

Exploring Usual Care for Patients with Low Back Pain
in Primary Care: A Cross-sectional Study of
General Practitioners, Physiotherapists
and ChiropractorsThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: BMJ Open 2023 (Aug 30); 13 (8): e071602 ~ FULL TEXT
OPEN ACCESS Simon Dyrløv Madsen • Lars Morsø • Werner Vach • Merethe Kirstine Andersen
Jesper Lykkegaard • Berit Schiøttz-Christensen • Mette Jensen Stochkendahl
Department of Sports Science and Clinical Biomechanics,
University of Southern Denmark,
Odense, Denmark
Objectives: To explore the elements and composition of care provided by general practitioners (GPs), physiotherapists (PTs) and chiropractors (DCs) to patients with low back pain (LBP).
Design: Observational study.
Setting: Primary care setting, Denmark.
Participants: Primary care clinicians (GPs, PTs and DCs) in the Region of Southern Denmark were invited to register consecutive adult patient visits with LBP as the primary complaint.
Primary outcome measures: Clinicians reported care elements provided to patients with LBP. Elements varied due to professional differences (eg, prescriptive rights). Data were descriptively analysed, on group and individual levels, for frequency and combination of care elements, and practice patterns were explored with latent class analysis.
Results: The clinicians (33 GPs, 67 PTs and 43 DCs with a median experience of 15 years and 59% were females) registered 3,500 patient visits. On average, the visits involved patients aged 51 years, and 51% were with females. The frequencies of common care elements across professions were information (42%-56% of visits between professions) and advice (56%-81%), while other common elements for GPs were pain medication (40%) and referrals to PTs (36%), for PTs, use of exercises (81%) and for DCs, use of manual therapy (96%). Substantial variation was observed within professions and distinct practice patterns, with different focuses of attention to information and advice versus exercise and manual therapy, were identified for PTs and DCs.
Conclusions: These data indicate substantial variation in the care elements provided by GPs, PTs and DCs to LBP patients. The compositions of care and practice patterns identified challenge the understanding of usual care as a uniform concept and professions as homogeneous groups. Strategic use of particular care elements in different parts of treatment courses is indicated. Longitudinal data and qualitative enquiry are needed to assess if or how care is tailored to individual patients.
Keywords: Back Pain; Complementary Medicine; Health Services Administration & Management; Musculoskeletal Disorders; Pain Management; Primary Care
From the FULL TEXT Article:
Introduction
Low back pain (LBP) is a global challenge for individuals and healthcare systems due to years lived with disability. [1] It is common across age groups, and over any 2 weeks, almost one in six people in Denmark report very bothersome LBP. [2]
LBP is, in most cases, a non-specific condition3 with a variable course [4, 5] that is dependent on multifactorial biopsychosocial contributors. [6] Consequently, patient-centred approaches to care are generally recommended. [7] In practice, this often entails a combination of different elements of care tailored to the individual patient’s needs. Multiple studies have investigated the care provided to patients with LBP in different primary care settings and provider groups. [8–12] Often, reported results include the frequency of various treatment modalities, medication prescriptions and referrals to advanced diagnostic imaging or specialist care. However, the combination of care elements is rarely under scrutiny. For example, in a study of German physiotherapists (PTs), more than 24 single elements of care were reported. [9] This gives numerous possibilities for combining these elements of care at individual patient visits or over several visits, but little is known about how clinicians combine these different elements or the level of variation within and across provider groups.
In Denmark, most patients with LBP seek care from general practitioners (GPs), PTs and chiropractors (DCs). All are subject to the Danish clinical practice guidelines for non-surgical management of LBP and lumbar radiculopathy, recommending patient education, supervised exercise and manual therapy, and discouraging pharmacological treatment and routine use of diagnostic imaging and acupuncture. [13] These recommendations are largely concordant with international clinical practice guidelines, although there is some variation regarding pharmacological treatment. [14]
In many clinical practice guidelines (Danish and international), recommendations are based on interventions compared with usual care. [14] However, with the numerous potential combinations of care, the composition of usual care for LBP is often not well conceptualised or universally defined. [15] Further, recommended elements of care may be combined with non-recommended elements. A Canadian study of a chiropractic teaching clinic showed that most treatment plans for LBP patients included guideline-concordant care (eg, patient education, exercise and spinal manipulation/mobilisation) but also often non-recommended care like manual therapy as mono-therapy. [16] This monodisciplinary example indicates that both recommended and non-recommended elements of care may be provided concomitantly. Still, it does not provide insights into the most frequent combinations of care offered to patients with LBP or whether the findings are generalisable to other primary healthcare provider groups that care for LBP patients.
The overall aim of this study was to explore the composition of care provided by GPs, PTs and DCs to patients with LBP. As the composition of care may vary over a treatment course, we focused on a rather well-defined part of the course, namely the initiation and early implementation.
Specifically, we pursued the following:
Within each professional group, we described the frequency of 21 elements of care provided from the first to the sixth visit.
We compared the frequency of the most common elements of care across clinicians within each professional group.
We studied the combination of care elements at single visits and compared this across the professional groups and clinicians within each group.
We characterised clinicians within professions by profiles defined by the frequency of specific care elements across all visits and identified practice patterns for these groups of clinicians.
Methods
A cross-sectional observational study design was used to explore practice patterns.
Setting
The Danish healthcare system is tax funded and provides free access to GPs who serve as gatekeepers and have referral rights to diagnostic imaging and specialised care. PTs and DCs can be accessed directly without a referral from GPs but at a fee for service. Partial reimbursement (approximately 40%) is granted to PT patients who have a formal referral from a GP and to all DC patients regardless of referral (about 20%). PTs do not have official referral rights but can recommend referrals (eg, to advanced imaging) through written, electronic communication with GPs. DCs have referral rights to advanced imaging and secondary spine care, and the majority have in-house radiography equipment.
Participants
All GPs (936 GPs) and clinics with PTs (103 clinics with 734 PTs) and DCs (69 clinics with approximately 193 DCs) working in primary care and registered under the National Health Insurance in the administrative Region of Southern Denmark, covering approximately 1.2 million inhabitants, were invited through postal mail to participate in a prospective survey registration of consecutive visits with adult patients (age >16) with LBP as their primary complaint.
Survey
In brief, participating clinicians were asked to register all visits regarding LBP on paper charts in anonymised format, including data on patient and management characteristics. The participants manually ticked off a one-page paper registration chart with 45–47 variables after every visit ( see online supplemental file 1 for an English version of the GP registration chart). The number of variables varied between professions due to differences in treatment modalities, medication prescription and referral rights. Collected variables included clinician characteristics (profession, sex and years of experience), patient characteristics (age in years, sex, factors associated with poor prognosis and clinical findings) and visit number (defined as the number of visits the patient had had before in the current visit in this episode of LBP). Variables relating to poor prognosis and clinical findings were predefined, and their presence were indicated by the participant ticking off the variable on the paper chart. To guide the participants in filling in the chart, they were provided with an overview of easy-to-read definitions of each variable, and the requested minimum and maximum number of ticks in each domain. Extracts of patient characteristics are presented in the Results section, while full details are presented elsewhere. [17] Before release, the registration charts were pilot tested by three to five clinicians from each of the three professions resulting in minor revisions. We followed the procedures of Audit Projekt Odense (APO), [18] which have previously been shown to be a viable method for extensive data collections in primary care.
The outcomes were particular elements of care selected from the Danish clinical practice guidelines for non-surgical management of recent-onset LBP and lumbar radiculopathy [13] and common elements of care based on consensus in the multidisciplinary working group who discussed the registration charts before the study. The care elements were in the chart domain, Actions today, organised according to outcome category: information (information about LBP including prognosis), advice (advice on self-management), exercise (exercise instructions, directional exercise or active exercise), manual therapy, acupuncture (acupuncture/dry needling), pain medication (non-steroidal anti-inflammatory drug (NSAID), adjuvant analgesics (gabapentin/Lyrica/tricyclic antidepressants) or opioids), referrals (referrals to, or recommendations of, GPs, PTs, DCs or the secondary care spine centre), imaging (MRI and X-ray), discussion of lifestyle factors (PTs) and discussion of pain medication (DCs). Information, advice and manual therapy were available for all professions.
Data collection and management
Data were collected within a period from October to December 2019, which ran for 2 weeks for PTs and DCs, and 4 weeks for GPs, in order to match the expected daily volume of patients with LBP in each profession. The clinicians were instructed to register consecutive visits and fill in the registration chart during, or immediately after, every patient visit with LBP as the primary complaint. After the data collection, data (check marks and numbers) were entered manually in a Pascal programme independently by two data managers (research assistants with extensive familiarity and experience in the method) and checked for consistency by a third member from the research team.
Statistical analysis
To investigate recently initiated treatment courses, we included only data from the first to the sixth visits. This cut point also aligned with the national mean number of visits to Danish chiropractors, which is six visits. [19] In addition, we partially investigated the care elements in relation to the visit number in order to check whether this period was sufficiently homogeneous. The denominator of this study was patient visits. As visits were registered consecutively without patient identifiers, patients may have been registered more than once. Visits with missing information about the provided care elements were excluded. No imputation was performed.
Descriptive analyses of patients’ characteristics at visits and clinicians’ characteristics were reported as counts and percentages for binary variables and mean (SD) or median (IQR) for continuous variables.
To describe the GPs’ total prescription of pain medication, we created the variable ‘pain medication’ by combining the three variables relating to GPs’ prescription of NSAIDs, adjuvants and opioids. Further, GPs referrals were merged into ‘referrals to PTs/DCs’, ‘referrals to secondary care’ (MRI, emergency room or the spine centre) and ‘referrals to PT/DC or secondary care’ to illustrate broader elements of care. Exercise instructions were available for GPs and DCs but not for PTs. For ease of comparison between the professions, we created a variable, ‘exercise instructions’, by combining PTs’ two variables (directional exercise and active exercise).
At the professional level, visit number distribution, the number of single elements of care per total number of visits were reported as counts and percentages. The frequency of single elements of care by visit number and the distribution of the frequency of the four shared care elements across clinicians were illustrated graphically.
With respect to the variation across the individual clinicians, we generated a variety of figures depicting certain aspects of the use of care elements for each clinician. Clinicians with very few visits would disturb the visual impression of the variation, as the distribution of care elements within such clinicians would mainly reflect random noise. Hence, clinicians with less than five visits were excluded from individual clinician-level analyses.
The variation in the single elements of care at the individual clinician level was presented graphically by plotting the sorted frequency of single care elements per total number of visits with 95% CIs for each clinician.
The number of care elements combined at each visit was reported as medians and IQR and presented graphically. The frequency of individual clinicians’ combination of care elements is illustrated as stacked bar charts based on the most frequent combinations observed. The frequencies of using specific care elements across all visits were used to define a profile for each clinician. These profiles are presented graphically in bar charts. For both types of bar charts, the clinicians were sorted by the first dimension of a multidimensional scaling applied to the clinicians’ frequencies of all care elements in order to ensure that clinicians with similar patterns appear close together. The clinicians were numbered consecutively within each profession.
To explore if distinct practice patterns (ie, groups of clinicians with similar combinations of care elements within the professions) could be identified, latent class analysis (LCA) was carried out for PTs and DCs. Due to the participating GPs’ low registration of visits, we could not perform the LCA on the GP data. We limited the analysis of PTs and DCs to the four most frequent elements of care (information, advice, exercise and manual therapy) shared between the two professions. For each profession, we ran the generalised structural equation modelling for two latent classes using the option of randomly predicted start values (five draws). We repeated this for three and four classes, and the final number of classes was chosen based on (1) clinical relevance with distinctive features, (2) class sizes and (3) within-class variation. Data were analysed in Stata V.17, StataCorp.
Patient and public involvement
To ensure reflection of everyday clinical practice, stakeholder representatives (clinicians and researchers with current or previous clinical experience) from GPs, PTs and DCs participated in a multidisciplinary working group that developed the survey chart. The working group was formed based on expression of interest at an annual meeting under the auspice of the Odense APO group, where clinicians from the three primary care professions in the Region of Southern Denmark were openly invited to participate. No patients were involved in the project.
Results
Clinician characteristics

Table 1

Table 2

Table 3

Table 4
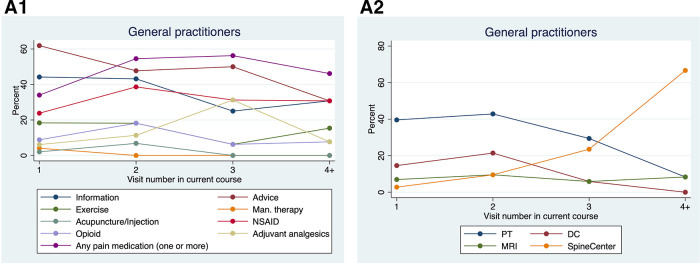
Figure 1
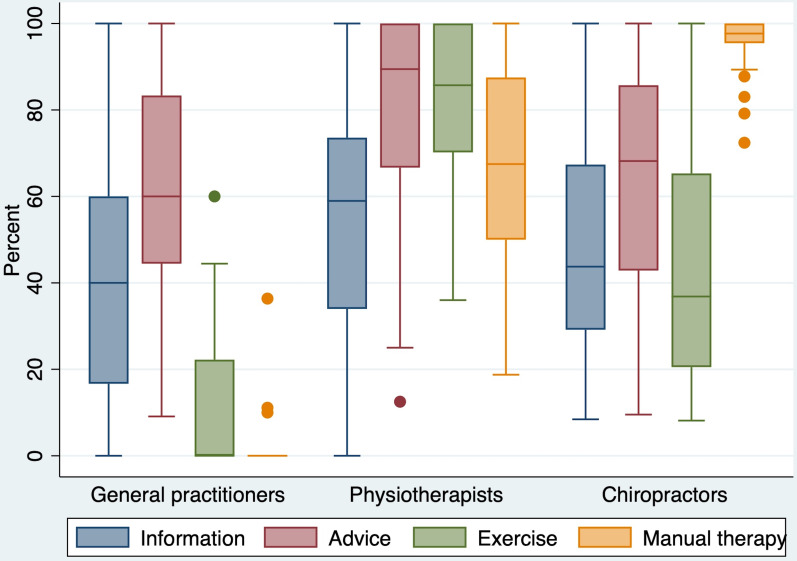
Figure 2
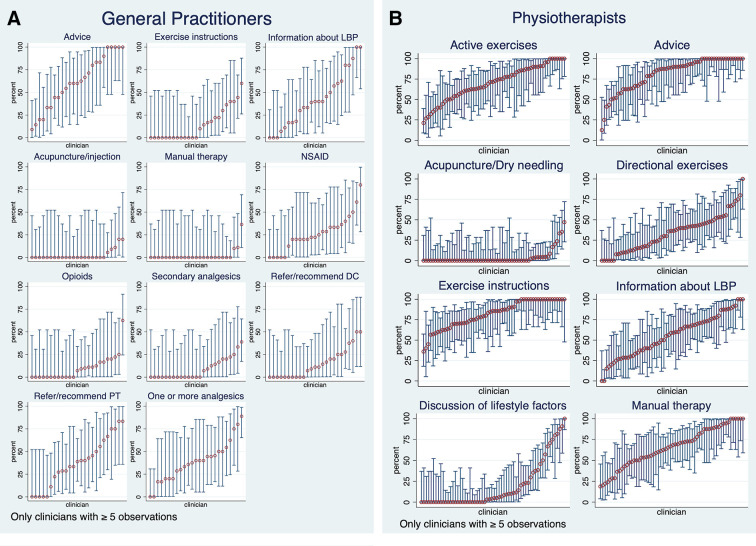
Figure 3 A total of 143 clinicians (33 GPs, 67 PTs and 43 DCs with a 4%, 9% and 22% participation rate, respectively) collected data from 4,791 LBP visits. After excluding 1,280 visits beyond the 6th visit and 11 visits with missing data on the care elements provided, GPs collected information from n=220 visits, PTs from n=1,068 visits and DCs from n=2,212 visits. Ultimately, data on 3,500 visits from recently initiated treatment courses were analysed. Clinicians had a median experience of 15 years (IQR 5–23), and 59% were females (see Table 1).
Visit characteristics
On average, the visits were with a patient aged 51 years, 51% with a female, and 62% and 17% with a patient having had several previous disabling episodes of LBP and back-related leg pain below the knee, respectively (see Table 2). GPs had significantly more first-time visits and fewer later (third to sixth) visits compared with PTs and DCs (the distribution of visit numbers is presented in Table 3).
Frequency of care elements at the profession level
Table 4 shows the frequency of care elements for each profession. The most frequent elements of care were information (GPs (42%), PTs (56%), DCs (49%)) and advice (GPs (56%), PTs (81%) and DCs (66%)). GPs provided pain medication in 40% of visits and referred to PTs or DCs in almost half of the visits (47%); PTs gave exercise instructions in 81% of visits and provided manual therapy in 65% of visits; DCs provided manual therapy in almost every visit (96%) and exercise instructions in 45%.
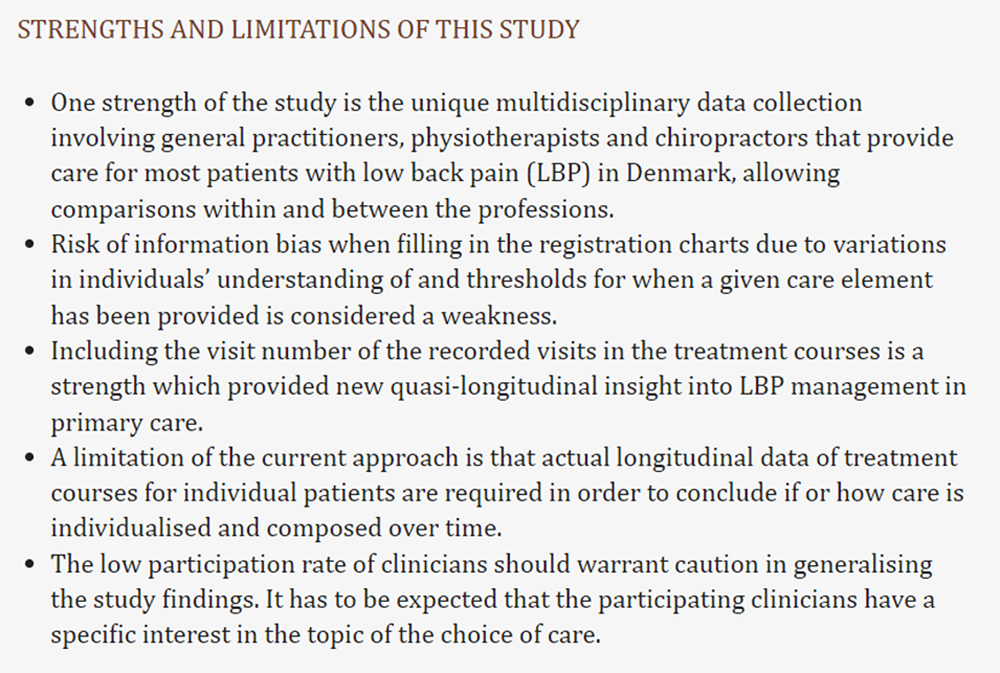
The frequencies of some care elements varied with visit number, as depicted in Figure 1A–C. Generally, giving information and advice happened more frequently in the initial two visits, whereas many elements of care were provided with a somewhat constant frequency. GPs most often referred to PTs and DCs in the first two visits, MRI referrals were relatively stable, whereas referrals to the spine centre in secondary care were more frequent in later visits.
When comparing the four single elements of care used in all three professions (information, advice, exercise and manual therapy, Figure 2), we observed some variation in their use. Common for all three professions, we observed wide-ranging IQRs indicating considerable variation in using single care elements within each profession.
Frequency of care elements at the clinician level
Due to having registered less than 5 visits, 8 GPs (24% of GPs) with 22 visits (10% of GP visits) and 7 PTs (10% of PTs) with 19 visits (2% of PT visits) were excluded from individual clinician-level analyses. The excluded clinicians were comparable to the included with respect to age, sex, experience and provided care elements (data not shown). The frequency of the outcomes varied between clinicians. Figure 3A–C depict these distributions for all single care elements. Information and advice were provided by nearly all clinicians (more than 88% and 100%, respectively) in at least one visit (figure 3A–C), whereas some care elements were rare and hardly provided at any visits (eg, GPs providing manual therapy or PTs providing acupuncture).
Most GPs prescribed pain medication, most commonly NSAIDs, but one in five did not prescribe NSAIDs at any visits (figure 3A). In contrast, other GPs prescribed pain medication in more than four out of five visits. A similar pattern could be observed for primary care referrals with a large difference between GPs with frequent and infrequent use (figure 3A).
Advice and exercise were used in all visits by approximately one-third of the PTs but in less than half of the visits for others (figure 3B). More than one-third of DCs provided manual therapy in every visit, while only a handful of clinicians provided it in less than 90% of visits (figure 3C). Exercise instructions were provided by all DCs, but the frequency varied between use in 8%–100% of visits for DCs with a median frequency of 37%. Some care elements had lower frequencies such as acupuncture for PTs and DCs (table 3), but while three out of four PTs and half the DCs did not use acupuncture at any point, some used it in more than half of the visits (figure 3B,C).
Combinations of care elements at single visits
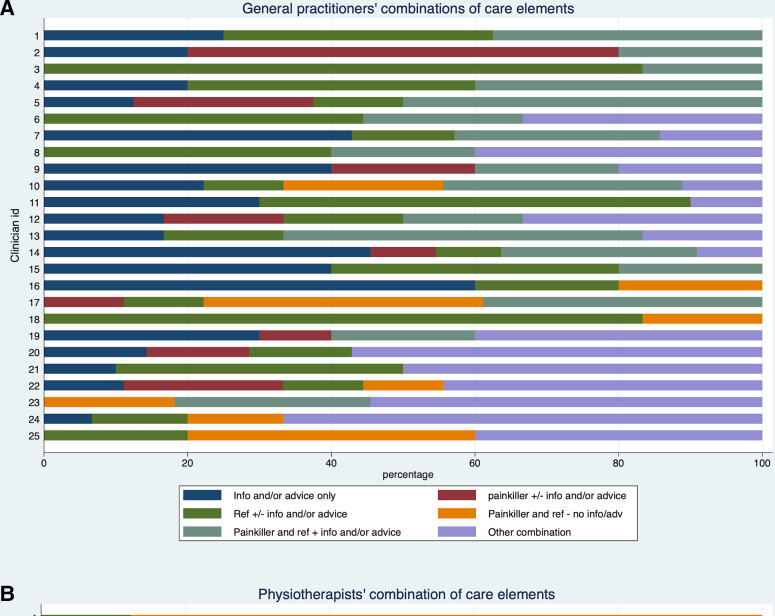
Figure 4
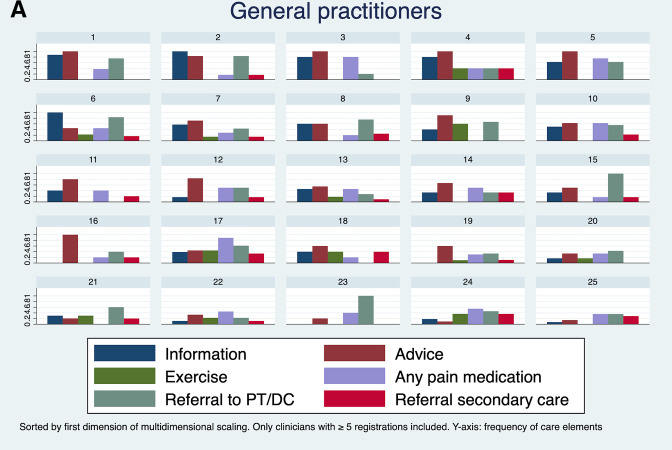
Figure 5
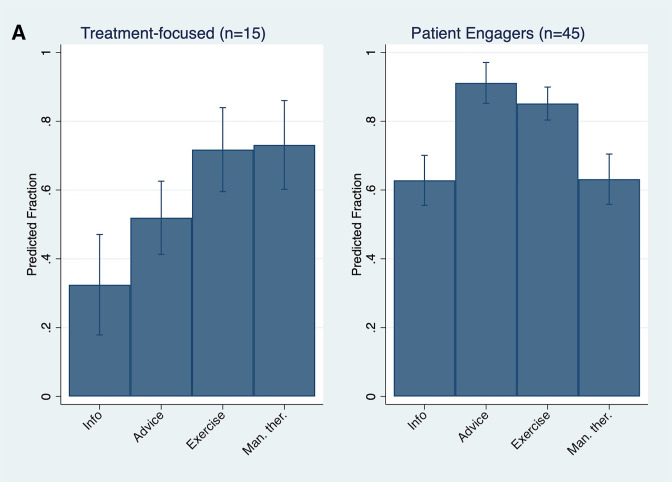
Figure 6 The median number of care elements per visit was two for GPs, and three for PTs and DCs (see online supplemental file 2). Figure 4A–4C depicts the variation in the frequency specific combinations across the clinicians. The figures illustrate a large variation among clinicians where some tend to use one (or two) specific combinations of care elements in most visits, while others mixed different combinations of care more frequently. Figure 4C of DCs illustrates this point. We observe a pattern with a fraction of the clinicians using manual therapy only, while others combine manual therapy with information, advice and exercise, and some alternate combinations more often.
Frequency profiles of clinicians
Each clinician can be characterised by a profile defined by the frequencies of using specific elements of care across all visits. These profiles are shown in Figure 5A–C. In these graphs, the clinicians are already ordered by grouping clinicians with similar profiles side by side. This way, it becomes visible that there are subgroups of clinicians with similar profiles, but across the groups, there are distinct differences in the profiles.
Latent class analysis
When exploring groups using similar combinations of care, LCA resulted in two practice patterns for PTs, and three practice patterns for DCs, as shown in Figure 6A,B. For both PTs and DCs, the addition of another practice pattern resulted in a small class including only four clinicians. The third practice pattern for PTs, to some extent, added another distinct practice pattern, but with small class size and large within-group variation. For the DCs, the fourth practice pattern had a small class size and lacked clinical distinctiveness. Therefore, the analyses’ endpoints were two PT and three DC practice patterns.
PT practice patterns
The first PT practice pattern consisted of 15 PTs (25%) who were characterised by often providing exercise instructions and manual therapy accompanied by no or little to medium information and advice (named ‘treatment focused’). The second practice pattern (named ‘patient engagers’) consisted of 45 PTs (75%) who were characterised by often providing exercise and advice, a higher provision of information but lower use of manual therapy compared with the treatment-focused group, and additionally, discussed lifestyle factors in a higher proportion of visits (26% vs 8% of visits).
DC practice patterns
DCs, in all three practice patterns, provided manual therapy at almost every visit. The practice patterns were distinguished based on the use of information, advice and exercises with a pattern of increasing use from the ‘DC low’ group (17 DCs (39%)), to the ‘DC medium’ (14 DCs (33%)) and ‘DC high’ (12 DCs (28%)). Additionally, clinicians in the DC practice patterns had different features in additional elements of care provided; clinicians in the DC low and DC medium groups more often used acupuncture/dry needling than DC high (12% and 11% vs 5% of visits), and less frequently discussed pain medication with patients (6% and 12% vs 22% of visits).
Discussion
Based on 3,500 LBP visits, this study explored the composition of care elements provided to patients with LBP by GPs, PTs and DCs. At first glance, the three professions provided elements of care well aligned with the traditional professional roles; GPs prescribed pain medication and referred to PTs, PTs provided exercise instructions and DCs, manual therapy. However, closer inspections revealed large variations in the frequency of several care elements within and between the professions. These findings challenge both the stereotypical images of the clinicians and usual care as a uniform concept within groups of clinicians. By exploring the combinations of particular care elements, we have illustrated some of the most frequent combinations and the large variation among individual clinicians, thereby demonstrating the heterogenic composition of care provided to patients with LBP.
This study shows that clinicians have large variations in LBP management, combine elements of care differently and have distinct practice patterns. GPs’ elements of care could not be explored to the same extent as the PTs and DCs due to fewer registrations for each GP, but our results indicate substantial variation among GPs as well as among PTs and DCs. Our LCA seemed to uncover certain patterns. For example, some clinicians tend to use verbal elements of care throughout the treatment course while others, such as treatment-focused PTs and DC low, use them less frequently. This could indicate that some clinicians generally prioritised dialogue and interaction with the patient as an important care element as opposed to others with an affinity for ‘hands-on’ or more tangible or physical management. Previous studies have identified that some PTs [20] and DCs [21] experience difficulties when managing the psychosocial needs of their patients. Our findings indicate that at least some clinicians engage in dialogue with their patients, and thus potentially open the opportunity for addressing these patient circumstances.
Clinical practice guidelines from Denmark [22] and internationally [13] stipulate that information about the diagnosis and prognosis of LBP must be provided to all patients with LBP. In our other study on these data, information was only provided in 44% (GPs) to 76% (DCs) of first-time visits. [23] Underuse of patient education has previously been reported for primary care clinicians, [24–26] but this study adds to the knowledge about (lack of) provision of patient education by describing the frequency beyond the first consultation and by showing the substantial variation intraprofessionally including the substitutes of care elements between clinicians. Whether the content of information and advice given were in line with best evidence and LBP clinical practice guidelines is unknown, but differences in the frequencies at which clinicians register to provide information and advice are obvious. Another study shows that Danish PTs often informed about the benign nature of LBP but were hesitant to advise on return to normal activity and work, while they provided advice on posture and ergonomics which is not recommended. [26] This example, along with several others, [16, 27] illustrates the eclectic composition of recommended and non-recommended care across primary care.
The variation seen in the elements of care may be partly explained by variations in patient characteristics. A previous study demonstrated that patients with LBP in Danish general practice are significantly more severely affected in terms of pain intensity, disability and sick leave compared with patients with LBP in chiropractic practice. These differences may partially explain interprofessional differences, but probably offer little explanation of the major intraprofessional differences in the practice profiles. Whether differences in the combination of specific care elements reflect a tailoring of care to patient characteristics should be examined in future research. Further, investigations of private health insurances and other financial incentives, healthcare cultures, and individual factors in both patients and clinicians (eg, personal beliefs and preferences), may contribute to a fuller understanding of the complex interplay of system, setting, provider and patient-level factors that may influence care delivery. [28, 29]
The GPs were the only profession allowed to prescribe pain medication. Compared with a similar study conducted in 2011, [30] the prescription of NSAIDs has decreased from 52% to 28%, and the number of visits resulting in any prescription of pain medication decreased from 82% to 40%, which is a positive trend considering current clinical practice guidelines. However, in the 2011 study, the most frequently prescribed medication was weak analgesics such as paracetamol (66% of visits). Thus, the total use of pain medication in our study is likely underestimated, as weak and non-prescriptive pain medication was not included in the registration chart.
Strengths and weaknesses
We used a well-established method with thoroughly tested procedures, including detailed written instructions, for the data collection, with which the GPs were especially familiar, and the quick manual registration chart of care elements in proximity to the patient visit in order to limit recall bias. Whether the clinicians included all eligible patients is unknown.
The data collection resulted in a large dataset by the three major professions providing care for patients with LBP in Denmark. All clinicians from the three professions in the Region of Southern Denmark were invited, but clinicians were self-selected, and we do not know whether participants were representative of the entire clinician populations. Our study found considerable variation in care among the clinicians in our sample, indicating that this variation is likely to be present in a representative population as well. However, a larger and confirmed representative sample would enable us to further examine and strengthen our estimates of the frequencies and variation of care elements. With the observed considerable variation of care provided, we believe this issue is of limited consequence to our results. However, it has to be expected that the clinicians have a particular interest in the topic which, combined with a relatively low participation rate, calls for caution in generalising the study findings.
Elements of care were based on the Danish guideline recommendations combined with strong multidisciplinary stakeholder involvement in developing and refining procedures to ensure compatibility with common practice. However, we were forced to rely on self-assessment and self-reporting, which can lead to bias. We included both recommended and non-recommended elements of care, and we cannot exclude the possibility that some clinicians preferred to provide socially acceptable answers. Also, despite detailed definitions of care elements, clinicians may have had different thresholds for when they perceived a particular element was provided. Other care elements may have been provided but not included in the survey. Furthermore, given that an element with the same label was provided does not mean that the care delivered was comparable. For example, the information and advice given may not necessarily have been in concordance with recommendations from clinical practice guidelines, and manual therapy covers a wide range of treatment techniques.
The survey method focused on care at the visit level rather than at the individual patient level. Thus, we cannot describe specific treatment courses of individual patients over time. Performing the same type of analyses at the patient level will probably paint a different picture, as there can be (meaningful) variation from visit to visit within the treatment course of a single patient. The change in the frequency of certain care elements over time indicates such meaningful variation. However, additional sources for meaningful variation could be avoiding overload at single visits or exact repetition. Full quantification and understanding of variation in care across clinicians and the degree to which care is modified for individual patients would require access to individual patients’ longitudinal data over complete treatment courses, allowing for reconstructing the chosen care strategy for each patient. Further, adopting a whole-system perspective and multilevel data collection would allow for a more nuanced analysis of this complex and dynamic phenomenon.
Assessments of a profession’s adherence to clinical guidelines are typically based on the group mean and proportions of the professionals adhering to single items or domains. [24, 26, 27] However, qualitative studies have identified different barriers to guideline adherence for LBP management. These include clinicians’ beliefs that guidelines limit clinician autonomy, everyday implementation is impractical, and clinical experience and judgement supersede guidelines. [31] Our study supplements the results of the qualitative studies. It suggests that designing guideline implementation initiatives assuming clinicians are one homogeneous group would likely lead to unsuccessful results. To improve guideline adherence in implementation efforts, more individualised, clinician-centred approaches may help identify non-compliant clinician groups or groups with a substandard provision of care, so resources can be guided towards where maximum potential impact can be achieved.
Future studies, particularly qualitative enquiries, may help shed light on the concept of usual care: how clinicians choose their management strategies, how it develops over a treatment course and what factors influence the choice of management as well as the context and circumstances different clinicians work under that may affect care.
Conclusion
The study points to a substantial variation in elements of care provided by GPs, PTs and DCs to patients with LBP. We provide some evidence that indicates differences in practice patterns between clinicians within and across professions that challenge the stereotypical images of clinicians and usual care as a uniform concept within groups of clinicians. Longitudinal data and qualitative enquiry are needed to assess if or how care is tailored to individual patients.
Supplementary Material
Reviewer comments (322K, pdf)
Author's manuscript (87M, pdf)Acknowledgements
We thank Susanne Døssing Berntsen, Audit Project Odense, for handling and mailing the registration charts to the participants. We would also like to acknowledge the work done by the primary care consultants to enrol clinicians in the study and to thank the clinicians for their contribution. Safe storage and analyses were carried out in OPEN Analyse, OPEN, Open Patient data Explorative Network, Odense University Hospital, Region of Southern Denmark.
Contributors:
SDM is responsible for the overall content as the guarantor of this study. SDM, LM, MKA, JL, BS-C and MJS contributed to the concept development and design. WV, LM and MJS supervised SDM in the analysis and writing of the first draft of the manuscript, and all authors critically reviewed, approved and agreed to the accountability of the final manuscript.
Funding:
The data collection was funded by the Association of Danish Physiotherapists foundation for clinical practice (grant number A2951), the Foundation for Promotion of Chiropractic Research and Postgraduate Education (grant number R126-A2763), and the General Practitioners’ Quality and Postgraduate Foundation in the Region of Southern Denmark (grant number 07/18). The first author was funded by the Foundation for Promotion of Chiropractic Research and Postgraduate Education (grant number R126-A2638) and IMK Foundation (grant number N/A). The funders did not have any influence on the study design, data collection, management, analysis, interpretation or publication of results.
Ethics approval
This study involves human participants but according to Danish legislation, surveys are not considered health science research notifiable to the Research Ethics Committee System, c.f. Committee Act Art. 14, paragraph 1. By Danish legislation, the authorised legal department at the University of Southern Denmark approved the study (ID #11.226). Participants gave informed consent to participate in the study before taking part.
References:
Wu A., March L., Zheng X., Huang J., Wang X., Zhao J., et al.
Global Low Back Pain Prevalence and Years Lived with
the Global Burden of Disease Study 2017
Annals of Translational Medicine 2020 (Mar); 8 (6): 299Jensen HAR, Davidsen M, Ekholm O, et al..
Danskernes Sundhed – Den Nationale Sundhedsprofil 2017.
København: Statens Institut for Folkesundhed, Sundhedsstyrelsen, 2018.Henschke N, Maher CG, Refshauge KM, et al..
Prevalence of and screening for serious spinal pathology in patients
presenting to primary care settings with acute low back pain.
Arthritis Rheum 2009;60:3072–80.
10.1002/art.24853Dunn KM, Hestbaek L, Cassidy JD.
Low Back Pain Across the Life Course
Best Pract Res Clin Rheumatol 2013 (Oct); 27 (5): 591-600Kongsted A, Kent P, Axen I, Downie AS, Dunn KM.
What Have We Learned From Ten Years of
Trajectory Research in Low Back Pain?
BMC Musculoskelet Disord. 2016 (May 21); 17 (1): 220Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, Hoy D, Karppinen J et al.
What Low Back Pain Is and Why We Need to Pay Attention
Lancet. 2018 (Jun 9); 391 (10137): 2356–2367
This is the second of 4 articles in the remarkable Lancet Series on Low Back PainFoster NE, Anema JR, Cherkin D, Chou R, Cohen SP, et al.
Prevention and Treatment of Low Back Pain:
Evidence, Challenges, and Promising Directions
Lancet. 2018 (Jun 9); 391 (10137): 2368–2383
This is the third of 4 articles in the remarkable Lancet Series on Low Back PainKamper SJ, Logan G, Copsey B, et –al.
What is Usual Care for Low Back Pain? A Systematic Review of
Health Care Provided to Patients with Low Back Pain in
Family Practice and Emergency Departments
Pain. 2020 (Apr); 161 (4): 694–702Bahns C, Happe L, Thiel C, et al..
Physical therapy for patients with low back pain in Germany:
a survey of current practice.
BMC Musculoskelet Disord 2021;22:563.
10.1186/s12891-021-04422-2Beliveau PJH, Wong JJ, Sutton DA, Simon NB, Bussieres AE, Mior SA, et al.
The Chiropractic Profession: A Scoping Review of Utilization Rates,
Reasons for Seeking Care, Patient Profiles,
and Care Provided
Chiropractic & Manual Therapies 2017 (Nov 22); 25: 35Mior S, Wong J, Sutton D, Beliveau PJ, Bussières A, Hogg-Johnson S, French S.
Understanding patient profiles and characteristics of current chiropractic practice:
a cross-sectional Ontario Chiropractic Observation and Analysis STudy (O-COAST)
BMJ Open 2019 (Aug 26); 9 (8): e029851French SD, Charity MJ, Forsdike K, et al..
Chiropractic observation and analysis study (COAST):
providing an understanding of current Chiropractic practice.
Med J Aust 2013;199:687–91.
10.5694/mja12.11851Stochkendahl MJ, Kjaer P, Hartvigsen J et al.
National Clinical Guidelines for Non-surgical Treatment of Patients
with Recent Onset Low Back Pain or Lumbar Radiculopathy
European Spine Journal 2018 (Jan); 27 (1): 60–75Corp N, Mansell G, Stynes S, et al..
Evidence-based treatment recommendations for neck and low back pain
across Europe: A systematic review of guidelines
European J Pain 2021 (Feb); 25 (2): 275–295Somerville S, Hay E, Lewis M, et al..
Content and outcome of usual primary care for back pain:
a systematic review
Br J Gen Pract 2008 (Nov); 58 (556): 790-797Csiernik B, Smith A, Plener J, et al..
Intervention usage for the management of low back pain in
a Chiropractic teaching clinic.
Chiropr Man Therap 2022;30:3.
10.1186/s12998-022-00412-wLykkegaard J, Christensen BS, Hansen A, et al..
Management of patients with low back pain in the region of Southern Denmark
(in Danish: Håndtering Af Patienter MED Lænderygsmerter I region Syddanmark)
[Audit Projekt Odense]. 2019. Available:
https://www.apo-danmark.dk/_files/ugd/43637f_
0f297d0cab604350a72223116a79a2d9.pdf
[Accessed 22 Aug 2023].Hansen MP, Lykkegaard J, Søndergaard J, et al.
How to improve practice by means of the Audit Project Odense method
Br J Gen Pract 2022 (Apr 28); 72 (718): 235-236Kiropraktorer I Dagens Danmark. 2021. Available:
https://www.danskkiropraktorforening.dk/media/2435/om-kiropraktorer
-til-sundhedsuddannede-dkf-september-2021.pdf
[Accessed 22 Aug 2023].Synnott A, O’Keeffe M, Bunzli S, et al..
Physiotherapists may Stigmatise or feel unprepared to treat people
with low back pain and Psychosocial factors that influence recovery:
a systematic review.
J Physiother 2015;61:68–76.
10.1016/j.jphys.2015.02.016Stilwell P, Hayden JA, Des Rosiers P, et al..
A qualitative study of doctors of Chiropractic in a Nova Scotian practice-based
research network: barriers and Facilitators to the screening and management
of Psychosocial factors for patients with low back pain.
J Manipulative Physiol Ther 2018;41:25–33.
10.1016/j.jmpt.2017.07.014Lin I, Wiles L, Waller R, Goucke R, Nagree Y, Gibberd M, et al.
What Does Best Practice Care for Musculoskeletal Pain Look Like?
Eleven Consistent Recommendations From High-quality
Clinical Practice Guidelines: Systematic Review
British J Sports Medicine 2020 (Jan); 54 (2): 79–86Morsø L, Lykkegaard J, Andersen MK, et al.
Providing Information at the Initial Consultation to Patients with Low Back
Pain Across General Practice, Chiropractic and Physiotherapy -
A Cross-Sectorial Study of Danish Primary Care
Scand J Prim Health Care 2022 (Oct 31); 1–9Di Iorio D, Henley E, Doughty A.
A survey of primary care physician practice patterns
and adherence to acute low back problem guidelines.
Arch Fam Med 2000;9:1015–21.
10.1001/archfami.9.10.1015Williams CM, Maher CG, Hancock MJ et al.
Low Back Pain and Best Practice Care:
A Survey of General Practice Physicians
Archives of Internal Medicine 2010 (Feb 8); 170 (3): 271–277Husted M, Rossen CB, Jensen TS, et al..
Adherence to key domains in low back pain guidelines:
A cross-sectional study of Danish Physiotherapists.
Physiother Res Int 2020;25:e1858.
10.1002/pri.1858Amorin-Woods LG, Beck RW, Parkin-Smith GF, Lougheed J, Bremner AP.
Adherence to Clinical Practice Guidelines Among Three Primary
Contact Professions: A Best Evidence Synthesis of the Literature
for the Management of Acute and Subacute Low Back Pain
J Can Chiropr Assoc 2014 (Sept); 58(3): 220–237Atsma F, Elwyn G, Westert G.
Understanding unwarranted variation in clinical practice:
a focus on network effects, reflective medicine
and learning health systems.
Int J Qual Health Care 2020;32:271–4.
10.1093/intqhc/mzaa023Landon SN, Padikkala J, Horwitz LI.
Identifying drivers of health care value:
a Scoping review of the literature.
BMC Health Serv Res 2022;22:845.
10.1186/s12913-022-08225-6Poulsen L, Munck A.
Low back pain from initial contact with Healthcare to completed treatment
(in Danish: Lændesmerter Fra Primær Kontakt MED Sundhedsvæsnet til
Færdigbehandlet) [Audit Projekt Odense]. 2011. Available:
https://www.apo-danmark.dk/_files/ugd/43637f_f3819c11a7084
7419bb043b1ecadc81d.pdf
[Accessed 20 Dec 2022].Slade SC, Kent P, Patel S, et al..
Barriers to primary care clinician adherence to clinical guidelines
for the management of low back pain: A systematic review
and Metasynthesis of qualitative studies.
Clin J Pain 2016;32:800–16.
10.1097/AJP.0000000000000324
Return to WHAT IS USUAL CARE?
Return to INITIAL PROVIDER/FIRST CONTACT
Since 9-20-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |