016;387:475–490Rollins NC, Bhandari N, Hajeebhoy N, et al.
Lancet Breastfeeding Series Group. Why invest, and what it will take
to improve breastfeeding practices?
Lancet. 2016;387:491–504Dunn RL, Kalich KA, Henning MJ, Fedrizzi R.
Engaging field-based professionals in a qualitative assessment of barriers
and positive contributors to breastfeeding using the social ecological model.
Matern Child Health J. 2015;19:6–16US Department of Health and Human Services.
Healthy People 2020. 2nd ed
Washington DC: US Government Printing Office; 2020International Lactation Consultant Association.
Standards of Practice for International Board Certified Lactation Consultants.
Morrisville, NC: International Lactation Consultant Association; 2013Genna CW, ed.
Supporting Sucking Skills in Breastfeeding Infants., 3rd ed
Burlington MA: Jones & Bartlett; 2017.Marmet C, Shell E.
Therapeutic positioning for breastfeeding
In: Genna CW, ed. Supporting Sucking Skills in Breastfeeding Infants.
Burlington, MA: Jones & Bartlett; 2017:399–416.Coryllos E, Genna CW, Fram JL.
Minimally invasive treatment for posterior tongue-tie (the hidden tongue-tie)
In: Genna CW, ed. Supporting Sucking Skills in Breastfeeding Infants.
Burlington, MA: Jones & Bartlett; 2017:269–278.Genna CW.
Breastfeeding infants with congenital torticollis.
J Hum Lact. 2015;31:216–220.Ghaheri BA, Cole M, Fausel SC, Chuop M, Mace JC.
Breastfeeding improvement following tongue-tie and lip-tie release:
a prospective cohort study.
Laryngoscope. 2017;127:1217–1223.O’Callahan C, Macary S, Clemente S.
The effects of office-based frenotomy for anterior and posterior ankyloglossia on breastfeeding.
Int J Pediatr Otorhinolaryngol. 2013;77:827–832.Tamura Y, Matsushita S, Shinoda K, Yoshida S.
Development of perioral muscle activity during suckling in infants:
a cross-sectional and follow-up study.
Dev Med Child Neurol. 1998;40:344–348.Bu Lock F, Woolridge MW, Baum JD.
Development of co-ordination of sucking, swallowing and breathing:
ultrasound study of term and preterm infants.
Dev Med Child Neurol. 1990;32:669–678.Genna CW, Sandora L.
Breastfeeding: normal sucking and swallowing
In: Genna CW, ed. Supporting Sucking Skills in Breastfeeding Infants.
Burlington, MA: Jones & Bartlett; 2017:1–48.Genna CW.
The influence of anatomical and structural issues on sucking skills
In: Genna CW, ed. Supporting Sucking Skills in Breastfeeding Infants.
Burlington, MA: Jones & Bartlett; 2017:209–268.Colquhoun HL, Levac D, O’Brien KK, et al.
Scoping reviews: time for clarity in definition, methods, and reporting.
J Clin Epidemiol. 2014;67:1291–1294.Arksey H, O’Malley L.
Scoping studies: towards a methodological framework.
Int J Soc Res Methodol. 2005;8:19–32.Wambach K, Riordan J.
Breastfeeding and Human Lactation. 5th ed
Burlington, MA: Jones & Bartlett; 2016.Harbour R, Lowe G, Twaddle S.
Scottish Intercollegiate Guidelines Network: the first 15 years (1993-2008).
J R Coll Physicians Edinb. 2011;41:163–168.Hawk C, Minkalis AL, Khorsan R, et al.
Systematic Review of Nondrug, Nonsurgical Treatment of Shoulder Conditions
J Manipulative Physiol Ther 2017 (Jun); 40 (5): 293–319Guyatt GH, Oxman AD, Vist GE, et al.
GRADE: An Emerging Consensus on Rating Quality of Evidence
and Strength of Recommendations
British Medical Journal 2008 (Apr 26); 336 (7650): 924–926Tow J, Vallone SA.
Relationship in the care of the breastfeeding newborn:
lactation consultant and chiropractor.
J Clin Chiropr Pediatr. 2009;10:626–632.Vallone SA, Carnegie-Hargreaves F.
The Infant with Dysfunctional Feeding Patterns –
The Chiropractic Assessment
J Clinical Chiropractic Pediatrics 2016 (May); 15 (2): 1230Vallone S.
Evaluation and Treatment of Breastfeeding Difficulties Associated with
Cervicocranial Dysfunction: A Chiropractic Perspective
Journal of Clinical Chiropractic Pediatrics 2016 (Dec); 15 (3): 1301–1306Gray C.
20+ years of infant craniosacral therapy practice.
Midwifery Today Int Midwife. 2015:16–19.Westcott N.
Use of cranial osteopathy in the treatment of infants with breast feeding problems
or sucking dysfunction.
Aust J Holist Nurs. 2004;11:25–32.Biedermann, H.
Manual Therapy in Children: Proposals for an Etiologic Model
J Manipulative Physiol Ther 2005 (Mar); 28 (3): e1–e15Herzhaft-Le Roy J, Xhignesse M, Gaboury I.
Efficacy of OMT with lactation consultations for biomechanical sucking difficulties.
J Hum Lact. 2017;33:165–172.Fraval M.
A pilot study: osteopathic treatment of infants with a sucking dysfunction.
Am Acad Osteopath J. 1998;8:25–33.Vallone S.
Chiropractic Evaluation and Treatment of Musculoskeletal Dysfunction
in Infants Demonstrating Difficulty Breastfeeding
J Clinical Chiropractic Pediatrics 2004 (Dec); 6 (1): 349–366Lavigne V.
Lactation consultants’ perceptions of MSK disorders affecting breastfeeding:
cross-sectional survey.
Clin Lact. 2016;7:30–36.Miller A, Miller JE.
Is tongue tie really the problem? Incidence of ankyloglossia in an
infant population presented with suboptimal feeding: a cross-sectional survey.
J Clin Chiropr Pediatr. 2017;16:1350–1354.Alcantara J, Alcantara JD, Alcantara, JU.
The Chiropractic Care of Infants with Breastfeeding Difficulties
Explore (NY) (Nov) 2015; 11 (6): 468–474Cornall D.
Promoting Optimal Breastfeeding Through the Osteopathic Therapeutic Cycle.
Footscray, Victoria, Australia: Victoria University; 2015.Fry LM.
Chiropractic and Breastfeeding Dysfunction: A Literature Review
Journal of Clinical Chiropractic Pediatrics 2014 (Mar); 14 (2): 1151-1155Todd AJ, Carroll MT, Mitchell EK.
Forces of Commonly Used Chiropractic Techniques for Children:
A Review of the Literature
J Manipulative Physiol Ther. 2016 (Jul); 39 (6): 401–410Todd AJ, Carroll MT, Robinson A, Mitchell EK.
Adverse Events Due to Chiropractic and Other Manual Therapies for Infants and Children:
A Review of the Literature
J Manipulative Physiol Ther. 2015 (Nov); 38 (9): 699–712Collins K, Alcantara J, Holt K.
Resolution of breastfeeding and gastrointestinal complaints in infant twins
with plagiocephaly and scaphocephaly following birth trauma: a case series.
J Pediatr Matern Fam Health. 2015;1:34–41.Drobbin E, Stallman J.
Resolution of breastfeeding and latching difficulty following subluxation based
chiropractic care: case report and review of literature.
J Pediatr Matern Fam Health Chiropr. 2015;3:102–108.Ferranti M, Alcantara J, Adkins M.
Resolution of breastfeeding difficulties and plagiocephaly in an infant
undergoing chiropractic care.
J Pediatr Matern Fam Health Chiropr. 2016;2:42–45.Hubbard M.
Pediatric cholelithiasis and breastfeeding difficulties:
a chiropractic case report.
J Clin Chiropr Pediatr. 2014;14:1144–1150.Lavigne V.
A narrative review and case report: frenotomy procedure in neonate with tongue-tie.
J Clin Chiropr Pediatr. 2012;13:1025–1031.Lund GC, Edwards G, Medlin B, Keller D, Beck B, Carreiro JE.
Osteopathic manipulative treatment for the treatment of hospitalized
premature infants with nipple feeding dysfunction.
J Am Osteopath Assoc. 2011;111:44–48.Tutt G, Mesidor RG.
Resolution of torticollis, plagiocephaly and breastfeeding difficulties
in an infant following subluxation based chiropractic care.
J Ped Mat Fam Health - Chiropr. 2014;2:14–20.Wall V, Glass R.
Mandibular asymmetry and breastfeeding problems: experience from 11 cases.
J Hum Lact. 2006;22:328–334.Williams S.
Improvement of congenital torticollis, plagiocephaly and breastfeeding issues
in an infant following subluxation based chiropractic care: a case study.
J Pediatr Matern Fam Health Chiropr. 2014;4:87–94.Summers J, Ludwig J, Kanze D.
Pierre robin sequence in a neonate with suckling difficulty and weight loss.
J Am Osteopath Assoc. 2014;114:727–731.Lucas A, Gibbs JA, Lyster RL, Baum JD.
Creamatocrit: simple clinical technique for estimating
fat concentration and energy value of human milk.
Br Med J. 1978;1:1018–1020.Biedermann H.
Kinematic imbalances due to suboccipital strain in newborns.
J Man Med. 1992;6:151–156.Hewitt E.
Chiropractic care for infants with dysfunctional nursing: a case series.
J Clin Chiropr Pediatr. 1999;4:241–244.Marchand A, Miller J, Mitchell C.
Diagnosis and Chiropractic Treatment of Infant Headache Based on Behavioral Presentation
and Physical Findings: A Retrospective Series of 13 Cases
J Manipulative Physiol Ther. 2009 (Oct); 32 (8): 682–686Stewart A.
Pediatric chiropractic and infant breastfeeding difficulties:
a pilot case series study involving 19 cases.
Chiropr J Aust. 2012;42:98–107.Miller, J. E., Miller, L., Sulesund, A. K., & Yevtushenko, A.
Contribution of Chiropractic Therapy to Resolving Suboptimal Breastfeeding:
A Case Series of 114 Infants
J Manipulative Physiol Ther 2009 (Oct); 32 (8): 670–674Vallone SA.
Hands in support of breastfeeding: manual therapy
In: Genna CW, ed. Supporting Sucking Skills in Breastfeeding Infants. 3rd ed
Burlington, MA: Jones & Bartlett; 2017:279–308.Marchand AM.
A Proposed Model With Possible Implications for Safety and
Technique Adaptations for Chiropractic Spinal Manipulative
Therapy for Infants and Children
J Manipulative Physiol Ther 2015 (Nov); 38 (9): 713–726Koch LE, Koch H, Graumann-Brunt S, Stolle D, Ramirez JM, Saternus KS.
Heart rate changes in response to mild mechanical irritation of
the high cervical spinal cord region in infants.
Forensic Sci Int. 2002;128:168–176.Upledger JE.
Craniosacral therapy.
Phys Ther. 1995;75:328–330.Sullivan C.
Introducing the cranial approach in osteopathy and the treatment of infants and mothers.
Complement Ther Nurs Midwifery. 1997;3:72–76.Ingram J, Johnson D, Copeland M, Churchill C, Taylor H.
The development of a new breastfeeding assessment tool and the
relationship with breast feeding self-efficacy.
Midwifery. 2015;31:132–137.Meier PP, Engstrom JL, Zuleger JL, et al.
Accuracy of a user-friendly centrifuge for measuring creamatocrits
on mothers’ milk in the clinical setting.
Breastfeed Med. 2006;1:79–87.Rogers GD, Thistlethwaite JE, Anderson ES, et al.
International consensus statement on the assessment of interprofessional learning outcomes.
Med Teach. 2017;39:347–359.Carnes D, Plunkett A, Ellwood J, Miles C.
Manual Therapy for Unsettled, Distressed and Excessively Crying Infants:
A Systematic Review and Meta-analyses
BMJ open. 2018 (Jan 224); 8 (1): e019040Pohlman KA, Carroll L, Tsuyuki RT, Hartling L, Vohra S.
Active versus passive adverse event reporting after pediatric chiropractic
manual therapy: study protocol for a cluster randomized controlled trial.
Trials. 2017;18:575.Triano JJ, Lester S, Starmer D, Hewitt EG.
Manipulation peak forces across spinal regions for children using mannequin simulators.
J Manipulative Physiol Ther. 2017;40:139–146.Stainsby BE, Clarke MC, Egonia JR.
Learning spinal manipulation: a best-evidence synthesis of teaching methods.
J Chiropr Educ. 2016;30:138–151.Triano J, Giuliano D, McGregor M, Howard L.
Enhanced Learning of Manipulation Techniques Using Force-Sensing Table Technology (FSTT).
Toronto, Ontario, Canada: Higher Education Quality Council of Ontario; 2014.Hawk C, Schneider MJ, Vallone S, Hewitt EG.
Best Practices for Chiropractic Care of Children: A Consensus Update
J Manipulative Physiol Ther. 2016 (Mar); 39 (3): 158–168
Return to PEDIATRICS
Return to WOMEN's HEALTH
Return to the FEMALE ISSUES
Since 10-10-2021


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |