

Development of an Outcome Assessment Instrument
for Suboptimal Breastfeeding in Infants with
Musculoskeletal DysfunctionThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Clinical Chiropractic Pediatrics 2020 (Jun); 19 (1): 1621–1328 ~ FULL TEXT
OPEN ACCESS FROM: J Clinical Chiropractic Pediatrics 2022 (Nov); 21 (2): 1902–1903 ~ FULL TEXT
Cheryl Hawk, DC, PhD, Sharon Vallone, DC, FICCP, Jessie Young, DC and Valérie Lavigne, DC, MSc
Cheryl Hawk, DC, PhD
Professor, Texas Chiropractic College,
Pasadena, TX
Objectives: 1) to develop an outcome assessment instrument for suboptimal breastfeeding, the Musculoskeletal Infant Breastfeeding Assessment Questionnaire (MIBAQ); and 2) to collect preliminary data on short-term breastfeeding outcomes of infants receiving chiropractic care.
Methods: This descriptive cohort study was conducted in chiropractic offices using practice-based research methods. Participating Doctors of Chiropractic (DC) all reported frequently providing chiropractic care to infants with musculoskeletal imbalances accompanied by suboptimal breastfeeding. Their staff collected and transmitted data electronically to the central site. Participants were mothers of breastfeeding infants < 6 months of age first presenting for nursing dysfunction during the study period. Data forms were a brief focused history, pre-Musculoskeletal Infant Breastfeeding Assessment Questionnaire (MIBAQ), one-week post-MIBAQ and patient disposition. MIBAQ content was based on published observer-based questionnaires. The post-form included the Patient’s Global Impression of change (PGIC). The MIBAQ consisted of 23 questions about suckling-related symptoms using a 4-point Likert scale. Responses were summed for a total score (0-69). Pre- and post-scores were compared using a paired t-test. The Pearson correlation between the change score and the PGIC was also calculated.
Results: From May 15 through August 15, 2019, data were collected from 94 participants in 10 chiropractic offices; 100% collected the pre-MIBAQ and 81% the post-MIBAQ. Infants’ mean age was 51 days. The difference between the mean pre-MIBAQ score (23.5) and post-(one-week) MIBAQ score (17.1) was highly significant (p< .000), as was the correlation between the change score (6.4 points) and the PGIC (76% reported improvement; Pearson correlation= .562).
Conclusion: The MIBAQ appears to be a feasible instrument for use in chiropractic practices, and correlates highly with the PGIC, an established general outcome measure.
From the Full-Text Article:
Introduction
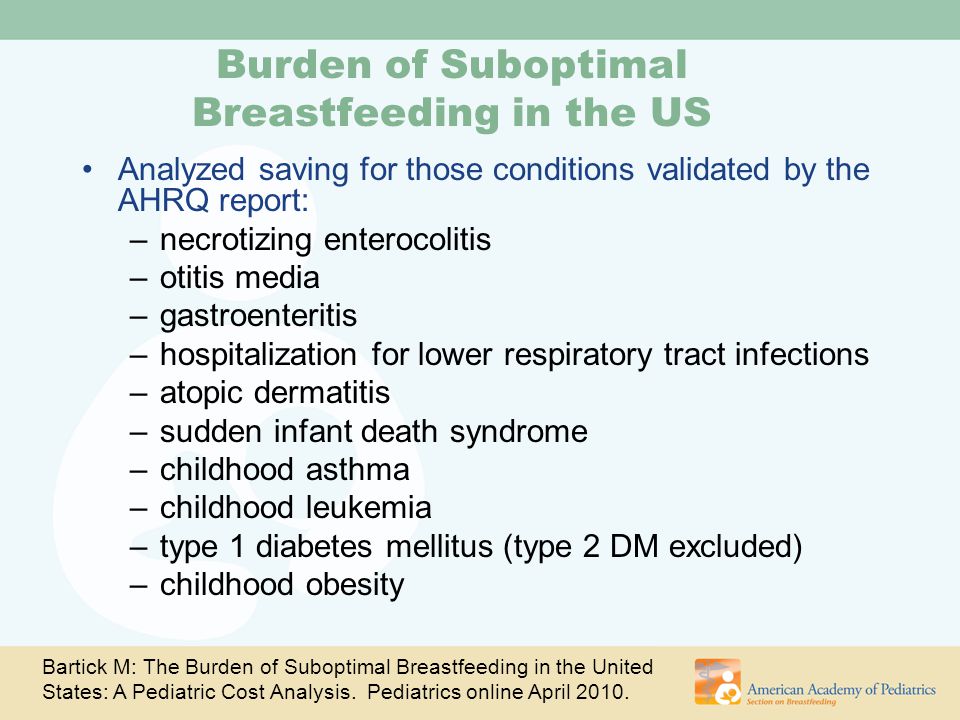
Authorities worldwide strongly recommend exclusively breastfeed for infants’ first six months, [1–4] and the World Health Organization further recommends that breastfeeding should continue, along with age-appropriate foods, to at least two years of age. [5] Anything less than these intervals is termed suboptimal breastfeeding. [1, 6] The 2015 United States Centers for Disease Control and Prevention statistics show that although 83% of infants started life breastfeeding, only 25% were exclusively breastfed at six months and by the age of 12 months, only 36% were breastfed at all. [7, 8]
Why is this the case, when it is universally acknowledged that “breast is best” for both infant and mother? [1, 2, 4, 6, 7] Many complex factors contribute to suboptimal breastfeeding, and public health agencies address factors at the community level and policy level. [9] Healthcare providers such as physicians, nurses, chiropractors and lactation counselors, who work directly with patients/clients, are advised by authorities such as the U.S. Preventive Services Task Force (USPSTF) to counsel new parents and provide them with information to encourage breastfeeding. [3]
Musculoskeletal factors
Although the biomechanics and physiology of infants’ suckling are known, [10–12] until fairly recently there has been a lack of emphasis on correcting musculoskeletal and/or biomechanical factors present in the infant which might interfere with successful breastfeeding, possibly due to the primary practitioner not recognizing them. [13] This is changing, with providers in medicine, osteopathic medicine, nursing, lactation counseling, chiropractic and dentistry beginning to explore the role of infant musculoskeletal issues in breastfeeding.
This includes not only biomechanical factors such as the mother properly positioning the infant, [14] but also musculoskeletal issues in the infant which interfere with the biomechanics of breastfeeding. The biomedical literature is increasing its attention to soft tissue dysfunctions such as ankyloglossia (tongue-tie), [15] which is often treated surgically and has been found to improve the infant’s ability to nurse successfully. [15–18]
However, little discussion is focused around differentiating the structural and functional components of ankyloglossia. The symptoms of tongue-tie and musculoskeletal dysfunction are similar because both create biomechanical alterations that result in similar symptoms. Normal anatomic variations of frenula coupled with compensatory musculoskeletal dysfunction also create issues that can lead to biomechanical alterations resulting in confounding symptoms complicating cases even further. Ruling out musculoskeletal issues such as TMJ dysfunction, myofascial tension involved in turning the head and sucking, segmental dysfunction and cranial asymmetries are important factors in cases of suboptimal breastfeeding to ensure proper breastfeeding biomechanics and differential diagnosis for proper treatment.
A recent scoping review found moderate-strength, favorable evidence, based on the GRADE criteria, [19] for the effectiveness of manual therapy, including chiropractic and osteopathic manipulation and soft tissue therapies, on suboptimal breastfeeding. [20] Because this evidence is still emergent, manual interventions which might improve infants’ ability to nurse effectively do not appear to be included in current guidelines. Since the existing evidence is promising, it is important that further research be conducted. To date, there has only been one randomized controlled trial (RCT) on the topic, in which osteopathic manipulation and soft tissue therapy, accompanied by lactation consultation, were found to improve infants’ latching ability immediately post-treatment. [21]
In this RCT, as well as other studies, such as case reports and case series, the assessment tools for breastfeeding success have been observer-based, conducted by a trained observer such as the lactation consultant. [22] These are not practical for widespread use in private practice, and most of the research done on the use of manual therapy for infants with suboptimal breastfeeding has been done in private chiropractic offices. [20] Therefore, the purpose of this project was to develop a user-friendly and valid outcome assessment instrument for suboptimal breastfeeding that will facilitate data collection on a broader scale.
Methods
This was an observational cohort study conducted in a number of chiropractic clinics in the U.S., using the methods of practice-based research (PBR). [23–25] PBR is a wellestablished method for collecting observational data from multiple clinical practices. [26]
The lead institution’s Institutional Review Board approved the project prior to any data collection. Clinic participation was a sample of convenience. The investigators invited Doctors of Chiropractic (DCs) who they knew had experience in treating infants with suboptimal breastfeeding. Practitioners who agreed to participate were given detailed instructions for their staff to collect data, including administering informed consent to participating mothers and deidentifying all data transmitted to the lead institution’s central office. Data were collected directly from the mothers of the treated infants, and from the treating DCs.
The lead institution’s Institutional Review Board approved the project prior to any data collection.
Eligibility criteria
Inclusion criteria: consecutively presenting mothers of currently breastfeeding infants age ≤ 6 months who bring their infant for care at a participating clinic in the study period.
Exclusion criteria: Mother declines to participate (that is, declines to fill out the forms).
Data collection
The participating offices collected all data on site using paper forms. The mothers completed three of the four forms and the treating clinician completed one form. The office identified each case with a pre-assigned identification number and did not include any personal identifiers. The office staff transmitted the forms electronically (scanned and emailed) to the central office.
Data collection period: One set of data was collected at the time of the infant’s first visit, prior to treatment. The other set was collected one week after the first visit, at a subsequent visit. We chose this interval because, based on the investigators’ clinical experience, some improvement would likely be apparent at one week, and it would be unlikely that the infant would already be discharged at that time. One of the key barriers to collecting follow-up data in PBR is attrition: it is extremely difficult to get complete followup once patients have completed a course of care. [23] Since our purpose was only to test the sensitivity of the instrument to clinical change, and not to evaluate final treatment outcomes, we chose a one-week treatment interval to minimize attrition.
Form administration : At the first visit:
History form completed by the mother: infant age, sex and history of use of lactation consultant, presence of tongue-tie and related medical treatment.
Pre-MIBAQ form (Musculoskeletal Infant Breastfeeding Assessment Questionnaire; see description below) completed by mother.
At visit approximately one week from the first visit:
Post-MIBAQ form completed by mother.
Disposition form completed by treating DC, including
1) number of visits to date;
2) discharge status;
3) treatment procedures used.We left it to the doctors’ interpretation of the techniques they used, so these should not be construed to indicate specific certification or training beyond basic chiropractic scope of practice.
Outcome measures

Table 1 MIBAQ form (Musculoskeletal Infant Breastfeeding Assessment Questionnaire We developed the MIBAQ based on a) relevant questionnaires published in the literature [22, 27–31] and b) the investigators’ clinical experience. [32–34] We identified four domains related directed to the mechanics of nursing (latching, sucking, swallowing, and symmetry) and one global domain. Table 1 lists the domains and associated items.
The MIBAQ consisted of 23 items using a Likert scale of 0–3, where0 = never or seldom;
1 = sometimes;
2 = often;
3 = very often or always.The pre- and post-forms were identical except that the Patient Global Impression of Change was included in the post-MIBAQ. We took a conservative approach to scoring, imputing all missing values as 0, which would indicate that the symptom was never/seldom present.
PGIC (Patient Global Impression of Change) form We included the Patient’s Global Impression of Change (PGIC) scale in the post-assessment as a comparison measure to assess the MIBAQ’s sensitivity to clinical change. The PGIC is a valid and reliable measure of patient-reported clinical change used widely throughout healthcare research and practice due to its simplicity and responsiveness. [35, 36] Furthermore, it is administered at a treatment endpoint only, not at baseline, making it even easier to use. It is suggested that it be combined with domain-specific items as well.
It consists of a 7–item Likert scale, where patients indicates how much their (condition or symptom) has improved since they started treatment, with7 = very much better,
6 = much better,
5 = a little better,
4 = no change,
3 = a little worse,
2 = much worse and
1 = very much worse.We adapted the PGIC for this study to read: Check the box for how your baby’s breastfeeding is now, compared to before treatment at this office.
Data management and analysis
The participating offices transmitted the de-identified forms electronically to the central office. They were keyentered into Excel databases and imported to SPSS (v.26) for cleaning and verification. We computed descriptive statistics for demographic and history variables. We computed total MIBAQ scores by summing all 23 items’ responses; the possible range would be 0–69, with lower scores indicating fewer symptoms of nursing dysfunction. We then compared total pre- and post-MIBAQ scores using a paired t-test. We compared the change score (difference between mean pre- and post-MIBAQ total scores) to the mean PGIC score using a Pearson correlation.
Results
Sample characteristics

Table 2

Table 3

Table 4

Table 5

Table 6

Table 7

Table 8 Ten participating DC offices collected baseline data from 94 mothers. The mean number of participants per office was nine, but the median was six (minimum, 1; maximum 35). Two offices collected the majority of the data (64%). We had demographic data on 93 infants (one form was not completed). Infants’ mean age was 51 days and the median was 40 (range 1–184 days). The infants were fairly evenly divided between boys and girls, with 52% boys. Eighty-three percent (77) of the mothers had consulted a lactation consultant. Of these, 73% were still seeing the lactation consultant; the mean number of visits was three, median two (range 1–22). Seventy-six percent of the infant had a tongue, lip or buccal tie, and of those, 63% had received medical treatment (see Table 2 for details).
Follow-up and treatment
Seventy-six of the 94 participants (81%) completed the oneweek follow-up. Doctors completed 100% of the discharge forms. For the 18 participants who did not do the follow-up, the doctors reported the reasons for dropping out for 17: 10 (59%) did not return for treatment and for seven (41%), the office forgot to give them the form. The number of treatment visits prior to the one-week post-MIBAQ was reported for 77 (82%) of participants. The mean number of visits in the one-week interval was 2.5 (median = 2; range 1–7). Doctors reported that 63% of infants were not discharged at one week, although for 22%, this question was left blank. For the 63% not discharged, the most common reasons given by the doctor were: nursing issues improve but not resolved (66%) and nursing issues resolved but infant needs treatment for other issues (19%). All reasons are listed in Table 3.
The participating DCs reported that cranial (88%) and cervical (78%) were the areas they most commonly treated, follow by thoracic (42%) and lumbar (27%). The most commonly reported manual procedure were craniosacral (82%) and soft tissue (69%). All procedures are listed in Table 4.
Outcomes
The baseline (pre-) MIBAQ scores for all 94 participants are shown in Table 5 (following page). The scores are displayed by the percent of participants responding “never or seldom,” to illustrate which questions were likely to be irrelevant to the outcomes. There were five items for which > 50% of mothers responded “never or seldom.”
Comparison of pre- to post-MIBAQ scores Table 6 (see page 1623) details the scores of the 76 participants who had both pre- and post-MIBAQ scores. There were five items with >50% of participants marking “never or seldom” in the pre-MIBAQ.
The mean total pre-MIBAQ score was 24.5 (possible range of 0–69) and mean total post-MIBAQ score was 17.1. The difference between these (6.4 points) was highly statistically significant (p< .001). Table 7 (following page) presents the details of the comparison.
Correlation of PGIC and MIBAQ The PGIC scores (see Table 8 following page) indicate that 76% of mothers reported improvement in their infant’s breastfeeding in the one-week treatment period. The PGIC score was highly significantly correlated (=.539, p< 0.01) with the change in the MIBAQ scores from pre- to post.
Discussion
The MIBAQ appears to be a feasible instrument to use in chiropractic clinical practice. The participating DCs achieved 100% follow-up with the discharge form, although over 20% did not fill out all the items on the form. For the participating mothers, 81% completed both the pre- and post- form. The doctors identified the reason for incomplete follow up by the participating mothers for 17 of the 18 lost to follow-up: for 59%, it was because she did not return at one week and in 41% of cases, the office forgot to administer the form. This means that the office failed to administer the post-MIBAQ for only 7 of 94 cases, which is a very low failure rate. Similarly, a follow-up rate with the participants of 81% is considered adequate, being high enough to minimize attrition bias. [37]
The MIBAQ also appears to be sensitive to clinical change. Pre- to post-changes were significantly correlated to the PGIC, which is a reliable, valid and clinically sensitive outcome measure. [35, 36] Furthermore, the MIBAQ provides condition-specific detail, while the PGIC is a global measure, and it is recommended that the PGIC be combined with measures for specific factors. [35, 36]
It is likely that the MIBAQ could be streamlined to include fewer questions; in this study, we noted five questions for which > 50% participants marked “never or seldom” at baseline, indicating that the item was either non-relevant, or they didn’t understand what it meant. However, since this study’s sample is not necessarily representative of all chiropractic or other health care providers’ practices, it would take a larger and more representative sample to conduct a factor analysis to consolidate the items in the MIBAQ. A shorter questionnaire that did not lose its clinical sensitivity would be preferable, if possible. Its reliability should also be assessed in future, larger studies. The PGIC, which we used to assess the validity of the MIBAQ, is a general measure which may be helpful to adopt as well.
Limitations
The chief limitation of this study was that our sample was likely not representative of DC practice, since it was a sample of convenience, with two of the doctors contributing 64% of the participants. Even with this limitation, we were able to demonstrate that the MIBAQ is sensitive to patientreported (in this case, proxy-patients) change.
Another limitation, although without bearing on the primary purpose of the study, was the short time frame for followup. We chose it in order to minimize attrition, which was successful. However, it is interesting that over one third (37%) of infants were discharged at one week, and that two thirds (76%) of infants had some degree of improvement within that period of time. Future studies should be planned to follow infants all the way to discharge, to obtain complete information on course of care as well as final outcomes rather than interim outcomes.
A large majority (76%) of mothers in this study reported that their infant had a tongue, lip or buccal tie, and of those, 63% had received medical treatment. Because tongue-tie was not the focus of the study, these data are limited by the lack of more detailed information on this finding and by the fact that the sample size was not large enough to do a subanalysis of infants that had had the procedure compared to those that had not.
The small sample size also precluded subanalyses by other demographics, particularly the infants’ age. Primary breastfeeding issues thus could not be differentiated from those arising after the neonatal period. However, this was not the purpose of this study, and the age range of 0–6 months was adequate for the initial assessment of the MIBAQ instrument.
Conclusion
The Musculoskeletal Infant Breastfeeding Assessment Questionnaire (MIBAQ) is a feasible and clinically responsive patientoriented outcome measure that may be useful as a method to collect outcomes of manual treatment of musculoskeletal dysfunctions in infants with suboptimal breastfeeding. Future studies should employ larger and more representative samples, perhaps of other practitioners as well as chiropractors who care for infants with musculoskeletal factors related to suboptimal breastfeeding.
Acknowledgements
The International Chiropractors Association (ICA) provided partial funding to make this study possible.
We could not have done this study without the DCs and their office staff who generously donated their time and efforts to collect data.
The doctors are: Faraneh Carnegie Hargreaves, DC; Lisa K. Goodman, DC, CCSP, CACCP; Elise G. Hewitt, DC, DICCP; Valerie Lavigne, DC, MSc (coauthor); Natalie Muth, DC; Natalie Pagnani-Gendron, DC; Kelli Patenaude, DC, CACCP; Sarah Radabaugh, DC; Sharon Vallone, DC, FICCP (coauthor); Jennifer Veit, DC, DICCP; Jessie Young, DC (coauthor).
The support staff are: Nikki Burnett, Alyssa Krizek, Susan Lodrioor, Victoria MacKenzie and Christine Muska.
We also thank Texas Chiropractic College students Joanna Caballero and Gemma McDonald for assisting in communicating with the chiropractic offices and for data management.
References:
Bartick MC, Schwarz EB, Green BD, et al.
Suboptimal breastfeeding in the United States:
Maternal and pediatric health outcomes and costs.
Matern Child Nutr. 2017;13(1).AWHONN.
AWHONN Position Statement: Breastfeeding.
Washington DC: AWHONN;2015.USPSTF.
Guide to Clinical Preventive Services.
Washington, DC: Agency for Healthcare Research and Quality (AHRQ); 2014.Global Breastfeeding Collective.
Global Breastfeeding Scorecard, 2017.
Geneva, Switzerland: World Health Organization; 2017.World Health Organization.
Breastfeeding.
Geneva, Switzerland: World Health Organization; 2019.Bartick M, Reinhold A.
The burden of suboptimal breastfeeding in the United States:
a pediatric cost analysis.
Pediatrics. 2010;125(5):e1048-1056.CDC.
Breastfeeding Report Card, United States 2016.
Atlanta, GA: Centers for Disease Control and Prevention;2016.Centers for Disease Control and Prevention.
National Immunization Survey.
National Immunization Survey (NIS) website, accessed August 16, 20182018.U.S. Department of Health and Human Services.
Healthy People 2020. In. 2nd ed.
Washington DC: U.S. Government Printing Office; 2020.Tamura Y, Matsushita S, Shinoda K, Yoshida S.
Development of perioral muscle activity during suckling in infants:
a cross-sectional and follow-up study.
Dev Med Child Neurol. 1998;40(5):344-348.Bu’Lock F, Woolridge MW, Baum JD.
Development of co-ordination of sucking, swallowing and breathing:
ultrasound study of term and preterm infants.
Dev Med Child Neurol. 1990;32(8):669-678.Genna C, Sandora L,.
Normal sucking and swallowing.
In: Genna CW, ed. Supporting Sucking Skills in Breastfeeding Infants.
Burlington MA: Jones and Bartlett; 2017:1-48.Lavigne V.
Lactation consultants’ perceptions of MSK disorders affecting breastfeeding:
cross-sectional survey.
Clin Lactation 2016;7(1):30-36.Marmet C, Shell E.
Therapeutic positioning for breastfeeding.
In: Genna CW, ed. Supporting Sucking Skills in Breastfeeding Infants.
Burlington MA: Jones and Bartlett; 2017 399-416.Coryllos E, Genna CW, Fram JL,.
Minimally invasive treatment for posterior tongue-tie.
In: Genna CW, ed. Supporting Sucking Skills in Breastfeeding Infants.
Burlington MA: Jones and Bartlett; 2017:269-278.Ghaheri BA, Cole M, Fausel SC, Chuop M, Mace JC.
Breastfeeding improvement following tongue-tie and lip-tie release:
A prospective cohort study.
Laryngoscope. 2017;127(5):1217-1223.O’Callahan C, Macary S, Clemente S.
The effects of office-based frenotomy for anterior and
posterior ankyloglossia on breastfeeding.
Int J Pediatr Otorhinolaryngol. 2013;77(5):827-832.Lavigne V.
A narrative review and case report: frenotomy procedure in neonate with tongue-tie.
J Clin Chiropr Pediatr. 2012;13:1025-1031.Guyatt GH, Oxman AD, Vist GE, et al.
GRADE: an emerging consensus on rating quality of evidence
and strength of recommendations.
BMJ. 2008;336(7650):924-926.Hawk C, Minkalis, A Webb, C Hogan O, & Vallone S.
Manual Interventions for Musculoskeletal Factors in Infants
with Suboptimal Breastfeeding: A Scoping Review
J Evidence-Based Integrative Medicine 2018 (Dec 12); 23: 1–12Herzhaft-Le Roy J, Xhignesse M, Gaboury I.
Efficacy of OMT with lactation consultations for
biomechanical sucking difficulties.
J Hum Lact. 2017;33(1):165-172.Sartorio BT, Coca KP, Marcacine KO, Abuchaim ESV, Abrao A.
Breastfeeding assessment instruments and their use
in clinical practice.
Rev Gaucha Enferm. 2017;38(1):e64675.Hawk C, Long CR, Boulanger K.
Development of a practice-based research program.
J Manipulative Physiol Ther. 1998;21(3):149-156.Hawk C, Long C, Boulanger K.
Patient Satisfaction With the Chiropractic Clinical Encounter:
Report From a Practice-based Research Program
J Neuromusculoskeletal System 2001: 9 (4): 109–117Hawk C, Long CR, Boulanger KT.
Prevalence of Nonmusculoskeletal Complaints in Chiropractic Practice:
Report From a Practice-based Research Program
J Manipulative Physiol Ther 2001 (Mar); 24 (3): 157–169Bussieres A, Cote P, French S, et al.
Creating a Chiropractic Practice-Based Research Network (PBRN):
Enhancing the management of musculoskeletal care.
J Can Chiropr Assoc. 2014;58(1):8-15.Miller AS, Huizinga B, Pinkster M, Telford ACJ, ten Heggeler JM, Miller JE.
Development and Testing of a Multidimensional Parent Reported Outcome Measure
for Common Presenting Complaints of Infancy: The UK Infant Questionnaire
J Clinical Chiropractic Pediatrics 2016; 15(3):1292-1300Jensen D, Wallace S, Kelsay P.
LATCH: a breastfeeding charting system and documentation tool.
J Obstet Gynecol Neonatal Nurs. 1994;23(1):27-32.Jensen D, Wallace S, Kelsay P.
A new breastfeeding assessment tool.
J Hum Lact. 1994;10(1):9-10.Matthews MK.
Developing an instrument to assess infant breastfeeding behaviour
in the early neonatal period.
Midwifery. 1988;4(4):154-165.Ingram J, Johnson D, Copeland M, Churchill C, Taylor H.
The development of a new breast feeding assessment tool and
the relationship with breast feeding self-efficacy.
Midwifery. 2015;31(1):132-137.Vallone S.
Chiropractic Evaluation and Treatment of Musculoskeletal Dysfunction
in Infants Demonstrating Difficulty Breastfeeding
J Clinical Chiropractic Pediatrics 2004 (Dec); 6 (1): 349–366Vallone SA, Carnegie-Hargreaves F.
The Infant with Dysfunctional Feeding Patterns –
The Chiropractic Assessment
J Clinical Chiropractic Pediatrics 2016 (May); 15 (2): 1230Vallone S.
Evaluation and Treatment of Breastfeeding Difficulties Associated
with Cervicocranial Dysfunction: A Chiropractic Perspective
J Clinical Chiropractic Pediatrics 2016 (Dec); 15 (3): 1301–1306Rampakakis E, Ste-Marie PA, Sampalis JS, Karellis A, Shir Y, Fitzcharles MA.
Real-life assessment of the validity of patient global impression of change in fibromyalgia.
RMD Open. 2015;1(1):e000146.Scott W, McCracken LM.
Patients’ impression of change following treatment for chronic pain:
global, specific, a single dimension, or many?
J Pain. 2015;16(6):518-526.Babic A, Tokalic R, Amilcar Silva Cunha J, et al.
Assessments of attrition bias in Cochrane systematic reviews are
highly inconsistent and thus hindering trial comparability.
BMC Med Res Methodol. 2019;19(1):76.
Return to PEDIATRICS
Since 2-03-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |