A Comprehensive Review
of Chiropractic ResearchThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




By Anthony L. Rosner, Ph.D., LL.D.[Hon.], LLC
]
Director of Research and Education for the Foundation for Chiropractic Education
and Research (FCER) until its demise (1992-2007), and current Director of Research
at International College of Applied Kinesiology (USA).
I. Introduction A. Perspectives B. First Major Interdisciplinary Cohort Study C. Endorsements in Back Pain Care by Government Agencies II. The State of Evidence-Based Practice A. Definitions of EBM B. Limitations of EBM and Transformation to "Evidence-Informed" III. Basic Research A. Importance of Test Organisms B. Anatomy C. Biomechanics D. Neurology E. Hormones F. Inflammation IV. Outcomes Research A. Methods of Measurement B. Musculoskeletal 1. Back Pain Research a. The RAND Appropriateness and Utilization Study b. Comparisons with Acupuncture, NSAIDs, Muscle Relaxants 2. Neck Pain Research a. The RAND Appropriateness Study b. Other Studies c. Whiplash Research 3. Headache Research a. Tension Headache b. Cervicogenic Headache c. Migraines and Unclassified Headaches: d. Pediatric Headache e. Basic Research: The Myo-Dural Bridge f. The Duke Headache Evidence Report 4. Extremities a. Upper Extremities b. Lower Extremities C. A Non-musculoskeletal 1. Observed as a "By-product" 2. Infantile Colic 3. Enuresis 4. Asthma 5. Dysmenorrhea/Premenstrual Syndrome 6. Otitis Media 7. Heart Rate Variability 8. Hypertension 9. Case Study Support D. Cognitive Changes V. Safety A. Major Complications: Relative Risks of Activities B. Study of the Vertebral Artery and Artery Wall 1. Structural Considerations 2. Mechanisms of Dissection 3. Role of Homocysteine C. Linking Cerebrovascular Accidents to Manipulation 1. Risk Factors 2. Other Adverse Events 3. Flaws in the Medical Literature VI. Cost-Effectiveness Research A. Rationale B. Methodological Concerns C. Leading Types of Studies 1. Workers' Compensation Data 2. Databases from Insurers and Practitioners D. An Economist's Evaluation of the Literature VII. Wellness and Prevention A. Significance in Healthcare Delivery B. Recent Research VIII. Conclusions References The Data Tables
I. Introduction
A. Perspectives:
In the space of just 115 years from its inception, chiropractic has emerged as the third largest healthcare profession in the United States offering diagnostic as well as therapeutic services to patients. It has reached this lofty height driven by research which has made particularly dramatic strides over the past 30 years, supported by a budget which represents merely an infinitesimal fraction of that applied to medical and pharmaceutical research.
Like all health professions, chiropractic regularly tests the effectiveness, safety, and costs of its approaching health care. Studies continue to show that chiropractors offer the public a viable alternative to invasive healthcare (drugs, surgery) especially in the treatment of musculoskeletal problems such as back, neck, and headache pain. But chiropractic treatments are likewise effective in the treatment of non-musculoskeletal health issues, including infantile colic, enuresis, asthma, dysmenorrheal, otitis media, hypertension, and heart rate variability. And few medical professions outside of chiropractic can offer such healthcare solutions with equal safety and cost records.
Having been historically been placed in the category of alternative and complementary medicine, chiropractic because of its rapid growth in its research has now been deemed to have reached the crossroads of mainstream and alternative medicine. [1] As a hybrid, it appears to have successfully incorporated many of the research methodologies of orthodox medicine while striving to maintain its distinct healthcare paradigm. Indeed, when the practitioners primary means of patient care and published randomized clinical trials supporting that intervention are matched, chiropractic can be shown to enjoy a higher percentage of interventions thus supported when compared to such other medical disciplines as general practice, inpatient general surgery, dermatology, or hematology-oncology. [2] In other words, chiropractic can now claim to have attained at least as much of a scientific grounding as other medical interventions based upon its research.
So what is it that one means by chiropractic research? The research related to the practice of chiropractic, to be reviewed in this chapter, has been presented in multiple dimensions, including:1. Published clinical articles;
2. Literature reviews;
3. Surveys and public opinion research;
4. Analyses of insurance claims [actuarial research]; and
5. Guidelines
B. First major interdisciplinary cohort study:
One of the first lines of evidence in support of chiropractic intervention that could be considered to be more robust came in 1985 from a prospective observational study of 283 patients suffering from chronic low back and leg pain, drawn from a university back pain clinic reserved for patients who had not responded to previous conservative or operative treatment. Given a 23 week regimen of daily spinal manipulation by an experienced chiropractor, 81% of these patients with referred pain and 48% of those with nerve compression displayed improvements in pain grades after their assessments at 1 month followed by 3month intervals. The research was noteworthy in that it represented a collaboration between chiropractic [David Cassidy] and medical providers [William Kirkaldy-Willis] and was published in a leading medical journal. [3
C. Endorsements in back pain care by government agencies:
In 1979, just four years after chiropractic research received its assessment from the historic NINDS Conference, extensive investigations in 1979 by the Commission of Inquiry in New Zealand of chiropractic in the United States, Canada, United Kingdom and Australia as well as New Zealand culminated in the release of a report which concluded that modern chiropractic is a soundly-based and valuable branch of health care in a specialized area neglected by the medical profession." [4] Some thirty years later, it was evident from the extent and quality of chiropractic research that dramatic changes were in evidence. Regarding back pain as assessed by government agencies in the:U.S., [5]
Canada, [6]
Great Britain, [7]
Sweden, [8]
Denmark, [9]
Australia, [10] and
New Zealand, [11]One could argue that chiropractic care appears have vaulted from last place to first as a treatment option for musculoskeletal disorders.
For example, according to the assessment of back pain treatment by a U.S. government agency, the Agency for Health Research and Quality [formerly the Agency for Health Care Policy and Research], the strength of the evidence found to support manipulation was rated sufficiently highly to place this intervention as one of two leading options [together with the use of analgesics and nonsteroidal anti-inflammatory drugs [NSAIDs] to be considered from 27 different types of interventions reviewed. [5] The comparative gradings of evidence supporting each of these interventions are displayed in TABLE 1 (shown below the References Section), in which spinal manipulation was only one of two options found to have a positive effect with as high as a B grade. The British guidelines lauded that there is considerable evidence that manipulation can provide short-term symptomatic benefits in certain patients, [7] while the Danish report echoed this sentiment by declaring that manual treatment can be recommended for patients suffering from acute low-back symptoms and functional limitations of more than 23 days duration. [9]
II. The State of Evidence-Based Practice
A. Definitions of EBM:
Evidence-based medicine [EBM] was introduced as a term to denote the application of treatment that has been proven and tested in a rigorous manner to the point of its becoming 'state of the art.' [12] Its intention has been to ensure that the information upon which doctors and patients make their choices is of the highest possible standard. [13] To reach a clinical decision based upon the soundest scientific principles, EBM proposes five steps for the clinician to follow as shown in TABLE 2. [14]
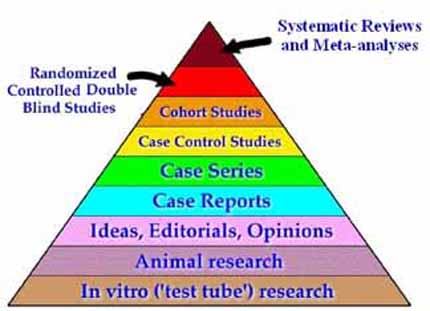
Step 2 [accessing the best evidence] customarily follows a totemic relationship of the available designs of clinical research, shaped as a pyramid and shown in FIGURE 1. [15]
Here it is evident that systematic reviews and meta-analyses occupy the rarefied top echelon, followed by randomized controlled double blind studies [RCTs] and thence by cohort studies, case control studies, case series, and case reports. It is only at the second rung from the bottom that one discloses what is presumed to be the lowly category of animal research. This is clearly an absurd finding, the ramifications of which will be discussed below in Section IIIA.
It is also apparent in Step 4 of TABLE 2 that there has been a greening of the original concepts of simply rating evidence by the paint-by-the-numbers approach of simply grading the evidence of published research papers. For here the epidemiologist David Sackett has made clear that such realities as patient subgroups and comorbidities play a major role in therapeutic decisions, such that clinical judgment becomes recognized as significant as well: [16][EBM] means integrating individual clinical expertise with the best available external clinical evidence from systematic research. By individual clinical expertise we mean the proficiency and judgment that we individual clinicians acquire through clinical experience and clinical practice. By best available external clinical evidence we mean clinically relevant research, often from the basic sciences of medicine, but especially from patient centered clinical research into the accuracy and precision of diagnostic tests [including clinical examination], the power of prognostic markers, and the efficacy and safety of therapeutic, rehabilitative, and preventive regimens. Good doctors use both individual clinical expertise and the best available external evidence, and neither alone is enough [emphasis added]. Without clinical expertise, practice risks becoming tyrannized by external evidence, for even excellent external evidence may be inapplicable to or inappropriate for an individual patient. Without current best external evidence, practice risks becoming rapidly out of date, to the detriment of patients.
STEP PROCESS 1. Converting the need for information [about prevention, diagnosis, prognosis, therapy, causation, etc.] into an answerable question [Also known as formulating a clinical question]. 2. Finding the best evidence with which to answer that question. 3. Critical appraisal of the research evidence for validity, impact, and application. 4. Integration of the critically appraised research evidence with the expertise of the practitioner and the patient's unique biology, values and circumstances. 5. Evaluating the effectiveness of the process in improving patient care and practitioner efficiency in executing steps #14 and seeking ways to improve both.
B. Limitations of EBM and Transformation to "Evidence-Informed" Best Practices:
Figure 1: The Hierarchy of Clinical Evidence [15]
Cracks in the foundation of one of the strongest pillars of conventional definitions of EBM based upon the pyramid shown in FIGURE 1 began to appear in the 1980s, when the quality of observational [cohort, case series] studies was found to improve, such that their predictive value in clinical situations could now be compared to that seen in the more rigorous RCTs. [17, 18]
At the same time, RCTs began to be seriously challenged due to their limited applicability in clinical situations. [19, 20] Among other problems, RCTs were found to lack insight into lifestyles, nutritional interventions, and long-latency deficiency diseases. [21] Quirks have likewise surfaced which demonstrate how even the exalted meta-analysis is subject to human error and bias. [22]
In addition to factoring in the judgment of the clinician to EBM, effective patient care requires, in the final analysis, the attributes of the actual patient. Such patient-based outcome measures as the Health Related Quality of Life Index and cost-effectiveness will continue to grow as elements which cannot be ignored in EBM. Indeed, it has been argued that “the most compelling and growing” component of EBM is the empowerment of the patient in the decision-making process. [23] With patients being the best judge of values, clinical decisions are becoming recognized as necessarily shared between the patient and clinician. [24]
This shifting of the EBM sands echoes what a few years ago appeared to be a revolutionary upheaval suggested by Wayne Jonas, who presented what appeared to be for all intents and purposes a virtual inversion of the classical evidence pyramid.
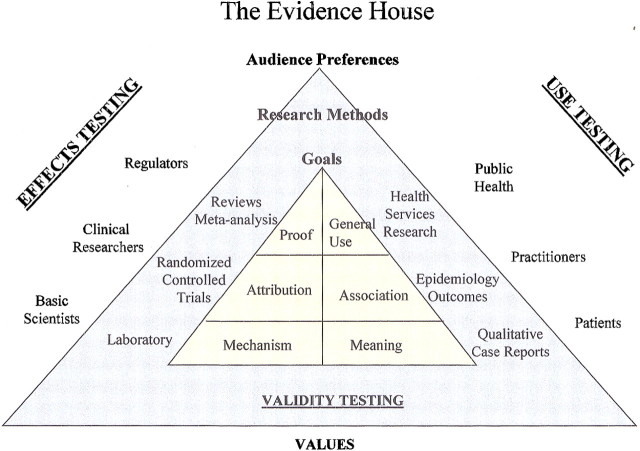
Figure 1.5: The Evidence House Affords Greater Accessibility To Important Information [25]
In Jonas' presentation of the “Evidence House”, such entities as use testing, public health, and audience preferences gained ascendancy. [25]
Despite all these revisions, these upgrades of EBM have not been able to outrun all of the most severe critics of EBM. When EBM is applied in a unilateral, heavy-handed manner, it has run the risk of becoming a “regime of truth” in such a manner as to discourage free inquiry.
Put in other terms, it is questionable whether many current models of EBM promote the multiple ways of knowing considered to be important in most health disciplines, [26] falling under a spell which Foucault has referred to as a “clinical gaze.” [27]
For these reasons, proponents of EBM have fallen back to a position in which the best evidence is now considered to guide or inform rather than mandating a clinical decision. [28, 29]
III. Basic Research
A. Importance of Test Organisms:
The two key reasons for seeking a test organism in research are that:[i] it presents a simplified picture of an area of interest, maintaining its essential features; and
[ii] it lends itself to experimental manipulations which are more difficult or impossible in the more complex [usually human] arena. One prominent feature and advantage of the test organism is that it allows direct examination of living tissues, shedding further light upon complex biological interactions.According to Howard Vernon, animal models as a class of test organisms enable the investigator to: [30]
1. Test theories derived from conceptual models.
2. Provide data to support clinical experience.
3. Apply a high degree of experimental control.
4. Explore cause and effect relationships from prospective studies.
5. Explore "treatment" effects when a lesion is reversed.
6. Explore physiologic components of subluxations.
7. Explore behavioral effects in chronic experiments.Medicine could not have developed without the use of test organisms. This would encompass everything from our understanding of genetic principles from the plants of Gregor Mendel or the bacteria on the Petri dishes of Alexander Fleming, Seymour Benzer, or Bruce Ames. It extends to the treatment of anthrax from the sheep of Louis Pasteur, the isolation of insulin by Banting and Best from dogs, and the identification of the conditioned reflex from Ivan Pavlov's dogs. Indeed, no less an authority than the British Royal Society of Medicine argues that virtually every major medical advancement of the 20th century relied upon the use of animals in some fashion. [31]
Chiropractic research is no exception. As Charles Henderson has so aptly pointed out, even the differences between animals and humans have opened the way to major discoveries essential for understanding basic concepts in neuroscience. [32] Thus giant squid axons that are 1001000 times larger than their mammalian counterparts have given researchers the opportunity to measure the ionic composition of neural cytoplasm and study changes in membrane potentials. [33] The eggs of the clawed African frog, Xenopus laevis, have allowed the development of patch clamp technique to study ionic currents generated by newly formed channels. [34] More recently, degenerative changes following spinal fixation that could be considered attributes of the subluxation have been identified in the rat. [35] This followed the groundbreaking experiments in the 1980s by Sato and Swenson who clearly identified changes in the sympathetic nervous system that followed mechanical stresses to the spinal column in rats. [36] And finally there has been a proliferation of data from Xue-Jun Song which have demonstrated the multifaceted analgesic effects of instrument-assisted manipulation [37] or the administration of the B-vitamins [38] in rats which have been subjected to neural injury. These are but a very few examples of the significant advances in our understanding of the physiological processes which attend human disorders and their alleviation through healthcare management.
B. Anatomy:
A key concept of chiropractic has consistently been the relationship between structure and function. That said, numerous investigations into the associations of spinal structures and neurons shed considerable light upon the possible mechanisms of the manipulative techniques of the spine specified in chiropractic healthcare, as well as the disorders that they were designed to treat.
Clinically significant relationships between spinal structures and neural elements could be deduced from the earlier surface cryoplaning technique described by Rauschning, whose observations of degenerative changes of the intervertebral foramina [IVF] revealed encroachments of the nerve root complex and radicular vessels upon extension and rotation of the specimen. [39] Transforaminal ligaments, shown to cause a significant decrease of IVF size, [40] were later identified as possible agents of nerve root entrapment. In the upper spine, overlapping connections between neurons in the neck and head and face provided a mechanism for the referral of upper cervical dysfunction to the head, offering a rationale for the chiropractic treatment of some cases of headache. [41]
Measuring the endoneural fluid pressure in the dorsal root ganglia of rats, Rydevik provided an explanation as to how pressure on the DRG could lead to radicular symptoms. [42] As far as linkages to back pain were concerned, a number of investigations by Bogduk and Groen described the innervation of the intervertebral disc [IVD in the lumbar region [43, 44] and the anterior and posterior longitudinal ligaments. [45]
A major pillar of chiropractic theory suggests that an essential component of the vertebral subluxation complex is the development of adhesions in the zygopophysial joints as the result of hypomobility which develops in these structures, [46, 47] and that spinal manipulation would be capable of breaking up these fixations in a process known as "gapping." [48, 49] The finding by Cramer and his colleagues that gapping did indeed occur in healthy volunteers subjected to spinal manipulation [50, 51] therefore provided noteworthy support to this aspect of chiropractic theory.
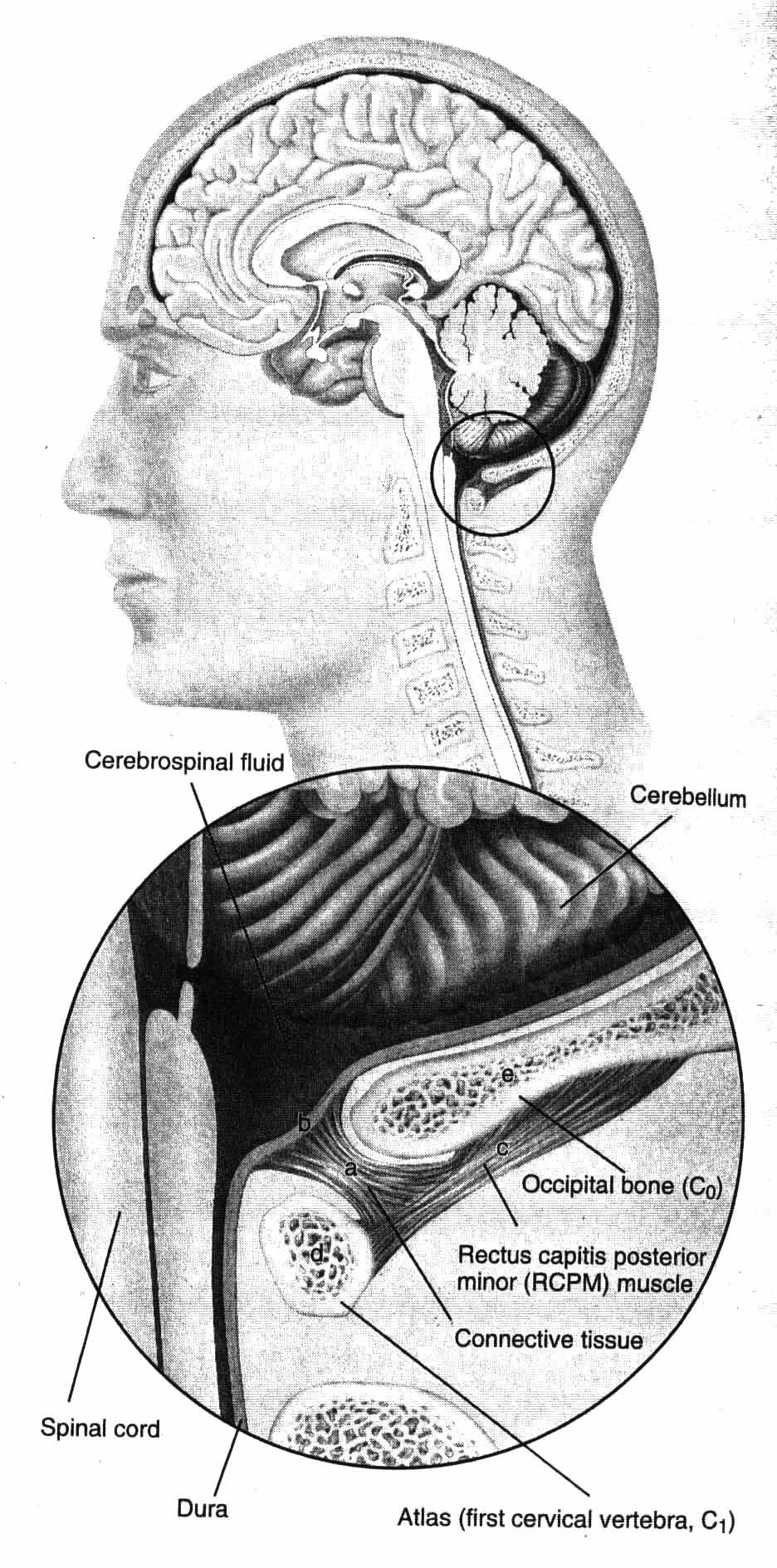
Another productive line of inquiry regarding anatomical components of the spine involves connective tissue attachments to the spinal dura mater. The posterior aspect of the spinal dura appears to be anchored by bridges from the foramen magnum, posterior arch of C1, spinous process of C2, [52] the rectus capitus posterior minor muscle, [53] the ligamentum nuchae, [54] and the ligamenta flava between C1C2 and C6C7. [55] All these attachments are proposed to retain the dura mater posteriorly during cervical extension [to prevent buckling of the dura mater into the spinal cord] and flexion [to prevent forward movement of the dura which would compress the spinal cord]. Their role would prevent dural tension leading to headaches [56] or other forms of neck pain and cervical myopathy. [54]
An additional area of recent anatomical investigation has involved scoliosis, whose cause remains unknown and which has been highly refractory to treatment. A group of rats developed thoracolumbar scoliosis within a week after dental derangement [an induced malocclusion] such that the resulting tilt of the C1 vertebra could affect the alignment of the adjacent vertebrae and lead to the destabilization of the vertical alignment of the spine. [57]
One model which appears to reconcile a broad range of patient presentations with the characteristics of the spinal subluxation is buckling, defined as a deformation within the multisegmented nature of the spinal column caused by an overload and/or muscle stiffness which falls short of its intended activity. Buckling then leads to a concentration of local tissue stress which, if sufficiently large, will lead to pain and inflammation. [58, 59]
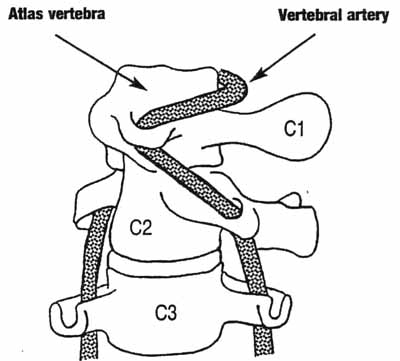
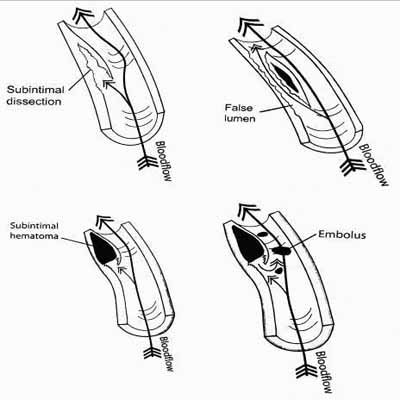
A final element of considerable importance to the safety of manipulation is the vertebral artery, a topic to be discussed in further detail below [Section V]. The composition of the vertebral wall has been discussed in some detail by Rosner, essential for understanding how arterial integrity may be compromised by natural causes. [60] Numerous recent studies have indicated that blood flow following extreme rotation and extension appears to decrease. [56, 61, 62]
C. Biomechanics:
At the core of biomechanics research is the assessment of the interaction of imposed mechanical forces and the bones, muscles, ligaments, and other soft tissues which experience them. This understanding is essential for chiropractors, whose primary objective is to restore balance and mobility to the spinal column and other musculoskeletal structures subjected to translational, rotational, compressive and distractive forces.
John Mennell did much to emphasize the heart of biomechanics, stressing that the loss of a functional movement demanded a return to mechanics. Loss or alteration of movement was understood to accompany the pain treated by a chiropractor, the element of interest being joint play. [63] This required a thorough understanding of the forces internally at the joint surfaces, in addition to those experienced when the practitiioners hand meets the patient's body.
These principles were advanced in numerous investigations, harking back to the studies of Janse and Illi in the 1940s. [64, 65] More recently, Adams and Wood were able to determine peak normal forces, their duration and impulses by inserting a force transducer between the hands of practitioner and a model of the patients body. [66] These results were subsequently refined in the 1990s by Herzog, Kawchuk, Conway and others at the University of Calgary, applying these measurements to different techniques of manipulation to all regions of the spine. [67, 68] Carrying this line of inquiry forward, Triano and Shultz [69] demonstrated in a study involving 6 chiropractors employing 3 different techniques [each on 11 patients] that:
Precise forces of manipulation at the joint surface are significantly influenced
by the type of technique as well as patient posture;
Clinically significant forces are delivered at the joint surface level; and
These forces approximate those seen in common daily tasks, such as on jobs
requiring lifting and twisting movements.More specific force measurements at the vertebral areas affected by adjustments was accomplished either by surgery or using intact cadaveric human spine specimens. In patients undergoing lumbar surgery, Keller found peak displacements of the vertebrae of about 0.6 mm within 10 milliseconds at forces of 30N150N, as applied either by mechanical force with the Activator as an adjusting instrument or by very high-velocity thrusts. [70] In cadaveric human lumbar spines, vertebral translations were 12 mm, rotations were 13°, and capsule strain magnitudes were approximately 5% after simulated high velocity spinal manipulations. [71]
Turning to the use of geometric data, a number of investigators performed displacement measurements in live subjects. One such approach was to assess in vivo spine motion by digital video fluoroscopy. [71] Another was to assess the motion of the patient's head during two different techniques of cervical manipulation. [72] A third was to measure the effect of loading frequency on spine stiffness and nonlocal displacement effects in the lumbar region by employing machine-controlled cyclic mobilizations. [73] Combining both force and geometric measurements, Van described the 3-dimensional force applied during high-velocity, low amplitude manipulations of all regions of the spine. [74]
Arguably one of the most inclusive models of subluxation and the application of biomechanics has come from the novel external fixation model in rats described by Cramer, Henderson and coworkers at both the National University of Health Sciences and Palmer University. Here the spinous processes of L4L6 were fixed by a noninvasive, removable yoke for up to 8 weeks [FIGURE 2]. Osteophytes and degenerative articular changes of the facet joints could be observed for fixation times as short as 1 week and became irreversible after 4 weeks of fixation. [35] Changes in spinal stiffness were also noted, being greater in magnitude and producing greater misalignments during forced extension testing for longer linked periods before removal of the yoke. [75]
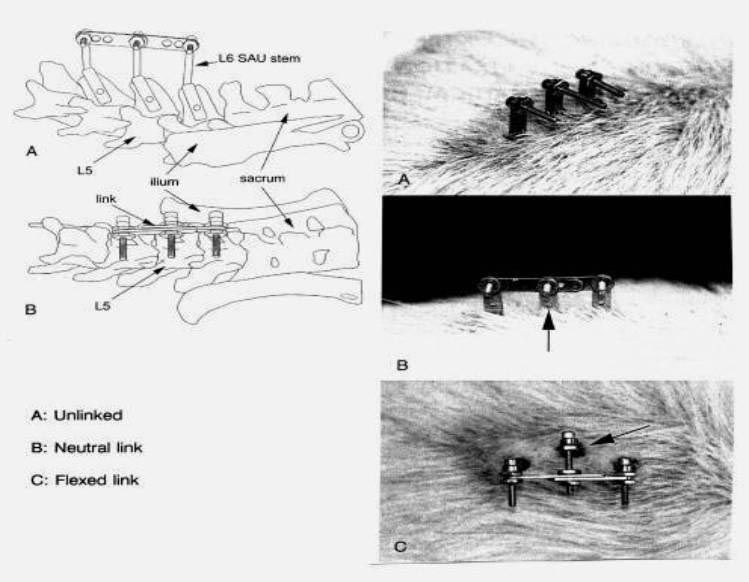
Figure 2: External link animal model for subluxation [35, 75]
D. Neurology:
Harking back to Solon Langworthy's assertion that the core of chiropractic principles lies in the nervous system], [76] we need to review some of the key research accomplishments relating to neural activity in response to both manipulations and the dysfunctions they are intended to treat. For it is indeed the nervous system which provides the necessary communication links to hormonal, inflammatory, immune and visceral activity in addition to pain perception -- all of which are to be discussed later in this chapter.
A wide variety of neurophysiologic studies are simply not possible to perform in humans; thus, animal models once again come to the forefront for providing the necessary evidence for chiropractic in the basic sciences. TABLE 3 is a sampling of some of the earlier outcome effects achieved in a variety of animals as the result of different types of interventions, all involving noxious stimuli. [36, 7786] Quite distinct from pain are effects which extend far from the area of stimulation. With several of the investigations showing that nerve conductivity is specifically affected, [77, 78, 83] it is clear that the nervous system provides an essential link between the experimentally produced aberrations and the physiological changes observed. Additional investigations using rats have been able to elicit decreases in both mean arterial pressure and nerve blood flow following saline injections into the ipsilateral L4/L5 facet joint. [87] Further experiments by the same investigator [Sato] demonstrate decreased gastric motility in response to a somatic stimulation [skin pinch]. [88]
Thus, a wide range of stimuli are capable of producing physiological responses, providing a much broader canvas with which subluxations can e represented in experimental research and again placing the nervous system at the center.
The complete description of the autonomic nervous system and its division into the sympathetic and parasympathetic branches is beyond the scope of this chapter, but is provided elsewhere. [89] With regards to changes in neural function in response to either stress or manipulation, however, several observations can be brought to light:
- [90, 91] The same responses are observed with the injection of an inflammatory cocktail into the same region. [37]
Insertion of a small pin into the IVF of the L4 and L5 vertebral joints of the experimental rat, mimicking a space-reducing lesion, produces thermal and mechanical hyperalgesia in the hindlimb and increases the excitability of dorsal root ganglion cells
- [92]
Reflex responses in paraspinal muscles are attenuated by activating Z-joint receptors in rats, regarding noxious stimulation of nerves in the intervertebral disk. Accordingly, there may be interaction between spinal joint receptors and he processing mechanisms for spinal reflexes.
- [93]
Abnormal somatosensory evoked potentials from the paraspinal musculature are found correlating with decreased pain responses after lumbar manipulation, possibly due to a central effect of sensory processing.
- [94]
In a cohort of 12 subjects with a history of recurrent neck stiffness and/or neck pain but no acute symptoms at the time of study, a single session of cervical spine manipulation reveals a significant decrease in the amplitude of 2 components of somatosensory evoked potentials, lasting 20 minutes following the intervention. The implication is that cervical spine manipulation may alter cortical somatosensory processing and sensorimotor integration, shedding light upon the mechanisms for the relief of pain and restoration of functional ability which are the most widely observed outcomes to treatment by spinal manipulation.
- [95]
In subjects subjected to side-posture manipulation, both Hoffman reflex and M-wave responses display the greatest attenuation with actual manipulation--as opposed to a positioning maneuver.
- [96]
Following SI joint manipulation, there is a decreased inhibitory effect of knee joint pathology on quadriceps muscle activity, suggesting an interaction between spinal manipulation and the inhibition of voluntary activities produced by pain.
- [9799]
Power spectrum analyses of patient electrocardiograms suggest alterations of sympathetic and parasympathetic activity produced by spinal manipulation.
- [100] The proprioreceptors, displaying a unique response to the thrusting portion of the applied load suggests that these receptors might contribute to the therapeutic effects of spinal manipulation. [101]
In the experimental cat, muscle spindles and Golgi tendon organs in paraspinal muscles respond to vertebral loads with force-time profiles resembling those in spinal manipulation.
E. Hormones:
The manner in which the endocrine system relates to chiropractic is best represented through three approaches:
The way pain is associated with the endocrine system and the implications
in the relief of pain through spinal manipulation;
The way stress is associated with the endocrine system and the way its
detrimental effects on health may be relieved by spinal manipulation; and
A description of specific endocrine disorders and their responses
to spinal manipulation.
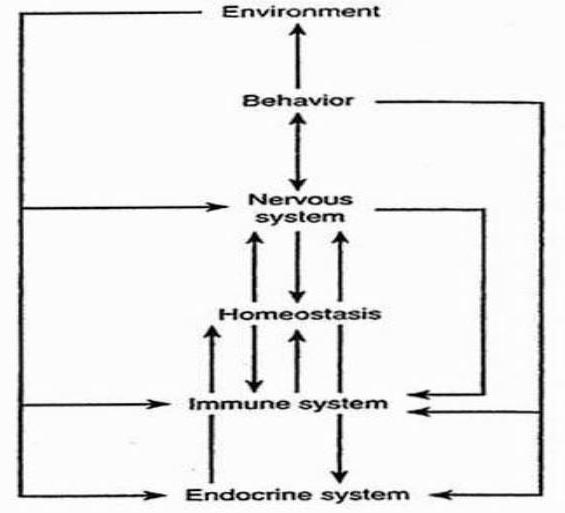
Figure 3: Interaction of stress with various body systems [104]
The psychologic and psychosocial influences on the course of human disease have led to the science of psychoneuroiimunology [PNI] used to describe the communication system between the mind and body. [102, 103] A considerable body of research established that through a complex system of feedback loops and interactions, a close communication among the CNS, the immune system, and hormones by means of the hypothalamic-pituitary-adrenal [HPA] axis existed [104] [FIGURE 3].
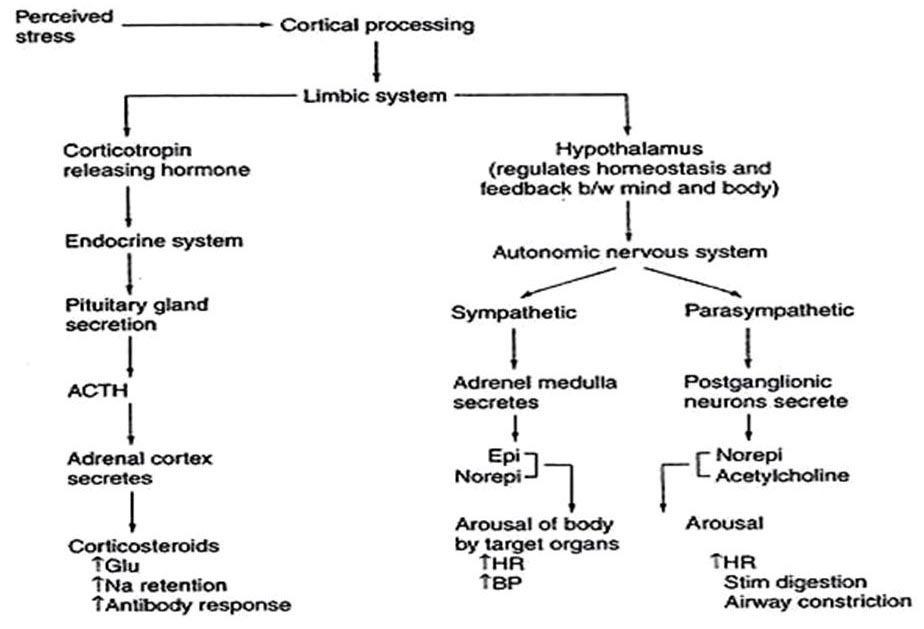
Once stress is experienced, distinct chemical entities including the neuropeptides and neurohormones function as a primary means of intercellular communication. The end result is the complex pathway shown in FIGURE 4, the most important aspect of which is the secretion of corticosteroids -- in particular, glucocorticoids [including cortisol] from the adrenal cortex in response to adrenocorticoid [ACTH] secretion from the anterior lobe of the pituitary. Glucocorticoids subsequently exert a variety of effects on the cardiovascular system, muscle, and immunologic activity -- much of which is detrimental. Connections between increased cortisol levels and stressful events has been well documented. [105, 106]
The fact is that chronic stress has been shown to promote an extensive variety of disorders, some of which are life threatening. These include: infections from cold viruses [107] and herpes; [108] heart disease; [109, 110] gastrointestinal dysfunction; [111] insulin-dependent diabetes mellitus [in animal models]; [104] and systemic lupus erythematosus. [103]
Figure 4: Psychoneuroendocrine stress responses
The most direct evidence that chiropractic appears to relieve stress is from two recent randomized clinical trials. One found that spinal manipulation significantly reduced the intensity of emotional arousal reported by phobic college students. [112] A second demonstrated significant reductions in validated anxiety, depression and stress scores in asthmatic patients who were manipulated, as opposed to those who merely reported to chiropractic centers for consultation. [113] The previous trial and two additional investigations involving either chiropractic manipulation [114] or massage [115] indicated the spinal manipulation may also reduce salivary cortisol levels.
The evidence that chiropractic is effective in relieving pain, reviewed below in Section IV, is mentioned here in its possibly being mediated by two hormonal metabolites found to respond to spinal manipulation. Beta-endorphins [enkephalins] have been proposed to display a gating, palliative effect at the first synaptic relay in the spinal cord, limiting the transmission of pain information from the peripheral pain receptor to the brain. [116] Investigations by Vernon [117] revealed approximately an 8% increase in the level of plasma endorphins 5 minutes after a single rotary manipulation in asymptomatic men. This effect was not repeated in other studies; [118, 119] ; however, only Vernon's study employed measurements timed to more closely match the rapid postintervention physiologic events suggested by others [120] and are more indicative of the short half-life of plasma beta-endorphin. [121] Two specific forms of the prostaglandins, the hormones responsible for uterine contraction and suspected to be the cause of menstrual pain in dysmenorrhea, were found in a pilot study by Brennan to be suppressed together with menstrual pain after side-posture manipulation, as opposed to patients who received a low-force sham procedure. [122] Inconclusive results were obtained in a follow-up full-scale randomized clinical trial; [123] however, major design flaws in that particular investigation have virtually invalidated its results. [22]
In addition to the hormonally driven dysmenorrhea being relieved by spinal manipulation, [122, 124127] numerous endocrine disorders have been reported to respond to spinal manipulation. These include premenstrual syndrome, [128130] hypertension, [131134] and even extremely preliminary single case reports suggesting that diabetes [135] and hot flashes during menopause [136] could diminish as well. One additional trial failed to distinguish a difference in the blood pressures of dieting patients, with or without spinal manipulation included in treatment. [137] To explain this particular discrepancy, both the chiropractic technique and frequency of manipulation need to be explored further.
A comprehensive description of the endocrine system and its relation to chiropractic has been provided elsewhere. [138]
F. Inflammation:
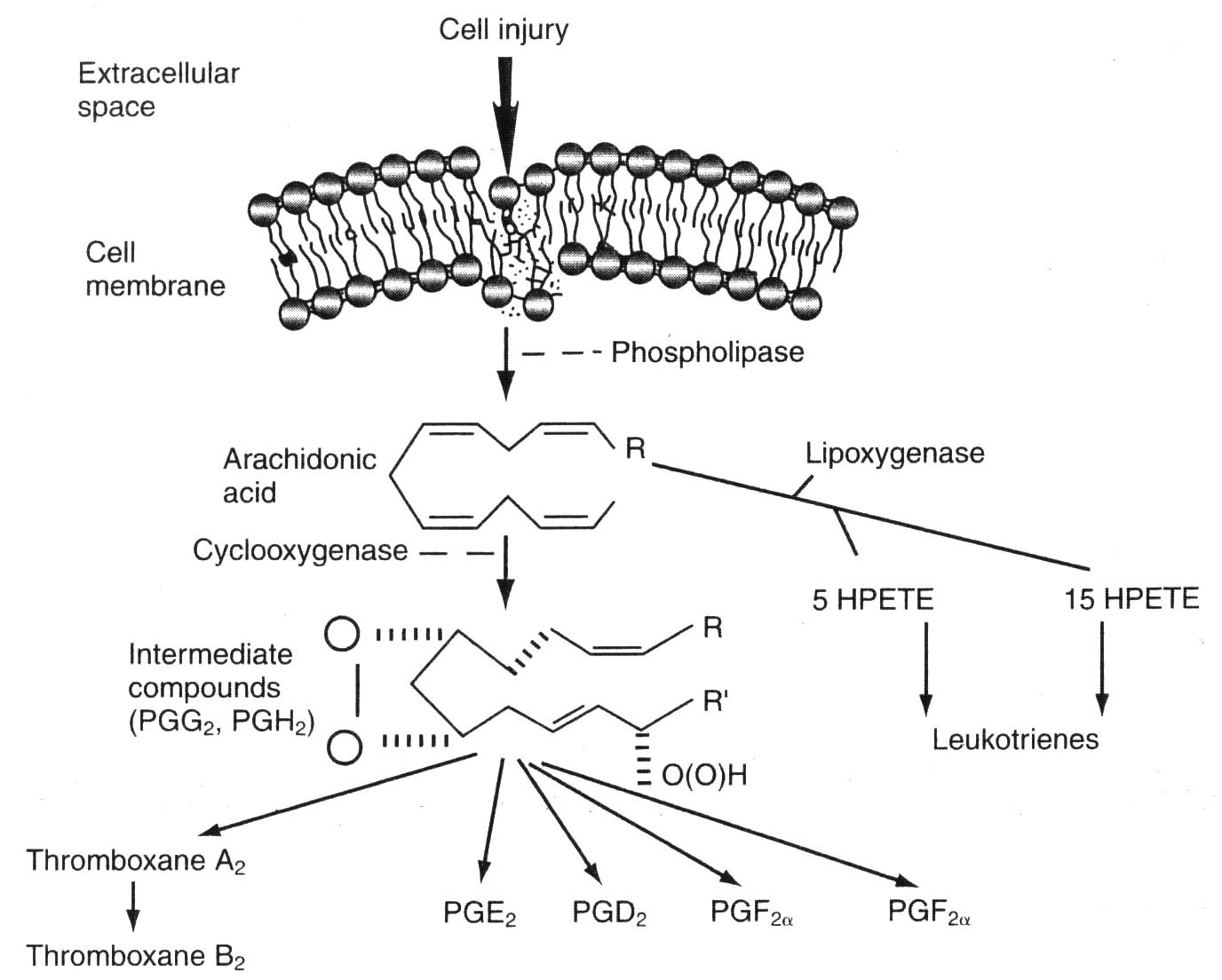
Figure 5: Chemical events following cell injury [139]
Inflammation is a twofold response of the vascular tissue in an organism, both to remove harmful stimuli--such as pathogens, damaged cells, or irritants -- or to initiate healing. In the acute phase, it can be experienced by redness, pain, heat, swelling, and loss of function. The immune system and a variety of cells within the injured tissue participate as well. At the site of cellular injury, the locus of pain in the peripheral nervous system, a cascade of chemical events occurs. It is characterized by the production of arachidonic acid and its conversion by cyclooxygenase to intermediates ultimately resulting in the production of the prostaglandins. This sequence is depicted in FIGURE 5. [139]
If left unchecked, this process becomes chronic and can lead to a number of conditions including hay fever and other allergies, inflammatory bowel diseases, rheumatoid arthritis, autoimmune diseases, and atherosclerosis. Playing a central role in several stages of atherosclerosis are the cytokines, which are neuropeptides acting like hormone messengers to integrate the functional activity of other immune cells. [140] They orchestrate the production of adhesion molecules, matrix metalloproteinases, and reactive oxygen species that may also be released from lesions. Particularly active in this capacity is the pro-inflammatory cytokine interleukin IL-6, which travels to the liver and elicits an acute-phase response, resulting in the release of C-reactive protein, fibrinogen, and plasminogen activator inhibitor [PAI]-1, all essential components to the development of atherosclerosis. [141, 142]
It turns out that control of this process can be linked directly to chiropractic, in that preliminary evidence in both animal models and humans suggests that spinal manipulation may be effective in retarding or reducing several indicators of inflammation.
By injecting an inflammatory cocktail directly into the L5 intervertebral foramen of experimental rats, Song and his colleagues were able to evoke a broad spectrum of indicators of neural excitability and inflammation, including[i] thermal hyperalgesia, demonstrated by quicker foot withdrawal in response to heat;
[ii] mechanical allodynia, shown by more rapid foot withdrawal in response to touch;
[iii] hyperexcitability of the dorsal root ganglia, revealed by electrophysiological recordings; and
[iv] vascularization and satellitosis, seen as cellular inflammations under the microscope.All these indicators diminished with time following the application of mechanical manipulations to the L5 or L5 and L6 spinous process by means of the Activator adjusting instrument; no such effects if the manipulation was directed to the L4 joint. The implication was that mechanically applied manipulation can significantly reduce the severity and duration of pain and hyperalgesia caused by inflammation of the lumbar intervertebral foramen. [37]
This narrative shifts to humans with the finding by Teodorczyk-Injeyan that asymptomatic humans who are subjected to a bilateral hypothenar thrust procedure in spinal manipulation and who experience a cavitation display a marked decrease in their blood serum levels of the pro-inflammatory cytokines. [143] At the same time, levels of the anti-inflammatory cytokines increased. [144] Neither effect was observed in the absence of cavitations. [143, 144] To close this intriguing circle of evidence linking spinal manipulation and the control of the potentially lethal pro-inflammatory cytokines, further research is necessary to determine whether these effects can be duplicated in:[i] humans experiencing back or other types of pain, and
[ii] experimental rats.One vital step in this direction is a recent finding that the pro-inflammatory cytokines IL-1 alpha, IL-1 beta, tumor necrosis factor alpha, and IL-6 are all elevated within weeks in experimental rats which are subjected to repetitive motion injuries. [145] Thus we are left with the intriguing possibility that spinal manipulation may be able to retard or forestall potentially life-threatening human conditions.
IV. Outcomes Research
A. Methods of Measurement:1. Design issues: As in other outcomes clinical research, chiropractic investigations require reproducible and verifiable measurements from multiple points of view involving both the patient and clinician. TABLE 4 illustrates five such perspectives:
[1] the results of physical examinations;
[2] functional abilities;
[3] patient perception regarding pain, satisfaction, duration of complaint, and use of medications;
[4] general health and psychosocial assessments; and
[5] direct and indirect costs of treatment.All these indices have been verified in the literature; use of the measures represented on this list helps to ensure that an outcomes study achieves sufficient construct validity.
At the same time, outcomes research [particularly involving physical interventions] is tarnished by what appears at first glance to be a conundrum. FIGURE 1 has listed outcome studies in order of decreasing rigor, from the most fastidious, demanding [and costly] RCT to anecdotes arising from everyday clinical experiences. One might assume at first that the most controlled investigation [the clinical trial] would yield the most useful information. Indeed, the clinical trial has been referred to as the "gold standard" [146] in clinical research. But paradoxically, because the double-blind study is so controlled, this most rigorous member of the clinical research hierarchy presents its own difficulties in its generalizability:
The characteristics of its own experimental patient base [including comorbidities] may differ significantly from those of the individual presenting complaints in the doctor's office.
Potentially important ancillary treatments are restricted, screening out conceivably significant and perhaps unidentified elements that occur in the natural setting of the patient's visit to the physician.
Outcome results chosen may not necessarily be those used to evaluate a patient's welfare under care of an actual physician.
Experimental groups may not be large enough to reach statistical significance, even though the clinical effect may be real in many individuals.
Thus, experimental designs at the "lowly" end of the spectrum, such as anecdotes, single case reports, offer their own form of generalizability, although they are of an uncontrolled and often confounded nature. Again, this does not mean that they fail to provide clinical significance. Ideally, to support a particular type of intervention, what is needed are research results from both ends of the hierarchy shown in FIGURE 1, to capture both the rigor and the generalizability sought in clinical documentation. It is, after all, material from the anecdotes and clinician's office that provide the impetus and inspiration to design and conduct an RCT in the first place.
2. Systematic reviews, meta-analyses: In an effort to filter out low-quality studies, rating systems of trial quality have abounded as an attempt to assure that that the edifice of evidence used to warrant a therapeutic approach is more than a house of cards. These form the cornerstone to both systematic literature reviews and meta-analyses, the former defined as a comprehensive and rigorous review of the peer-reviewed scientific literature requiring a predetermined threshold of graded quality in order to be included. In meta-analyses, on the other hand, actual effect sizes are calculated from pooled results of different clinical trials using a variety of statistical procedures and taking into account the size of each study.
A multiplicity of scoring systems for trial quality exists, but their essence is perhaps best reflected by the rating chart shown in TABLE 5. It is taken from a recent blend of narrative and systematic reviews by a group of leading clinical chiropractic researchers headed by Gert Bronfort. [147] What is perplexing is that two out of the eight criteria for quality recognize blinding of the patient or practitioner as an attribute for quality ratings. As mentioned previously, successful blinding of these parties in any trial involving physical interventions is virtually impossible.
This is only the beginning of limitations of systematic reviews and particularly meta-analyses. In a critique of the latter design, Feinstein argues that some of their problems include: [148]
Disparate groups of patients of varying homogeneity across different studies are tossed into one analysis like a mixed salad, overwriting the clinician's need to know about subgroups which relate more to the patients actually seen.
The weighting of studies of different quality may be inaccurate or absent altogether.
There is the need to know about real-world effects [severity in illness, comorbidities, changes in schedule, pertinent co-therapies, clinically relevant outcomes] in presentation and treatment.
The statistical treatments in the papers pooled are inconsistent.
As a means to alleviate the limitations of randomized clinical trials, systematic reviews, and meta-analyses, modified designs based upon a blending of observational and experimental studies have been proposed. Among these are Pragmatic Clinical Trials [PCTs] and Whole Systems Research [WSR].
PCTs ask practical questions about the risks, benefits, and costs of intervention as they would occur in routine clinical practice. In addition, they include a diverse population of study participants, recruiting from a variety of practice settings and collect data from a broad range of health outcomes. The interventions which they select are clinically relevant. [149]
WSR uses observational studies and includes qualitative as well as quantitative research. In so doing, it provides the opportunity to assess the meaning that patients attribute to an intervention, probing the process and context by which healing occurs. Outcomes which are relevant to the patients are selected, and the approach explores how the intervention fits with a patient's life. [150] In so doing, it reveals the role that expectations may play in healing. [150] Essentially, WSR seeks to describe the effectiveness of the entire clinical encounter rather than simply a single procedure. [151]
B. Musculoskeletal:
1. Back pain research:
a. The RAND Appropriateness and Utilization Study:
An early milestone in musculoskeletal disorders research with regard to the back and chiropractic can be credited to the RAND Corporation, a non-profit private corporation which conducts research and development [hence, the acronym] and which gained prominence with research for the U.S. military during World War II. In addition to defense, RAND's research fields include the health sciences, education, applied economics, sociology, and civil justice.
Several years and millions of dollars in the making, the RAND Appropriateness and Utilization Study sought to provide "a comprehensive set of indications for performing spinal manipulation with low back pain," the guidelines being based upon[1] a review of the literature,
[2] appropriateness ratings by both multidisciplinary and all-chiropractic panels of experts and
[3] field studies abstracted from five geographical sites: Portland, OR; Minneapolis, MN; Miami, FL; San Diego, CA; and Toronto, ONT.The significance of the literature review of 67 articles and 9 books published between 1952 and 1991 lay in the fact that it established that chiropractors within the United States performed 94% of all the manipulative care for which reimbursement was sought, with osteopaths delivering 4% and general practitioners and orthopedic surgeons accounting for the remainder. [152] Support was consistent with the use of spinal manipulation as a treatment for patient with acute low-back pain and an absence of other signs or symptoms of lower limb nerve-root involvement. If minor lower limb neurological findings or sciatica was present, the evidence was then deemed to be either insufficient or conflicting. There was no systematic report on the frequency of complications.
The appropriateness of chiropractic spinal manipulation was assessed by two expert panels, one multidisciplinary and one all-chiropractic, each rating a comprehensive array of over 1500 clinical scenarios for appropriateness or inappropriateness of chiropractic intervention. These scenarios were characterized by length of symptoms, clinical course of the pain, presence of comorbid diseases, history in response to previous treatments for back pain, findings upon physical examination, and findings on lumbosacral radiographs as well as CT or MRI. Among the appropriate conditions recognized by the multidisciplinary panel [153] for chiropractic intervention were[1] acute [<3 weeks' duration] back pain with the absence of neurological findings, or
[2] acute back pain with minor neurological findings and uncomplicated lumbosacral radiographs.In the final ratings, panelists rated 7% of all conditions as appropriate -- although these conditions represent the majority of back pain patients. As might be anticipated, the all-chiropractic panel [154] rated a higher percentage [27%] of all conditions as appropriate. Inappropriate ratings by the multidisciplinary and all-chiropractic panels were 60% and 48%, respectively. Amongst the all-chiropractic panel as opposed to the multidisciplinary panel, there was greater agreement [63% vs. 36%].
Depending upon the criteria for assessment, the field studies have yielded varying levels of appropriateness of chiropractic intervention. These have been grafted onto the the recommendations of each of the two expert panels described above. For one site [San Diego, CA], the level of appropriateness varied between 38% and 74% and the level of inappropriateness ranged from 19% and 7%, depending upon whether the criteria of the multidisicplinary or the all-chiropractic panel were applied. Data from other geographic areas of the United States will be required before inferences for the national population can be drawn, although it has been demonstrated that such a study is feasible. [155] These investigations simply served as forerunners for many different types of studies, all of which provided substantial evidence in support of the chiropractic management of back pain.
b. More recent achievements:
1) Systematic reviews and guidelines:
Interestingly, the earlier guidelines and systematic reviews of randomized clinical trials addressed to back pain and manipulation emphasized acute rather than chronic low back pain as having the more robust evidence in support of manipulation's effectiveness. [5, 156, 157] By 1997, however, more evidence supporting the effectiveness of spinal manipulation compared to other interventions became more apparent for chronic as well as for acute conditions. [158] That trend has held up through the more contemporary systematic reviews of Bronfort [159, 160] and very recently by the Scientific Commission of the Council on Chiropractic Guidelines and Practice Parameters [CCGPP]. [161] Bronfort's systematic review indicates that with all patients with chronic low-back pain, there is moderate evidence that[i] spinal manipulation with mobilization is superior to usual medical care for patient improvement; and
[ii] high-dose manipulation is superior to low-dose manipulation for pain reduction in the short term.
In randomized clinical trials in which most, but not all, patients had chronic low-back pain, there is moderate-to-strong evidence that:[i] manipulation is superior to usual medical care alone; and
[ii] manipulation with mobilization is superior to physical therapy and to home exercise in the long term. [161]
The CCGPP literature synthesis represented a blending of[i] a consensus process developed at RAND, [162]
[ii] the Cochrane Collaboration review of literature for low-back pain,
[iii] the guidelines developed by what had been the Agency for Health Care Policy and Research, [5] and
[iv] published recommendations for the development of clinical guidelines. [163]In retrieving 64 randomized clinical trials, 12 guidelines, 13 systematic reviews and meta-analyses, and 11 cohort studies, the Commission reviewed the evidence in support of spinal manipulation as a means to reduce symptoms and improve function in low-back pain patients and concluded that "as much or more" evidence exists for managing chronic as for acute and subacute conditions. For the cross-section of treatment approaches taken, the Commission issued ratings of the strength of evidence in their support as shown in TABLE 6. [161]
In the interim from 19922008, however, several systematic reviews came to less sanguine conclusions. Assendelft concluded in 2005, for instance, that there is no evidence that spinal manipulation therapy is superior to either standard treatments for patients with acute or chronic low back pain. [164] To begin, this could be interpreted in the same breath to indicate that, in terms of the pain or disability outcomes scales evaluated, spinal manipulation is not inferior. A second systematic review suggested that spinal manipulation "has small clinical benefits that are equivalent to other commonly used therapies" and does not reduce the costs of care following an initial course of therapy. [165] And a third which called itself a systematic review of systematic reviews concluded that the data fail to demonstrate that spinal manipulation is effective for a wide variety of medical problems. For back pain, spinal manipulation was deemed to be superior to sham manipulation but not conventional interventions -- and the prevalence of adverse events discouraged its use. [166] All of these reviews, however, are fraught with significant weaknesses such that they must be interpreted with extreme caution, if not skepticism. These flaws are summarized in TABLE 7.
In terms of resolving conflicting reviews, the devil clearly is in the details. For example, in a recent presentation at a chiropractic research conference sponsored by the Health Resources and Services Administration, [167] Gert Bronfort emphasized how apparently related reviews actually embodied differing goals and methodologies, such that they could easily be misinterpreted or confused. With regard to back pain, for instance, the contrast between the Assendelft [164] and Bronfort [159] reviews can be demonstrated as follows:
Assendelft [164] Bronfort [159] To assess if SMT is better than anything else To assess if SMT is an effective treatment Stastical pooling using an unusual method Statistical pooling is not possible SMT is only equal to sham therapy or therapy judged to be ineffective or even harmful SMT offers more short-term relief than mobilization or detuned diathermy
2) Practice-based reseach for chronic low back pain:
An early and most dramatic example of a Pragmatic Clinical Trial [See Section IV.A.2.] as part of the strategy to employ practice-based research was provided in 1990 by Meade. A total of 741 patients at 11 clinical centers were randomized to receive either chiropractic or conventional hospital treatment in their respective natural settings. In contrast to many trials in which the relief of an intervention is observed for only a brief period, the Meade study followed patients for two [168] and three [169] years and showed that patients undergoing chiropractic treatment yielded disability scores that were lower than those experienced by the conventionally treated cohort by a clinically significant amount. One problem that has been raised regarding the Meade study, however, is that only 28% of its patients were randomized into the chiropractic branch of treatment. [169]
These findings were buttressed and expanded in a later study involving 2870 patients with acute and chronic low back pain who visited either medical or chiropractic physicians' offices and given customary care. By 2 weeks, maximizing at 1 month, and persisting for 2 years, clinically important advantages in both pain and disability scores were found in patients experiencing chiropractic treatment. A real-world outcome typical of practice-based research was shown by the number of pain days within the past year recalled by patients, substantially fewer being reported by the chiropractic cohort [FIGURE 6]. [170]
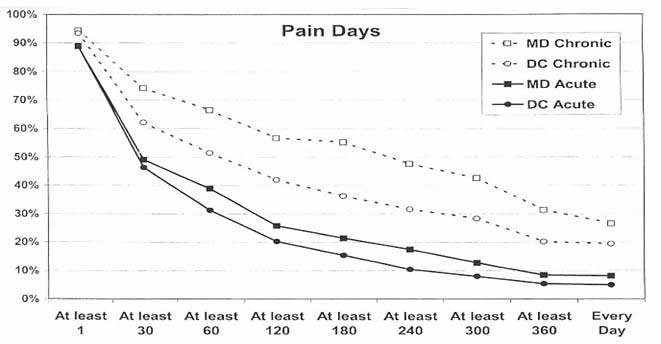
Figure 6: Patients with LBP treated by medical and chiropractic physicians:
Pain day recall at 36month follow-up: Cumulative probabilities [170]
3) Comparisons with acupuncture, NSAIDs, muscle relaxants:
One of the most dramatic outcomes in a randomized clinical trial was offered by Giles and Muller in a multidisciplinary spinal pain unit of the Townsville General Hospital in Australia. Here, 115 patients experiencing chronic [>13 weeks] of back and neck pain were randomly allocated to either medication with NSAIDs [Celebrex or Vioxx], needle acupuncture, or chiropractic spinal manipulation by means of high-amplitude, low-velocity applications to a vertebral joint. At the end of 9 weeks of treatment, the highest proportion of individuals reaching full recovery [asymptomatic status] was found for manipulation [27.3%], followed by acupunture [9%] and medication [5%]. For improvements in disability [Oswestry scale], and range of motion, the chiropractic cohort again displayed superior outcomes. While improvements in pain scores [VAS] for the back were greatest for the chiropractic intervention [50% vs 15% for acupuncture, 0% for NSAIDs], they were slightly inferior to those obtained by acupuncture for neck pain [42% vs 50% for acupuncture, 0% for NSAIDs]. [171] These results were later found to be sustained for most patients at 1year of follow-up. [172]
4) Dose-response characteristics:
Until recently, an area of outcomes evidence lacking meaningful documentation pertained to two highly practical areas of chiropractic practice:[i] how many treatments at what frequency produces an optimal effect; and
[ii] are the effects enhanced by including ancillary treatments to the manipulative procedure that is at the core of chiropractic treatment?This void has been largely fulfilled by a recent study by Haas, who demonstrated that, regarding spinal manipulations for low back pain, the beneficial effects for both pain and disability continue to accrue for up to 12 patient visits within a 3week period. These results were apparent at both 4 weeks following the initiation of chiropractic treatment and at 12 weeks. Furthermore, the extended benefits at 12 weeks of follow-up were experienced only if ancillary physical medicine interventions were included with the manipulative treatments [FIGURE 7]. [173] . Therefore, such techniques as hot and cold applications, electrical muscle stimulation, and ultrasound may very well exert a synergistic effect in enhancing and extending the benefits of spinal manipulation. Previously, these physical medicine methods had been judged to be ineffective when used in isolation. [5] Furthermore, the study indicated that, for at least some low back pain patients, cessation of treatment before 12 treatments are completed may be premature. [173]
This study has profound implications in reestablishing the limitations that may have been imposed upon chiropractors by third party payors. It also demonstrates that multifaceted rather than one-dimensional approaches in treating back pain may be in the patient's best interest.
5) Early vs late intervention, preventive SMT:
An important part of the overall planning for the optimum frequency of chiropractic adjustments is the timing of the first intervention. One randomized trial which shed light upon this question involved the randomized assignment of 102 patients with acute low back pain into treatment groups which stipulated a combined treatment of manual therapy, exercise, and biopsychosocial education in one cohort and a waiting period involving no treatment for the other. As might be expected after 6 weeks, the group which was actively treated displayed superior outcome scores relating to disability, mood, general health, and quality of life. At longer terms of follow-up, pain and disability scores of the two groups converged while mood, general health, and quality of life remained superior in the treated group. The implication in this investigation was that an early intervention regimen including manual therapy offers better outcomes. [174]
In terms of prevention, two studies involving elderly populations have been provided. As part of a comprehensive geriatric assessment program, the RAND Corporation studied a subpopulation of patients who were under chiropractic care compared to those who were not and found that the individuals electing continuing chiropractic care were:
Free from the use of a nursing home [95.7% vs 80.8%];
Free from hospitalizations for the past 23 years [73.9% vs 52.4%];
More likely to report a better health status;
More likely to exercise vigorously;
- [175]
More likely to be mobile in the community [69.6% vs 46.8%].
More suggestive data concerning prevention comes from a recent study of patients with chronic low back pain who were divided into two groups, one receiving 12 treatments within a single month and the other adding to this regimen one treatment every 3 weeks for an extended 9 months [1214 additional visits]. In terms of disability [as indicated by a modified Oswestry questionnaire], the group receiving the supplementary maintenance treatments continued to improve throughout the entire 10 month period, while the cohort lacking the additional visits reverted to baseline levels within that same period. [176] The authors of this study speculate that repeated chiropractic visits may have been the direct cause for the improvement of disability scores due to
[a] improved trunk mobility, [177]
[b] facilitated release of entrapped synovial folds or relaxation of hypertonic muscle by sudden stretching, [178] or
[c] the disruption of articular or periarticular lesions. [179]It is important to emphasize that this particular study addresses supportive [tertiary maintenance] care as opposed to primary maintenance care.
6) Pediatrics research:
Despite the wealth of studies regarding low-back pain outcomes in adult populations [180] and the fact that low back pain is the condition most frequently associated with chiropractic care, [181] there have been no controlled trials to date on the outcomes of chiropractic treatment for low-back pain in pediatric and adolescent populations, according to searches on MEDLINE from 19872006 and MANTIS from 19922006. From this undertaking, only one cohort [182] and three case studies [183185] involving spinal manipulation by a chiropractor could be identified.
This gap in the pediatric low back pain literature fortunately has begun to be addressed with a more recent prospective study of consecutive pediatric patients with low-back pain seeking treatment from randomly selected chiropractors within the cities of Calgary, Alberta and Toronto, Ontario, Canada. Chiropractors were eligible to participate if they were in practice for a minimum of 5 years and saw a minimum average of two pediatric patients per week. A maximum of 5 consecutive cases between the ages of 4 and 18 with a new episode of mechanical low back pain [not previously treated by a chiropractor] were accepted. Low back pain was defined as pain or discomfort in the area bounded by the lowest set of ribs in the patient's back to the lower edge of the buttocks. A total of 15 chiropractors provided data on 54 patients, 61% of which were acute presentations and 47% relating to the onset of a traumatic event. All patients were followed until they reported resolution of the problem, discharge, referral, or discontinuation of treatment. Assessment of low back pain was accomplished by means of two indices:[i] the visual analog scale [VAS], and
[ii] a subjective 5point Likert scale. The mean VAS upon presentation was 5.6.The most commonly used form of intervention was spinal manipulation, with 95% of follow-up visits including this therapy. Included in additional treatments were passive manual therapy, such as soft tissue treatments and mobilization and such modalities as interferential current and ultrasound. Just 7.7% of patients underwent active management, such as patient-directed home exercises, nutrition, and other education.
Within a 6week course of management, "much improvement" [Grade 4 on the Likert scale] was attained in 62% of the patients, with a median time of 16 days. "Important improvement"" [Grade 3.8 on the VAS] was reported from 87% of the patients with a median time of 28 days. Patients with chronic low back pain were less likely to respond within the median number of treatments. [182]
Given the fact that chronic patients were less likely to respond and that relatively few practitioners employed active management strategies, it appeared to the authors that further education of chiropractors regarding this particular mode of treatment was indicated. Because there was no natural history comparison group, it is not possible to directly implicate cause and effect from this particular study. However, there does seem to be a clear implication that the majority of pediatric patients with low back pain [especially acute] respond positively to chiropractic treatment. [182]
The case studies, all addressing lumbar disc herniation experienced by adolescents, require our further attention. All support a prudent course of healthcare, beginning with the most conservative and least invasive modalities and progressing until a positive outcome is attained. [183185] A study by Hession described a progression from flexion-distraction to side-posture manipulation, with full recovery experienced by 8 weeks with no recurrence of complaints by 16 months after treatment. [183] Kazemi depicted a far more involved and lengthy course of treatments -- all conservative -- for 20 weeks, yielding a patient who was pain-free at one year of follow-up. [184] King's report described an adolescent who began treatment conservatively [even with a return referral from a neurosurgical consultation] but ultimately underwent surgery for disc removal after just 3 weeks of visits to both chiropractic and allopathic providers. [185] Taken together, these three case studies cannot establish cause-and-effect but do provide a blueprint as to how pediatric musculoskeletal conditions might best be managed by both the chiropracic and allopathic communities. It is also clear that further clinical research including the more controlled design of randomized clinical trials would add invaluable evidence to further support the chiropractic care of pediatric and adolescent populations with back pain.
Despite the multiplicity of outcome studies for adults, [186190] which have gained recognition in a study conducted by Duke University and endorsed by the Agency for Health Research and Quality, [191] there have not been formally constructed manipulation outcome trials with pediatric populations. Rather, there have been numerous case studies and case series, a portion of which have appeared in the peer-reviewed journals. Tension-type, cervicogenic, and even migraine headache have been described with positive outcomes. [192197] Lisi's investigation is noteworthy in that it reports that the cervicogenic headache frequency decreased to just twice a month after only a single treatment. [197] Other than Hewitt's positive case report, [193] no published outcome studies pertaining to neck and shoulder pain specifically in children could be located. For the present, the encouraging results of the adult clinical trials [156161] can be interpolated and melded with the aforementioned positive pediatric case outcomes [192197] to suggest that spinal manipulation in the treatment of pediatric headaches enjoys a modest base of evidence.
7) Lumbar disc herniation research:
Regarding disc herniations, it has been shown that more than a third of total health care and societal costs may be attributed to 12% of low back pain patients who undergo surgery for disc herniation. [198] Compared to outcomes of patients undergoing conservative care for disc herniations, surgical patients were found to improve just as rapidly and completely as experienced by a randomized clinical trial, [199] and even more rapidly and completely if seen through the lens of an observational study. [200] The striking results of the latter study speak to the possible importance of patient expectations in nonblinded, nonrandomized selections of therapy; however, they must also be interpreted with caution due to the possible confounding of results in self-reported nonrandomized studies. [200] What must be kept in mind is that lumbar disk surgeries have been reported to have a complication rate of 24%, almost half of which are major in nature. [201]
Two randomized trials currently support the wisdom of considering spinal manipulation as a treatment option for this condition. One study involving 51 cases of myelographically confirmed disc herniation compared rotational mobilization to conventional physical therapy [e.g., diathermy, exercise, and postural education]. The manipulation group demonstrated greater improvement in range of motion and straight leg raising compared to the physical therapy cohort, leading Nwuga to conclude that manipulation was superior to conventional treatment. [202]
The second trial examined 40 patients with unremitting sciatica diagnosed as due to lumbar disc herniation with no clinical indication for surgical intervention. Subjects were randomized into two treatments: [i] chemonucleolysis [chymopapain injection under general anesthesia] and manipulation [15minute treatments over 12 weeks, including soft tissue stretching, low-amplitude passive maneuvers of the lumbar spine and the judicious use of side-posture manipulations]. Back pain and disability were appreciably lower in the manipulated group at 2 and 6 weeks with no improvement or deterioration in the chemonucleolytic group. By 12 months there were improvements in both groups with a tendency toward superiority in the manipulated cohort. [203]
Further support for manipulation in the treatment of disc herniations is provided from several prospective studies. [204208] The largest involved 517 patients diagnosed with lumbar disc protrusion, 77% of these having favorable response from pain after manipulative therapy. [207] A literature review from Cassidy [209] suggests that an additional 14 of 15 patients with lumbar disc herniations experienced significant relief from pain and experienced clinical improvement after a 2- to 3-week course of side-posture manipulation.
2. Neck Pain Research:
a. The RAND Appropriateness Study: Manipulation and Mobilization of the Cervical Spine
As it had for the low back pain study, the RAND Corporation conducted both a literature review and a multidisciplinary panel appropriateness study for cervical spine, headache, and upper extremity disorders. With regard to the cervical spine, the RAND literature review suggested that short-term pain relief and enhancement of the range of motion might be accomplished by manipulation or mobilization in the treatment of subacute or chronic neck pain; literature describing acute neck pain was regarded as scanty [210] and remains abbreviated to this day.
As in the earlier low back study, [152155] the appropriateness of chiropractic cervical spinal manipulation was assessed by an expert multidisciplinary panel, rating an array of more than 1,400 clinical scenarios for appropriateness of chiropractic intervention. In the final ratings, panelists rated 41% of all conditions as appropriate and 43% as inappropriate for chiropractic with disagreement on only 2% of all conditions. [211]
b. Other studies
Leaping ahead from the RAND study to the most current assessment, a special Neck Pain task force recently commissioned by the Bone and Joint Decade [20002010] conducted a critical review of the literature published between 1980 and 2006 to assemble the best evidence associated with neck pain and related disorders. Regarding noninvasive intervention strategies, 359 relevant papers were retrieved with 170 accepted as scientifically admissible. For neck pain excluding whiplash,[i] manual and supervised exercise interventions,
[ii] l ow-level laser therapy, and
[iii] possibly acupuncture were regarded as more effective than no treatment, sham, or alternative interventions.Regaining function as soon as possible was considered to be a key component of those treatments found to be most effective. [212]
Leading up to this comprehensive review were several intervening studies with a trend toward superiority in patients who experienced spinal manipulation in treatment. A randomized controlled trial conducted in 1993 by Koes revealed that, for subacute and chronic neck pain, the trial receiving the highest rating indicated that, for neck and back complaints together, improvements in severity of the main complaint were larger with manipulative therapy than for physiotherapy; for neck complaints only, the mean improvement in the main complaint as shown by the visual analog scale was slightly better for manipulative rather than physical therapy. [213] A trial authored by Cassidy one year earlier, studying 100 subjects with unilateral neck pain with referral into the trapezius, revealed that immediately after the intervention, 85% of the manipulated group and 69% of the mobilized group reported pain improvement. The decrease in pain intensity was more than 1.5 times greater in the manipulated group. [214] Improvements of 44% in the visual analogue scale and 41% in head repositioning were apparent in the manipulated group in a randomized clinical trial conducted by Rogers, as opposed to the respective values of 9% and 12% in the control group. The author suggested that there may be a possible effect of manipulations on proprioception in patients with chronic neck pain. [215]
Other trials failed to attribute superior effects to high-velocity spinal manipulation per se. Although improvements were observed, differences between the two interventions [chiropractic; physiotherapy] specified in the Skargren study [216] or between the three interventions [chiropractic; physiotherapy, intensive training] used by Jordan [217] could not be detected.
Yet the overall trend toward improvement with manual therapy as a whole in research conducted over the past 15 years is unmistakable. Hoving demonstrated in a trial with 183 patients that manual therapy which employed passive movements, specific articular mobilization, coordination, or stabilization techniques yielded advantages over matched 6week treatment regimens which specified physical therapy [exercise therapy, manual traction, stretching, massage, heat or interferential current] or continued care by general practitioners. [218]
Against a cohort of chronic neck pain patients given a comparable examination without intervention, a group of individuals with the same condition who experienced a pragmatic regimen of 1525 chiropractic treatments over a 5week period yielded significantly lower pain scores with greater head repositioning accuracy. The conclusion was that chiropractic care including high- and low-velocity amplitude techniques, myofascial release, and spine-stabilizing exercises could be effective in reducing pain of cervical origin--as well as proprioceptive sensibility. [219] The keyword here may be "chronic," for it has been found in recent systematic reviews that the literature supporting the effectiveness of spinal manipulation in managing acute neck pain remains limited [220] or inconclusive, [221] while if chronic patients are included the level of evidence rises to "moderate" if[i] manipulation or mobilization are compared to general practitioner care for short-term pain reduction of pain,
[ii] mobilization is compared to care from a family physician or physical therapist. [221]Considering the role of exercise, a clearly beneficial effect could be shown in one systematic review when it was coupled to manipulation or mobilization. Distinct benefits could be demonstrated in one group of patients receiving this combined treatment against a waiting list control for acute, subacute, or chronic mechanical neck disorders with regard to pain reduction, improvement of function, or global perceived effects. No such superiority could be seen if exercise was omitted. [222] A trend toward improvement by adding exercise to spinal manipulation could also be seen in one randomized clinical trial involving treatments over 11 weeks. [223]
c. Whiplash research
The problem facing both diagnosticians and victims facing whiplash is that most moderate to severe cases are invisible upon standard medical examination. As elusive as the "smoking gun" might be regarding this condition, it involves a broader array of soft tissue, neurological, and temporomandibular joint problems than presumed only a decade ago. [224] In Quebec alone, the fact that whiplash in 1989 accounted for 20% of all traffic injury insurance claims with an average compensation period of 108 days [225, 226] led the Quebec Task Force on Whiplash and Associated Disorders to conclude that "neck pain is to the automobile what low back pain is to the workplace." [227]
The elusiveness of a definitive, reproducible pathology for whiplash-associated disorders [WAD] have often led the legal and insurance communities as well as the medical to erroneously conclude that there is no physical or organic basis for the symptoms of WAD. This has produced charges of malingering or litigation neurosis on the part of the patient, leading to the overlaying of psychosocial factors which have only compounded the problem.
Because WAD has been such an elusive target, the work of the Quebec Task Force has not been able to escape criticism. Freeman [228] has raised several objections to the Task Force Guidelines, including the following:
Near total elimination of relevant literature: The fact that 99.994% of all articles were eliminated before consideration raises a strong possibility that instructive as well as useless data were discarded.
Arbitrary recommendations: In the resulting absence of literature to consider, the Task Force gave its own opinion equal weight with primary research data, lending a misleading sense of robustness to its recommendations.
- [229236]
Propagation of the myth that most WAD patients recover in 612 weeks: Upon closer examination this time course has no basis no primary research; in fact, considerable data already cited contradicts this impression and paints a far bleaker picture.
The undertaking was sponsored by an insurance industry: SAAQ [Societe d'assurance automobile du Quebec] as the sponsoring organization of the entire project would be expected to have an "obvious and serious" interest in its outcome, possibly compromising the objectivity of the literature research, evaluation, and ultimate recommendations of the Task Force.
From a morphological point of view, immobilization of the neck following the soft tissue trauma which accompanies WAD is indefensible. Severe soft tissue injury [rupture of muscles, joint capsules, and synovial folds] can be expected around the cervical spines of accident victims. [229] Consequently, scar formation, cross-linking of collagen fibers, and adhesions might be expected to result in traumatized soft tissues that were not rehabilitated soon after injury. Specifically:
- [231, 232]
Healing without proper motion will cause a disorganized matrix to appear, with adhesions and unnecessary scar formation.
- [232]
Early exercise and joint motion in rehabilitation produces a better collagen concentration, which is superior to scar tissue.
- [233, 234]
Improved tensile strength is observed in the collagen deposit when proper rehabilitation takes place after injury.
- [235] With decreased vascularization, rapid degeneration of the muscle spindles occurs -- with subsequent revascularization changing their shape and neural innervation. [236]
If venous blood supply to paraspinal muscles is depressed for 2 hours [which might be anticipated in some soft tissue injuries], irreversible muscle damage occurs.
One would thus conclude that a plausible rationale exists for managing whiplash by spinal manipulation; however, the outcomes evidence in support of this remains limited. One study demonstrated that, in subjects whose side bending of the neck was asymmetrical and who had a history of neck trauma and frequent episodic neck stiffness, a single lower cervical adjustment delivered to the side of the most restricted movement was capable of reducing the extent of asymmetry, but only briefly (for periods less than 48 hours). [237] A second investigation involving 93 patients in a retrospective review by structured telephone interviews indicated that those with restricted range of neck movement following whiplash injury were the most likely to improve after chiropractic manipulation. Many patients had received previous treatments, particularly physiotherapy. [238] Additional supporting evidence might be inferred from a prospective study of
23 patients with subacute whiplash-associated disorders who reported an increased cervical range of motion and reduced pressure-pain threshold after cervical spine adjustments, [239] as well as one case study involving an unstable C3/C4 motor segment following a lateral-impact motor collision. [240]
However, more recent systematic literature reviews have been mixed in their findings. The aforementioned Bone and Joint Decade Task Force on Neck Pain and Its Associated Disorders concluded that educational videos, mobilization and exercises seem to be more beneficial than usual care or physical modalities. [212] On the other hand, another systematic search from various databases from January 2000May 2006 accepted only 9 studies out of 290 screened and concluded that, because of vague and inadequate explanation of results in several instances, that there was not enough evidence to suggest that spinal manipulation is an effective treatment for whiplash. [241]
3. Headache Research:
The treatment of headaches with spinal manipulation has generated a proliferation of research in the peer-reviewed literature, reflected in part by multiple outcomes research designs. At least 13 randomized clinical trials have been reported, [186, 242254] the remainder being case series, retrospective series, or prospective series. [255265] These have been amply summarized by five literature reviews, [266270] four of them systematic. [266269] Additional basic research which will be addressed below [271274] describes a possible mechanism of cervicogenic headache and as such provides compelling support to the wisdom of considering chiropractic intervention as a key strategy for the management of headaches.
Published studies have generally classified headaches into three major groups, as recommended by the International Headache Society. [275]
a. Tension Headache
Figure 8: Outcomes of Tension-type Headache Patients in Clinical Trial: Spinal Manipulation vs Amitriptyline [186]
The most dramatic of the trials pertaining to tension headaches [186as published in 1995. A group of 70 patients who were administered chiropractic health care over a 6week period displayed parity to a cohort of 56 patients who were administered amitriptyline [a leading medical intervention for headache treatment] over the same period, in terms of four primary outcome measures [headache frequency, total headache pain, OTC medication use, and global health]. More significantly, during the 4week followup period, patients undergoing spinal manipulation maintained their improvements while medicated patients reverted to baseline values [FIGURE 8]. What this result implied was that spinal manipulation rather than one type of medication had the potential of conferring benefits to headache patients that were more long-lasting. Of profound importance is the fact that this particular study was rated the highest in quality of all trials compared in the three independent systematic literature reviews mentioned earlier. [266268]
The enhanced consequences of chiropractic management in the treatment of tension headaches is supported by two other randomized controlled trials, [243, 244] although sample sizes were smaller so as to blunt the statistical analyses of these particular results. High-velocity thrusting did not seem to confer additional benefits upon patients given massage and trigger-point therapy, as shown in one other trial by Bove and Nilsson. [245] Even though this particular investigation would suggest that high-velocity thrusting confers no additional benefits for managing tension headache, it is clear that both groups of patients which had been administered massage [an arguable component of chiropractic management] showed significant and indistinguishable improvements over baseline values in all the outcome measures observed. The danger of misinterpretation arises when chiropractic healthcare is equated with only one of its elements [high-velocity manipulation].
Outcomes obtained in nonrandomized clinical research are similarly supportive. Mootz reported improvements in frequency, intensity, and duration in 11 patients subjected to cervical manipulation, cold packs, and trigger point therapy. [255] Droz, on the other hand, witnessed improvements in pain in a large cohort of 332 patients administered spinal manipulative therapy. [256]
Figure 9: Connective Tissue Bridge Between Rectus Capitus Posterior Minor Muscle and Apinal Dura [272]
As pointed out earlier [Section III], not all research evidence which supports the wisdom of a particular healthcare intervention comes to us from outcomes research. Sometimes a clarification of what appears to be an underlying mechanism provides an invaluable complement to effectiveness studies observed in traditional clinical trials. Nowhere is this more evident than in the recent discovery from direct tissue dissections of what appears to be a connective tissue bridge between the rectus capitus posterior minor muscle [RCPM] and the dorsal spinal dura at the atlanto-occipital junction.
According to Gary Hack and his coworkers, the dura-muscular connection transmits forces from the cervical spine joint complex to the pain-sensitive dura. Trauma to the upper spine could then result in atrophic changes in the RCPM. Consequently, adverse tension in the spinal dura could further substantiate the role of spinal manipulation as a means to alleviate this tension and offer valuable support to the effectiveness of SMT as a viable treatment for cervicogenic headache. [271] These structural relationships are demonstrated in FIGURE 9. [272]
Support for this model is shown in a parallel study in which 31 out of 39 consecutive patients who underwent plastic surgical forehead rejuvenation procedures encompassing resection of the corrugator supercilli muscle displayed total elimination or improvement of migraine headache, with improvements lasting at least 47 months. [273] Thus it is quite possible that various types of headache are at least in part triggered by tension of various muscular bridges, the relaxation of which [presumably by spinal manipulation] could bring about substantial relief from the original complaint. The idea that such a multiplicity of muscular bridges exist is supported by the findings of Humphreys, who demonstrated the existence of the ligamentum nuchae in addition to the rectus capitus muscle, anchored between the occipital bone and the C1 vertebra. [274]
f. The Duke Headache Evidence Report
To verify the clinical outcomes evidence supporting spinal manipulation and a variety of other physical and behavioral interventions in the management of headache, the Agency for Health Quality and Research began a process of systematic review of the literature that was virtually identical to that completed with the release of guidelines pertaining to low back pain, as discussed earlier. [5] Unfortunately, funding cuts to the agency caused this process to be aborted after the headache literature review had begun, and the work of the multidisciplinary committee charged with performing the literature evaluation and developing ratings of the evidence was ultimately shipped to the Duke Center for Health Policy Research and Education for safekeeping.
It was at this juncture in which I, with funds from the National Chiropractic Mutual Insurance Company, was able to mandate that an updated systematic literature review of tension and cervicogenic headache be done, taking into account the rapid proliferation of new literature to be grafted onto the work of the disbanded headache committee. This new undertaking led the staff at the Duke Center to screen citations from the literature, abstract the data into evidence tables, analyze the quality and magnitude of results from these studies, and draft an evidence report with peer review from a panel of 19 experts representing a broad, multidisciplinary coalition of healthcare providers.
Starting with over 2500 citations from such sources as MEDLINE, MANTIS, CRAC, CINAHL, PsychoINFO, the Cochrane Controlled Trials Register, and additional articles obtained by referral, the panel obtained bibliographies of both physical and behavioral options for treating headache which were either prospective, controlled trials aimed at either relief from or prevention of attacks of tension-type or cervicogenic headache. Among the physical interventions reviewed in this report were:[i] cervical spine manipulation,
[ii] low-force techniques [such as cranial sacral therapy, massage (including trigger point release)];
[iii] mobilization;
[iv] stretching;
[v] heat therapy;
[vi] ultrasound;
[vii] transcutaneous electrical nerve stimulation (TENS)];
[viii] surgery; and
[ix] exercise (including those that are postural].Among the behavioral interventions reviewed were:
[i] relaxation;
[ii] biofeedback;
[iii] cognitive-behavioral [stress management] therapy; and
[iv] hypnosis.The final report, which gave copious recognition to much of the chiropractic research headache literature cited earlier, [242270] was significant in that it concluded that non-pharmacological treatments are of growing importance and, "if effective and available...[they] may be the first choice for most patients. " Furthermore, it indicated that drug treatments are not suitable for all patients, may produce undesired side effects, and are not universally effective. [277] The importance and high credibility of this document lay in the facts that
[i] Duke is one of 12 research centers given trademark status by the U.S. Department of Health and Human Services,
[ii] the 19 member interdisciplinary panel that performed the literature review was of extremely high caliber, and
[iii] the evidence review was comprehensive -- encompassing all behavioral and physical treatments for both tension-type and cervicogenic headache.
4. Extremities:
Manipulation of the musculoskeletal system for treatment of pain and reduced motion is not limited to the back or neck. Over the past decade, the extremities have become increasingly recognized as an area responsive to manual therapy. This is supported by reports which indicate that upper and lower extremity problems account for up to 20% of all chiropractic care, half of which pertains to lower extremity pain and injury. [278282] Indeed, the treatment of extremities is the second most frequently applied procedure within the chiropractic profession. [278]
a. Upper extremities
The shoulder girdle, for example, may be amenable to such treatment. One clinical trial in The Netherlands randomized 150 patients with shoulder symptoms and dysfunction were randomized into groups receiving either usual medical care [information, oral analgesics, NSAIDs, corticosteroid injections, referral to physiotherapy] or high-velocity low-amplitude manipulations in addition to the medical regimen over a 12-week period. After 12, 26 and 52 weeks, distinct advantages in the manipulated cohort were reported in severity of the main complaint, shoulder pain and disability, and general health. The conclusion was that spinal manipulation accelerated the recovery of shoulder symptoms. [283]
Compression of the median nerve within the vicinity of the wrist may lead to unilateral or bilateral paresthesia in the fingers, with or without pain in the wrist, palm, and/or forearm proximal in the area of compression. This condition, known as carpal tunnel syndrome [CTS], presents a variety of symptoms and is commonly confused with tendinitis. One of its major causes is the protracted strain on an extended or flexed wrist caused by repetitive stress, often found in the workplace and therefore having the potential to affect a significant population.
The rationale for manipulation is to take pressure off the transverse carpal ligament and add adjustments of the lunate to help decompress the tunnel. It represents a departure from traditional spinal adjustment; in its application to the extremities instead, it provides a conservative, noninvasive alternative to surgery. [284]
A systematic review of upper extremity conditions performed on the CINAHL, MEDLINE and MANTIS databases yielded 64 articles, including 6 clinical trials, 14 case reports for the wrist and hand, 8 case reports for the elbow, and 36 case reports involving the shoulder. Although the level of evidence overall was judged to be extremely modest, what was most striking was that the chiropractic treatment was multimodal in nature, involving both the spinal and peripheral structures and using both joint and soft tissue methods. This was judged to be at odds with the general perception of other healthcare providers that chiropractors employ mostly manipulative methods of treatment. [285]
Although few in number at the present, the randomized clinical trials addressing CTS offer encouragement in that discrete improvements in a broad cross-section of outcome measures [physical and mental distress scores, nerve conduction, vibrometry, and pain scores] in patients compared to their initial conditions are noted in all groups undergoing manipulative therapy. Their improvements were comparable to those achieved by ibuprofen [286] physical therapy or corticosteroid injection. [287] In the latter trial plus one additional investigation, [288] manipulative therapy displayed the potential to accelerate improvement in certain groups of patients, although corticosteroid injections produced more rapid improvements in patients with diagnosed disorders in synovial structures as opposed to functional disorders of the cervical spine, upper thoracic spine, or the upper ribs [the shoulder girdle]. [288]
Case series designs addressing manipulative therapy for carpal tunnel syndrome have also yielded encouraging results. A series of 22 volunteers screened for CTS by electrodiagnostic characteristics, symptoms, and physical examination received either manual soft tissue mobilization or soft tissue mobilization assisted with Graston instruments. Improvements to 3 months were observed in nerve conduction latencies, wrist strength, wrist motion, and subjective evaluations of signs and symptoms of CTS. [289] A second cohort of volunteers at least 60 years of age who suffered from upper extremity [hand, wrist, or shoulder] dysfunction experienced manual manipulation, mobilization, and ancillary treatments [soft tissue procedures, McKenzie physical therapy assessment, application of ice and heat, treatment with home stretching, postural exercises] 13 times per week over a 5week period and reported improvements in self-reported pain and functional status. [290]
Case control studies supporting chiropractic intervention in the management of this condition suggest that, in 38 subjects, a broad array of dietary, exercise, and manipulative interventions result in statistically significant improvements in several strength measures of up to 25% over pretreatment values; [291] improved objective pain and distress levels were observed in 22 returning subjects to persist for at least 6 months post-treatment. [292]
Osteopathic manipulation has also been shown to be effective in two case series studies by Benjamin Sucher. The first, involving four patients with CTS, showed both clinical improvement and changes in MRI imaging that revealed that the anteroposterior and transverse dimensions of the carpal canal increased significantly after treatment. EMG/NCS measurements were able to document electrical improvement consistent with the clinical recovery. [293] Both clinical and electrical improvement were subsequently observed in a larger group of 16 patients with CTS. [294]
b. Lower extremities
Two extensive literature reviews regarding manipulative therapy and the lower extremities have recently been published, one by Hoskins [295] and the other guided by the conclusions of the Council on Chiropractic Guidelines and Practice Parameters [CCGPP] and being more limited by defining chiropractic treatment using applied manipulative therapy with or without adjunctive treatment. [296] The CCGPP study was particularly comprehensive with its inclusion of randomized controlled/clinical trials, case series, and case studies, as well as in its judicious weighing of the implications of such features as the introduction of innovative concepts or insights, or the absence of intention-to-treat analyses.
In the 39 studies [8 for the knee, 7 the ankle, 2 the foot, and 1 the hip] reviewed in the CCGPP study, levels of evidence were judged to be "fair" if(a) there were studies of appropriate design of sufficient strength, but there were inconsistencies or minor doubts about generalizability, bias, design flaws, or the adequacy of sample size, or
(b) the evidence was gleaned from weaker designs but confirmed in separate studies.
Evidence was "limited" if there were either(a) studies with substantial uncertainty due to design flaws or adequacy of sample size, or
(b) a limited number of studies of weak design for answering the question addressed.Brantingham and his coauthors concluded that the evidence was "fair" for manipulative therapy of the knee and/or full kinetic chain, and or the ankle and/or foot combined with multimodal or exercise therapy for knee osteoarthritis, patellofemoral pain syndrome, and ankle inversion sprain. Evidence was deemed to be "limited" for manipulative therapy combined with multimodal exercise therapy for hip osteoarthritis. [296]
This was not to be construed as a discouraging result, as Brantingham concluded overall that "the present studies for lower extremity disorders appear to parallel the results and overall beneficial outcomes per spinal research." [163, 228] Indeed, the table has been effectively set for a broader consideration of what constitutes the musculoskeletal disorders amenable to chiropractic care, for the author has suggested that "it may be useful to investigate the most effective methods of manipulation/mobilization for every joint in the human body [italics mine]." [296]
C. Non-musculoskeletal:
1. Observed as a "by-product"
An early systematic indication that non-musculoskeletal as well as musculoskeletal conditions were responsive to chiropractic care came from a study of 87 Swedish Chiropractic Association members, each of whom surveyed 20 consecutive adult patients whose chief complaint was musculoskeletal in nature. Treatments included a spinal adjustment or manipulation. What was found was that 23% of these patients reported at least one positive benefit, which extended beyond the musculoskeletal system, the most common involving the respiratory and digestive systems. The percentage of individuals reporting non-musculoskeletal improvements increased steadily with the number of spinal areas treated. [297]
These findings were confirmed and extended by an international research consortium, which extracted data from 385 chiropractors and 5,607 patients from 7 countries [Canada, United States, Mexico, Hong Kong, Japan, Australia, and South Africa] in a cross-sectional survey, revealing similar proportions of chiropractic patients originally seeking treatment for a musculoskeletal condition who reported improvements in nonmusculoskeletal complaints after treatment. Similar to the preceding Swedish study, most common were improved breathing [27%], digestion [26%], circulation [21%], and resolution of tinnitis [19%]. [298]
2. Infantile colic
First described in 1894 as dyspepsia, infantile colic has most recently been described as the unexplainable and uncontrollable crying in babies aged 03 months for more than 3 hours per day, more than 3 days a week, and more than 3 weeks. Some studies have described flexing of the knees against the abdomen with clenching of the fists and extension of the trunk or extremities. [299] Although the condition has been regarded to be self-limiting and benign, its effect upon parent-child relationships can be construed to be stressful if not damaging.
To buttress years of promising clinical observations, a number of interventions have recently been conducted [TABLE 8] [299305] with results for over 450 patients that are mostly supportive. All involve chiropractic spinal manipulation applied either by fingertip or a computer-assisted solenoid adjusting device. What is most dramatic is the comparison shown with a medical treatment -- the surfactant dimethicone [FIGURE 10] -- which not only produced a considerably lesser effect from 510 days after the start of treatment, but produced worsening of symptoms as was apparent in 7 of the medicated group of patients. [299] While the effects of manipulation compared to a hand-held placebo group did not appear to differ statistically in one study by Olafsdottir, a trend toward superiority in the numbers of patients affected is apparent. Furthermore, more of the manipulated group indicated "some" or "marked" improvement. [300] Elsewhere, a pilot randomized clinical trial suggested that the complete resolution of symptoms could be found in 93% of the subjects undergoing up to 6 treatment sessions over a 2week period. [301] What remains a matter of mystery is whether Olafdottir [315] adjusted areas of the spine that were different from those manipulated in the other randomized clinical trials, possibly accounting for the divergent results.
While spinal manipulation is usually associated with the treatment of musculoskeletal disorders, these data create two possible interpretations. As indicated by Wiberg, [299] either spinal manipulation has been shown to be effective in the treatment of a visceral disorder or infantile colic is, in fact, a musculoskeletal disorder rather than the visceral condition it is commonly assumed to be. In either case, these data provide further support for considering the use of spinal manipulation in treating specified pediatric conditions.
3. Enuresis
This condition has been described as having multifactorial origins. [306] It has been proposed that spinal joint dysfunction could disrupt the integration of somatic, spinal, parasympathetic and sympathetic nerve pathways--constituting a significant contribution to the patient's enuretic condition. Thus, clinical studies that have appeared in the literature involving over 200 patients, [307310] suggest that spinal manipulative therapy may play a role in managing this condition [TABLE 9]. The results of the randomized clinical trial [307] are difficult to ignore.
While the majority of cases did not appear to respond in one of the studies, [308] it was felt that more information could have been obtained in the presence of a control group given a sham procedure in a randomized controlled trial. In that particular study, the manipulated group did indeed display a significant improvement over its own baseline values while the placebo group did not. However, the mean pre- to post-treatment night frequency group for the test group compared with that of the control group was not quite statistically significant at the 5% level. [308] A larger sample size would most likely have created a statistically robust difference between the groups. In addition, despite its minuscule n of 1 design, Gemmell's study displayed a time-series improvement following manipulation which defied the natural course of improvement. [310] The remaining case study also reported significant improvement. [309]
4. Asthma
The typical control of asthma by medication is primarily through antiinflammatory agents [inhaled steroid or beta-2-agonists [bronchodilators], the last of which when used excessively may actually contribute to an increase of mortality and morbidity. [312] There has thus been a shift toward using anti-inflammatory agents; at the same time, questions have been raised as to whether alternative and less invasive means are available for controlling this condition.
Spinal manipulation has been proposed as an option for treating this specific condition primarily for two reasons. The first is that vertebral dysfunctions assumed to underlie chiropractic management could produce reflex irritations of the somatic and autonomic nervous system; second, from both a neurological and biochemical point of view, chestwall function or bronchial airway tone and/or responsiveness might be expected to be adversely affected by such a lesion -- leading to a increased risk for an asthmatic attack. [313]
Reduction or elimination of these joint aberrations might thus be expected to reduce the incidence of asthmatic events.
In addition to descriptive or anecdotal data which have reported a positive clinical effect of spinal manipulation for asthma, [314, 315] four randomized clinical trials plus a pilot, three cohort studies, one crossover investigation, and four case studies involving over 550 patients as shown in TABLE 10 offer measurable support for spinal manipulative therapy in the management of this condition. [113, 316328] Lung function improvements per se may not be detectable, [316, 319] but quality of life scores improved by 1028%, led by activity scale changes. [319] The largest randomized clinical trial to date, which is attempting to compare different manipulative techniques in the management of asthma, is currently underway in Australia. Although data on symptoms, quality of life and distress are forthcoming in this study, preliminary cortisol measurements indicate that with manipulation [as opposed to patients visiting but remaining untreated], cortisol levels decrease. [313] Immunoglobulin A levels, on the other hand, specifically increase in treated asthmatic patients. These results are noteworthy in that prolonged elevations of cortisol have been shown to be potentially life-threatening [including being a cardiovascular risk factor [110, 329] ], leading to the development of bronchial hyperresponsiveness and asthma. [330]
The apparently negative study appearing in The New England Journal of Medicine, stating that "the addition of chiropractic spinal manipulation to usual medical care for four months had no effect on the control of childhood asthma," requires further comment. This statement was based upon the failure of active and sham-manipulated patient groups aged 7 to 16 years to be differentiated in terms of their outcomes in both quality of life and airway function. What is indisputable is that there were major improvements from baseline to followup observed in each of the groups. [316] The problem arises when one considers what was actually done in the sham procedures. Prolonged applications to no less than 3 distinct anatomical areas [gluteal, scapular, cranial] to the patient were described. Admittedly, these were not high-velocity contact procedures, but this appears to obscure an important phenomenon. Two pieces of evidence strongly suggest that simple contact with patients through sham procedures may produce significant effects in terms of asthma relief. The first indicates that, with respect to the reflexive inhibition of the alpha-motoneuron pool in human subjects, sham and active manipulative procedures display little difference. This is to suggest that cutaneous receptors, muscle spindles, and joint mechanoreceptors individually or in concert are significantly affected by so-called sham procedures. [95] The second arises from studies of Field from the University of Miami, in which low-force massage as opposed to no contact with the patient was sufficient to elicit differential, beneficial responses in overcoming asthma symptoms, lowering anxiety scores, and reducing cortisol levels. [115] This more than anything else should indicate that physical contact with the patient is sufficient to trigger a cascade of physiological changes which Balon erroneously dismissed in his asthma study.
In this context, the reader must take note that chiropractic extends beyond high-velocity, low-amplitude adjustments. It encompasses a broad range of both high-velocity and low-force techniques together with ancillary procedures, many of which have obviously been embedded in the sham procedures described. In its attempt to craft a fastidious design, the Balon trial [316] appears to have missed the forest for the trees, by attempting to portray the essence of chiropractic care as the lack of differentiation between the sham and manipulated experimental groups.
A contrast between sham and experimental interventions is apparent in the osteopathic literature inasmuch as thoracic function tests display a difference between sham and active procedures in a crossover design. [321] Reductions in the use of medications are apparent after manipulations from the reports of several cohort and case studies. [322325, 328]
5. Dysmenorrhea/Premenstrual Syndrome
For over 250 patients, the outcome studies shown in TABLE 11 point out marked improvements in menstrual pain and distress associated with dysmenorrhea and premenstrual syndrome. [122, 123, 127, 331334] Particularly noteworthy are the results from the pilot study performed by Kokjohn, which indicated clear improvements for patients subjected to higher manipulative forces in a side-posture procedure. Here it was evident that such patients experienced reductions in pain and their menstrual distress survey scores as well as significant decreases of the prostaglandins associated with menstrual cramping. In this manner, both clinical outcomes and a physiological mechanism (as discussed above in section III.E.) were clearly associated with the high-velocity chiropractic intervention and not the sham procedure. [122]
The apparently negative outcome in one of the full-scale trials [123] is easily explained by a myriad of irregularities in its design. The problems begin with the eligibility requirements of patients, which in the larger study were relaxed in order to attain sufficient recruitment. The result was that patients were sometimes admitted having experienced no pain within the past 48 hours and did not have to forego exercises or NSAIDs for a blackout period prior to the trial, in contrast to what had been required in the pilot study which had far stricter admission requirements. [122] In the latter trial, only a single practitioner delivered sham and active treatments and, not surprisingly, the experiment delivered positive results [122] as opposed to the lack of significant differences between the treatment and sham groups in the full-scale trial. [123] The fact that multiple therapists delivered sham and active treatments with no confirmation of standardized training or uniformity of application of thrusts represents yet another liability of the full-scale trial. Taken together, the flaws in the larger study are of such a magnitude as to invalidate the entire study.
Less rigorous support for the effectiveness of manipulation in managing dysmenorrhea is offered in the remaining pilot investigation [127] as well as the randomized comparative study, the latter providing a different chiropractic technique. [334] For treating premenstrual syndrome, the supporting evidence is more tenuous but uniformly encouraging. [332334]
6. Otitis media
Otitis media is the term used to describe the inflammation of the middle ear, the region between the ear drum and the outer ear. Although still lacking a randomized clinical trial, a substantial body of evidence exists to support considering chiropractic intervention for managing otitis media. To begin, such standard medical treatments as antibiotics and tympanostomy tubes have been shown to have limited applications, serious complications, and in the case of antibiotics have often been irrationally prescribed. [335338]
TABLE 12 outines the results of large cohort and case studies for over 850 patients, offering support for the effectiveness of chiropractic or osteopathic manipulative therapy for treating this condition. [339347] It can be seen that the majority of otitis media cases treated with spinal manipulation appear to be resolved within 10 days, most responding to fewer than 5 adjustments [342344] and many requiring only one or two treatments. [342, 343] Particularly intriguing is the fact that patients with no history of prior ear discomfort were much more likely to show early improvement, avoiding the cost and time of further interventions. [342] Normalization of otoscopic and tympanographic results likely occurred more quickly in cases of acute rather than chronic otitis media as shown in two studies. [342, 343] Fewer surgeries and episodes of acute otitis media were also encountered by patients undergoing osteopathic manipulative treatments. [339] Mastoiditis [the chief complication of otitis media] occurs only 0.22% of the time, even without antibiotic treatment; [348] it behooves the physician to consider not only chiropractic spinal manipulation as a treatment option for otitis media, but as a possible first alternative in light of the more rapid responses achieved in acute cases.
7. Hypertension
A list of studies involving nearly 475 patients affected with hypertension undergoing spinal manipulation is provided in TABLE 13. Two each of randomized clinical trials, pilot studies, crossover designs, nonequivalent comparisons, case series, and case studies plus one cohort study often reveal significant decreases in blood pressure measurements, [131134, 137, 349356] One of the most dramatic decreases in both systolic and diastolic pressure [13 and 8 mm, respectively, at week 8] has recently been reported by Bakris for a low-force chiropractic intervention described as the National Upper Cervical Chiropractic Adjustment [NUCCA]. The rationale for this approach was that looping arteries at the base of the brain were observed in one study to lead to arterial compression of the left lateral medulla oblongata in 51/53 hypertensive patients. When vascular decompression of the medulla was performed in 42 of the 53 patients, a reduction in hypertension was observed in 76% of them. By changing the position of the Atlas vertebra by means of the NUCCA technique, effecting such a decompression, it was held that reductions in blood pressure would ensue. This hypothesis was borne out in that both substantial reductions of blood pressure and rotational displacements of the Atlas vertebra [the restoration of alignment] immediately followed NUCCA treatments. Of considerable importance are the facts that[a] 85% of the patients treated required only a single adjustment, and
[b] the effects persisted throughout the 8week duration of the study. [134]Because there was no variation of heart rate, it was proposed that changes in sympathetic tone were not responsible for the changes in blood pressure observed. [134] On the other hand, one of the principal drivers of blood pressure -- serum aldosterone -- was observed to decrease in one of crossover studies; [133] however, the actual blood pressure effect was extremely brief. The failure to register sustained lowerings in a few of the studies [133137, 350] might be attributable to the technique applied or the severity of the condition.
8. Heart rate variability
Linkages of spinal dysfunctions to cardiac function can be traced to the observations of Jarmel, [358] who drew from several sources in the literature suggesting that prevention of sudden cardiac death should be directed toward controlling neurophysiologic factors which could enhance ventricular vulnerabilty. [359362] One source of destabilizing neural input to the heart was proposed to be vertebral dysfunction, the correction of which could be of value in reducing susceptibility to sudden cardiac death. [358] Because spinal manipulation was suggested to relieve the neural irritation caused by vertebral dysfunction, [363, 364] the use of such an intervention for preventing or forestalling the events leading to cardiac mortality became a subject for further study. In particular, decreased heart rate variability in response to stress was linked to greater risks of mortality. [361]
What is intriguing is that heart rate variability (HRV, the analysis of beat-to-beat oscillations in heart rate) was once thought to be merely noise in an electrocardiogram. [365] But using a Fourier mathematical analysis, it was possible to translate the oscillations into frequency ranges, [365, 366] measured either within a 24 hour period using time domain statistical analysis or short-duration recordings of 5 minutes using frequency domain statistical analysis. A complete description as to how HRV can calculate a qualitative index of autonomic function, accurate reflecting the sympathetic and parasympathetic tone and sympathovagal balance, has been provided, with low frequencies (LF) linked to sympathetic activity. [367, 368]
HRV outcomes following spinal manipulation have been demonstrated with 60 patients, primarily with crossover randomized clinical trials (TABLE 14). Increases of frequency ranges which are indicative of greater sympathetic output to the heart were shown following either cervical (C2) [97] or thoracic [98] manipulation by Budgell. The same result was demonstrated in 3 patients by Welch in the thoracic region. Inexplicably, a decrease in LF activity, suggesting a relative increase in parasympathetic activity, was found by the same author after manipulations in the cervical region. [99] While opposing effects of manipulation regarding sympathetic and parasympaethic nervous system activity appear to be linked to manipulations of different regions of the spine, this particular finding needs to be repeated with a substantially larger cohort of patients before its apparent divergence from the results of Budgell [113] can be taken up in detail.
The remaining case study shown in TABLE 14 was not able to come to definitive conclusions regarding the power analysis of HRV. However, the establishment of more uniform heartbeats and the disappearance of trigeminal pulses which appeared in the electrocardiogram are noteworthy. [369]
9. Case study support
As has been noted in TABLES 814 [298300, 309, 310, 325328, 334, 345347, 355, 356, 369] and in more recent and progressive literature reviews, [296, 370] the results of case studies have often served as a beacon for guiding future, more rigorous clinical research designs. That said, numerous nonmusculoskeletal conditions not previously described or studied with larger numbers of patients have been reported to respond to spinal manipulative therapy. These are shown in TABLE 15, [371379] hopefully to guide larger clinical investigations in the future. In so doing, these case studies would have performed the same function as those which motivated all the studies previously described in this report pertaining to both musculoskeletal and nonmusculoskeletal conditions.
D. Cognitive changes:
Changes in the nervous system, as discussed above in Sections III.D. and IV.C.8., have implicated that alterations in central nervous system processing take place after spinal manipulation. This would be expected to affect both somatosensory transmission [93] and motor control. [380] A prospective double-blind randomized controlled trial involving 36 chiropractic students attempted to determine if cortical processing, as shown by response times to a mental rotation reaction-time task, is altered by spinal manipulation. After one high-velocity, low-amplitude upper cervical adjustment, subjects displayed an average decrease in mental rotation reaction times of 98 ms, equivalent to a 14.9% improvement. The effect was specific in cognitive processing as distinct from improving movement time by the fact that following adjustments there was no significant change a simple reaction-time task, which required a minimal amount of cortical processing. The evidence suggested that upper cervical adjustments may affect cortical processing. [381]
A similar experiment involving 10 patients aged 2446 from a private chiropractic practice involved moving a cursor onto a target appearing on a computer screen. The experimental group, which had one high-velocity, low-amplitude adjustment to areas of joint dysfunction, registered improvements of about 9%. The control group, undergoing a resting period after completing a baseline task, displayed only a 2% improvement. The validity of this observation was compromised by the fact that the control group consisted of only a single patient. Yet the implication, again, seemed to be that a spinal adjustment could influence motor behavior and/or cognition. [382]
V. Safety
A. Major complications: Relative risks of activities:
A number of studies have linked chiropractic manipulation to adverse events, the most serious and widely studied being strokes following dissections of the vertebral artery. [383388] Regarding the risks of cervical manipulation in producing vertebral artery dissections (VADs) several retrospective studies against large population bases have been conducted. As shown in TABLE 16 [389397] , a large sampling of such studies indicate that the number of serious complications or cerebrovascular accidents (CVAs) as established by researchers from both the chiropractic and medical professions ranges from 1 case per 400,000 manipulations to zero in 5 million. Data from the RAND Corporation suggests the rate of vertebrobasilar accident or other complications [cord compression, fracture, or hematoma] to be 1.46 per million manipulations, with the rates of serious complications and death from cervical spine manipulation estimated to be 0.64 and 0.27 per million manipulations, respectively. [266] A more recent retrospective review, involving the largest number of presumed cervical manipulations performed [134.5 million] over the longest period of time [10 years], used malpractice claims from the Canadian Chiropractic Protective Association. It revealed a total of 43 cases of neurological symptoms retrieved from patient records, 23 of which involved stroke. The total yield of strokes, therefore, was 23/134.5M, a frequency rate of 1 per 5.85 million [0.17 per million] cervical manipulations, equivalent to one stroke per 1430 chiropractic practice years or a stroke occurrence rate of one per 48 chirochiropractic practice careers. [396]
The risk estimates attributed to cervical manipulation are significantly less [by orders of magnitude] than those associated with various medical procedures and lifestyle activities as shown in TABLE 17. [266, 398404] In an exhaustive review of risk estimates from multiple phases of life, Rome points out that the substantially greater
risks attributed to the medical procedures have been deemed "acceptable" by the routine adoption of such terminologies as "risk-adjusted mortality rates" and "net clinical benefits." The problem becomes all the more ironic in that, in Rome's words, "there seems a reluctance to concede the application of these terms outside the medical profession." [405] The risks inherent in other lifestyle activities, also appearing to be readily accepted by the public at large, are apparent in TABLE 17 and again outweigh those associated with cervical manipulation by several orders of magnitude. In striking contrast to the dire media warnings about the risks of cervical manipulation in the media. [406411]
B. Study of the vertebral artery and artery wall:
1. Structural considerations
Figure 11: The Vertebral Artery between the Atlas and Axis vertebrae [60]
The vertebral and basilar arteries, comprising the vertebrobasilar system, supply blood to the posterior brain. The vertebral artery (VA) itself, emerges from the subclavian artery, passes through he transverse foramina of C6C1 to become the atlantal segment as it exits through the transverse foramen of C1. It is here that the atlantal segment abruptly bends from a vertical to horizontal orientation. It is at this juncture (Figure 11) at which the artery is believed to be most susceptible to injury related to sudden and/or extreme head movement. [412] Three layers from inside to out (tunica intima, tunica media, tunica adventia) comprise the cervical arteries, as shown in Figure 12. [413]
2. Mechanisms of dissection
As the layer which makes up the vessel lining, the tunica intima is more susceptible to tearing [413] and as such is the typical site of the initial defect which initiates a VAD. A typical developing dissection as shown in Figure 13A indicates the formation of an intimal flap following an initial tear, with the potential for the separation of layers caused by blood flowing into the breach. Further damage may be wrought by pulsatile pressure to the muscular layer causing further splitting of the intima and media during a dissection. Subintimal hemorrhaging may rupture back into the arterial lumen distally, creating a double (false) lumen ( Figure 13B). As blood accumulates within the separated vessel layers, a thrombus is created with further deformation of the intima and obstruction of blood flow (Figure 13C). If emboli detach from the primary thrombus, they may travel distally to block progressively smaller vessels in the brain (Figure 13D). [413]
Figure 13: Dissections of the Cervical Arteries [413]
Perhaps the most compelling information that needs to be brought forward to bring the debate about cervical manipulations into objective terms has to do with the fact that a significant number (and most likely the majority) of VADs happen to be spontaneous cervical artery dissections (sCADs). Numerous reports to be discussed below, addressing both the frequency of occurrence of VADs and their association with virtually any activity associated with turning the head, should reduce the utility of attributing strokes to cervical manipulations to virtually an academic exercise.
As shown in TABLE 18, the annual incidence of spontaneous VADs in hospital settings has been estimated to occur at the rate of 11.5 per 100,000 patients [414] The corresponding VAD incidence rate in community settings has been reported to be twice as high. [415, 416] Using an estimated value of 10 from the literature to represent an average number of manipulations per patient per episode, [417] it becomes apparent that the proposed exposure rate for CVAs attributed to spinal manipulation is equivalent to the spontaneous rates for cervical arterial dissections as reported. [414416] If the threat of stroke or stroke-like symptoms is to be properly assessed, therefore, at least half our attention needs to be directed toward the spontaneous events instead of primarily or solely upon spinal manipulation.
Furthermore, a large number of common lifestyle activities have been shown to be associated with cerebral ischemia [TABLE 19 A] [405] or VADs themselves [TABLE 19 B]. [418 All are decidedly nonmanipulative. By way of illustration, one recent investigation has described beauty parlor stroke syndrome and salon sink radiculopathy confirmed by both patient symptoms and blood flow velocities in the bilateral vertebral and carotid arteries as measured by a diagnostic ultrasound instrument. [419]
3. Role of homocysteine, its detection, and means to reduce its effects
For over 30 years, the amino acid homocysteine has been implicated as key component of atherosclerotic disease. [420428] More direct observations point toward the disruption of the structures of collagen and elastin in the arterial wall:
- [429]
In the majority of skin biopsies taken from patients with cervical arterial dissections, irregular collagen fibrils and elastic fiber fragmentations have been found.
- [429] and serine elastases, [430] directly or indirectly leading to the decrease in vitro of the elastin content of the arterial wall. The opening and/or enlargement of fenestra in the medial elastic laminae would be expected to lead to the premature fragmentation of the arteriaL elastic fibers and degradation of the extracellular matrix. [429, 430]
Homocysteine activates metalloproteinases
- [431]
Homocysteine has been shown to block aldehydic groups in elastin, inhibiting the cross-linking needed to stabilize elastin.
- [432]
The cross-linking of collagen may also be impaired by homocysteine.
- [426]
Experimentally elevated levels of homocysteine produce patchy desquamation of 10% of the aortic surface in baboons.
- [428]
Endothelium-dependent and flow-mediated vascular dilation is impaired in individuals with elevated levels of homocysteine.
- [433]
In cell culture experiments, addition of homocysteine into the medium induces cell detachment from the endothelial cell monolayer.
Yet even a tighter coupling between sCADs and increased amounts of homocysteine have been shown by the following observations:
- [434]
Patients undergoing sCADs are more than three times as likely as asymptomatic patients to yield plasma homocysteine levels exceeding 12 micromoles/L. They are also more than twice as likely to have elevated homocysteine as patients experiencing ischemic strokes without arterial dissection.
- [435]
CAD patients yield average homocysteine levels of 17.9 micromoles/L while asymptomatic patients report an average of 6.0 micromoles/L.
- [420]
Homocysteine levels exceeding 10.2 micromoles/L are associated with a doubling of vascular risk.
- [434] This metabolic block would be expected to cause homocysteine to accumulate intracellularly. [436]
A genetic defect in humans involving tetrahydrofolate reductase, the enzyme which produces the methyl-donating cofactor required to convert homocysteine to methionine, is associated with elevations of the rates of sCADs.
The striking association of homocysteine with sCAD raises the possibility that a relatively simple diagnostic test is at hand for determining patients at risk for sCAD and who would accordingly be advised to avoid cervical manipulation. Until recently, the gold standard methodology for determining plasma homocysteine has been high pressure liquid chromatography, gas chromatography and mass spectrometry. [437439] Fortunately, this cumbersome technology has recently been correlated with a much simpler enzyme conversion immunoassay [EIA]. [440] An even more rapid assay method by means of an automated analyzer is also available, requiring only microliter amounts of reagent and sample. [441] This essentially means that homocysteine levels can be determined in any number of clinical reference laboratories already established to measure blood analytes.
To date, the assessment options for vertebrobasilar artery risk each have significant drawbacks and as a whole have been unable to identify any particular factor that is useful for screening. [442, 443] Provocation tests in particular are problematic in that in several aspects they replicate the risks associated with cervical manipulation by requiring the placement of the head and neck in extreme extension and rotation [444] False negative findings compared to angiograms have been reported; [445] reliability and validity have not been reliably tested; [443] and the suggestion has been made that these tests be de-emphasized. [446] In the midst of this disorder, determining homocysteine levels as a predictor of arterial fragility seems to be a plausible, rapid and inexpensive procedure that is no more invasive than a routine blood glucose determination.
A more extensive discussion of spontaneous arterial dissections, the proposed involvement of homocysteine, and means to determine homocysteine clinically has been published elsewhere. In addition, there is evidence presented to suggest that homocysteine levels may be lowered by folate, raising the possibility that a commonly available vitamin might be of utility in forestalling or preventing a potentially life-threatening condition. [60]
C. Linking cerebrovascular accidents to manipulation
1. Risk factors
Although symptomatology of neck pain may mimic that of an incipient or ongoing VAD, the primary signal of arterial distress is a sudden onset of headache or neck pain which patients often report is unlike any experienced previously. Signs and symptoms of actual vertebrobasilar ischemia which should be regarded as further suggestions of an impending vertebrobasilar artery event are: [447]
- Diplopia or other visual problems
- Dizziness: vertigo or lightheadedness
- Drop attacks
- Dysarthria
- Dysphagia
- Ataxia of gait
- Nausea, possibly with vomiting
- Numbness
- Nystagmus
When considering a patient for neck manipulation, a number of risk factors should be weighed carefully before treatment is considered: [447]
- Dizziness, unsteadiness, giddiness, and vertigo
- Age <45
- Migraine
- Connective tissue disease:
- Autosomal dominant polycystic kidney disease
- Ehlers-Danlos Type IV
- Marfan Syndrome
- Fibromuscular dystrophy
- Recent infection, particularly upper respiratory
2. Other adverse events
Despite numerous reports which have suggested that spinal manipulation is capable of causing disk herniations and cauda equina syndrome (CES), [448451] estimates of the frequency of such events arising from spinal manipulations performed for any reason range from 1 in 1 million [405, 451] to 1 in over 100 million. [157, 452] A more recent systematic review of prospective and retrospective studies as well as review papers yielded a risk estimate of worsened disk herniation or CES to be less than 1 in 3.7 million, three to five orders of magnitude less than such accepted means of treating lumbar disk herniations as the use of NSAID medications or surgery. [453]
More minor and transient events attending chiropractic manipulation have been reported in the literature.
These have been of short duration, relatively infrequent, and rarely severe. A sampling of such incidents includes:
- [454]
Increased neck pain or stiffness
- [455]
Headache and radiating pain
- [397]
Lightheadedness, dizziness, fainting (incidence 16/1000)
- [397]
Headache, numbness, tingling in upper limbs (incidence 4/100)
- [455]
Severe headache (case reports, pediatric)
- [453]
Mid-back soreness (case reports, pediatric)
- [456]
Musculoskeletal soreness
- Tiredness, nausea, ringing in ears (incidence <8%)
[453]
3. Flaws in the Medical Literature
While much of the medical literature attempts to establish an association of spinal manipulation with adverse events, [382388] it fails to fulfill the basic principles of causality established over 40 years ago by Bradford Hill. [457] What is required to demonstrate true epidemiological causation is the satisfaction of all the following:
Strong associations with a diagnosis which is consistent across samples and groups
Temporal relationship of treatment and adverse event
Biological plausibility
Lack of conflict with alternative explanations
Demonstration that reduced exposure to the putative causal agent results in reduction or prevention of the adverse event.
In terms of the most severe events -- the VADs -- seven common flaws can be identified in the bulk of the medical literature which attempts to link VADs with spinal manipulation:
There is the failure to disclose that the majority of VADs are spontaneous, cumulative, or caused by factors other than spinal manipulation (TABLE 18).
There is the failure to disclose the potential benefits of the procedure, as must be done in reporting true risk-benefit ratios.
There is the failure to place the risks of manipulation in the context of those produced by other medical treatments or lifestyle activities (TABLE 17).
There is the failure to report the actual frequency of spinal manipulations administered.
There is the failure to account for the possibility that patients experiencing CVAs are reported more than once.
- [418, 447, 458]
There is the failure to report the rates of CVAs following manipulation by parties other than licensed chiropractors.
There is the blanket assumption that patients undergoing adverse events following a manipulation would fail to report such instances to either the attending chiropractor or appropriate authority.
The one major omission in numerous case-control studies which suggested that the incidence of strokes was greater in patients who had recently undergone spinal manipulations by a chiropractor compared to individuals who had not [387, 388] has thankfully and finally been addressed. In a study of 818 VBA strokes in a hospitalized population of over 100 million person-years, Cassidy and his co-workers demonstrated that strokes were just as likely to occur if patients with headache or neck pain visited a primary care physician rather than a chiropractor, suggesting that the cause of the stroke could not be plausibly associated with any element unique to chiropractic. More likely, the stroke was already in progress when any healthcare intervention was sought. [459]
To amplify this point even further by way of demonstration, a recent case control study of a patient with a nontraumatic episode of head and neck pain revealed the benefits of taking a careful case history before ordering any intervention. Here it was found that the patient displayed sufficient warning signs to warrant a delay in administering spinal manipulation. Within a week of watchful waiting, the patient experienced a CVA anyway. Again the implication was that factors resulting in a stroke were in progress at the time the patient first sought consultation from a healthcare practitioner. [460]
VI. Cost-Effectiveness Research
A. Rationale
Given that rising healthcare costs in America now consume 16% of the Gross National Product and that their inflation of nearly 8% in 2004 was almost triple the overall national inflation rate, [461] cost-effectiveness is clearly a major factor in assessing the capacity to deliver effective healthcare. When it comes to managing back pain as the leading condition treated by chiropractic, we are faced with daunting statistics when it comes to cash outlays. According to the 1998 Medical Expenditure Survey, for instance, it was shown that total health care expenditures for back pain were $90.7B, more than 15% of which represented the costs of prescription drugs. [462] In terms of spine care, annual expenditures rose 65% from 1997 to 2005 while the health status of individuals with spine problems failed to improve, indicating that the money invested in this pursuit was not returning a sufficient value. [463] And in terms of neck pain, no form of surgical surgery has been shown to be superior to nonsurgical care or watchful waiting. [464] Finally, Dr. Richard Deyo's comment on back pain has clearly raised a red flag concerning conventional care:"Calling a physician a back-pain expert, therefore, is perhaps faint praise -- medicine has at least a limited understanding of the condition. In fact, medicine's reliance on outdated ideas may have actually contributed to the problem." [465]
Consequently and fortunately, there is a body of research one can focus upon when it comes to the cost-effectiveness of chiropractic care.
B. Methodological concerns
Typically, initial chiropractic visits including a complete medical evaluation, diagnosis and treatment. Numerous comparisons have been made with the costs which would be encountered in visits to a medical physician. Here it is essential to note that most costs for chiropractic visits are included in the bill received from the chiropractor's office, whereas in the medical course of treatment, external costs such as[i] referrals to medical specialists including physical therapists,
[ii] the purchase of medications, and
[iii] laboratory tests, most costs from the medical provider per se are not.In actual figures, it has been shown that 80% of the total cost of chiropractic treatment is billed from the chiropractor, whereas only 20% of the total medical costs of treatment appear on bills directly from the medical physician. [466] Even though the total number of visits to a chiropractic office for treating a given episode may be numerous, therefore, the patient needs to be mindful of this accounting.
To begin with appraisal of cost-effectiveness studies, one must assess the minimal criteria and common deficiencies of cost-effectiveness studies. In reviewing cohort studies in occupational low back pain, Baldwin identifies 6 requirements: [467]
The sample must be identified immediately after the onset of pain.
The study must obtain data on the prior history of back pain.
Standardized outcomes measures must be collected.
The total costs of an episode of back pain must be measured accurately.
Costs must be evaluated from the viewpoint of a pre-identified payor.
Multivariate models must be used to control for patient differences.
Looking at the other side of the coin, Branson has cited 5 common deficiencies in investigations pertaining to cost-effectiveness: [468]
Patient characteristics (severity, chronicity) are not factored in.
Standardized diagnoses within or between providers is not controlled in retrospective studies.
Payments actually received as not the same as those billed.
There is an absence of all direct costs, such as
(a) all visits to the provider,
(b) prescription and nonprescription drugs or supplements,
(c) laboratory costs,
(d) diagnostic imaging,
(e) referral to specialists, and
(f) hospital costs.
There is a poor representation of indirect costs, such as
(a) workdays lost by the patient,
(b) retraining for replacement labor,
(c) caregivers to assist in domestic duties,
(d) iatrogenic events, and
(e) legal costs.
C. Leading types of studies
1. Workers' Compensation Data
Attention is immediately drawn as to how healthcare dollars might have been inappropriately spent for back pain in workers' compensation from disbursements recorded, in which benefits were disbursed by the State of Georgia to medical and chiropractic physicians from 20012004 according to the data shown in TABLE 20: [469] Here it can be seen that chiropractors received 1% or less of the funds paid to medical physicians and just 2.84.5% of the disbursements paid to physical therapists. Since low back pain has been proposed to represent 33% of all workers compensation costs and 16% of all workers compensation claims, [470] it is immediately apparent that chiropractic care may not represent a significant cost burden as suggested by such entities as the Workers Compensation Research Institute in their overall conclusions. [471, 472] Indeed, one of the major methodological concerns which compromises the data from the latter study group is that costs of providers other than chiropractors were split into separate categories, whereas all costs relating to chiropractors were bundled into a single entity. [471, 472]
Recent retrospective data from the Division of Workers' Compensation Claims in Florida revealed drastic savings when chiropractic was compared to non-chiropractic care for specific low back injuries during the period 19941999. Here total costs per claim were less than half for chiropractic care ($7,500 vs $16,500); the average time required to reach maximum medical improvement was 37% less (161 vs 219), and the average number of days required to return to work was reduced by 30% as well (77 vs 130). Incredibly and most shocking was the fact that, during this same period, utilization of chiropractors for such injuries decreased by 75% with at most only a 15% reduction of the number of cases treated by non-chiropractors. [473]
Much the same pattern was found in Texas. In this instance, the authors retrieved over 70 articles, reports, published studies, and treaties on the costs and effectiveness of chiropractic care and analyzed data on nearly 900,000 Texas Workers Compensation Claims from 19962001. Here chiropractors treated 30% of workers with lower back injuries but accounted for just 9.1% of the total costs and 17.5% of the medical costs, [474] mimicking the previously discussed results from Georgia [469] representing the disproportionately low benefits apportioned to chiropractors.
These same trends persisted in the state of North Carolina, in which a retrospective review of 96,627 claims between 1975 and 1994 archived by the North Carolina Industrial Commission produced the same compelling and ultimately unsettling data. Here it was shown that the treatment costs, total costs, and total time of disability for medical providers was $3,519, $17,673, and 176 days, respectively. The corresponding figures for chiropractic care, on the other hand, were just $663, $3,318, and 33 days. Just as shown previously, [469, 474] the utilization rates for medical (85.4%) and chiropractic (0.8%) providers were far from equal. [475]
Oklahoma yielded similar findings, in which a 41% savings in direct costs with expanded access to chiropractic care for lower back sprains and strains was demonstrated. In actual amounts, these savings translated to $14,190,011 annually. [476]
Similar findings could be extracted from studies overseas. Ebrall's study of the Victorian WorkCare Scheme in Australia from the early 1990s matched 998 medical with an equal number of chiropractic claims for patients with mechanical low-back pain and found that the number of compensation days was 392 when the provider was a chiropractor and 774 when the provider was a medical practitioner. The average compensation payment was four times greater with medical management ($1,569 vs $392). [477] Similar data from the WorkCover Authority in a neighboring province (New South Wales) during the same period revealed that the average chiropractic treatment cost for 20 randomly selected cases was $299.65, less than half the $647.20 average medical treatment cost per case. [478]
2. Databases from insurers and practitioners
Insurance companies often use larger databases, which are less prone to possible skewing by regional workers' compensation data. The challenge still exists however, that problems remain for all retrospective studies in that all claims filed require verification to be certain that they correspond to the actual conditions experienced and treatments rendered.
Several earlier studies from Utah, [479] Iowa, [480] and Florida [481] provided preliminary data which suggested a significant savings in costs when chiropractic was compared to medical care for back problems. Perhaps even more important was the fact (often neglected in cost-effectiveness studies as suggested above) that days lost from work were significantly less for patients under chiropractic care. [479481] Other early data from Oregon suggested that chiropractic care was more expensive and prolonged. [482]
A key conceptual advance representing the bundling of the full costs of episodes (i.e., the careful inclusion of all relevant treatment costs, not solely the costs of out-patient doctor visits) associated with either the medical or chiropractic care of patients was accomplished by Stano. Factoring in key patient demographic and insurance characteristics as well as case mix severity differences, Stano ran final cost comparisons in a total of 6799 patients from a total database of over 400,000. His conclusions were straightforward and dramatic. When all episodes of care were considered, the mean total costs were $1000 for each medical episode and $493 per chiropractic episode. [483]
Later observational studies by the same author at 13 general medical practices and 51 chiropractic, community-based clinics revealed higher rather than lower chiropractic costs. However, the data were misleading in that(a) the distributions of total costs were highly skewed, especially for the chiropractic group,
(b) prescription drug costs from the charts of medical patients may be underestimated,
(c) the costs for imaging or referral services rendered or independently sought by patients outside the sample providers' clinics were not included,
(d) a disproportionately high percentage of chiropractic patients (42%) paid out-of-pocket whereas only 7% of medical patients did so, and (e) costs for patients who might have undergone surgery were not considered. [484]The same authors revisited the issue of cost-effectiveness three years later with a cohort of 2780 patients visiting either 60 chiropractors or 11 medical doctors in their own offices and concluded that, although chiropractic costs continued to be higher, they were more than offset by the fact that clinically important differences in pain and disability improvement were found only in the chiropractic patients. Coupled with greater patient satisfaction and considering the importance of indirect costs as discussed above (Section VI.B), the authors now concluded that chiropractic care appeared to be relatively cost-effective for chronic patients. [485] The same conclusion regarding quality of life and cost-effectiveness of spinal manipulation was echoed in a much larger study in actual treatment settings in the United Kingdom. [486]
If chiropractors were admitted into an integrative service as gatekeepers in an Independent Physicians' Association (IPA), dramatic cost reductions were observed in several investigations. In a retrospective study over a 4year period by Sarnat, hospital admissions were reduced by 43% and hospital days were reduced by 58% with the average length of stay cut by 34% when comparisons were made to conventional health maintenance organizations which had not awarded primary care privileges to chiropractors. [487] In an updated study over a 7year period, the decreased utilization of hospitals, pharmaceuticals, and outpatient surgeries and procedures was sustained by chiropractors compared to medical providers. Actually, decreased utilization of more expensive and invasive medical procedures was uniformly achieved by all primary care providers whose orientation was toward complementary and alternative medicine, regardless of their licensure. [488]
Another perspective was offered by an insurance plan in a 4year retrospective claim analysis, comparing 700,000 health plan members with an additional chiropractic coverage benefit and 1M members of the same health plan without the benefit. Including the chiropractic benefit resulted in(a) lower annual total healthcare expenditures ($1,463 vs $1,671),
(b) lower average back pain episode-related costs for back pain patients ($289 vs $399),
(c) a reduction of claims through medical doctors, and
(d) lower utilizations of plain radiographs, magnetic resonance imaging, back surgeries, and hospitalizations.The savings were even greater than those reported because all pharmacy costs, costs of physical therapy on referral, and post-surgical patients were omitted. The sheer magnitude of the study group made this one of the largest analyses ever performed on the economic impact of chiropractic; however, it needs to be noted that this study was confined to one health plan in one state and that cause and effect have not been firmly established. Nevertheless, the trends of these data are undeniable. [489]
One corollary of this study was to ask whether adding the chiropractic benefit created an additional demand for medical care services, thereby adding significant costs. An investigative group from the same insurance firm responsible for the previous study [489] found that the presence of the chiropractic benefit did not appear to increase the number of patients seeking care for neuromusculoskeletal conditions, offering substantial refutation to this argument. [490] A second outgrowth of these investigations was to compute the actual costs of surgery, CT/MRI, plain-film radiography, and surgery for patients with or without the benefit. Those individuals with the benefit incurred reductions of costs in these categories from 225% for back pain and 1331% for neck pain. [491]
In viewing the cost of physician services through the lens of Medicare, similar advantages to chiropractic care could be found. Muse & Associates undertook an examination of the utilization, cost and effects of chiropractic services on Medicare program costs compared to similar data for beneficiaries treated by other provider types. Using data from a compilation from the Centers for Medicare and Medicaid Services, the study group compared the data from 1.5M who received chiropractic care against the remainder of the 5.8M total who did not. Beneficiaries who received chiropractic care had lower average Medicare payments per capita for all Medicare services ($4,426 avs $8,103), lower average Medicare payments per capita for the treatment of selected conditions ($380 vs $594), and fewer encounters with physicians. [492]
Finally, a more recent study which has captured more of the direct and indirect costs required for a comprehensive cost analysis as discussed above of medical services (Section VI.B) was provided in Europe, offering the additional benefit of a "bootstrapping" processing of costs which bypassed the assumptions required for conventional statistical analyses. In this study, patients undergoing manual therapy, physiotherapy, or conventional care from a general practitioner for neck pain were compared in a randomized clinical trial. The total costs of the manual therapy were one-third those of the other two groups; in addition, the manual therapy group displayed more rapid improvement in pain intensity, perceived recovery, and quality of life than the medical or physiotherapy cohorts for up to 26 weeks. [508]
D. An economist's evaluation of existing literature
Pran Manga, an economist at the University of Ottawa, has been twice commissioned by the Provincial Government of Ontario to assess the effectiveness and cost-effectiveness of chiropractic management of low-back pain. His assessment of the comparative cost data in his first report led him to conclude that:"There is an overwhelming body of evidence indicating that chiropractic management of low back pain is more cost-effective than medical management. We reviewed numerous studies that range from very persuasive to convincing in support of this conclusion. The lack of any convincing argument or evidence to the contrary must be noted and is significant to us in forming our conclusions and recommendations." [6]
The cost advantages for chiropractic for matched conditions appear to be so dramatic that Manga, in his second report, concluded that doubling the utilization of chiropractic services from 10% to 20% may realize savings as much as $770 million in direct costs and $3.8 billion in indirect costs. Four out of five patients of chiropractors have endured their problems for more than 6 months, typically undergoing medical care and/or physiotherapy before even reaching their chiropractor. [494]
VII. Wellness and Prevention
A. Significance in healthcare delivery
The reemphasis of healthcare upon preventive services has been widely regarded as essential if America's healthcare system is to survive into the future. The rising costs of healthcare, now exceeding 15% of the gross national product with outcome results which indicate that the United States has far less to show for its healthcare expenditures in terms of longevity and quality of life permit no alternative but to pursue prevention aggressively. A complete overhaul of healthcare delivery involving preventive health measures as an integral part has been strongly recommended in a recent report from the Institute of Medicine of the National Academies. [495] The persistence of public unawareness of the benefits of particular interventions plus the placement of practical obstacles for physicians being able to deliver effective services has been reported by a research group from McMaster University. [496]
B. Recent research
In terms of prevention and potential l cost savings, two studies involving elderly populations are difficult to ignore. As part of a comprehensive geriatric assessment program, the RAND Corporation studied a subpopulation of patients who were under chiropractic care compared to those who were not and found that the individuals under continuing chiropractic care were:
Free from the use of a nursing home [95.7% vs 80.8%];
Free from hospitalizations for the past 23 years [73.9% vs 52.4%];
More likely to report a better health status;
More likely to exercise vigorously;
More likely to be mobile in the community {69.6% vs 46.8%].
Although it is impossible to clearly establish causality, it is clear that continuing chiropractic care is among the attributes of the cohort of patients experiencing substantially fewer costly healthcare interventions. [175] This demands a closer look at the potential advantages of continuing chiropractic care for elderly patients.
A second review of a larger cohort of elderly patients across the United States compared direct expenditures [hospital care, physicians' services, nursing home] between groups of patients who were under maintenance chiropractic care and those who were not. Nearly a threefold savings of mean annual expenditures was reported as follows:
$ 3,105 : Maintenance care
- [497]
$10,041 : No maintenance care
Other studies involving preventive measures for non-elderly populations exist as well. One such investigation reviewed the consequences of implementing an on-site industrial chiropractic program which included the early detection, treatment, prevention and occupational management of musculoskeletal injuries 2 days per week. For the 21 months after implementation of the program, the total number of days of lost time, costs per claim, rate premiums, and especially the number of surgeries decreased dramatically. Cost savings from avoided surgeries alone amounted to $900,000 for these preventive measures. [498]
A second study recruited 59 adults aged 1827 from two elite Australian Rules football teams and randomized them into intervention and control groups. The control group was administered standard club, medical, paramedical and sports science management, including medication, surgery, manipulative physical therapy, massage, strength and conditioning, and rehabilitation. The intervention group included all these procedures and added pragmatic chiropractic management, involving manual therapies and/or soft tissue therapies to the spine, pelvis, and lower extremities at a minimum weekly frequency for 6 weeks, then one treatment for every 2 weeks for a 3month period. The chiropractic intervention resulted in the lower incidence of injuries to the hamstrings, lower limb muscles, and knees with far shorter periods of play missed as well. A lower incidence of overall back pain was also reported. [499]
Again the implications are that there may be considerable potential savings in direct costs spent for medical care with patients who are undergoing continuing chiropractic care on a maintenance basis. When return-to-work and other indirect costs are figured in (as implied in the Coulter study described above [175] ), far greater savings would be expected.
But perhaps the most persuasive data of all comes from a recent study [176] of patients with chronic low back pain who were divided into two groups, one receiving 12 treatments within a single month and the other adding to this regimen one treatment every 3 weeks for an extended 9 months (1214 additional visits). In terms of disability (as indicated by a modified Oswestry questionnaire), the group receiving the supplementary maintenance treatments continued to improve throughout the entire 10 month period, while the cohort lacking the additional visits reverted to baseline levels within that same period. This is clearly depicted in the Oswestry scores over a 10-month period as indicated in Figure 21. The authors of this study speculate that repeated chiropractic visits may have been the direct cause for the improvement of disability scores due to(a) improved trunk mobility, [193]
(b) facilitated release of entrapped synovial folds or relaxation of hypertonic muscle by sudden stretching, [500] or
(c) the disruption of articular or periarticular lesions. [501]
VIII. Conclusions
This discussion has attempted to review the position and potential of chiropractic research from a multiplicity of perspectives. It began with a historical review, together with a critical assessment of the state of what is currently called evidence-based medicine. When assessing the rationale for choosing a particular healthcare intervention, this discussion has, in its review of basic research, emphasized the importance of biological plausibility, since this turns out to be one of the basic elements of causation as established by Bradford Hill over 40 years ago. [457] Indeed, without the insights afforded by research in the basic science fields of molecular biology, microbiology, physiology, biochemistry, genetics, physics, and chemistry as well as anatomy, discoveries which have been of such a benefit to medicine over the past centuries would have been drastically curtailed.
Following a discussion of methodologies, the review of outcomes research was conducted from the viewpoints of both musculoskeletal and nonmusculoskeletal disorders which appear to have notable literature supporting the efficacy of chiropractic care in their management. Adhering to the basic tenet in medicine of Primum non nocere (First do no harm), this chapter reviewed a multiplicity of considerations regarding the safety of spinal manipulation, including an expanded discussion as to how a significant proportion of the incidents attributed to manipulation most likely originated from metabolic defects compromising arterial integrity. It became apparent that any risks of spinal manipulation, while remaining an objective which further research and best practices strives to reduce, are orders of magnitude less than those encountered for medical interventions treating the same or similar conditions managed by chiropractic.
In terms of practicality and accessibility of healthcare alternatives, the relative costs of medical procedures relating to conditions most commonly managed by chiropractic care needed to be reviewed. Differing experimental approaches -- many lacking attention to indirect costs -- were presented and assessed and provide a noteworthy rationale for elevating chiropractic management to a higher priority in the healthcare marketplace.
Finally, to conform with today's necessity to emphasize prevention and the maintenance of good health, instances in the literature in which chiropractic management was found to forestall or prevent further problems, disabilities, or expenses were reviewed. It goes without saying that preventive measures go hand-in-hand with substantially lowering overall healthcare costs.
The role of such research as has been reviewed in this chapter in establishing best practices for any healthcare intervention can never be underemphasized. It is sobering to note, for instance, in a very recent review of guideline recommendations to establish benchmarks for the quality of care in cardiology, Tricoci and his colleagues found that such advisories often rest upon lower levels of evidence or expert opinion. The proportion of recommendations for which there is no conclusive evidence was also found to be growing. [502 If guidelines for such invasive, costly, and procedures with relatively high risks for cardiology exist, one can only imagine that guidelines for conditions with lower mortalities might receive even less scrutiny. This is why the level of research evidence needs to be upgraded and perhaps revisited with more attention devoted to other types of research besides outcomes, the latter being often the only standard upon which the advisability of a particular mode of healthcare is commonly based. It is hoped that the multiple forms of consideration offered in this discussion provide a meaningful first step in that direction.
REFERENCES:
Meeker WC, Haldeman S.
Chiropractic: A Profession at the Crossroads of Mainstream and Alternative Medicine
Annals of Internal Medicine 2002; 136: 216227.
Wenban AB.
Is Chiropractic Evidence Based? A Pilot Study
Journal of Manipulative and Physiological Therapeutics 2003; 26(1): 47
Kirkaldy-Willis W, Cassidy J.
Spinal Manipulation in the Treatment of Low-back Pain
Canadian Family Physician 1985 (Mar); 31: 535540Chapman-Smith D.
The chiropractic profession: Basic facts, independent evaluations, common questions answered.
The Chiropractic Report September 2008; 22(5): p. 4.
Bigos S, Bowyer O, Braen G, et al.
Acute Low Back Pain in Adults. Clinical Practice Guideline No. 14.
AHCPR Publication No. 95-0642. Rockville, MD:
Agency for Health Care Policy and Research, Public Health Service,
U.S. Department of Health and Human Services. December 1994.
Manga P, Angus D, Papadopoulos C, Swan W.
A Study to Examine the Effectiveness and Cost-Effectiveness of Chiropractic Management of Low-Back Pain.
Richmond Hill, Ontario, CANADA: Kenilworth Publishing, 1993.
Rosen M. Back pain.
Report of a Clinical Standards Advisory Group Committee on back pain. May 1994,
London: HMSO.
Commission on Alternative Medicine, Social Departementete,
Legitimization for Vissa Kiropraktorer, Stockholm, SOU [English Summary] 1987; 12: 13-16.
Danish Institute for Health Technology Assessment:
Low-Back Pain - Frequency, Management and Prevention From an HTA Perspective
Danish Health Technology Assessment 1999; 1(1).
Thompson CJ.
Second Report, Medicare Benefits Review Committee, Canberra, AUSTRALIA:
Commonwealth Government Printer, June 1986, Chapter 10 [Chiropractic].
Hasselberg PD.
Chiropractic in New Zealand, Report of A Commission of Inquiry.
Wellington, NEW ZEALAND: Government Printer, 1979.
Gupta M.
A critical appraisal of evidence based medicine: Some ethical considerations.
Journal of the Evaluation of Clinical Practice 2003; 9: 111-121.
Coulter A, Entwistle VA, Gilbert D.
Sharing decisions with patients: Is the information good enough?
British Medical Journal 1999; 318: 318-322.
Sackett DL, Straus S, Richardson WS, Rosenberg WMC, Haynes B.
Evidence-based medicine: How to practice and teach EBM.
Edinburgh, SCOTLAND: Churchill Livingstone, 2000.
http://phpartners.org/tutorial/04-ebph/2-keyConcepts/images/4.2.7.1.jpg.
Downloaded 02/18/08.
Sackett DL.
Evidence-based medicine.
Seminars in Perinatology 1997; 21: 3-5.
Benson K, Hartz AJ.
A comparison of observational studies and randomized, controlled trials.
New England Journal of Medicine 2000; 342(25): 1878-1886.
Concato J, Nirav-Shah, Horwitz RI.
Randomized, controlled trials, observational studies and the hierarchy of research designs.
New England Journal of Medicine 2000; 342(25): 1887-1892.
Wallach H, Jonas WB, Lewith GT.
The role of outcomes research in evaluating complementary and alternative medicine.
Alternative Therapies in Health and Medicine 2002; 8(3): 88-95.
Tonelli MR.
The philosophical limits of evidence-based medicine.
Academic Medicine 1998; 73(12): 1234-1240.
Heany R.
Long-latency deficiency disease: Insights from calcium and vitamin D.
American Journal of Clinical Nutrition 2003; 78: 912-919.
Rosner A.
Fables or Foibles: Inherent Problems with RCTs
J Manipulative Physiol Ther 2003 (Sep); 26 (7): 460467Fisher CG, Wood KB.
Introduction to and Techniques of Evidence-based Medicine
Spine (Phila Pa 1976) 2007 (Sep 1); 32 (19 Suppl): S6672O'Connor A.
Using patient decision aids to promote evidence-based decision making.
EMB Notebook 2001; 6: 100-102.
Jonas W
The Evidence House: How to Build an Inclusive
Base for Complementary Medicine
Western Journal of Medicine 2001 2001 (Aug); 175 (2): 7980Holmes D, Murray SJ, Perron A, Rail G.
Deconstructing the evidence-based discourse in health sciences: Truth, power and fascism.
International Journal of Evidence Based Healthcare 2006; 4: 180-186.
Foucault M.
The Birth of the Clinic: An Archaeology of Medical Perception.
New York, NY: Random House, 1973.
Glasziou P.
Evidence based medicine: Does it make a difference? Make it evidence informed practice with a little wisdom.
British Medical Journal 2005; 330(7482): 92; discussion 94.
Rycroft-Malone J.
Evidence-informed practice: From individual to context.
Journal of Nursing Management 2008; 16(4): 404-408.
Vernon H.
Basic scientific evidence for chiropractic subluxation.
In Gatterman MI [Ed], Foundations of Chiropractic Subluxation.
St. Louis, MO: Mosby, 1995, pp. 35-55.
Royal Society of Medicine. The use of non-human animals in research: A guide for scientists. London, UNITED KINGDOM, Royal Society of Medicine, 2004, p. 1.
Henderson CNR.
Animal models in the study of subluxation and manipulation: 1964-2004.
In Gatterman, MI. Foundations of Chiropractic, 2nd Edition.
St.Louis, MO: Elsevier Mosby, 2005, p.53.
Hodgkin AL.
The conduction of the nervous impulse. Liverpool, England:
Liverpool University Press, 1964.
Stuhmer W.
Electrophysiological recordings from Xenopus oocytes.
Methods in Enzymology 1998; 293: 280-300.
Cramer G.D., Fournier J.T., Henderson C.N., Wolcott C.C.
Degenerative Changes Following Spinal Fixation in a Small Animal Model
J Manipulative Physiol Ther 2004 (Mar); 27 (3): 141154Sato A, Swenson RS.
Sympathetic nervous system response to mechanical stress of the spinal column in rats.
Journal of Manipulative and Physiological Therapeutics 1984; 7(3): 141-147.
Song, XJ, Gan, Q, Cao, J-L, Wang, Z-B, and Rupert, RL.
Spinal Manipulation Reduces Pain and Hyperalgesia After
Lumbar Intervertebral Foramen Inflammation in the Rat
J Manipulative Physiol Ther. 2006 (Jan); 29 (1): 513Wang ZB, Gan Q, Rupert RL, Zeng YM, Song XJ.
Thiamine, pyridoxine, cyanocoalbumin and their combination inhibit thermal, but not mechanical hyperalgesia in rats with primary sensory neuron injury.
Pain 2005; 114: 266-277.
Rauschning WJ.
Normal and pathological anatomy of the lumbar root canals.
Spine 1987; 12: 1008-1019.
Bakkum BW, Mestan M.
The effects of transforaminal ligaments on the size of T11 to L5 human intervertebral foramina.
Journal of Manipulative and Physiological Therapeutics 1994; 17: 517-522.
Hu JW, Vernon H.
Properties of neurons in the upper cervical dorsal horn that receive cervical afferent inputs in rats.
Proceedings of the International Conference on Spinal Manipulation 1991; 35-36.
Rydevik B, Myers RR, Powell HC.
Pressure increase in the dorsal root ganglion following mechanical compression closed compartment syndrome in nerve roots.
Spine 1989' 14: 574-576.
Bogduk N, Tynan W, Wilson AS.
The nerve supply to the human lumbar intervertebral discs.
Journal of Anatomy 1981; 132: 39-56.
McCarthy PW.
Studies into the innervation of the intervertebral disc.
Proceedings of the International Conference on Spinal Manipulation 1991; 213.
Groen GJ, Baljet B, Crukker J.
Nerves and nerve plexuses of the human vertebral column.
American Journal of Anatomy 188: 282-296.
Janse J.
Principles and Practice of Chiropractic: An Anthology.
Lombard, IL: National College of Chiropractic, 1976.
Mooney V, Robertson J.
The facet syndrome.
Clinical and Orthopedic Research 1976; 115: 149-156.
Engel R, Bogduk N.
The menisci of the lumbar zygapophyseal joints.
Journal of Anatomy 1982; 135: 796- 809.
Giles LG, Taylor JR.
Human zygopophyseal joint capsule and synovial fold innervation.
British Journal of Rheumatology 1987; 26: 93-98.
Cramer GD, Tuck NR, Knudsen JT, Fonda SD, Schliesser JS, Fournier JT et al.
Effects of side-posture positioning and side-posture adjusting on the lumbar zygapophyseal joints as evaluated by magnetic resonance imaging: A before and after study with randomization.
Journal of Manipulative and Physiological Therapeutics 2000; 23: 380-394.
Cramer GD, Gregorson DM, Knudsen JT, Hubbard BB, Ustas JA, Cantu JA.
The effects of side-posture positioning and spinal adjusting on the lumbar Z joints: A randomized controlled trial with sixty-four subjects.
Spine 2002; 27(22): 2459-2466.
Von Lanz T.
Uber die Ruckenmarkshaute: I: Die konstructive Form der harten Haut des menschlichen Ruckenmarkes und ihrer Bander.
Arch entwicklungsmech Org 1929; 118: 252-307.
Hack GD, Koritzer RT, Robinson WL, Hallgren RC, Greenman PE.
Anatomic relation between the rectus capitis posterior minor muscle and the dura mater
Spine 1995; 20: 2484-2486.
Mitchell BS, Humphreys BK, O'Sullivan E.
Attachments of the ligamentum nuchae to cervical posterior spinal dura and the laterial part of the occipital bone.
Journal of Manipulative and Physiological Therapeutics 1998; 21: 145-148.
Shinomiya K, Dawson J, Spengler DM, Konrad P, Blumenkopf B.
An analysis of the posterior epidural ligament role on the cervical spinal cord.
Spine 1996; 21: 2081-2088.
Alix ME, Bates DK.
g J Manipulative Physiol Ther 1999 (Oct); 22 (8): 534539
D'Attilio M, Filippi MR, Femminella B, Festa F, Tecco S.
The influence of an experimentally-induced malocclusion on vertebral alignment in rats: A controlled pilot study.
Cranio 2005; 23(2): 119-129.
Triano J.
The mechanics of spinal manipulation. In Herzog W [Ed].
Clinical Biomechanics of Spinal Manipulation. New York, NY:
Churchill Livingstone, 2000, pp. 92-190.
McGill SM.
Low back disorders.
In Evidence-based Prevention and Rehabilitation.
Champaign, IL: Human Kinetics, 2002.
Rosner AL.
Spontaneous Cervical Artery Dissections and Implications for Homocysteine
J Manipulative Physiol Ther 2004 (Feb); 27 (2): 124132Li YK, Zhang YK, Lu CM, Zhong SZ.
Changes and implications of blood flow velocity of the vertebral artery during rotation and extension of the head.
Journal of Manipulative and Physiological Therapeutics 1999; 22: 91-95.
Licht P, Christensen HW, Hojgaard P, Hoilund-Carlsen PF.
Triplex ultrasound of vertebral artery flow during cervical rotation.
Journal of Manipulative and Physiological Therapeutics 1998; 21: 27-31.
Mennell J.
Understanding manipulative medicine in general practice.
Journal of Manipulative and Physiological Therapeutics 1989; 12(3): 231-235.
Janes J, Hauser H, Wells BF.
Chiropractic Principles and Technic, 2nd Edition.
Chicago, IL: National College of Chiropractic, 1947.
Illi FWH.
The Vertebral Column, Life Line of the Body. Chicago, IL:
National College of Chiropractic, 1951.
Adams AA, Wood J.
Forces used in selected chiropractic adjustments of the low back: A preliminary study.
Research Forum 1984; 1: 5-9.
Kawchuk GN, Herzog W, Hasler EM.
Forces generated during spinal manipulative therapy of the cervical spine: A pilot study.
Journal of Manipulative and Physiological Therapeutics 1992; 15: 275-278.
Kawchuk GN, Herzog W.
Biomechanical characterization [fingerprinting] of five novel methods of cervical spine manipulation
Journal of Manipulative and Physiological Therapeutics 1993; 16(9): 573-577.
Triano J, Schultz AB.
Loads transmitted during lumbosacral spinal manipulative therapy.
Spine 1997; 22: 1955-1964.
Keller TS, Colloca CJ, Gunzburg R.
Neuromechanical Characterization of in vivo Lumbar Spinal Manipulation.
Part I. Vertebral Motion
J Manipulative Physiol Ther. 2003 (Nov); 26 (9): 567578Breen AC, Allen R, Morris A.
Spine kinematics: A digital videoflouorscopic technique.
Journal of Biomedical Engineering 1989; 11: 224-228.
Triano JJ, Schultz AB.
Motions of the head and thorax during neck manipulations.
Journal of Manipulative and Physiological Therapeutics 1994; 17: 149-155.
Lee M, Svensson L.
Effect of loading frequency on response of the spine to lumbar posteroanterior forces.
ournal of Manipulative and Physiological Therapeutics 1993; 16: 439-446.
Van G, Zoest G, Gosselin G.
Three-dimensionality of direct contact forces in chiropractic spinal manipulative therapy.
Journal of Manipulative and Physiological Therapeutics 2003; 26(9): 549-556.
Henderson CNR, Cramer GD, Zhang Q, DeVocht JW, Fournier JT.
Introducing the External Link Model for Studying Spine Fixation and Misalignment: Part 2, Biomechanical Features
J Manipulative Physiol Ther 2007 (May); 30 (4): 279294
Wardwell WI.
Chiropractic: History and Evolution of a New Profession.
St. Louis, MO: Mosby Year Book, 1992, pp. 78-82.
Triano J, Luttges M.
Subtle intermittent mechanical irritation of the sciatic nerve of mice.
Journal of Manipulative and Physiological Therapeutics 1980; 3(2): 75-80.
Israel V.
Changes in nerve physiology in the rat after induced subluxation.
M.Sc. thesis, summarized in Articulations Aug 1983; 9-10.
Christiansen J, Meyer J.
Altered metabolic enzyme activities in fast and slow twitch muscles due to induced sciatic neruopathy in the rat.
Journal of Manipulative and Physiological Therapeutics 1987; 10(5): 227-231.
DeBoer KF, Schutz M, McKnight ME.
Acute effects of spinal manipulation on gastrointestinal myoelectric activity in conscious rabbits.
Manual Medicine 1988; 3: 85-94.
Brennan PC, Kokjohn K, Triano JJ, Fritz TE, Wardrip CL, Hondras MA.
Immunologic Correlates of Reduced Spinal Mobility: Preliminary Observations in a Dog Model
Proceedings of the International Conference on Spinal Manipulation, 1991; 118121
Christiansen JA, Beals S, Burnham G, Magnani M, Urbanek S.
Enzyme changes in rabbit muscles due to chronic compressive nerve irritation.
Proceedings of the World Federation of Chiropractic Congress, 1991.
Gillette RG, Kramis RC, Roberts WJ.
Characterization of spinal somatosensory neurons having receptive fields on lumbar tissues of cats.
Pain 1993; 54(1): 85-98.
Hu JW, Yu X-M, Vernon H, Sessle BJ.
Excitatory effects on neck and jaw muscle activity of inflammatory irritant injections into cervical paraspinal tissues.
Pain 1993; 55: 243-250.
Sato A, Sato Y, Swenson RS.
Effects of morphine on somatocardiac sympathetic reflexes in spinalized cats.
Journal of the Autonomic Nervous System 1985; 12: 175-184.
Araki T, Ito K, Kurosawa M, Sato A.
The somato-adrenal medullary reflexes in rats.
Journal of the Autonomic Nervous System 1981; 3: 161-170.
Budgell B, Holtz H, Sato A.
Spinovisceral reflexes evoked by noxious and innocuous stimulation of the lumbar spine.
Journal of the Neuromusculoskeletal System 1995; 3(3): 122-131.
Sato A, Sato Y, Shimado F, Torigata Y.
Change in gastric motility produced by nociceptive stimulation of the skin in rats.
Brain Research 1975; 87: 151-159.
Cauwenbergs P.
Vertebral subluxation and the anatomic relationship of the autonomic nervous system.
In Gatterman MI [Ed]. Foundations of Chiropractic Subluxation.
St. Louis, MO: Mosby-Year Book, Inc., 1995, pp. 234-266.
Song XJ, Xu DS, Vizcarrra C, Rupert RL.
Onset and recovery of hyperalgesia and hyperexcitability of sensory neurons following intervertebral foramen volume reduction and restoration.
Journal of Manipulative and Physiological Therapeutics 2003; 26(7): 426-436.
Song XJ, Vizcarra C, Xu D-S, Rupert RL, Wong Z-N.
Hyperalgesia and neural excitability following injuries to central and peripheral branches of axons and somata of dorsal root ganglion neurons.
Journal of Neurophysiology 2003; 89: 2185-2193.
Indahl A, Kaigle AM, Reikeras O, Holm SH.
Interaction between the porcine lumbar intervertebral disc, zygapophyseal joints, and paraspinal muscles.
Spine 1997; 22: 2834-2840.
Zhu Y, Haldeman S, Starr A, Seffinger MA, Su SH.
Paraspinal evoked cerebral potentials in patients with unilateral low back pain.
Spine 1993; 18: 1096-1102.
Haavik-Taylor H, Murphy B.
Cervical Spine Manipulation Alters Sensorimotor Integration:
A Somatosensory Evoked Potential Study
Clin Neurophysiol. 2007 (Feb); 118 (2): 391402Dishman JD, Dougherty PE, Burke JR.
Evaluation of the effect of postural perturbation on motoneural activity following various methods of lumbar spinal manipulation.
The Spine Journal 2005; 5: 650-659.
Suter E, McMorland G, Herzog W, Bray R.
Conservative lower back treatment reduces inhibition in knee-extensor muscles: A randomized controlled trial.
Journal of Manipulative and Physiological Therapeutics 2000; 23: 76-80.
Budgell B, Hirano F.
Innocuous mechanical stimulation of the neck and alterations in heart-rate variability in healthy young adults.
Autonomic Neuroscience: Basic and Clinical 2001; 91: 96-99.
Budgell B, Polus B.
The effects of thoracic manipulation on heart rate variability: A controlled crossover trial.
Journal of Manipulative and Physiological Therapeutics 2006; 29(8): 603-610.
Welch A., Boone R.
Sympathetic and Parasympathetic Responses to Specific Diversified Adjustments to Chiropractic
Vertebral Subluxations of the Cervical and Thoracic Spine
Journal of Chiropractic Medicine 2008 (Sep); 7 (3): 8693Pickar, JG and Wheeler, JD.
Response of Muscle Proprioceptors to Spinal Manipulative-like Loads in the Anesthetized Cat
J Manipulative Physiol Ther. 2001 (Jan); 24 (1): 211Dishman JD, Bulbulian R.
Spinal reflex attenuation associated with spinal manipulation.
Spine 2000; 25(19): 2519=2525.
Benson H, Greenwood MM, Klemchuk H.
The relaxation response: Psychophysiologic aspects and clinical applications.
International Journal of Psychiatry and Medicine 1975; 6(1): 87-98.
Ader R, Cohen H, Felten D.
Psychoneuroimmunology: Interactions between the nervous system and the immune system.
Lancet 1995; 345: 99-103.
Morgan LG.
Psychoneuroimmunology: The placebo effect and chiropractic.
Journal of Manipulative and Physiological Therapeutics 1998; 21(7): 484-491.
Bassett JR, Marshall PM, Spilllane R.
The physiological measurement of acute stress [public speaking] in bank employees.
International Journal of Psychophysiology 1987; 5(4): 265-273.
Kirschbaum C, Helhammer DH.
Salivary control in psychobiological research: An overview. Neuropsychobiology 1989; 22(3): 150-169.
Walker L.
Psychological assessment and intervention: Future prospects for women with breast cancer.
Seminars in Surgical Oncology 1996; 12: 76-83.
Schedlowski M, Schmidt M.
Stress and the immune system.
Naturwissenschaften 1996; 83: 214-220.
Cohen S, Tyrell D, Smith A.
Psychological stress and susceptibility to the common cold.
New England Journal of Medicine 1991; 325(9): 606-612.
Avina-Zubieta J, Paz F, Galindo-Rodriguez G.
Rheumatic manifestations of neurological and psychiatric diseases.
Current Opinions in Rheumatology 1997; 9: 51-55.
Berin M, Perdue M.
Effect of psychoneural factors on intestinal epithelial function.
Canadian Journal of Gastroenterology 1997; 11: 353-357.
Peterson KB.
The effects of manipulation on the intensity of emotional arousal in phobic subjects exposed to a threat stimulus: A randomized, controlled, double-blind clinical trial.
Journal of Manipulative and Physiological Therapeutics 1997; 20(9): 602-606.
Ali S, Hayek R, Holland R, McKelvy S-E, Boyce K, Curson P.
Effect of Chiropractic Treatment on the Endocrine and Immune System in Asthmatic Patients
Proceedings of the 9th International Conference on Spinal Manipulation.
Des Moines, IA: Foundation for Chiropractic Education and Research. In press, 2002.Tuchin PJ.
The effect of chiropractic spinal manipulation on salivary cortisol levels.
Journal of Australian Chiropractic and Osteopathy 1998; 7(2): 86-92.
Field T, Henteleff T, Hernandez M, Martinez E, Mavunda K, Kuhn C, Schanberg S.
Children with asthma improved pulmonary functions after massage therapy.
Journal of Pediatrics 1998; 32(5): 854-858.
Iversen LL.
The chemistry of the brain.
Scientific American 1979; 241(3): 134-149.
Vernon HT, Dhami MSI, Howley TP, Annett R.
Spinal manipulation and beta-endorphin: A controlled study of the effect of a spinal manipulation on plasma beta-endorphin levels in normal males.
Journal of Manipulative and Physiological Therapeutics 1986; 9(2):115-123.
Christian GF, Sissons D, How HY, Jamison J, Alder B, Fullerton M, Funder JW.
Immunoreactive ACTH, beta-endorphin, and cortisol levels in plasma following spinal manipulative therapy.
Spine 1988; 13(12): 1411-1417.
Luisetto G, Spano D, Steiner W, Tagliaro F, Darling P, Campacci R.
Plasma levels of beta-endorphin and calcitonin before and after maniplative treatment of patients with cervical arthrosis and Barre's Syndrome.
In Mazarelli JP [Ed], Chiropractic Interprofessional Research.
Torino, ITALY: Edizioni Minerva, 1982, pp. 47-52.
Herzog W, Scheele D, Conway PJ.
Electromyographic Responses of Back and Limb Muscles Associated With Spinal Manipulative Therapy
Spine (Phila Pa 1976). 1999 (Jan 15); 24 (2): 146152
Strand F.
Physiology: A Systems Approach.
New York, NY: Collier McMillan, 1983.
Kokjohn K, Schmid DM, Triano JJ, Brennan PC.
The effect of spinal manipulation on pain and prostaglandin levels in women with primary dysmenorrhea.
Journal of Manipulative and Physiological Therapeutics 1992; 15(5): 279-285.
Hondras M, Brennan PC.
The effect of spinal manipulation on pain and prostaglandin levels in women with primary dysmenorrhea.
Pain 1999; 81: 105-114.
Hitchcock ME.
The manipulative approach to the management of primary dysmenorrhea.
Journal of the American Osteopathic Association 1976; 75: 97-100.
Arnold-Frochot S.
Investigation of the effect of chiropractic adjustments on a specific gynecological symptom: Dysmenorrhea.
Journal of the Australian Chiropractic Association 1981; 10(1): 6-10, 14-16.
Liebl NA, Butler LM.
A Chiropractic Approach to the Treatment of Dysmenorrhea
Journal of Manipulative and Physiological Therapeutics 1990(Feb); 13 (2): 101106
Thomason PR, Fisher BL, Carpenter PA, Fike GL.
Effectiveness of spinal manipulative therapy in treatment of primary dysmenorrhea: A pilot study.
Journal of Manipulative and Physiological Therapeutics 1979; 2(3): 140-145.
Hubbs EC.
Vertebral Subluxation and Premenstrual Tension Syndrome: A Case Study
Research Forum 1986(Summer); 2 (4): 100102
Stude DE.
The management of symptoms associated with premenstrual syndrome.
Journal of Manipulative and Physiological Therapeutics 1991; 14(3): 209-215.
Walsh MM, Polus B.
A Randomized, Placebo-controlled Clinical Trial on the Efficacy of Chiropractic Therapy on Premenstrual Syndrome
Journal of Manipulative and Physiological Therapeutics 1999(Nov); 22 (9): 582585
Yates RG, Lamping DL, Abram NL, Wright C.
Effects of Chiropractic Treatment on Blood Pressure and Anxiety: A Randomized, Controlled Trial
Journal of Manipulative and Physiological Therapeutics 1988(Dec); 11 (6): 484488
McKnight M.E., DeBoer K.F.
Preliminary Study of Blood Pressure Changes in Normotensive Subjects Undergoing Chiropractic Care
J Manipulative Physiol Ther 1988 (Aug); 11 (4): 261266Wagnon RJ, Sandefur RM, Ratliff CR.
Serum aldosterone changes after specific chiropractic manipulation.
American Journal of Chiropractic Medicine 1988; 1(2): 66-70.
Bakris G, Dickhotz M, Meyer DM, Kravitz G, Avery E, Mille M, Brown J, Woodfield C, Bell B.
Atlas vertebra realignment and achievement of external pressure goal in hypertensive patients: A pilot study.
Journal of Human Hypertension 2007; 21(5): 347-352.
Kfoury PW.
Chiropractic and holistic management of type II diabetes mellitus.
Digest of Chiropractic Economics 1995; 37(4): 37-40.
Weber M, Masarsky CS.
Cervicothoracic subluxation and hot flashes in a perimenopausal subject: A time-series case report.
Journal of Vertebral Subluxation Research 1(2): 33-38, 1996.
Goertz CH, Grimm RH, Svendsen K, Grandits G.
Treatment of Hypertension with Alternative Therapies (THAT) Study: A randomized clinical trial.
Journal of Hypertension 2002; 20(10): 2063-2068.
Rosner A.
Endocrine disorders.
In Masarsky CS, Todres-Masarsky M. Somatovisceral Aspects of Chiropractic:
An Evidence-Based Approach. New York, NY:
Churchill Livingstone, 2001, pp. 187-202.
Raj RP.
Pain Medicine: A Comprehensive Review.
St. Louis, MO: Mosby, 1996, p. 13.
Sompayrac L.
How the Immune System Works, 2nd Edition. Malden, MA:
Blackwell Publishing, 2003.
Packard RS, Libby P.
Inflammation in atherosclerosis: From vascular biology to biomarker discovery and risk prediction.
Clinical Chemistry 2008; 54(1): 24-38.
Libby P, Ridker PM.
Inflammation and atherosclerosis: From population biology and bench research to clinical practice.
Journal of the American College of Cardiology 2006; 48: A33-A46.
Teodorczyk-Injeyan, JA, Injeyan, HS, and Ruegg, R.
Spinal Manipulative Therapy Reduces Inflammatory Cytokines but Not
Substance P Production in Normal Subjects
J Manipulative Physiol Ther 2006 (Jan); 29 (1): 1421Teodorczyk-Injeyan JA, Injeyan HS, Ruegg R.
Spinal manipulative therapy [SMT] augments production of anti-inflammatory cytokine IL-10 in normal subjects.
Proceedings of 9th Biennial Congress of the World Federation of Chiropractic, pp. 143-144.
Al-Shatti T, Barr AE, Safadi FF, Amin M, Barbe MF.
Increase in inflammatory cytokines in median nerves in a rat model of repetitive motion injury.
Journal of Neuroimmunology 2005; 167: 13-22.
Report of the US Preventive Services Task Force,
Baltimore, MD: Williams & Wilkins, 1989.
Bronfort, G, Haas, M, Evans, R, Kawchuk, G, and Dagenais, S.
Evidence-informed Management of Chronic Low Back Pain
with Spinal Manipulation and Mobilization
Spine J. 2008 (Jan); 8 (1): 213225Tunis SR, Stryer DB, Clancy CM.
Practical clinical trials: Increasing the value of clinical research for decision making in clinical and health policy.
Journal of the American Medical Association 2003; 290(12): 1624-1632.
Verhoef MJ, Lewith G, Ritenbaugh C, Boon H, Fleishman S, Leis A.
Complementary and alternative medicine whole systems research: Beyond identification of inadequacies of the RCT.
Complementary Therapies in Medicine 2005; 13: 206-212.
Verhoef MJ, Casebeer Al, Hilsden RJ.
Assessing Efficacy of Complementary Medicine: Adding Qualitative Research Methods to the "Gold Standard"
Journal of Alternative and Complementary Medicine 2002 (Jun); 8 (3): 275281
Hawk C, Knorsa R, Lisi A, Ferrance RJ, Evans MW.
Chiropractic Care for Nonmusculoskeletal Conditions: A Systematic Review
With Implications For Whole Systems Research
J Altern Complement Med. 2007 (Jun); 13 (5): 491512Shekelle, P.G., Adams, A.H., Chassin, M.R. et al.
The Appropriateness of Spinal Manipulation for Low-Back Pain.
Project Overview and Literature Review
Santa Monica, CA: RAND, 1991. Report No.: R-4025/2-CCR/FCER.Shekelle, P.G., Adams, A.H., Chassin, M.R. et al.
The Appropriateness of Spinal Manipulation for Low-back Pain:
Indications and Ratings by a Multidisciplinary Expert Panel
RAND: Santa Monica, CA, 1991, Monograph No. R-4025/2-CCR/FCER.Shekelle PG, Adams AH, Chassin MR, Hurwitz EL, Park RE, Phillips RB, Brook RH.
The appropriateness of spinal manipulation for low back pain: Indications and ratings by an all-chiropractic expert panel.
RAND: Santa Monica, CA, 1992, Monograph No. R-4025/3-CCR/FCER.
Shekelle, P.G., Hurwitz, E.L., Coulter, I., Adams, A.H., Genovese, B.
The Appropriateness of Chiropractic Spinal Manipulation for Low Back Pain: A Pilot Study
J Manipulative Physiol Ther. 1995; 18: 265270Anderson R, Meeker WC, Wirick BE, Mootz RD, Kirk DH, Adams A.
A meta-analysis of clinical trials of spinal manipulation.
Journal of Manipulative and Physiological Therapeutics 1992; 15(3): 181-194.
Shekelle PG, Adams AH, Chassin MR, Hurwitz EL, Brook RH:
Spinal manipulation for low-back pain.
Annals of Internal Medicine 1992; 117: 590-598.
van Tulder MW, Koes BW, Bouter LM.
Conservative treatment of acute and chronic nonspecific low back pain: A systematic review of randomized controlled trials of the most common interventions.
Spine 1997; 22(18): 2128-2156.
Bronfort G Haas M Evans RL et al.
Efficacy of Spinal Manipulation and Mobilization for Low Back Pain and Neck Pain:
A Systematic Review and Best Evidence Synthesis
Spine J (N American Spine Soc) 2004 (May); 4 (3): 335356Bronfort G, Haas M, Evans R, Kawchuk G, Dagenais S.
Evidence-informed management of chronic low back pain with spinal manipulation and mobilization.
The Spine Journal 2008; 8: 213-225.
Lawrence DJ, Meeker W, Branson R, Bronfort G, Cates JR, Haas M, Haneline M et al.
Chiropractic Management of Low Back Pain and Low Back-Related Leg Complaints:
A Literature Synthesis
J Manipulative Physiol Ther 2008 (Nov); 31 (9): 659674Leape LL, Park RE, Kahan JP, Brook RH.
Group judgments of appropriateness: The effect of panel composition:
Quality Assurance in Health Care 1992; 4: 151-159.
National Health and Medical Research Council:
A guide to the development, implementation and evaluation of clinical practice guidelines.
Canberra, AUSTRALIA: AusInfo, 1999.
Assendelft WJJ, Morton SC, Yu EI, Suttorp MJ, Shekelle PG.
Spinal manipulative therapy for low back pain: A meta-analysis of effectiveness relative to other therapies.
Annals of Internal Medicine 2003; 138: 871-881.
Cherkin DL, Sherman SJ, Deyo RA, Shekelle PG.
A review of the evidence for the effectiveness, safety, and cost of acupuncture, massage therapy, and spinal manipulation for back pain.
Annals of Internal Medicine 2003; 138: 898-906.
Ernst E, Canter PH.
A systematic review of systematic reviews of spinal manipulation.
Journal of the Royal Society of Medicine 2006; 99: 189-193.
Bronfort G.
Conflicting evidence: What's the problem?
American Association of Chiropractic Colleges/Research Agenda Conference XI,
Vienna, VA, March 17, 2006.
Meade TW, Dyer S, Browne W, et al.
Low Back Pain of Mechanical Origin: Randomised Comparison of Chiropractic and Hospital Outpatient Treatment
British Medical Journal 1990 (Jun 2); 300 (6737): 14311437Meade TW, Dyer S, Browne W, et al:
Randomised Comparison of Chiropractic and Hospital Outpatient Management for Low Back Pain:
Results from Extended Follow up
British Medical Journal 1995 (Aug 5); 311 (7001): 349351Haas M, Goldberg B, Aickin M, Ganger B, Attwood M.
A Practice-Based Study of Patients With Acute and Chronic Low Back Pain
Attending Primary Care and Chiropractic Physicians: Two-Week to 48-Month Follow-up
J Manipulative Physiol Ther 2004 (Mar); 27 (3): 160169Giles LFG, Muller R.
Chronic Spinal Pain: A Randomized Clinical Trial Comparing Medication, Acupuncture, and Spinal Manipulation
Spine (Phila Pa 1976) 2003 (Jul 15); 28 (14): 14901502
Muller R, Giles LGF.
Long-term Follow-up of a Randomized Clinical Trial Assessing the Efficacy of Medication, Acupuncture, and Spinal Manipulation for Chronic Mechanical Spinal Pain Syndromes
Journal of Manipulative and Physiological Therapeutics 2005 (Jan); 28 (1): 311
Haas, M., Groupp, E., and Kraemer, D.F.
Dose-response for Chiropractic Care of Chronic Low Back Pain
Spine J 2004 (Sep); 4 (5): 574583Wand BM, Bird C, McAuley JH, Dore CJ, MacDowell M, De Souza LH.
Early intervention for the management of low back pain.
Spine 2004; 29(21): 2350-2356.
Coulter ID, Hurwitz EL, Aronow HU, Cassata DM, Beck JC.
Chiropractic Patients in a Comprehensive Home-Based Geriatric Assessment, Follow-up
and Health Promotion Program
Topics In Clinical Chiropractic 1996 (Jun): 3 (2): 4655Descarreaux M, Blouin JS, Drolet M, Papadimitriou S, Teasdale N:
Efficacy of Preventive Spinal Manipulation for Chronic Low-Back Pain and Related Disabilities:
A Preliminary Study
J Manipulative Physiol Ther 2004 (Oct); 27 (8): 509514Fritz JM, Irrgang JJ.
A comparison of a modified Oswestry Low Back Pain Disability Questionnaire and the Quebec Back Pain Disability Scale.
Physical Therapy 2001; 81: 776-788.
Aure, OF, Nilsen, JH, and Vasseljen, O.
Manual Therapy and Exercise Therapy in Patients With Chronic Low Back Pain:
A Randomized, Controlled Trial With 1-Year Follow-Up
Spine (Phila Pa 1976) 2003 (Mar 15); 28 (6): 525531Evans DW.
Mechanisms and Effects of Spinal High-velocity, Low-amplitude Thrust Manipulation:
Previous Theories
J Manipulative Physiol Ther 2002 (May); 25 (4): 251262Meeker WC, Mootz RD, Haldeman S.
Back to basics: The state of chiropractic research.
Topics in Clinical Chiropractic 2002; 9(1): 1-13.
Shekelle PG, Brook RH.
A community-based study of the use of chiropractic services.
American Journal of Public Health 1991; 81(4): 439-442.
Hayden JA, Mior SA, Verhoef MJ.
Evaluation of Chiropractic Management of Pediatric Patients with Low Back Pain: A Prospective Cohort Study
Journal of Manipulative and Physiological Therapeutics 2003 (Jan); 26 (1): 18
Hession EF, Donald GD.
Treatment of multiple lumbar disk herniations in an adolescent athlete utilizing flexion distraction and rotational manipulation
Journal of Manipulative and Physiological Therapeutics 1993 (Mar); 16 (3): 185-92..
Kazemi M.
Adolescent lumbar disc hernatioin in a tae kwon do martial artist: A case report.
Journal of the Canadian Chiropractic Association 1999; 43: 236-242.
King L, Mior SA, Devonshire-Zielonka K.
Adolescent lumbar disc herniation: A case report.
Journal of the Canadian Chiropractic Association 1996; 40: 15-18.
Boline, PD, Kassak, K, Bronfort, G, Nelson, C, and Anderson, AV.
Spinal Manipulation vs. Amitriptyline for the Treatment of Chronic Tension-type Headaches:
A Randomized Clinical Trial
J Manipulative Physiol Ther 1995 (Mar); 18 (3): 148154Nilsson N, Christensen HW, Hartvigsen J.
The Effect of Spinal Manipulation in the Treatment of Cervicogenic Headache
Journal of Manipulative and Physiological Therapeutics 1997 (Jun); 20 (5): 326330
Nelson CF, Bronfort G, Evans R, Boline P, Goldsmith C, Anderson AV:
The Efficacy of Spinal Manipulation, Amitriptyline and the Combination of Both Therapies
for the Prophylaxis of Migraine Headache
J Manipulative Physiol Ther 1998 (Oct); 21 (8): 511519Kjellman GV, Skagren EI, Oberg BE.
A critical analysis of randomised clinical trials on neck pain and treatment efficacy: A review of the literature.
Scandinavian Journal of Rehabilitative Medicine 1999; 31(3): 139-152.
Bronfort G, Assendelft WJJ, Evans R, Haas M, Bouter L.
Efficacy of Spinal Manipulation for Chronic Headache: A Systematic Review
Journal of Manipulative and Physiological Therapeutics 2001 (Sept); 24 (7): 457466
McCrory D.C., Penzien D.B., Hasselblad V., Gray R.N.
Evidence Report: Behavioral and Physical Treatments for Tension-type and Cervicogenic Headache
In: Duke University Evidence-based Practice Center CfCHPR, editor.
Foundation for Chiropractic Education and Research; Des Moines, IA: 2001.Haney V.
Chronic pediatric migraine-type headache treated by long-term inderol prior to chiropractic care: A case report.
Proceedings of the National Conference on Chiropractic Pediatrics,
Palm Beach, FL, October 1993, pp. 132-140.
Hewitt EG.
Chiropractic care of a 13-year old with headache and neck pain: A case report.
Journal of the Canadian Chiropractic Association 1994; 34(3): 160-162.
Kastner U, Deutsch J, Lackner R.
Chronic headache in children and chiropractic manipulation.
Conference Proceedings of the Chiropractic Centennial Foundation,
Washington, DC, July 1995, pp. 286-287.
Cochran JA.
Chiropractic treatment of childhood migraine headache: A case study.
Proceedings of the National Conference on Chiropractic Pediatrics,
Vancouver, British Columbia, CANADA, October 1994, pp.85-90.
Anderson-Peacock ES.
Chiropractic care of children with headaches: Five case reports
Journal of Clinical Chiropractic Pediatrics 1996; 1(1): 18-27.
Lisi AJ, Dabrowski Y.
Chiropractic Spinal Manipulation for Cervicogenic Headache in an 8-Year-Old
Journal of the Neuromusculoskeletal System 2002 (Fall); 10 (3): 98103
Gibson JNA, Grant I, Waddell G.
The Cochrane review of surgery for lumbar disc prolapse and degenerative lumbarspondylosis.
Spine 1999; 24: 1820-1832.
Weinstein JN, Tosteson TD, Lurie JD, Tosteson ANA, Hanscom B, Skinner JS, Abdu WA, Hilibrand AS, Boden SD, Deyo RA.
Surgical vs. nonoperative treatment for lumbar disk herniation:
The Spine Outcomes Research Trial [SPORT]: A randomized trial.
Journal of the American Medical Association 2006; 296(20): 2441-2450.
Weinstein JN, Lurie JD, Tosteson TD, Skinner JS, Hanscom B, Tosteson ANA, Herkowitz H, Fischgrund J, Camissa FP, Albert T, Deyo RA.
Surgical vs Nonoperative treatment for lumbar disk herniation: The Spine Outcomes Research Trial [SPORT]: Observational cohort.
Journal of the American Medical Association 2006; 296(20): 2451-2459.
Fritzell P, Hagg O, Wessberg P, Nordwall A,
Swedish Lumbar Spine Study Group. A multicenter randomized controlled trial from the Swedish Lumbar Study Group.
Spine 2001; 26: 2521-2534.
Nwuga VCB.
Relative therapeutic efficacy of vertebral manipulation and conventional treatment in back pain management.
American Journal of Physical Medicine 1982; 61(6): 273-278.
Burton AK, Tillotson KM, Cleary J.
Single-blind Randomised Controlled Trial of Chemonucleolysis and Manipulation in the Treatment of Symptomatic Lumbar Disc Herniation
European Spine Journal 2000 (Jun); 9 (3): 202207
Henderson RS.
The treatment of lumbar disk intervertebral disk protrusion: an assessment of conservative measures.
British Medical Journal 1952; 2: 597-598.
Mensor MC.
Non-operative treatment, including manipulation, for lumbar intervertebral disc syndrome.
Journal of Bone and Joint Surgery 1955; 37A: 925-936.
Chrisman OD.
A study of the results following rotary manipulation in the lumbar intervertebral disc syndrome.
Journal of Bone and Joint Surgery 1964; 46A: 517-524.
Kuo PP-F, Loh Z-C.
Treatment of lumbar intervertebral disc protrusions by manipulation.
Clinical Orthopedics 1987; 215: 47-55.
d'Ornano J, Conrozier T et al.
Effets des manipulations vertebrales sur la hernie discale lombaire.
Review of Medical Orthopedics 1990; 19: 21-25.
Cassidy JD, Thiel HW, Kirkaldy-Willis KW.
Side posture manipulation for lumbar disc herniation.
Journal of Manipulative and Physiological Therapeutics 1993; 16(2): 96-103.
Coulter I, Hurwitz EL, Adams A, et al.
The Appropriateness of Spinal Manipulation and Mobilization of the Cervical Spine.
RAND Monograph Report, Santa Monica, CA: RAND; 1996.Coulter I, Shekelle PG, Mootz RD, Hansen DT.
The use of expert panel results: The RAND panel for appropriateness of manipulation and mobilization of the cervical spine.
Topics in Clinical Chiropractic 1995; 2(3): 54-62.
Hurwitz, EL, Carragee, EJ, van der Velde, G et al.
Treatment of Neck Pain: Noninvasive Interventions: Results of the Bone and Joint Decade
20002010 Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S123152Koes BW, Bouter LM, van Mameren H, Essers AH, Verstegen GJ, Hofhuizen DM, Houben JP, Knipschild PG.
A randomised clinical trial of manual therapy and physiotherapy for persistent back and neck complaints: Subgroup analysis and relationship between outcome measures.
Journal of Manipulative and Physiological Therapeutics 1993; 16(4): 211-219.
Cassidy JD, Lopes AA, Yong-Hing K.
The immediate effect of manipulation versus mobilization on pain and range of motion in the cervical spine: A randomized controlled trial.
Journal of Manipulative and Physiological Therapeutics 1992; 15(9): 570-575.
Rogers RG.
The Effects of Spinal Manipulation on Cervical Kinesthesia in Patients With Chronic Neck Pain: A Pilot Study
Journal of Manipulative and Physiological Therapeutics 1997 (Feb); 20 (2): 8085
Skargren EI, Oberg BE, Carlsson PG, Gade M.
Cost and effectiveness analysis of chiropractic and physiotherapy treatment for low back and neck pain.
Spine 1997; 22: 2167-2177.
Jordan A, Bendix T, Nielsen H, Hansen FR, Ost D, Winkel A.
Intensive training, physiotherapy, or manipulation for patients with chronic neck pain: A prospective, single-blinded, randomized clinical trial.
Spine 1998; 23(3): 311-318.
Hoving JL, Koes BW, de Vet HC, van der Windt DA, Assendelft WJ, van Mameren H, et al.
Manual Therapy, Physical Therapy, or Continued Care by a General Practitioner
for Patients with Neck Pain. A Randomized, Controlled Trial
Annals of Internal Medicine 2002 (May 21); 136 (10): 713722Palmgren JJ, Sandstrom PJ, Lundqvist FJ, Heikkila H.
Improvement After Chiropractic Care in Cervicocephalic Kinesthetic Sensibility and Subjective Pain Intensity in Patients with Nontraumatic Chronic Neck Pain
Journal of Manipulative and Physiological Therapeutics 2006 (Feb); 29 (2): 100106
Vernon HT, Humphreys BK, Hagino CA.
A systematic review of conservative treatments for acute neck pain not due to whiplash.
Journal of Manipulative and Physiological Therapeutics 2005; 28(6): 443-448.
Bronfort G, Haas M, Evans RL, Bouter LM.
Efficacy of Spinal Manipulation and Mobilization for Low Back Pain and Neck Pain: A Systematic Review and Best Evidence Synthesis
Spine Journal 2004 (May); 4 (3): 335356
Gross AR, Hoving JL, Haines TA, Goldsmith CH, Kay T, Aker P, Bronfort G,
Cervical Overview Group. A Cochrane review of manipulation and mobilization for mechanical neck disorders.
Spine 2004; 29(14): 1541-1548.
Evans R, Bronfort G, Nelson B, Goldsmith CH.
Two-year Follow-up of a Randomized Clinical Trial of Spinal Manipulation
and Two Types of Exercise Patients With Chronic Neck Pain
Spine (Phila Pa 1976) 2002 (Nov 1); 27 (21): 23832389Foreman SM, Croft AC.
Whiplash Injuries: The Cervical Acceleration/Deceleration Syndrome, 2nd Ed.
Baltimore, MD: Williams & Wilkins, 1995.
Girard N.
Statistiques descriptives dur la nature des blessures.
Quebec. Regie de l'assurance automobile du Quebec.
Direction des services medicaux et de la readaption. Internal document. Quebec, 1989.
Giroux M.
Les blessures a la colonne cervicale. Importance du probleme.
Le Medicin du Quebec, Montreal, September 22-26, 1991.
Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, Zeiss E.
Scientific Monograph of the Quebec Task Force on Whiplash-Associated Disorders
Redefining Whiplash and its Management
Spine (Phila Pa 1976). 1995 (Apr 15); 20 (8 Suppl): S1-S73Freeman MD, Croft AC, Rossignol AM.
Whiplash Associated Disorders: Redefining Whiplash and Its Management
by the Quebec Task Force ~ A Critical Evaluation
Spine (Phila Pa 1976) 1998 (May 1); 23 (9): 10431049Jonsson H, Bring G, Rauschning W, Sahlstedt B.
Hidden cervical spine injuries in traffic accident victims with skull fractures.
Journal of Spinal Disorders 1991; 4(3): 251-263.
Akeson WH, Ameil D, Mechanic CL, Soo SL-Y, Harwood FC, Hamer ML.
Collagen cross-linking alterations in joint contractures. Changes in the reducible cross-links in periarticular connective tissue after nine weeks of immobilization.
Connective Tissue Research 1977; 5: 15-19.
Frank C, Woo SL-Y, Amiel D, Harwood F, Gomez M, Akeson W.
Medical collateral ligament healing--a multidisciplinary assessment in rabbits.
American Journal of Sports Medicine 1983; 11: 379-389.
Long ML, Frank C, Schachlan NS, Dittrick D, Edwards GE.
The effects of motion on normal healing ligaments [Abstract].
Proceedings of the Orthopedic Reseach Society 1982; 7: 43.
Fronek J, Frank C, Amiel D, Woo SL-Y, Coutts RD, Akeson WH.
The effects of intermittent passive movement [IPM] in the healing of medical collateral ligament [Abstract].
Proceedings of the Orthopedic Research Society 1983; 8: 31.
Gelberman RH, Manske PR, Akeson WH, Woo SL-Y, Lundborg G, Amiel D.
Flexor tendon repair.
Journal of Orthopedic Research 1986; 4: 119-128.
Crock H.
Low back surgery.
International Chiropractic Conference, London, England, September 1987.
Baker D.
Development and regeneration of mammalian muscle spindles.
Scientific Progress 1984; 69: 45- 64.
Nansel D, Peneff A, Cremata E, Carlson J.
Time Course Considerations for the Effect of Lower Cervical Adjustments with Respect to the Amelioration of Cervical Lateral Flexion Passive Endrange Asymmetries, and on Blood Pressure, Heart Rate, and Plasma Catecholamine Levels
Journal of Manipulative and Physiological Therapeutics 1991 (Oct); 14 (8): 450456
Khan S, Cook J, Gargan M, Bannister G.
A Symptomatic Classification of Whiplash Injury and the Implications for Treatment
Journal of Orthopaedic Medicine 1999; 21 (1): 2225
Suter E, Harris S, Rosen M, Peterson D.
Cervical spine adjustment improves muscle strength of the upper extremities in patients with subacute whiplash.
Symposium Proceedings, World Federation of Chiropractic
6th Biennial Congress, pp. 229-230.
Kessinger RC, Boneva DV.
Case study: Acceleration/deceleration injury with angular kyphosis.
Journal of Manipulative and Physiological Therapeutics 2000; 23(4): 279-287.
Martin Saborido C, Garcia Lizana F, Alcazar Alcazar R, Sarria-Santamera
Efectividad de las tecnias de manipulacion espinal en la 51lesion por latigazo-51 [Effectiveness of spinal manipulation in treating whiplash injuries].
Aten Primaria 2007; 39(5): 241-246.
Fernandez-de-las-Penas C, Alonso-Blanco C, San-Roman J, Miangolarra-Page IC.
Methodological quality of randomized controlled trials of spinal manipulation and mobilization in tension-type headache, migraine, and cervicogenic headache.
Journal of Orthopedic and Sports Physical Therapies 2006; 36(3): 160-169.
Bitterli J, Graf F, Robert F, Adler R, Mumenthaler M.
Zur objektivierung der manualtherapeutischen beeinfluessbarket des spondylogenen korpschemerzes [Objective criteria for the evaluation of chiropractic treatment of spondylitic headache].
Nervenarzt 1977; 48(5): 159-162.
Hoyt WH, Shaffer F, Bard DA, Benesler JS, Blankenhorn GD III, Gray JH, Hartman WT, Hughes LC.
Osteopathic manipulation in the treatment of muscle-contraction headache.
Journal of the American Osteopathic Association 1979; 78: 322-325.
Bove G, Nilsson N.
Spinal manipulation in the treatment of episodic tension-type headache.
Journal of the American Medical Association 1998; 280(18): 1576-1579.
Nilsson N, Christensen HW, Hartvigsen J.
The Effect of Spinal Manipulation in the Treatment of Cervicogenic Headache
Journal of Manipulative and Physiological Therapeutics 1997 (Jun); 20 (5): 326330
Nilsson N.
A Randomized Controlled Trial of the Effect of Spinal Manipulation in the Treatment of Cervicogenic Headache
Journal of Manipulative and Physiological Therapeutics 1995 (Sep); 18 (7): 435440
Whittingham W.
Randomized placebo controlled clinical trial of efficacy of chiropractic treatment for chronic cervicogenic headaches.
Symposium Proceedings, 6th Biennial Congress, World Federation of Chiropractic,
Paris, FRANCE, May 21-26, 2001, pp. 231-232.
Jull G, Trott P et al.
A Randomized Controlled Trial of Exercise and Manipulative Therapy for Cervicogenic Headache
Spine (Phila Pa 1976) 2002 (Sep 1); 27 (17): 18351843Haas M, Groupp E, Aickin M, Fairweather A, Ganger B, Attwood M, et al.
Dose Response for Chiropractic Care of Chronic Cervicogenic Headache
and Associated Neck Pain: A Randomized Pilot Study
J Manipulative Physiol Ther 2004 (Nov); 27 (9): 547553Parker G, Tupling H, Pryor D.
A controlled trial of cervical manipulation for migraine.
Australian and New Zealand Journal of Medicine 1978; 8: 589-593.
Nelson CF, Bronfort G, Evans R, Boline P, Goldsmith C, Anderson AV.
The Efficacy of Spinal Manipulation, Amitriptyline and the Combination of Both Therapies for the Prophylaxis of Migraine Headache
Journal of Manipulative and Physiological Therapeutics 1998 (Oct); 21 (8): 511519
Tuchin PJ, Pollard H, Bonello R.
A Randomized Controlled Trial of Chiropractic Spinal Manipulative Therapy for Migraine
J Manipulative Physiol Ther 2000 (Feb); 23 (2): 9195Jensen IK, Nielsen FF, Vosmar L.
An Open Study Comparing Manual Therapy With the Use of Cold Packs in the Treatment
of Post-traumatic Headache
Cephalalgia 1990 (Oct); 10 (5): 241250
Mootz RD, Dhami MSI, Hess JA, Cook RD, Schorr DB.
Chiropractic treatment of chronic episodic tension type headache in male subjects: a case series analysis.
Journal of the Canadian Chiropractic Association 1994; 38(3): 152-159.
Droz JM, Crot F.
Occipital headaches: statistical results in the treatment of vertebrogenic headache.
Annals of the Swiss Chiropractic Association 1985; 8: 127-136.
Vernon HT.
Spinal Manipulation and Headaches of Cervical Origin
Journal of Manipulative and Physiological Therapeutics 1989 (Dec); 12 (6): 455468
Wight JS.
Migraine: A statistical analysis of chiropractic treatment.
Chiropractic Journal 1978; 12: 363-367.
Stodolny J, Chmielewski H.
Manual therapy in the treatment of patients with cervical migraine.
Manual Medicine 1989; 4: 49-51.
Turk Z, Ratkolb O.
Mobilization of the cervical spine in chronic headaches.
Manual Medicine 1987; 3: 15- 17.
Haney V.
Chronic pediatric migraine-type headache treated by long-term inderol prior to chiropractic care. A case report.
Proceedings of the National Conference on Chiropractic Pediatrics,
Palm Beach, FL, October 1993, pp. 132-140.
Hewitt EG.
Chiropractic care of a 13-year old with headache and neck pain. A case report.
Journal of the Canadian Chiropractic Association 1994; 4(3): 160-162.
Kastner U, Deutsch J, Lackner R.
Chronic headache in children and chiropractic manipulation.
Conference Proceedings of the Chiropractic Centennial Foundation,
Washington, DC, pp. 286-287.
Cochran JA.
Chiropractic treatment of childhood migraine headache: A case study.
Proceedings of the National Conference on Chiropractic Pediatrics,
October 1994, pp. 85-90.
Lisi AJ, Dabrowski Y.
Chiropractic spinal manipulation for cervicogenic headache in an 8-year old.
Journal of the Neuromusculoskeletal System 2002; 19(3): 98-103.
Hurwitz EL, Aker PO, Adams AH, Meeker WC, Shekelle PG.
Manipulation and Mobilization of the Cervical Spine:
A Systematic Review of the Literature
Spine (Phila Pa 1976) 1996 (Aug 1); 21 (15): 17461760Kjellman GV, Skagren EI, Oberg BE.
A critical analysis of randomised clinical trials on neck pain and treatment efficacy: A review of the literature.
Scanidavian Journal of Rehabilitative Medicine 1999; 31: 139- 152.
Bronfort G, Assendelft WJJ, Evans R, Haas M, Bouter L.
Efficacy of Spinal Manipulation for Chronic Headache: A Systematic Review
Journal of Manipulative and Physiological Therapeutics 2001 (Sept); 24 (7): 457466
Vernon H.
The effectiveness of chiropractic manipulation in the treatment of headache: An exploration of the literature.
Journal of Manipulative and Physiological Therapeutics 1995; 18(9): 611-617.
Vernon, H, McDermaid, CS, and Hagino, C.
Systematic Review of Randomized Clinical Trials of Complementary/Alternative Therapies
in the Treatment of Tension-type and Cervicogenic Headache
Complementary Therapies in Medicine 1999 (Sep); 7 (3): 142155Hack GD, Koritzer RT, Robinson WL, Hallgren RC, Greenman PE.
Anatomic Relation Between the Rectus Capitis Posterior Minor Muscle and the Dura Mater
Spine 1995 (Dec); 20 (23): 2484-2486
Hack G, Dunn G, Toh MY.
The anatomist's new tools.
1998 Medical and Health Annual, Chicago,IL:
Encyclopedia Britannica, 1997, pp. 16-29.
Gayuron B, Vargha A, Michelow BJ, Thomas T, Davis J.
Corrugator supercilii muscle reaction and migraine headaches.
Plastic and Reconstructive Surgery 2000; 106: 429-434.
Humphreys BK, Kenin S, Hubbard B, Cramer GD.
Investigation of connective tissue attachments to the cervical spinal dura mater.
Clinical Anatomy 2003; 16: 152-159.
International Headache Society.
Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain.
Cephalalgia 1988; 8 [suppl 7]; 1-96.
Bogduk N.
The anatomical basis for cervicogenic headache.
Journal of Manipulative and Physiological Therapeutics 1993; 15(1): 67-69.
McCrory DC, Penzien DB, Hasselblad V, Gray RN.
Evidence Report: Behavior and Physical Treatments for Tension-type and Cervicogenic Headaches
Des Moines, IA: Foundation for Chiropractic Education and Research, 2001.
Christensen M, Kollasch M, Ward R, Kelly R. Day A, zumBrunnen J.
Evidence Report: Behavior and Physical Treatments for Tension-type and Cervicogenic Headaches
Greely, CO: National Board of Chiropractic Examiners; 2005. pp. 67-100.
Nelson, C., Lawrence, D., Triano, J., Bronfort, G., Perle, S., Metz, R. D., et al.
Chiropractic As Spine Care: A Model For The Profession
Chiropractic & Osteopathy 2005 (Jul 6); 13: 9Barnes PM , Powell-Griner E , McFann K , Nahin RL:
Complementary and Alternative Medicine Use Among Adults:
United States, 2002
Advance Data 2004 (May 27); 343: 119Mootz RD, Cherkin DC, Odegard CE, Eisenberg DM, Barassi JP, Deyo RA.
Characteristics of Chiropractic Practitioners, Patients, and Encounters
in Massachusetts and Arizona
J Manipulative Physiol Ther. 2005 (Nov); 28 (9): 645653Cherkin DC, Deyo RA, Sherman K, Erro JH, Hrbek A, Davis RB, Eisenberg DM.
Characteristics of Visits to Licensed Acupuncturists, Chiropractors,
Massage Therapists, and Naturopathic Physicians
J Am Board Fam Pract 2002; 15 (6): 463-480Bergman GJD, Winters JC, Gronier KH, Pol JJM, Meyboom-de-Jong B, Posterna K, van der Heijden GJMG.
Manipulative Therapy in Addition to Usual Medical Care for Patients with Shoulder Dysfunction and Pain: A Randomized, Controlled Trial
Annals of Internal Medicine 2004 (Sep 21); 141 (6): 432-439
McHardy, A, Hoskins W, Pollard H, Onley R. Windsham R.
Chiropractic treatment of upper extremity conditions: A systematic review.
Journal of Manipulative and Physiological Therapeutics 2008; 31(2): 146- 159.
Davis PT, Hulbert JR.
Carpal tunnel syndrome: Conservative and nonconservative treatment: A chiropractic physician's perspective.
Journal of Manipulative and Physiological Therapeutics 1998; 21(5): 356-362.
Davis PT, Hulbert JR, Kassak KM, Meyer JJ.
Comparative Efficacy of Conservative Medical and Chiropractic Treatments for Carpal Tunnel Syndrome: A Randomized Clinical Trial
Journal of Manipulative and Physiological Therapeutics 1998 (Jun); 21 (5): 317326
Winters JC, Sobel JS, Groenier KH, Arendzen HJ, Meyboom-de Jong B.
Comparison of Physiotherapy, Manipulation, and Corticosteroid Injection for Treating Shoulder Complaints in General Practice: Randomised, Single Blind Study
British Medical Journal 1997 (May 3); 314 (7090): 13201325
Strait BW, Kuchera ML.
Osteopathic manipulation for patients with confirmed mild, modest, and moderate carpal tunnel syndrome.
Journal of the American Osteopathic Association 1994; 94(8): 673.
Burke J, Buchberger DJ, Carey-Loghman T, Dougherty PE, Greco DS, Dishman JD.
A pilot study comparing two manual therapy interventions for carpal tunnel syndrome.
Journal of Manipulative and Physiological Therapeutics 2007; 30(1): 50-61.
Hulbert JR, Osterbauer P, Davis PT, Printon R, Goessl C, Strom N.
Chiropractic treatment of hand and wrist pain in older people: Systematic protocol development Part 2: Cohort natural-history treatment trial.
Journal of Chiropractic Medicine 2007; 6: 32-41.
Bonebrake AR, Fernandez JE, Marley RJ, Dahalan JB, Kilmer KJ.
A treatment for carpal tunnel syndrome: Evaluation of objective and subjective measures.
Journal of Manipulative and Physiological Therapeutics 1991; 13(9): 507-520.
Bonebrake AR, Fernandez JE, Dahalan JB, Marley RJ.
A treatment for carpal tunnel syndrome: Results of a follow-up study.
Journal of Manipulative and Physiological Therapeutics 1993; 16(3): 125-139.
Sucher BM.
Myofascial manipulative release of carpal tunnel syndrome. Documentation with magnetic resonance imaging.
Journal of the American Osteopathic Association 1993; 93(12): 1273-1278.
Sucher BM.
Palpatory diagnosis and manipulative management of carpal tunnel syndrome.
Journal of the American Osteopathic Association 1994; 94(8): 647-663.
Hoskins W, McHardy A, Pollard H, Windsham R, Onley R.
Chiropractic treatment of lower extremity conditions: A literature review.
Journal of Manipulative and Physiological Therapeutics 2006; 29: 658-671.
Brantingham JW, Globe G, Pollard H, Hicks M, Korporaal C, Hoskins W.
Manipulative therapy for lower extremity conditions: Expansion of literature review.
Journal of Manipulative and Physiological Therapeutics 2009; 32(1): 53-71.
Lebouef-Yde C, Axen I, Ahlefeldt G, Lidefelt P, Rosenbaum A, Thurnherr T.
The types and frequencies of improved nonmuculoskeletal symptoms reported after chiropractic spinal manipulative therapy.
Journal of Manipulative and Physiological Therapeutics 1999; 22(9): 559-564.
Leboeuf-Yde, C., Pedersen, E.N., Bryner, P., Cosman, D., Hayek, R.
Self-reported Nonmusculoskeletal Responses to Chiropractic Intervention:
A Multination Survey
J Manipulative Physiol Ther 2005 (Jun); 28 (5): 294302Wiberg, JM, Nordsteen, J, and Nilsson, N.
The Short-term Effect of Spinal Manipulation in the Treatment of Infantile Colic:
A Randomized Controlled Clinical Trial with a Blinded Observer
J Manipulative Physiol Ther 1999 (Oct); 22 (8): 517522Olafsdottir E, Forshei S, Fluge G, Markestad T:
Randomised Controlled Trial of Infantile Colic Treated With Chiropractic Spinal Manipulation
Archives of Disease in Childhood 2001 (Feb); 84 (2): 138141Mercer C, Nook BC.
The efficacy of chiropractic spinal adjustments as a treatment protocol in the management of infantile colic.
Proceedings of the 5th Biennial Congress,
Auckland, NEW ZEALAND, May 17-22, 1999, pp. 170-171.
Klougart N, Nilsson N, Jacobsen J.
Infantile Colic Treated by Chiropractors: A Prospective Study of 316 Cases
J Manipulative Physiol Ther 1989 (Aug); 12 (4): 281288Leach RA.
Differential Compliance Instrument in the Treatment of
Infantile Colic: A Report of Two Cases
Journal of Manipulative and Physiological Therapeutics 2002 (Jan); 25 (1): 5862
Pluhar G, Schobert PD.
Vertebral subluxation and colic: A case study.
Journal of Chiropractic Research and Clinical Investigation 1991; 7: 75-76.
Van Loon M.
Colic with projectile vomiting: A case study.
Journal of Chiropractic Pediatrics 1998; 3: 207-210.
Bennet-Johnson S.
Enuresis.
In Daitzman RJ [Ed], Clinical Behaviour Therapy and Behaviour Modification.
New York, NY: Garland STPM Press, 1980, pp. 81-141.
Reed WR, Beavers S, Reddy SK, Kern G.
Chiropractic management of primary nocturnal enuresis.
Journal of Manipulative and Physiological Therapeutics 1994; 17(9): 596-600.
Lebouef C, Brown P, Herman A, Leembruggen K, Walton D, Crisp TC.
Chiropractic care for children with nocturnal enuresis: A prospective outcome study.
Journal of Manipulative and Physiological Therapeutics 1991; 14(2): 110-115.
Blomerth PR.
Functional nocturnal enuresis.
Journal of Manipulative and Physiological Therapeutics 1994; 17(5): 335-338.
Gemmell HA, Jacobson BH.
Chiropractic management of enuresis: Time-series descriptive design.
Journal of Manipulative and Physiological Therapeutics 1989; 12(5): 386-389.
Palmer College of Chiropractic Adjusting Manual.
Davenport, IA: Palmer College of Chiropractic, 1983.
Sears MR, Taylor DR, Print CG, Lake DC, Li QQ, Flannery EM, Yates DM, Lucas MK, Herbison GP.
Regular inhaled beta-agonist treatment in bronchial asthma.
Lancet 1990; 336(8728): 1391-1396.
Dhami MSI, DeBoer KF.
Systemic effects of spinal lesions.
In Haldeman S [ed], Principles and Practice of Chiropractic, 2nd Edition.
Norwalk, CT: Appleton & Lange, 1992, pp. 115-135.
Beyeler W.
Experiences in the management of asthma.
Annals of the Swiss Chiropractic Association 1965; 3: 111-117.
Nilsson N, Christiansen B.
Prognostic factors in bronchial asthma in chiropractic practice.
Journal of the Australian Chiropractic Association 1988; 18: 85-87.
Balon J, et al.
A Comparison of Active and Simulated Chiropractic Manipulation as Adjunctive Treatment
for Childhood Asthma
New England Journal of Medicine 1998; 339(15): 1013-1020Guiney PA, Chou R, Vianna A, Lovenheim J.
Effects of osteopathic manipulative treatment on pediatric patients with asthma: A randomized controlled trial.
Journal of the American Osteopathic Association 2005;105: 7-12.
Nilsson NH, Bronfort G, Bendix T, Madsen F, Weeke B.
Chronic Asthma and Chiropractic Spinal Manipulation: A Randomized Clinical Trial
Journal of Clinical and Experimental Allergy 1995 (Jan); 25 (1): 8088
Bronfort G, Evans RL, Kubic P, Filkin P.
Chronic Pediatric Asthma and Chiropractic Spinal Manipulation: A Prospective Clinical Series and Randomized Clinical Pilot Study
Journal of Manipulative and Physiological Therapeutics 2001 (July); 24 (6): 369377
Nilsson N, Christiansen B.
Prognostic factors in bronchial asthma in chiropractic practice.
Journal of the Australian Chiropractic Association 1998; 18: 85-87.
Bockenhauer Se, Julliard KN, Lo KS, Huang KE, Sheth AM.
Quantifiable effects of osteopathic manipulative techniques on patients with chronic asthma.
Journal of the American Osteopathic Association 2002; 102(7): 371-375.
Jamison JR.
Asthma in a chiropractic clinic: A pilot study.
Journal of the Australian Chiropractic Association 1986; 16: 138-144.
Peet JB, Marko SK, Piekarczyk W.
Chiropractic response in the pediatric patient with asthma: A pilot study.
Chiropractic Pediatrics 1995; 1: 9-13.
Lines D.
A wholistic approach to the treatment of bronchial asthma in a chiropractic practice.
Chiropractic Journal of Australia 1993; 23: 408.
Garde R.
Asthma and chiropractic.
Chiropractic Pediatrics 1994; 1: 9-16.
Hunt J.
Upper cervical chiropractic care of a pediatric patient with asthma: A case study.
Journal of Clinical Chiropractic Pediatrics 2000; 1: 3-9.
Killinger LZ.
Chiropractic care in the treatment of asthma.
Palmer Journal of Research 1995; 2: 74-77.
Peet JB.
Case study: Eight year old female with chronic asthma.
Chiropractic Pediatrics 1997; 3: 9-12.
Dilman V, Dean W.
The Neuroendocrine Theory of Aging and Degenerative Diseases.
Pensacola, FL: Center for Bio-Gerontology, 1992, pp. 26-27.
Gleeson M, Clancy RL, Hensley MJ, Cripps AW, Henry RL, Wlodarczy JH, Gibson PG.
Development of bronchial hyperreactivity following transient absence of IgA.
American Journal of Respiratory and Critical Care Medicine 1996; 153[6 Pt 1]: 1785-1789.
Snyder BJ, Sanders GE.
Evaluation of the Toftness system of chiropractic adjusting for subjects with chronic back pain, chronic tension headaches, or primary dysmenorrhea.
Chiropractic Technique 1996; 8: 3-9.
Walsh BJ, Polus BI.
The Frequency of Positive Common Spinal Clinical Examination Findings in a Sample of
Premenstrual Syndrome Sufferers
Journal of Manipulative and Physiological Therapeutics 1999 (May); 22 (4): 216220Wittler MA.
Chiropractic Approach to Premenstrual Syndrome (PMS)
Journal of Chiropractic Research and Clinical Investigation 1992; 8 (2): 2629
Stude DE.
The management of symptoms associated with premenstrual syndrome.
Journal of Manipulative and Physiological Therapeutics 1991; 14(3): 209-216.
Pitkaranta A, Jero J, Arruda E, Virolainen A, Hayden FG.
Polymerase chain-reaction based detection of rhinovirus, respiratory syncytial virus, and coranovirus in otitis media with effusion.
Journal of Pediatrics 1998; 133(3): 390-394.
Tomasz A.
Multiple-antibiotic-resistant pathogenic bacteria: A report on the Rockefeller University Workshop.
New England Journal of Medicine 1994; 330(17): 1247-1251.
Evans-Pritchard, A.
Science in the dock as the antibiotic miracle crumbles.
Sunday Times [London], May 3, 1998, p. 1.
Mangione-Smith R, McGlynn EA, Elliott MN, Krogstad P, Brook RH.
The relationship between perceived parental expectations and pediatrician antimicrobial prescribing behavior.
Pediatrics 1999; 103(4 Pt1): 711- 718.
Mills MV, Henley CE, Barnes LLB, Carreiro JE, Degenhardt BF.
The use of osteopathic manipulative treatment as adjuvant therapy in children with recurrent acute otitis media.
Archives of Pediatrics and Adolescent Medicine 1003; 157(9): 861-866.
Sawyer C.E., Evans R.L., Boline P.D., Branson R., Spicer A.
A Feasibility Study of Chiropractic Spinal Manipulation Versus Sham Spinal Manipulation for
Chronic Otitis Media with Effusion in Children
J Manipulative Physiol Ther 1999 (Jun); 22 (5): 292298Froehle RM.
Ear Infection: A Retrospective Study Examining Improvement From Chiropractic Care and Analyzing Influencing Factors
Journal of Manipulative and Physiological Therapeutics 1996 (Mar); 19 (3): 169177
Fallon JM.
The Role of the Chiropractic Adjustment in the Care and Treatment of 332 Children with Otitis Media
Journal of Clinical Chiropractic Pediatrics 1997 (Oct); 2 (2): 167183
Fallon J, Edelman MJ.
Chiropractic care of 401 children with otitis media: A pilot study.
Alternative Therapies in Health and Medicine 1998; 4(2): 93.
Fysh PN.
Chronic recurrent otitis media: Case series of five patients with recommendations for case management.
Journal of Clinical Chiropractic Pediatrics 1996; 1: 66-78.
Phillips NJ.
Vertebral Subluxation and Otitis Media: A Case Study
Journal of Chiropractic Research and Clincal Investigation 1992; 8 (2): 3840
Peet J.
Case study: Chiropractic results with a child with recurrent otitis media accompanied by effusion.
Chiropractic Pediatrics 1996; 2: 8-10.
Thomas D.
Irritable child with chronic ear effusion/infections responds to chiropractic care.
Chiropractic Pediatrics 1997; 3: 13-14.
Diamant M, Diamant B.
Abuse and timing of use of antibiotic in acute otitis media.
Archives of Otolaryngology 1974; 100(3): 226-232.
Plaugher G, Long CR, Alcantara J, Silveus AD, Wood H, Lotun K, Menke JM, Meeker WC, Rowe SH.
Practice-based Randomized Controlled-comparison Clinical Trial of Chiropractic Adjustments and Brief Massage
Treatment at Sites of Subluxation in Subjects with Essential Hypertension: Pilot Study
Journal of Manipulative and Physiological Therapeutics 2002 (May); 25 (4): 221239
Morgan JP, Dickey JL, Hunt HH, Hudgins PM.
A controlled trial of spinal manipulation in the management of hypertension.
Journal of the American Osteopathic Association 1985; 85: 308-313.
Knutson G.A.
Significant Changes in Systolic Blood Pressure Post Vectored Upper Cervical Adjustment vs Resting
Control Groups: A Possible Effect of the Cervicosympathetic and/or Pressor Reflex
J Manipulative Physiol Ther 2001 (Feb); 24 (2): 101109Fischera AP, Celander DR.
Effect of osteopathic manipulative therapy on autonomic tone as evidenced by blood pressure changes and activity of the fibrinolytic system.
Journal of the American Osteopathic Association 1969; 68: 1036-1038.
Goodman R.
Hypertension and the Atlas Subluxation Complex
Journal of Chiropractic Research and Clinical Investigation 1992; 8 (2): 3032.
Connelly D, Rasmussen S.
The effect of cranial adjusting on hypertension: A case report.
Chiropractic Technique 1998; 10: 75-78.
Plaugher G, Bachman TR.
Chiropractic Management of a Hypertensive Patient
Journal of Manipulative and Physiological Therapeutics 1993 (Oct); 16 (8): 544549
McGee D.
Hypertension: A case study.
Journal of Chiropractic Research and Clinical Investigation 1992; 7: 5-7.
Janetta PJ, Segal R, Wolfson Jr SK.
Neurogenic hypertension: Etiology and surgical treatment 1: Observations in 53 patients.
Annals of Surgery 1985; 201: 391-398.
Jarmel ME.
Possible role of spinal joint dysfunction in the genesis of sudden cardiac death.
Journal of Manipulative and Physiological Therapeutics 1989; 12(6): 469-477.
Verrier RL, Hagestad EL.
Role of the autonomic nervous system in sudden death.
Cardiovascular Clinica 1985; 15: 41-63.
Lown B, Verrier RL.
Neural activity and ventricular fibrillation.
New England Journal of Medicine 1976; 294; 1165-1170.
Kleiger RE, Miller JP Bigger JT, Moss AJ.
Decreased heart rate variability and its association with increased mortality after acute myocardial infarction.
American Journal of Cardiology 1987; 59(4): 256-262.
Malliani A, Schwartz PJ, Zanchetti A.
Neural mechanism in life-threatening arrhythmias.
American Heart Journal 1980; 100: 705-715.
Thabe H.
Electromyography as Tool to Document Diagnostic Findings and Therapeutic Results Associated with Somatic Dysfunctions in the Upper Cervical Spinal Joints and Sacroiliac Joints
Manual Medicine 1986; 2 (2) : 5358
Shambaugh P.
Changes in electrical activity in muscles resulting from chiropractic adjustment: A pilot study.
Journal of Manipulative and Physiological Therapeutics 1987; 10: 300-304.
Karemaker JM.
Analysis of blood pressure and heart rate variability: Theoretical considerations.
In Low, PA (Editor). Clinical Autonomic Disorders, 2nd edition.
Philadelphia, PA: Lipincott-Raven Publishers, 1997, pp. 309-322.
Goldberger AL.
Fractal electrodynamics of the heartbeat.
Annals of the Academy of Sciences 1990; 591: 402-409.
Eingorn AM, Muhs GJ.
Rationale for assessing the effects of manipulative therapy on autonomic tone by analysis of heart rate variability.
Journal of Manipulative and Physiological Therapeutics 1999; 22(3): 161- 165.
Malik M.
Sympathvagal balance: A critical appraisal.
Circulation 1998; 98(23): 2643-2644.
Budgell BS, Igarashi Y.
Response of arrhythmia to spinal manipulation: Monitoring by ECG with analysis of heart-rate variability.
Journal of the Neuromusculoskeletal System 2001; 9(3): 97-102.
Hawk C, Khorsan R, Lisi AJ, Ferrance RJ, Evans MW.
Chiropractic Care for Nonmusculoskeletal Conditions: A Systematic Review With Implications For Whole Systems Research
Journal of Alternative and Complementary Medicine 2007 (Jun); 13 (5): 491512
Wagner T, Owen J, Malone E, Mann K.
Irritable bowel syndrome and spinal manipulation: A case report.
Chiropractic Technique 1995; 7(4): 139-140.
Quist DM, Duray SM.
Resolution of symptoms of chronic constipation in an 8-year old male after chiropractic treatment.
Journal of Manipulative and Physiological Therapeutics 2007; 30(1): 65-68.
Stude DE, Mick T.
Clinical Presentation of a Patient with Multiple Sclerosis and Response to Manual Chiropractic Adjustive Therapies
Journal of Manipulative and Physiological Therapeutics 1993 (Nov); 16 (9): 595600
Frach JP, Osterbauer PJ, Fuhr AW.
Treatment of Bell's Palsy by Mechanical Force, Manually Assisted Chiropractic Adjusting and High-voltage Electrotherapy
Journal of Manipulative and Physiological Therapeutics 1992 (Nov); 15 (9): 596598
Giesen JM, Center DB, Leach RA.
An Evaluation of Chiropractic Manipulation as a Treatment of Hyperactivity in Children
Journal of Manipulative and Physiological Therapeutics 1989 (Oct); 12 (5): 353363
Alcantara J, Heschong R, Plaugher G, Alcantara J.
Chiropractic Management of a Patient with Subluxations, Low Back Pain and Epileptic Seizures
Journal of Manipulative and Physiological Therapeutics 1998 (Jul); 21 (6): 410418
Sandefur R, Adams E.
The Effect of Chiropractic Adjustments on the Behavior of Autistic Children: A Case Review
Journal of Chiropractic 1987 (Dec); 24 (12): 21-25
Stephens D, Mealing D, Pollard H, Thompson P, Bilton D, Gorman RF.
Treatment of visual field loss by spinal manipulation.
Journal of the Neuromusculoskeletal System 1998; 6(2): 53-66.
Chinappi AS, Getzoff H.
The Dental-chiropractic Cotreatment of Structural Disorders of the Jaw and Temporomandibular Joint Dysfunction
Journal of Manipulative and Physiological Therapeutics 1995 (Sep); 18 (7): 476481
Hodges PW, Richardson CA.
Inefficient muscular stabilization of the lumbar spine associated with low back pain: A motor control evaluation of transversus abdominus.
Spine 1996; 21: 2640-2650.
Kelly DB, Murphy BA, Backhouse DP.
Use of a mental rotation reaction-time paradigm to measure the effects of upper cervical adjustments on cortical processing: A pilot study.
Journal of Manipulative and Physiological Therapeutics 2000; 23(4): 246-251.
Smith DL, Dainoff MJ, Smith JP.
The effect of chiropractic adjustments on movement time: A pilot study using Fitt's law.
Journal of Manipulative and Physiological Therapeutics 2006; 29(4): 257-266.
Lee KP, Carlini WG, McCormick GF, Walters GW.
Neurologic complications following chiropractic manipulation: A survey of California neurologists.
Neurology 1995; 45(6): 1213-1215.
Bin Saeed A, Shuaib A, Al Sulaiti G, Emery D.
Vertebral Artery Dissection: Warning Symptoms, Clinical Features and Prognosis in 26 Patients
Canadian Journal of Neurological Sciences 2000 (Nov); 27 (4): 292296Hufnagel A, Hammers A, Schonle P-W, Bohm K-D, Leonhardt G.
Stroke following chiropractic manipulation of the cervical spine.
Journal of Neurology 1999; 246(8): 683-688.
Norris JW, Beletsky V, Nadareishvilli ZG,
Canadian Stroke Consortium.
Canadian Medical Association Journal 2000; 163(1): 38-40.
Rothwell DM, Bondy SJ, Williams JI.
Chiropractic Manipulation and Stroke: A Population-based Case-control Study
Stroke 2001; 32 (5): 1054-1060
Smith WS, Johnston SC, Skalabrin EJ, Weaver M, Azari P, Albers GW, Gress DR.
Spinal manipulative therapy is an independent risk factor for vertebral artery dissection.
Neurology 2003; 60: 1424-1428.
Dvorak J, Orelli F.
How dangerous is manipulation of the cervical spine?
Manual Medicine 1985; 2: 1-4.
Patijn J.
Complications in manual medicine: A review of the literature.
Manual Medicine 1991; 6: 89-92.
Haldeman S, Chapman-Smith D, Petersen DM, eds.
Guidelines for Chiropractic Quality Assurance and Practice Parameters
The Mercy Conference ~ Major Recommendations
Gaithersburg, Md: Aspen Publishers Inc; 1993.Jaskoviak PA.
Complications arising from manipulation of the cervical spine.
Journal of Manipulative and Physiological Therapeutics 1980; 3: 213-219.
Henderson DJ, Cassidy JD.
Vertebral artery syndrome:
In Vernon H, ed. Upper cervical syndrome: Chiropractic diagnosis and treatment.
Baltimore: Williams & Wilkins, 1988. 195-222.
Carey PF.
A report on the occurrence of cerebral vascular accidents in chiropractic practice.
Journal of the Canadian Chiropractic Association 1993; 57(2): 104-106.
National Chiropractic Mutual Insurance Company,
unpublished case records 1991-1993.
Haldeman S, Carey P, Townsend M, Papadopoulos C.
Arterial Dissections Following Cervical Manipulation: The Chiropractic Experience
Canadian Medical Association Journal (CMAJ) 2001 2001 (Oct 2); 165: 905906Thiel HW, Bolton JE, Docherty S, Portlock JC:
Safety of Chiropractic Manipulation of the Cervical Spine: A Prospective National Survey
Spine (Phila Pa 1976). 2007 (Oct 1); 32 (21): 23752378Deyo RA, Cherkin DC, Loesser JD, Bigos SJ, Ciol MA.
Morbidity and mortality in association with operations on the lumbar spine: The influence of age, diagnosis, and procedure.
Journal of Bone and Joint Surgery Am 1992; 74(4): 536-543.
Seagroat V, Tan HS, Goldacre M. Bulstrode C, Nugent I, Gill L.
Effective total hip replacement: Incidence, emergency, readmission rate, and post-operative mortality.
British Medical Journal 1991; 330: 1431-1435.
Stremple JS, Boss DS, Davis CH, McDonald GO.
Comparison of post-operative mortality and morbidity in Veterans Affairs and nonfederal hospitals.
Journal of Surgical Research 1994; S6: 405-416.
Roebuck DJ.
Diagnostic imaging: Reversing the focus [letter].
Medical Journal of Australia 1995: 162: 175.
Phillips DP, Christenfeld N, Glynn LM.
Increase in US medication-error deaths between 1983 and 1993.
Lancet 1998; 351: 643-644.
Dabbs V Lauretti WJ
A Risk Assessment of Cervical Manipulation vs. NSAIDs for the Treatment of Neck Pain
J Manipulative Physiol Ther 1995 (Oct); 18 (8): 530536Dinman BD.
The reality and acceptance of risk.
Journal of the American Medical Association 1980; 244 (11):1226-1228.
Rome PL.
Perspectives: An Overview of Comparative Considerations of Cerebrovascular Accidents
Chiropractic Journal of Australia 1999; 29 (3): 87102
Brody J.
When Simple Actions Ravage Arteries
New York Times, April 30, 2001.
Bill Carroll Show, CFRB 1010 radio,
February 6, 2002, posted on the internet.
Evenson B.
National Post, February 7, 2002.
Hamburg J,
Medical Minute, WOR AM 710 radio,
February 22, 2002.
Jaroff L.
Back off, chiropractors!
TIME.com, February 27, 2002.
A different way to heal.
Episode of Scientific American Frontiers
Public Broadcasting System telecast, June 4, 2002.
Reddy M, Redy B, Schoggle A, Saringer W, Matula C.
The complexity of trauma to the cranio-cervical junction: Correlation of clinical presentation with Doppler flow velocities in the V3-segment of the vertebral arteries.
Acta Neurochiropractic (Wien) 2002; 144(6): 575-580.
Haneline M.T., Rosner A.L.
The Etiology of Cervical Artery Dissection
Journal of Chiropractic Medicine 2007; 6 (3): 110120Shievink WT, Mokri, B, O'Fallon WM.
Recurrent spontaneous cervical-artery dissection.
New England Journal of Medicine 1994; 330(6): 393-397.
Shievink WT, Mokri B, Whisnant JP.
Internal carotid artery dissection in a community: Rochester, Minnesota, 1987-1992.
Stroke 1993; 24(11): 1678-1680.
Giroud M, Fayolle H, Andre N, Dumas R, Becker F, Martin D, Baudoin N, Krause D.
Incidence of internal carotid artery dissection in the community of Dijon [Letter].
Journal of Neurology and Neurosurgical Psychiatry 1994; 57(11): 1443.
Carey TS, Garrett J, Jackman A, et al.
The Outcomes and Costs of Care for Acute Low Back Pain Among Patients
Seen by Primary Care Practitioners, Chiropractors, and Orthopedic Surgeons
New England J Medicine 1995 (Oct 5); 333 (14): 913917Terrett, AGJ.
Malpractice avoidance for chiropractors. 1. Vertebrobasilar stroke following manipulation.
Des Moines, IA. National Chiropractic Mutual Insurance Company, 1996.
Foye PM, Najar MP, Camme A Jr, Stitik TP, DePrince ML, Nadler SF, Chen B.
Prospective study of pain, dizziness, and central nervous system blood Flow in cervical extension: Vascular correlations to beauty parlor stroke syndrome and salon sink radiuculopathy.
American Journal of Physical Medicine and Rehabilitation 2002; 81(6): 395-399.
Graham IM, Daley LE, Refsum HM, Robinson K, Brattstrom LE, Ueland PM, Palma-Reis RJ, Boers GH, Sheahan RG, Israelsson B, Uiterwaal CS, Meleady R, McMaster D, Verhoef P, Witterman J, Rubba P, Bellet H, Wautrecht JC, de Valk HW, Sales Luis AC, Parrot-Rouland RM, Tan KS, Higgins I, Garcon D, Medrano MJ, Candito M, Evans AE, Andria G.
Plasma homocysteine as a risk factor for vascular disease: The European Concerted Action Project.
Journal of the American Medical Association 1997; 277: 1775- 1781.
McCully KS.
Vascular pathology of homocysteinemia: Implications for pathogenesis of arteriosclerosis.
American Journal of Pathology 1969; 56(1): 111-128.
Selhub J, Jacques PF, Bostom AG, D'Agostino RB, Wilson PW, Belanger AJ, O'Leary DH, Wolf PA, Schaefer EJ, Rosenberg IH.
Association between plasma homocysteine concentrations and extracranial carotid artery stenosis.
New England Journal of Medicine 1995; 332(5): 286-291.
Wald NJ, Watt HC, Law MR, Weir DG, McPartlin J, Scott JM.
Homocysteine and ischemic heart disease: Results of a prospective study with implications regarding prevention.
Archives of Internal Medicine 1998; 158(8): 862-867.
Nygard O, Nordehaug JE, Refsum H, Ueland PM, Farstad M, Vollset SE,
Plasma homocysteine levels and mortality in patients with coronary artery disease.
New England Journal of Medicine 1997; 337(4): 230- 236.
Stampfer MJ, Malinow R, Willett WC, Newcomer LM, Upson B, Ullmann D, Tishler PV, Hennekens CH.
A prospective study of plasma homoycyst(e)ine and risk of myocardial infarction in US physicians.
Journal of the American Medical Association 1992; 268(7): 877-881.
Harker LA, Slichter J, Scott CR, Russell R.
Homocysteinemia: Vascular injury and arterial thrombosis.
New England Journal of Medicine 1974; 291: 537-543.
Lenz SR, Sobey CG, Piegors DJ, Bohoptakar MY, Faraci FM, Malinow MR, Heistad DD.
Vascular dysfunction in monkey with diet-induced hyperhomocysteinemia.
Journal of Clinical Investigation 1996; 98: 24-29.
Woo KS, Chook P, Lolin YI, Cheung AS, Chan LT, Sun YY, Sanderson JE, Metreweli C, Celermajar DS.
Hyperhomocysteinemia is a risk factor for endothelial dysfunction in humans.
Circulation 1997; 96: 2542-2544.
Charplot P, Bescond A, Augler T, Chereyre C, Fratermo M, Rolland PH, Garcon D.
Hyperhomocysteinemia induces elastolysis in minipig arteries: Structural consequences, arterial site specificity and effect of captoprilhydrochlorothiazide.
Matrix Biology 1998; 17: 559-574.
Rahmani DJ, Rolland PH, Rosset E, Branchereau A, Garcon D.
Homocysteine induces synthesis of a serine elastase in arterial smooth muscle cells from multi-organ donors.
Cardiovascular Research 1997; 34(3): 597-602.
Jackson SH.
The reaction of homocysteine with aldehyde: An explanation of the collagen defects in homocystinuria.
Clinica Chimica Acta 1973; 45(3): 215-217.
Kang AH, Trelstad RL.
A collagen defect in homocystinuria.
Journal of Clinical Investigation 1973; 52(10): 2571-2578.
Wall RT, Harlan JM, Harker LA, Striker GF.
Homocysteine-induced endothelial cell injury in vitro: A model for the study of vascular injury.
Thrombolytic Research 1980; 18: 113-121.
Pezzini A, Del Zotto E, Archetti S, Negrini R, Bani P, Albertini A, Grassi M, Assanelli D, Gasparotti R, Vignolo LA, Magoni M, Padovani A.
Plasma homocysteine concentration, C677T MTHFR genotype, and 844-ins68bp genotype in young adults with spontaneous cervical artery dissection and atherothrombotic stroke.
Stroke 2002; 33(3): 664-669.
Gallai V, Caso V, Paciaroni M, Cardaioli G, Arning E, Bottiglieri T, Pernetti L.
Mild hyperhomocyst(e)inemia: A possible risk factor for cervical artery dissection.
Stroke 2001; 32: 714-718.
Lehninger AL, Nelson DL, Cox MM.
Principles of Biochemistry, 2nd Edition.
New York, NY: Worth, 1993, pp. 524-526.
Ueland PM, Refsum H, Stabler SP, Mainow MR, Anderson A, Allen RH.
Total homocysteine in plasma and serum: Methods and clinical applications.
Clinical Chemistry 1993; 39(9): 1764-1779.
Stabler SP, Marcell PD, Podell ER, Allen RH.
Quantitation of total homocysteine, total cysteine, and methionine in normal serum and urine using capillary gas chromatography-mass spectrometry.
Analytical Biochemistry 1987; 162(1): 185-196.
Pietzsch J, Julius U, Hanefeld M.
Rapid determination of total homocysteine in human plasma by using N(O,S)-ethoxycarbonyl ethyl ester derivatives and gas chromatography-mass spectrometry.
Clinical Chemistry 1997; 43(10): 2001-2004.
Frantzen F, Faaren AL, Alfheim I, Nordhei AK.
Enzyme conversion immunoassay for determining total homocysteine in plasma or serum.
Clinical Chemistry 1998; 44(2): 311-316.
Shipchandler MT, Moore EG.
Rapid, fully automated measurement of plasma homocyst(e)ine with the Abbott IMx analyzer.
Clinical Chemistry 1995; 41(7): 991-994.
Haldeman S, Kohlbeck FJ, McGregor M.
Unpredictability of Cerebrovascular Ischemia Associated with Cervical Spine Manipulation Therapy:
A Review of Sixty-four Cases After Cervical Spine Manipulation
Spine (Phila Pa 1976) 2002 (Jan 1); 27 (1): 4955McGregor M, Haldeman S, Kohlbeck FJ.
Vertebrobasilar compromise associated with cervical manipulation.
Topics in Clinical Chiropractic 1995; 2(3): 63-73.
Terrett AGL.
It is more important to know when not to adjust.
Chiropractic Technique 1990; 2: 1-9.
Bolton PS, Stick PE, Lord RSA.
Failure of clinical tests to predict cerebral ischemia before neck manipulation.
Journal of Manipulative and Physiological Therapeutics 1989; 12(4): 304-307.
Ferezy JS.
Neural ischemia and cervical manipulation: An acceptable risk.
ACA Journal of Chiropractic 1988; 22: 61-63.
Current Concepts: Spinal Manipulation and Cervical Arterial Incidents
(Triano JJ, Kawchuk G [Eds]). Clive, IA:
NCMIC Insurance Company, 2006, pp. 44-47.
Rivett D, Milburn P.
Complications arising from spinal manipulative therapy in New Zealand.
Physiotherapy 1997; 83: 626-632.
Rydell N, Raf L.
Spinal manipulation-treatment associated with a high risk of complications.
Lakartidningen 1999; 96: 3536-3540.
Assendelft WJ, Bouter LM, Knipschild PG.
Complications of spinal manipulation: A comprehensive review of the literature.
Journal of Family Practice 1996; 42: 475-480.
Powell F, Hanigan W, Olivero W.
A risk/benefit analysis of spinal maniplation therapy for relief of lumbar or cervical pain.
Neurosurgery 1993; 3: 73-79.
Haldeman S, Rubinstein SM.
Cauda equina syndrome in patients undergoing manipulation of the cervical spine.
Spine 1992; 17: 1469-1473.
Oliphant D.
Safety of Spinal Manipulation in the Treatment of Lumbar Disk Herniations:
A Systematic Review and Risk Assessment
J Manipulative Physiol Ther 2004 (Mar); 27 (3): 197210Hurwitz EL, Morgenstern H, Vassilaki M, Chiang I-M.
Frequency and clinical predictors of adverse reactions to chiropractic care in the UCLA Neck Pain Study.
Spine 2005; 30(13): 1477-1484.
Vohra, S, Johnston, BC, Cramer, K, and Humphreys, K.
Adverse Events Associated with Pediatric Spinal Manipulation: A Systematic Review
Pediatrics. 2007 (Jan); 119 (1): e275e283Rubinstein SM, Leboeuf-Yde C, Knol DL, de Koekkoek TE,
Pfeifle CE, van Tulder MW.
The Benefits Outweigh the Risks for Patients Undergoing Chiropractic
Care for Neck Pain A Prospective, Multicenter, Cohort Study
J Manipulative Physiol Ther 2007 (Jul); 30 (6): 408418Hill AB.
The environment and disease association, causation? President's Address.
Occupational Medicine 1965; 195-198.
Terrett AGJ:
Misuse of the Literature by Medical Authors in Discussing Spinal Manipulative Therapy Injury
J Manipulative Physiol Ther 1995 (May); 18 (4): 203210Cassidy JD, Boyle E, Cote P, et al.
Risk of Vertebrobasilar Stroke and Chiropractic Care: Results of a Population-based
Case-control and Case-crossover Study
Spine (Phila Pa 1976) 2008 (Feb 15); 33 (4 Suppl): S176183Kier AL, McCarthy PW.
Cerebrovascular Accident Without Chiropractic Manipulation: A Case Report
J Manipulative Physiol Ther 2006 (May); 29 (4): 330335Smith C, Cowan C, Sensening A, Catlin A,
Health Accounts Team. Health spending slows in 2003.
Health Affairs2006; 24(1): 186-194, reported by Kaufman M, Stein R.
Record share of economy is spent on health care.
Washington Post January 10, 2006, p. A01.
Luo X, Pietrobon R, Sun SX, Liu GG, Hey L.
Estimates and Patterns of Direct Health Care Expenditures Among Individuals
With Back Pain in the United States
Spine (Phila Pa 1976) 2004 (Jan 1); 29 (1): 7986Deyo RA, Mirza SK, Turner JA, Martin BI.
Overtreating Chronic Back Pain: Time to Back Off?
J Am Board Fam Med. 2009 (Jan); 22 (1): 6268The Back Letter 2004; 12(7): 79.
Deyo RA.
Low-back pain.
The Scientific American 1998; 49-53.
Manga P.
Economic Case for the Integration of Chiropractic Services into the Health Care System
Journal of Manipulative and Physiological Therapeutics 2000 (Feb); 23 (2): 118122
Baldwin ML, Cote P, Frank JW, Johnson WG.
Cost-effectiveness studies of medical and chiropractic care for occupational low back pain: A critical review of the literature.
The Spine Journal 2001; 1: 138-147.
Branson RA.
Cost Comparison of Chiropractic and Medical Treatment of Common Musculoskeletal Disorders:
A Review of the Literature After 1980
Topics in Clinical Chiropractic 1999; 6 (2): 5768http://swbc.georgia.gov/vgn/images/portal/cit_1210/21/
6/12724921At_A_Glance04.pdf.
Hooper P.
Dynamic Chiropractic 1994; 12(25).
Eccleston SM, Zhao X.
The anatomy of workers' compensation medical costs and utilization: Trends and interstate comparisons, 1996-2000.
Cambridge, MA: Workers Compensation Research Institute WC- 03-04, 2003.
Victor RA, Wang W.
Patterns and cost of physical medicine: Comparison of chiropractic and physician-directed care.
Cambridge, MA: Workers Compensation Research Institute, WC-02-07, 2002.
Folsom BL, Holloway RW.
Chiropractic care of Florida workers' compensation claimants: Access, costs and administrative outcome trends from 1994 to 1999.
Topics in Clinical Chiropractic 2002; 9(4): 33-53.
MGT of America, Inc.
Chiropractic Treatment of Workers' Compensation Claims in Texas
(Report commissioned by the Texas Chiropractic Association).
MGT of America, Inc., Tallahassee (FL); 2003Phelan S, Armstrong R, Knox D, Hubka M, Ainbinder D.
An Evaluation of Medical and Chiropractic Provider Utilization and Costs:
Treating Injured Workers in North Carolina
J Manipulative Physiol Ther 2004 (Sep); 27 (7): 442448Benefits of expanded access to chiropractic care in the Oklahoma Workers' Compensation System.
MGT report for Unified Chiropractic Association of Oklahoma, February 25, 2005.
Ebrall PS.
Mechanical Low-Back Pain: A Comparison of Medical and Chiropractic Management Within the Victorian WorkCare Scheme
Chiropractic Journal of Australia 1992 (Jun); 22 (2): 4753
Tuchin P.J., Bonello R.
Preliminary Findings of Analysis of Chiropractic Utilization and Cost in the Workers'
Compensation System of New South Wales, Australia
J Manipulative Physiol Ther 1995 (Oct); 18 (8): 503511Jarvis K.B., Phillips R.B., Morris E.K.
Cost Per Case Comparison of Back Injury Claims of Chiropractic Versus Medical Management
For Conditions With Identical Diagnostic Codes
J Occup Med 1991 (Aug); 33 (8): 847852Johnson M.R., Schultz M.K., Ferguson A.C.
A Comparison of Chiropractic, Medical and Osteopathic Care for Work-related Sprains and Strains
J Manipulative Physiol Ther 1989 (Oct); 12 (5): 335344Wolk S.
An Analysis of Florida Workers' Compensation Medical Claims for Back-related Injuries
Journal of the American Chiropractic Association 1988; 27(7): 50-59Nyiendo J.
Disability low back region workers compensation of claims. Part III: Diagnostic and treatment procedures and associated costs.
Journal of Manipulative and Physiological Therapeutics 1991; 14(5): 287-297.
Stano M.
The economic role of chiropractic: Further analysis of relative insurance costs for low back care.
Journal of the Neuromusculoskeletal System 1995; 3(3): 139-144.
Stano M, Smith M:
Chiropractic and Medical Costs of Low Back Care
Medical Care 1996 (Mar); 34 (3): 191204Haas M, Sharma R, Stano M.
Cost-effectiveness of Medical and Chiropractic Care for Acute and Chronic Low Back Pain
J Manipulative Physiol Ther 2005 (Oct); 28 (8): 555563UK BEAM Trial Team. United Kingdom Back Pain Exercise and Manipulation [UKBEAM] Randomised Trial: Cost-effectiveness of Physical Treatments For Back Pain in Primary Care
British Medical Journal 2004 (Dec 11); 329 (7479): 1381
Sarnat RL, Winterstein J, Cambron JA.
Clinical Utilization and Cost Outcomes from an Integrative Medicine Independent
Physician Association: An Additional 3-year Update
J Manipulative Physiol Ther 2007 (May); 30 (4): 263269Sarnat RL, Winterstein J, Cambron JA.
Clinical Utilization and Cost Outcomes from an Integrative Medicine Independent
Physician Association: An Additional 3-year Update
J Manipulative Physiol Ther 2007 (May); 30 (4): 263269Legorreta, AP, Metz, RD, Nelson, CF, Ray, S, Chernicoff, HO, and Dinubile, NA.
Comparative Analysis of Individuals With and Without Chiropractic Coverage:
Patient Characteristics, Utilization, and Costs
Archives of Internal Medicine 2004 (Oct 11); 164 (18): 19851892Metz, RD, Nelson, CF, LeBrot, T, and Pelletier, KR.
Chiropractic Care: Is It Substitution Care or Add-on Care in Corporate Medical Plans?
J Occup Environ Med 2004 (Aug); 46 (8): 847855Nelson CF, Metz RD, LaBrot T.
Effects of a Managed Chiropractic Benefit on the Use of Specific Diagnostic
and Therapeutic Procedures in the Treatment of Low Back and Neck Pain
Journal of Manipulative and Physiological Therapeutics 2005 (Oct); 28 (8): 564569Muse & Associates.
Utilization, Cost, and Effects of Chiropractic Care on Medicare Program Costs
Washington, DC, July 2001.
Korthals-deBos IBC, et al.
Cost Effectiveness of Physiotherapy, Manual Therapy, and General Practitioner Care
for Neck Pain: Economic Evaluation Alongside a Randomised Controlled Trial
British Medical Journal 2003 (Apr 26); 326 (7395): 911Manga P.
Enhanced Chiropractic Coverage Under OHIP as a Means for Reducing Health Care Costs, Ataining Better Health Outcomes and Achieving Equitable Access to Health Services
Report to the Ontario Ministry of Health, 1998 (Feb).
Institute of Medicine Committee on Quality of Health Care in America.
Crossing the Quality Chasm: A New Health System for the 21st Century
Washington, DC: National Academies Press; 2001Vogel AR, Paul S.
Follow-up: Bridging the gap between discharge and home.
Occupational Therapy in Health Care 2000; 13(1): 61-80.
Rupert RL, Manello D, Sandefur R.
Maintenance Care: Health Promotion Services Administered to US Chiropractic Patients Aged 65 and Older, Part II
Journal of Manipulative and Physiological Therapeutics2000 (Jan); 23 (1): 1019
Cooper SR, Pfefer MT.
Development of an on-site industrial chiropractic program.
Proceedings of the 9th Biennial Congress of the World Federation of Chiropractic,
Vilamoura, PORTUGAL, May 17-19, pp. 202-204.
Hoskins W, Pollard H.
The effects of sports chiropractic on the prevention of athletic injuries in elite athletes: A randomized, controlled trial.
Proceedings of the 9th Biennial Congress of the World Federation of Chiropractic,
Vilamoura, PORTUGAL, May 17-19, pp. 163-164.
Aure OF, Nilsen JH. Vasseljen O.
Manual Therapy and Exercise Therapy in Patients With Chronic Low Back Pain: A Randomized, Controlled Trial With 1-Year Follow-Up
SPINE (Phila Pa 1976) 2003 (Mar 15); 28 (6): 525531
Evans DW.
Mechanisms and effects of spinal high-velocity, low-amplitude thrust manipulation: Previous theories.
Journal of Manipulative and Physiological Therapeutics 2002; 25: 251-262.
Tricoci P, Allen JM, Kramer JM, Claliff RM, Smith SC.
Scientific evidence underlying the ACC/AMA Clinical Practice Guidelines
Journal of the American Medical Association 2009 (Apr 15); 301 (15): 1544
The Data Tables
TABLE 1: Clinical Care Methods: Strength of Evidence
as determined by AHRQ [5]
INTERVENTION EVIDENCE RESULT STRENGTH OF EVIDENCE 1. Patient Education + C 2. Back School + C 3. Acetaminophen + C 4. NSAIDs + B 5. Phenylbutazone C 6. Muscle Relaxants + C 7. Opiod Analgesics + C 8. Oral Steroids B 9. Colchicine B 10. Antidepressants B 11. Spinal Manipulation + B 12. Physical Agents/Modalities [a] [b] C 13. TENS C 14. Shoe Insoles + C 15. Shoe lifts [Lower Limb diff <2 cm] D 16. Lumbar Corsets/Back Belts D 17. Traction B 18. Biofeedback C 19. Trigger Point Injections C 20. Ligamentous/Sclerosant Injections C 21. Facet Point Injections C 22. Epidural Injectionsc [No Radiculopathy] D 23. Epidural Injections [c] [Radiculopathy] [d] + C 24. Acupuncture D 25. Limited Activity + D 26. Bed Rest >4 Days B 27. Conditioning Exercise + C
[a] = Includes ice, heat [including diathermy], massage, ultrasound, cutaneous laser treatment, electrical stimulation excluding TENS.
[b] = Insufficient proven benefit to justify their cost.
[c] = Steroids, lidocaine, opioids.
[d] = After failure of conservative treatment as a means to avoid surgery.
TABLE 3: Neural Responses to External Forces in Animal Models
Animal Intervention Effect Observed Mouse [77] Ligature implant around sciatic nerve Inflammation
Reduced nerve conduction velocity
Facilitation
Motor disturbances in gaitRat [78] External pressure on L6 Slower nerve conductivity Rat [36] Surgical clamp insertion with bending at T10-T11 Decreased blood pressure
Decreased renal nerve activityRat [79] Ligature implant around sciatic nerve Changes in gait
Changes in nerve conduction velocity
Enzymatic changes in denervated musclesRabbit [80] Manual manipulation Gastric smooth muscle inhibition Dog [81] Surgery plus glue injection into bilateral apophyseal joints in upper lateral spine Impairment of natural killer lymphocytes Rabbit [82] Miniature compression cuff around 1 sciatic nerve Decreased aldolase activity
Decreased lactic dehydrogenase activityCat [83] Surgical preparations
Percutaneous bradykinin injections into motion segmentSlowly increasing excitatory discharges
Expansion of receptive fields
Hyperresponsiveness to subsequent stimRat [84] Mustard oil injection into pararticular space around C2-C3 joint Excitatory effects in muscles that were not local, including biphasic response Cat [85] T3 and T4 dorsal nerve stim stimulation Activated cardiac somatosympathetic reflexes Rat [86] Dorsal spinal afferent nerve Specific somatosympathetic reflex stimulation
TABLE 4: Clinical Outcome Instruments in Chiropractic Research
TABLE 5: Scoring Criteria for Randomized Clinical Trials [147]
Similarity of baseline characteristics or adjusted effects reported
Concealment of treatment allocation
Blinding of patients
Blinding of provider/attention bias
Blinding of assessor/unbiased outcome assessment
Dropouts reported and accounted for in analysis
Missing data reported and accounted for in analysis
Intention-to-treat analysis/balanced cointervention
1.0 point awarded for YES rating
0.5 point awarded for PARTIAL rating
0.0 point awarded for NO rating
Quality score is calculated by dividing point total by 8 and multiplying the result by 100 to create a 100-point scale.
TABLE 6: CCGPP Evidence Ratings for Low-back Pain Interventions:
Summary of Conclusions [161]
TOPIC STRENGTH
OF
EVIDENCE [a]Acute LBP [<6 wk duration]:
Manipulation
Exercise
Specific exercise
A
I
CSubacute LBP [6-12 wk duration]:
Manipulation
Assurance/advice to stay in activities of daily living
Customizable exercise programs
Intensive training for severe pain
A
B
B
CChronic LBP [>12 wk duration]:
Manipulation
Exercise
Assurance/advice to stay in activities of daily living
A
B
BPostsurgical rehabilitation:
Exercise
CSciatica/radicular/radiating leg pain:
Manipulation
Assurance/advice to stay in activities of daily living
C
BConclusions exclude patients with red flag findings [contraindications to manipulation].
[a] Grades:
A: Good evidence from relevant studies
B: Fair evidence from relevant studies
C: Limited evidence from studies/reviews
I: No recommendations made because of insufficient or nonrelevant evidence.
Assendelft et al: [164]
Comparative side effects and relative safety issues are not addressed.
There is a mix of clinical judgment without foundation in evidence reviewed.
There are inadmissable criteria of quality.
The findings are in conflict with those of several national guidelines. [5-11]
Meta-analyses themselves are subject to bias and omissions.
There are contradictions in design when comparisons are made to sham treatments, general actitioners, analgesics, back school, exercise, physical therapy, and treatments considered to be inferior or harmful.
There are contradictions in evaluating clinical and statistical significance.
Data are not shown in areas of interest.
Fastidious treatments are not the same as complete clinical interventions.
There is a lack of long-term followup.
Cherkin et al: [165]
There is a failure to resolve conflicting reviews.
Exclusions of previous studies are difficult to rationalize.
Studies of questionable quality are included.
Ernst and Canter: [166]
There is a systematic bias in the current review.
The averaging of disparate methodologies and conclusions is arbitrary.
There are biases and omissions in other systematic reviews and meta-analyses cited.
Comparative side effects and relative safety issues are not addressed.
There are flaws in studies in which previous systematic reviews are based.
AUTHOR DESIGN #S AGE INTERVENT OUTCOME → RESULTS Wiberg [299] RCT 25 2-10 wk
SMT F
DimethiconeCrying [hrs]
70% drop, 5 days
20% drop, 5 daysOlafsdottir [300] RCT
32
243-9 wk
SMT F
Held 10 minSymptom scale
Improvement 70%
Improvement 60%Mercer [301] RCT
15
160-8 wk
SMT
Detuned USParent diary
93% resolved, 2 wk
NoneKlougart [302] PC 316 2-16 wk SMT F Crying [hrs]
75% drop, 14 daysLeach [303] Case
Study2 6-9 wk SMT I Crying [hrs]
50% drop after 1-4xPluhar [304] Case
Study1 12 wk HVLA and I Symptom
Resolved
RemissionVan Loon [305] Case
Study1 12 wk SMT
Diversified
WebsterSymptom
Resolved
RemissionRCT = Randomized Clinical Trial
PC = Prospective cohort
SMT = Spinal Manipulative Therapy
US = Ultrasound
HVLA = High velocity low-amplitude
F = Spinal manipulation applied with light fingertip pressure
I = Instrument-assisted [Activator or PulStar FRAS Sense Technology, Inc.]
x = Number of treatments
AUTHOR DESIGN #S AGE INTERVENT OUTCOME → RESULTS Reed [307] RCT
31
155-13 yr
SMT
ShamWet nights/2 wk
16%
0% < baselineLeBouef [308] Cohort 171 4-15 yr SMT Wet nights/wk
75% no responseBlomerth [309] Case 1 8 yr SMT Symptom Remission
ResolvedGemmell [310] Case 1 14 yr SMT T Dry/damp/wet
Trend to drynessP = Spinal manipulation, Palmer Package Adjusting Technique [311]
T = Spinal manipulation, Toggle Recoil
Sham = Activator at nontension setting
TABLE 10: Summary of Leading Outcomes Studies Involving Spinal
Manipulation For Managing Asthma
AUTHOR DESIGN #S AGE INTERVENT OUTCOME → RESULTS Balon [316] RCT 38
427-16 yr SMT D + S
ShamPEF Small rise
FEV No change
QOL Improved
Guiney [317] RCT 140 5-17 yr OMT
Sham touchPEF Significant rise
Nilsson [318] RCT 31 18-44 yr Dr
ShamLung function Unchanged
Symptoms Improved
Hyperreactivity ImprovedAli [113] RCT 150 C
C
h
wAQ SMT decreased
SF-36 SMT decreased
DASS SMT decreased
Cortisol SMT decreased
IgA SMT increasedBronfort [319] Pilot RCT 22
126-17yr SMT
ShamPEF N.S. change
FEV N.S. change
QOL Significant rise
Severity Significant drop
Symptoms No changeNilsson [320] RC 79 2-63 yr SMT Symptoms Resolved Brocken [321] Crossover 10 >18yr Thoracic exclus
ShamSignificantly reduced
No changeJamison [322] Cohort 15 8-45 yr SMT, Mob, Exer Medication use Reduced
Spirometry No changePeet [323] Cohort 8 4-12 yr SMT [CBP] Medication use Reduced
PEF ReducedLines [324] Case series 3 2-30 yr Chiro Symptoms Reduced
Medication use ReducedGarde [325] Case 1 6 yr SMT Inhaler use Ceased Hunt [326] Case 1 4 yr SMT I Symptoms Resolved Killinger [327] Case 1 18 yr SMT
[Palmer UC]Health status Improved Peet [328] Case 1 8 yr SMT Medication use Ceased OMT = Osteopathic Manipulative technique
D = Spinal manipulation, Diversified
S = Soft tissue techniques
Dr = Spinal manipulation with drop table
I = Instrument assisted
PEF = Peak expiratory flow
FEV = Forced expiratory volume
QOL = Pediatric Quality of Life Questionnaire
CBP = Chiropractic Biophysics
UC = Upper cervical
Mob = Mobilization
Exer = Exercise
C = Treatment at centers
c = Nontreatment at centers
h = Nontreatment at home
w = Nonsymptomatic patients at home
AQ = Asthma questionnaire
DASS = Depression and anxiety stress scale
PC = Retrospective case series
N.S. = Not significant
AUTHOR DESIGN #S AGE INTERVENT OUTCOME → RESULTS Hondras [123] RCT 138 18-45 yr SMT Side post
Sham side postVisual analog Both groups decreased
PGE [2] Both groups decreasedThomason [127] RCT Pilot 8 17-35 yr SMT HVLA
Sham I
No treatmentSymptoms Improved
No change
No changeKokjohn [122] RCT Pilot 45 20-49 yr SMT Side post
Sham side postVisual analog Decrease in SMT group
PGE [2] Decrease in SMT groupSnyder [331] RCS 26 SMT Toftness MDQ Improvement Walsh [332] Crossover 25 20-47 yr HVLA soft tiss Menstrual dist Decrease in SMT group Wittler [333] Case series 11 23-42 yr HVLA Gonstead Symptom Improvements in all Stude [334] Case 1 35 yr HVLA side post Symptom Improvement RCT = Randomized Clinical Trial
HVLA = High velocity low-amplitude
RCS = Randomized comparison study
Side post = Side posture
AUTHOR DESIGN #S AGE INTERVENT OUTCOME → RESULTS Mills [339] RCT 57 6 mo
6 yrRC
RC + OMTAOM episodes Reduced
Surgeries ReducedSawyer [340] RCT Pilot 22 6 mo
6 yrSMT Otoscopy Feasibile
Tympanometry
DiariesFroehle [341] Case series 46 <5 yr SMT A
SOT
AKParental decis 93% Fallon Case series 332 [342]
401 [343]<5 yr RF
D,G SMT
STEOtoscopy Resolved
Tympanometry ResolvedFysh [344] Case series 5 1-5 SMT [HVLA] Otoscopy Resolved Phillips [345] Case 1 23 mo SMT A Ear drainage, Reduced Pain Peet [346] Case 1 5 yr SMT [CBP] Clinical obs Resolved Thomas [347] Case 1 1 yr SMT Clinical obs Resolved RC = Regular care
OMT = Osteopathic manipulative therapy
SMT = Spinal manipulative therapy
HVLA = High velocity, low-amplitude
A = Activator
CBP = Chiropractic Biophysics
SOT = Sacro-occipital technique [occasionally]
AK = Applied kinesiology [occasionally]
D = Diversified
G = Gonstead
STE = Soft tissue effleurage
RF = 3o rotation, 5o lateral flexion
ep = Episodes
AUTHOR DESIGN #S AGE INTERVENT OUTCOME → RESULTS Goertz [137] RCT 140 25-60yr SMT/PT/diet
DietNo significant changes Yates [131] RCT 21 35-60 yr SMT I Sys BP SMT decrease Yates [131] RCT 21 35-60 yr SMT I
ShamSys BP SMT decrease
Dias BP Sham no changeBakris [134] RCT Pilot 26 21-75 yr SMT [NUCCA]
ShamSys BP SMT decrease
Dias BP Sham no changePlaugher [349] RCT Pilot 23 24-50 yr SMT Gonst
Light massage
No treatmentFeasibility Morgan [350] Crossover 29 48-50 yr OMT, soft tiss BP No significant change Wagnon [133] Crossover 18 20-50 yr SMT Gonst BP No significant change
Serum aldost Significant decreaseMcKnight [132] Cohort 75 20-35 yr SMT Sys BP Significant drop 14/53
Dias BP Significant drop 1/22Knutson [351] Nonequivalent 54 20-83 yr SMT
No treatmentSys BP Significant decrease
Dias BP No changeFischera [352] Nonequivalent 35 NL
22 hypertensOMT BP Greater decrease in hypertensive Goodman [353] Case series 8 SMT BP Decrease in 6/8 Connelly [354] Case series 3 41-74 yr SMT SOT BP Decrease in 2/3 Plaugher [355] Case 1 SMT Gonst BP Decrease McGee [356] Case 1 46 yr SMT HVLA BP Decrease OMT = Osteopathic manipulative treatment
PT = Adjunctive physical therapy techniques
Gonst = Gonstead chiropractic technique
SOT = Sacro Occipital Technique
NUCCA = National Upper Cervical Chiropractic Adjustment
Sys = Systolic blood pressure
Dias = Diastolic blood pressure
NL = Normal blood pressure
AUTHOR DESIGN #S AGE INTERVENT OUTCOME → RESULTS Budgell [97] RCT 25 21-40 yr Cervical SMT
ShamHRV LF increase
No changeBudgell [98] RCT 28 18-40 yr Thoracic SMT
ShamHRV LF increase
No changeWelch [99] Case series 3 44-50 yr
47-55 yrCervical SMT
Thoracic SMTHRV LF/HF decrease (p)
LF/HF increase (s)Budgell [369] Case 1 23 yr Cervical SMT HRV Lost trigeminal pulse
Bradycardia remainsLF = Low frequency, power analysis
HF = High frequency, power analysis
(p) = Parasympathetic increase
(s) = Sympathetic increase
Condition Reference Irritable bowel syndrome 371 Chronic constipation 372 Multiple sclerosis 373 Bell's Palsy 374 Hyperactivity 375 Epilepsy 376 Autism 377 Recovery of visual field loss 378 Temporomandibular joint dysfunction 379
TABLE 16: Probability of Stroke or Serious Adverse Events
Following Cervical Manipulation
SOURCE METHOD RISK Dvorak [389] Survey of 203 members of Swiss Society of Manual Medicine [all non-chiropractors] 1 serious complicaton/400,000 Patijn [390] Review of computerized registration system in Holland 1 complication/518,000 Haldeman [391] Extensive literature review to formulate practice guidelines 1-2 strokes/1,000,000 Jaskoviak/ [392]
HendersonClinical files of National College/ 15 year period 0 complication/5,000,000 Cassidy [393] Canadian Memorial Chiropractic College Clinic 0 complication/5,000,000 Hurwitz [266] RAND cervical study literature review 0.64 serious complication/1,000,000
0.27 death/1,000,000Carey [394] Claim review: Canada's largest malpractice insurance company 1 CVA/3,000,000
0 deaths/ 5 year periodNCMIC [395] Claim review: principal chiropractic malpractice insurance company within U.S. (3 year period) 1 CVA/2,000,000 Haldeman [396] Claim review: Canada's largest malpractice insurance company (10 year period) 0.17 CVA/1,000,000 Thiel [397] U.K. survey of 28,807 treatment consultatations 0 adverse event
TABLE 17: Risks in Perspective:
Comparison of Death Rates Attributed to Various Causes
RISK FREQUENCY [PER MILLION] Neurological complications from cervical manipulation 0.3 [266] Canoeing 10 [404] Soccer, football 39 [404] Drinking: 1 bottle of wine per day 75 [404] Automobile driving [United Kingdom] 169 [404] Nuclear bone scan 333 [401] GI bleeding due to NSAID use 400 [403] Spinal surgery 700 [398] Total hip replacement 4,900-15,300 [399] Smoking: 20 cigarettes per day 5,000 [404] Medication errors, outpatient 7,633 [402] Appendectomies 13,500 [400] Motorcycling 20,000 [404] Automobile driving [United Kingdom] 169 [404]
TABLE 18: Rates of Stroke Compared to Incidence of Arterial Dissections
RISK FREQUENCY [PER MILLION] Spontaneous, hospital-based [414] 10-15 Spontaneous, community-based [415, 416] 25-30 Cervical manipulation [389] 25 Cervical manipulation [390] 10-20* Cervical manipulation [392] 0 Cervical manipulation [266] 6.4* Cervical manipulation [394] 1.7* *Corrected to represent the average incidence per patient, assuming the average number of manipulations per patient is equal 10, as is reported in the literature. [417]
TABLE 19A: Selected Activities Suspected of Disrupting Cerebral Circulation [405]
Angiography
Bleeding nose
Axial traction
Calisthenics
Cervical extension for xrays or CTS
Cervical rotation while backing up a car
Coughing
Dental procedure
Football
Gymnastics
Hanging out washing
Overhead work
Roller coaster
Telephone call
Traction and short wave diathermy
Trampoline
Watching aircraft
Yawning
TABLE 19B: Nonmanipulative Maneuvers Associated With CVAs [418]
Childbirth
By surgeon or anethetist during surgery
Calisthenics
Yoga
Overhead work
Neck extension during radiography
Neck extension for a bleeding nose
Turning the head while driving a vehicle
Archery
Wrestling
Emergency resuscitation
Star gazing
Sleeping position
Swimming
Rap dancing
Fitness exercise
Beauty parlor stroke
Tai Chi
TABLE 20: Workers' Compensation Benefits in Georgia [469]
Total WEEKLY Benefits Paid Out YEAR Claim Group 2001 2002 2003 2004 M.D $115,590,118 $ 98,419,180 $ 71,025,150 $ 18,786,118 Pharmacy $ 22,426,219 $ 16,292,692 $ 13,310,026 $ 2,228,745 PT $ 24,696,617 $ 22,731,637 $ 15,669,193 $ 4,087,587 D.C. $ 850,247 $ 641,805 $ 581,687 $ 184,654 
Return to HEADACHE
Return to CHIROPRACTIC RESEARCH
Return to EVIDENCEBASED PRACTICE


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |