

The Chiropractic Subluxation: Medical Evidence
in Support of the Subluxation ConstructThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Asia Pacific Chiropractic Journal 2023; 3.3 ~ FULL TEXT
OPEN ACCESS Peter Rome, DC, FICC and John D Waterhouse, DC, FACC
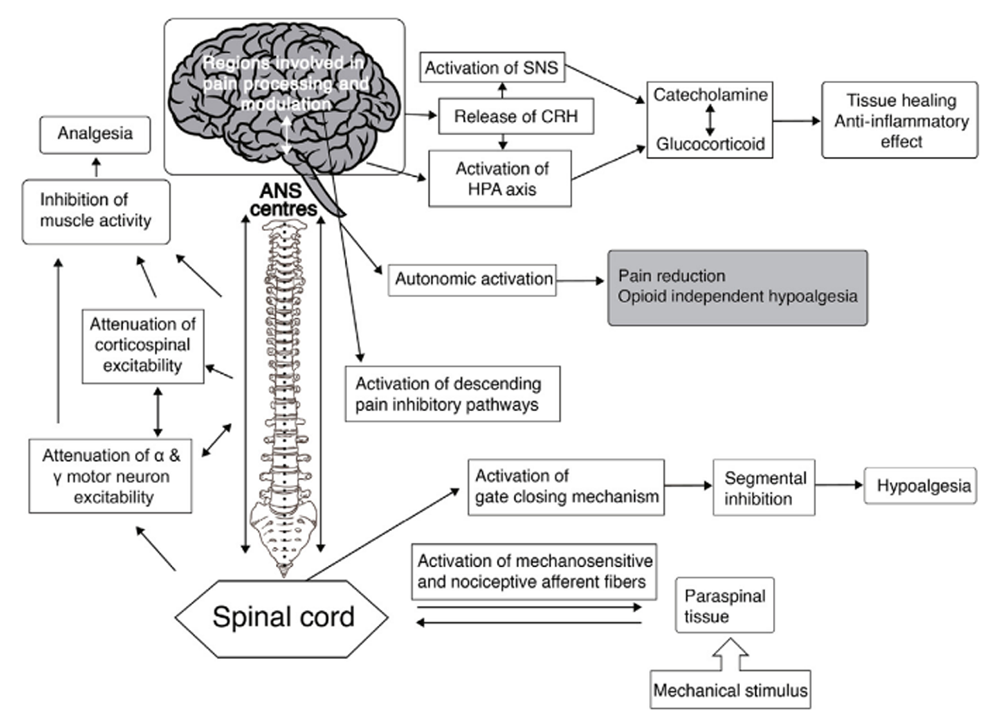
Neurophysiological effects of spinal manipulation
FROM: J Integrative Medicine 2019This presentation serves to demonstrate the widespread use and acceptance of the term subluxation. It acknowledges the broader chiropractic interpretation by recognition and adoption of the term outside the profession. In particular, it also emphasises the medical recognition supported by some of the medical evidence incorporating the construct of a chiropractic vertebral subluxation complex, and its utilisation in practice.
The vertebral subluxation concept is similar to the terms spinal dysfunction, somatic dysfunction, segmental dysfunction or the vague vertebral lesion. These terms are primarily used by osteopaths, physiotherapists and medical doctors to focus their manipulative techniques, but they relate primarily to the physical-mechanical aspects. In this respect, these terms are limited in what they signify. The implication of just plain osseous biomechanical dysfunction does not incorporate the wider ramifications of integrated neural, vascular, and internal associations which may involve greater ramifications, and should be more appropriately referred to as a vertebral subluxation complex (VSC).
Keywords: Medical Terminology; Vertebral Subluxation; Vertebral Subluxation Complex
From the Full-Text Article:
Introduction
The identity of a profession is in its name. It is also in the terminology adopted which underlies its raison d’etre, otherwise it would not be different to other professions. Particular terms portray the differences which have identified the chiropractic profession for over 120 years. These portray the basis of differentiating it as distinct from other professions in its scientific interpretation of the literature, clinical application, and philosophical rationale. [1]
The ‘vertebral subluxation’ is one of two keystones in chiropractic, and has been for its entire 127 year history since its foundation. The other term is ‘adjustment’ which may be identified as a refined and specific form of the more generalised generic term, ‘manipulation’. A number of these chiropractic adjusting techniques are unique to the profession. They have evolved and been modified over time and are perhaps not fully appreciated by some outside the profession. [2, 3]
It is noted however, that mounting manual therapy research in recent years is recognising the neurological element of spinal aetiologies, particularly in relation to the central sensitisation of pain, cervicogenic headaches, and lower back pain. [4-10]
Box 1 Not only is a chiropractic version of a subluxation acknowledged in medical literature, it is based on neurophysiological principles as noted by Sato, Sato, and Schmidt in their text ‘The impact of somatosensory input on autonomic functions’. [11] Their detailed studies confirm that spinal influence is particularly strong on the somatic element of somatosensory, somato-autonomic and somatovisceral reflexes. The significance of the role played by the spine lies with its integration with, and influence upon the autonomic nervous system. Sato et al recognise this by stating:
‘In contrast to the impressive body of knowledge concerning the effects of visceral afferent activity on autonomic functions, there is, generally speaking, much less information available on the reflex regulation of visceral organs by somatic afferent activity from skin, the skeletal muscle and their tendons, and from joints and other deep tissues. The elucidation of the neural mechanisms of somatically induced autonomic reflex responses, usually called somato-autonomic reflexes, is, however, essential to developing a truly scientific understanding of the mechanisms underlying most forms of physical therapy, including spinal manipulation and traditional as well as modern forms of acupuncture and moxibustion.’ (Emphasis added)
It should be noted that the spinal manipulation used by chiropractors is primarily directed at what they identify as vertebral subluxations, although these biomechanical disorders can affect various articulations throughout the body. The term is widely used by the profession. [16-33]
A search of the reveals 355 papers listed with the term ‘subluxation’ in their ‘title’, 549 under ‘Subject/Keyword’, and 917 in ‘All Field’s [34]
Review
We submit that as the ultimate authorities of Gray’s Anatomy and the World Health Organisation recognise the term ‘subluxation’ and ‘subluxation complex’, substantial researched evidence would need to be produced to oppose the concepts. However, there is additional evidence produced here which depicts medical recognition of the subluxation term and its rami>ications. This is represented by citing use of the term subluxation in a broader context in a range of medical textbooks on the spine, as well as a number of medical journal papers.
Gray’s Anatomy: Noted significance has to be attributed where it is stated in reference to the sacroiliac joint that ‘locking may occur …’ and that ‘This so-called subluxation of the sacroiliac joint causes pain’, and that ‘reduction by forcible manipulation may be attempted.’ [35]
World Health Organisation: While it seems somewhat imprecise to call it a disease, the vertebral subluxation has already been recognised by the World Health Organisation (WHO) in its publication, the World Classification of Diseases (ICD-10), which classifies ‘Biomechanical lesions, not elsewhere classified’ as item M99. It sub-classifies the VSC asitem M99.1: ‘Subluxation complex (vertebral)’.
Item M99.0 is designated ‘Segmental and somatic dysfunction’.These conditions come under the broader heading of ‘Diseases of the musculoskeletal system and connective tissue’ (M00- M99), and ‘Other disorders of the musculoskeletal system and connective tissue’ (M95-M99).
In placing M99.1 Subluxation Complex (Vertebral) under the classification of (M99.0 Segmental and somatic dysfunction) it recognises it as a distinctly separate entity. [36]
The vertebral subluxation has long been recognised by manual therapists and also by those involved in manual medicine, also known as manipulative medicine. It is recognised in the medical literature. Further recognition of the acceptance of the subluxation concept can be found by noting that there would be few if any, clinical findings in any health profession that have attracted some 500 synonyms, euphemisms, or other terms intimately related to the chiropractic subluxation. While not necessarily definitive proof in itself, this enigma of so many interpretations in the terminology may be seen as tacit recognition of an aberrant biological state, one that is different to normally functioning articular spinal segments, both anatomically and physiologically. [37-41]
Some critics question the subluxation because it is not clinically demonstrable, whereas it has been shown that inter-examiner agreement is particularly high. It has been suggested that to demonstrate or prove objectively that a patient has a headache would in fact be more difficult than proving that they have a subluxation. Similarly, anaesthesia has long been used in medicine but it is primarily based on empirical evidence. There is still much unknown about how it produces its necessary benefits, especially at the molecular level. This void has not raised questions as to whether or not it should be used, unlike those that query the subluxation. [42-48]
Some critics may suggest that the lack of a consistent definition is sufficient grounds for denying the existence of a subluxation. [1, 49] A similar claim could be made against the subluxation synonyms adopted by others. This would include terms such as manipulable lesion, facet joint lock, vertebral locking, end-play dysfunction, and cervical dysfunction, as well as others from a list.
Use of the term subluxation may be somewhat ambiguous in that it traditionally has had a different interpretation in the medical lexicon. While even that definition may be ill-defined, the case for the term of chiropractic subluxation or vertebral subluxation complex would clarify any ambiguity. The concept of a subluxation complex is subject to continuing interpretation as evidence emerges as well as other professions recognising it as a clinical entity. That evidence appears to be most supportive as no contradictory evidence or original research was identified.
There is noted evidence of medical use of chiropractic concepts particularly in European medicine, with many medical journals incorporating papers on these concepts, far more than in English language medical journals. Examples appear to be a distinct contradiction in attitude within medical circles. [50-58] In 1987, the medical doctor Gutmann stated in relation to birth trauma of infants that ‘The paediatrician’s diagnosis as well as the chiropractic and radiological examinations are of decisive importance…If the indications are correctly observed, chiropractic can often bring about remarkably successful results, because the therapy is a causal (i.e. pivotal) one.’ [59]
Logic alone would dictate that manipulation addresses a particular dysfunction, or a biomechanical spinal physiological abnormality. A manipulation would not be necessarily directed at a symptomless, normally functioning biomechanical spinal segment. Such a biological disturbance as the subluxation needs to be identified by nomenclature, to differentiate it from unaffected articulations. Chiropractic has survived and thrived today because it has recognised and addressed such lesions, and responded to patient demand - based on its understanding in managing subluxation-related disorders.
Medical Textbooks on Subluxations (Extracts)
The medical doctor Warbasse described the chiropractic model of a ‘subluxation’ in his text as early as 1918. He used that term to describe the vertebrogenic neurological implications of these clinical findings. He stated that ‘subluxations of vertebrae occur in all parts of the spine and in all degrees. When the dislocation is so slight as not to affect the spinal cord, it will still produce disturbances in the spinal nerves’. …. He later refers to these as ‘common subluxations’ and ‘Biner displacements’. [60]
Finnesson discusses a ‘Manipulable Spinal Lesion’ but recognises that it is euphemistically called a subluxation, osteopathic lesion, vertebral fixation, blockage and somatic dysfunction. Further, he does acknowledge vertebral malposition and abnormal vertebral motion, amongst other characteristics of the clinical finding. [61]
Schmorl and Junghanns would be two of the most noted medical spinal authorities who recognise segmental spinal disturbances. In discussing vertebral locking Schmorl and Junghanns nominate the spinal origin of autonomic influence when they refer to terms such as spondylogenic-neuro-autonomic, spondylogenic-vascular and spondylogenic pelvicopathy in relation to intervertebral insufficiency. (p. 219) They note that slight subluxation of vertebrae may occur. (p. 251) [62]
However, it is the noxious input from acute and chronic, sudden, and subliminal afferents that may constitute the key element in the vertebral subluxation complex. This would constitute a model of a somato-autonomic subluxation complex, the SASC. Schmorl and Junghanns also refer to ‘intervertebral instability and spondylogenic disturbances in relation to ‘interplay between sub-threshold autonomic nerve irritation and symptoms which appear a considerable distance from the nerve.’ (p. 227)
These authors recognise the dysfunction in a chiropractic subluxation and differentiate it from a medical subluxation, which they call articular locking and inefficient motor segment. They also note that ‘many physicians employ manipulations’ similar to those used by chiropractors and osteopaths. (p. 376) They discuss conservative treatment of intervertebral insufficiency and its spondylogenic sequelae and note the body’s own healing tendency and manual spinal treatment in relation to chiropractic and other manipulation professions. (p. 224)
Another authoritative medical text is by White and Panjabi who note that spinal manipulations for chiropractic subluxations must ‘produce improvement using mechanical alteration …’ on spinal structures ‘… that may be moved, stretched, stimulated, or relaxed’. [63]
A further medical doyen on the spine is Hadley. He describes ‘Subluxation (partial displacement) of the vertebral bodies ...’ (pps. 128-129), and a ‘spontaneous subluxation’ in recognition of the term.(pps. 132,127-149) [64]
Epstein notes that subluxations need to be evaluated clinically for restrictions of spinal movements, to confirm radiological findings. Alignment of spinous processes can be pathognomonic for subluxations. [65]
Keats notes that ‘Physiological subluxations can occur on children’s x-rays, simulating dislocations, particularly of C2 on C3 and C3 on C4 on forward flexion. In such circumstances there may be steps in lines 1 and 2, but line 3 will remain intact. All three lines are out of alignment with a real subluxation.’ [66]
In the textbook General Practice by the medical lecturer Dr John Murtagh from Monash University in Melbourne, Murtagh identifies the vertebral subluxation as vertebral dysfunction (and spinal dysfunction) as one of the possible etiological factors in a range of possible conditions. He also places emphasis on biomechanical lesion, as he regards vertebral dysfunction as one of only seven specified conditions that may simulate or masquerade as other conditions. Murtagh notes that a range of spondylogenic autonomic-related symptoms apart from pain syndromes may be associated with this dysfunction.
In the cervical spine these may include:
Headache
‘Migraine’-like headache
Myelopathy (sensory and motor changes in arms and legs)
Ipsilateral sensory changes of scalp
Dizziness/vertigo
Visual dysfunction.
Murtagh states however that ‘vertebrogenic pain syndromes have not been emphasised in medical training.’ [67, 68]
Lewit has used the term vertebrogenic in recognition of conditions originating from the spine.(p. 33) He also discusses this etiological relationship with visceral disorders. [69]
Maigne states quite clearly that ‘It is impossible to speak of manipulations without saying a word about “sacro-iliac subluxations”. These subluxations are one of the frequent conditions attended by chiropractors’. He notes further that these subluxations can be responsible for low-back pain, acute lumbagos, and sciaticas. Maigne also discusses a vertebrogenic association with a range of functional visceral disorders. [70]
There are sound physiological reasons for these clinical observations as have been outlined in such medical, chiropractic and osteopathic textbooks as:
Lewit K.
Manipulative therapy: musculoskeletal medicine.
Oxford, UK: Butterworth-Heinemann; 2009:281-297Biedermann H.
Manual therapy in children.
Edinburgh, UK: Churchill Livingstone 2004;133-144,195, 295-297Murtagh J.
General practice, 5e.
North Ryde, Australia, 2012, 1535 ppsMaigne R.
Orthopaedic medicine: a new approach to vertebral manipulation.
Spring>ield, MACharles C Thomas.
1972:27, 164, 192-209, 390Gatterman MI.
Foundations of chiropractic subluxation.
St Louis: Mosby, 1995, 487 pps.Leach RA.
The chiropractic theories. Principles and clinical applications. 3rd edn.
Baltimore: Williams & Wilkins. 1994, 401 ppsHaldeman S.
Principles and practice of chiropractic. 3rd ed.
New York: McGraw-Hill Medical: 2005, 1248 pps
The osteopathic author Greenman appears quite definite about the existence of vertebral disturbances when he states ‘Therefore SD or somatic dysfunction should be considered synonymous to, but not superior to nomenclature for segmental dysfunction, subluxation dysfunction, osteopathic lesion, or when referencing non-spinal bone misalignment structural deviation. References to that nomenclature are intended to engender speciBicity of diagnosis or assessment and to assist the reader who may know that condition by only that certain name.’ [71]
In citing Paris (1979) and Schmidt (2008). the physiotherapists Smale and Rayner acknowledge the gate control mechanisms of pain through the ‘biomechanical effects such as tissue lubrication or “correction of spinal joint subluxation”.’ [72]
Internationally, the chiropractic subluxation is recognised by at least two government departments in the USA. The US Medicare OfBice (Centers for Medicare and Medicaid) recognises the term subluxation in relation to spinal care provided by chiropractors. The US Agency for Healthcare Research and Quality also recognise the vertebral subluxation in chiropractic practice, noted as the Trauma Diagnosis Codes M9911 – M99.19, and as an AHRQ Guideline. [73-75]
In 2003, the US Department of Veterans Affairs (VA), Chiropractic Advisory Committee, ‘accepted public comments to assist in identifying issues and concerns regarding the development and implementation of a chiropractic health program within Veterans Health Administration (VHA).’ Under the Scope of Practice, it was stated that chiropractors provide ‘… care for neuromusculoskeletal conditions including the subluxation complex.’ It also stated that ‘Chiropractors must be allowed to use vertebral subluxations as a primary diagnosis when appropriate.’ Under the concluding section of B.4 Scope of Practice, it is stated that ‘Subluxation is speciBically mentioned in the statute as a unique area of chiropractic responsibility and authority and has been a long-standing element in federal health programs.’ [76]
In veterinarian practices the term subluxation was used more in a chiropractic sense at a conference in Germany. One course has presented material describing Vertebral and Extremity Challenge which allows the doctor to test for the presence of subluxations as well as determining the proper line of correction. Pelvic subluxation as defined in the basic certification course, is greatly expanded to define three types of pelvic categories. Methods for their diagnosis and correction are taught. Injury recall technique is a method to erase the neurological memory of past injuries which often interfere with normal healing, allowing subluxations to return. [77-80]
Discussion
The emergence of any new health profession may be identi>ied by its unique title. Similarly, its uniqueness may be identi>ied by its distinct use of particular terminology otherwise it could hardly be regarded as being different to any other profession. Consequently, chiropractic has developed two particularly distinctive terms; the ‘vertebral subluxation’ and the ‘vertebral adjustment’. As portrayed clinically and physiologically here, these two terms appear to have the potential to influence the ANS, and at times clinically signifies legitimate means of positively affecting a patients’ inherent recovery powers by their clinical outcomes. (81, 82)
The Vertebral Subluxation and Other Conditions.
The concept that subluxations are the cause of disease has long been dismissed. It is only political agitators who raise that superficial furphy. That subluxations may be an acknowledged factor in a range of conditions is not only a chiropractic observation, but a medical, physiotherapy and osteopathic one as well. (83)
Some of the most significant research and one of the most significant publications on the influence of somatic structures on the autonomic nervous system is not a chiropractic or osteopathic text. It is a full text report on the extensive research conducted on neurophysiology from neurophysiologists in Japan. No formal research has been found which contradicts the fundamental principles and findings published by Sato and colleagues in the numerous papers on their findings. (84, 85)
Subluxations have been associated with a range of headaches of neck origin. Cervicogenic headaches are also listed in the WHO’s ICD-10 and the medically recognised mediator with headaches is the autonomic nervous system. A cervicocranial syndrome is allocated as code M53.0. It would be imprudent to think that disturbance of the ANS ceases with headaches, when other areas may also be affected through this autonomic distribution. The 2013 edition of the International ClassiBication of Headache Disorders (ICHD) classifies a Cervicogenic Headache as ICHD-3 code 11.2.1. This designation must now regard cervical subluxations officially as a ‘medical’ term. (86,87)
Cailliet devotes a whole chapter to subluxation of the cervical spine and defines a subluxation as a derangement of the opposing joint surfaces, and just a degree of a luxation. (88 p.61) While acknowledging a wide range of potential neurological symptoms. (p. 37)
In 1970, Prof Stuart Butler reported on medical evidence by Braaf and Rosner. He stated that they averred that ‘More than 90% of recurring headaches can be traced to mechanical derangement of the cervical or neck portion of the spine produced by injury.’ This finding did not appear to alter the standard medical approach in the amelioration of headaches. (89)
In recognition of acceptance of the subluxation terminology, a 2015 study in North America found that a majority of the 7,455 chiropractic students surveyed agreed or strongly agreed (61.4%) that the emphasis of chiropractic intervention in practice is to eliminate vertebral subluxations/vertebral subluxation complexes. A further 15.2% neutral, and only 23.3% disagreeing. It is suggested that ‘modulation’ of vertebral subluxations may have attracted an even higher rate of agreement. (90)
Although many medical doctors accept, collaborate and in fact adopt chiropractic concepts, it is submitted that politically, these concepts are being adjudged critically by others where a traditional resistance to new concepts can be based on unsubstantiated opinion. This tends to disregard or ignore the medical citations presented here.
We would maintain that noxious somatovisceral reflexes (11, 91) are a key factor in cervicogenic headaches. (92) functional conditions such as vertebrogenic dysphagia, (93, 94) vertebrogenic dyspepsia ,(95) infantile colic. (96) and certain cardiovascular changes. (6, 7. These represent published studies of potential pathophysiology examples associated with the subluxation complex. There are also rather extensive clinical phenomena noted by European medical doctors. (97)
Removing the term subluxation from the chiropractic lexicon would effectively be a form of containment and a step away from what the profession has established and has successfully stood by for over a century, and now supported within the literature.
Conclusion
The evidence we have presented indicates that medicine, osteopathy, and physiotherapy have all used the term ‘subluxation’ in the chiropractic sense. However, the more appropriate, and inclusive descriptive term of vertebral subluxation complex is widely adopted in chiropractic and the WHO ICD-10. It would be most incongruous for chiropractic to move away from using subluxation when it is so well established.
A move to deny clarity to the essence of chiropractic may well affect the public image of the profession. As Hart states ‘Identifying the chiropractic profession with a focus on vertebral subluxation would give the profession uniqueness not duplicated by other health care professions and, therefore, might legitimatise the existence of chiropractic as a health care profession. An identity having a focus on vertebral subluxation would also be consistent with the original intent of the founding of the chiropractic profession.’ (82)
The term ‘vertebral subluxation’ has been in general use and understanding in the chiropractic profession as is ‘chiropractic subluxation’ and ‘vertebral subluxation complex’ (VSC). It is a part of the profession’s heritage.
Critics of concepts regarding subluxation offer no original evidence to support their case, and that appears to be just political opinion rather than providing evidence to substantiate their stand.
The evidence presented in this paper supports the contention that there would be no vertebrogenic symptoms associated with physiologically normal vertebral segments. The term designated by chiropractors to identify abnormal or pathophysiological segmental dysfunction is the vertebral subluxation.
It has been a part of chiropractic heritage for over 120 years.
References:
Johnson C.
Use of the Term Subluxation in Publications During
the Formative Years of the Chiropractic Profession
J Chiropractic Humanities 2011 (Dec); 18 (1): 1–9Pickar JG.
Neurophysiological Effects of Spinal Manipulation
Spine J (N American Spine Society) 2002 (Sep); 2 (5): 357–371Kang YM, Choi WS, Pickar JG.
Electrophysiological evidence for an intersegmental
reflex pathway between lumbar paraspinal tissues.
Spine 2002;27(3):E56-E63Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ.
The Mechanisms of Manual Therapy in the Treatment of Musculoskeletal Pain:
A Comprehensive Model
Man Ther. 2009 (Oct); 14 (5): 531–538Schmid A, Brunner F, Wright A, Bachmann LM.
Paradigm shift in manual therapy? Evidence for a central nervous system
component in the response to passive cervical joint mobilisation.
Man Ther 2008;13(5):397-396Vincenzino B, Cartwright T, Collins D, Wright A.
Cardiovascular and respiratory changes produced by
lateral glide mobilisation of the cervical spine.
Man Ther 1998;3:67-71Isaev AP, Sabiryanov AR, Lichagina SA, Sabiryanov ES.
Physiological mechanisms of the effects of manual therapy
on the orthostatic response of the cardiovascular system.
Human Physiol 2005;31(4):425-9Savigny P, Kuntze S, Watson P, et al.
National Institute for Health and Care Excellence (NICE 2009)
Early Management of Persistent Non-specific Low Back Pain
Royal College of General Practitioners Published date: May 2009Sharma A, Alahmari K, Ahmed I.
Efficacy of manual therapy versus conventional physical therapy in
chronic low back pain due to lumbar spondylosis. A pilot study.
Med Sci (Basel) 2015;3:55-63Reiman MP, Harris JY, Cleland JA.
Manual therapy interventions for patients with lumbar stenosis:
a systematic review.
NZ J Physioth 2009;37(1):17-28Sato A, Sato Y, Schmidt RF.
The impact of somatosensory input on autonomic functions.
Reviews of Physiology Biochemistry and Pharmacology.
Blaustein MP et al Eds.
Springer-Verlag, Berlin. 1997;130:1-2Mein EA, Richards DG, McMillin DL, McPartland JM, Nelson CD.
Physiological Regulation Through Manual Therapy
Physical Medicine and Rehabilitation: State of the Art Reviews 2000 (Feb); 14 (1)Richards DG, McMillin DL, Mein EA, Nelson CD.
Osteopathic Regulation of Physiology
AAOJ 2001 (Fall); 11 (3): 34-38Vigotsky AD, Bruhns RP.
The neurophysiological response to manual therapy and
its analgesic implication: a narrative review
https://dx.doi.org/10.7287/peerj.preprints.996v2 | CC-BY 4.0 Open Access | rec: 5 Jun 2015, publ: 5 Jun 2015Potter L, McCarthy C, Oldham J.
Physiological effects of spinal manipulation:
a review of proposed theories.
Physical Ther Rev. 2005;10:163-170Bolton SP.
“Subluxation,” “Chiropractic subluxation,” Volkman’s subluxation:
and Palmer’s Subluxation.” A commentary on style and usage.
Chiropr J Aust. 2010;40(2):77-85Budgell B.
Subluxation and Semantics: A Corpus Linguistics Study
J Can Chiropr Assoc. 2016 (Jun); 60 (2): 190–194Budgell BS.
Reflex Effects of Subluxation: The Autonomic Nervous System
J Manipulative Physiol Ther 2000 (Feb); 23 (2): 104–106Cates JR, Young DN, Guerriero DJ, et al.
Independent guideline appraisal summary report for vertebral subluxation
in chiropractic practice (CCP) guidelines.
J Chiropr Med. 2002;1(2):72-4Ebrall P.
Towards better teaching about the vertebral subluxation complex.
Chiropr J Aust. 2009;39(4):165-70Gatterman MI.
Foundations of chiropractic subluxation. 2nd ed.
St. Louis, Miss. Elsevier Mosby; 2005Gatterman MI.
Subluxation – Historical Perspectives
Chiropractic Journal of Australia 2009 (Dec); 39 (4): 151–164Good, C. (2010b).
The Great Subluxation Debate: A Centrist's Perspective
J Chiropractic Humanities 2010 (Jun); 17 (1): 33–39C Good
The Subluxation Syndrome: A Condition Whose Time Has Come?
J Chiropractic Humanities 2004; 11: 38–43Haavik-Taylor H, Holt K, Murphy B.
Exploring the Neuromodulatory Effects of the
Vertebral Subluxation and Chiropractic Care
Chiropractic Journal of Australia 2010 (Mar); 40 (1): 37–44Leach RA.
The chiropractic theories, principles and clinical applications.
3e. Baltimore: Williams & Wilkins. 1994Owens EF.
Chiropractic subluxation assessment: what the research tells us.
J Can Chiropr Assoc. 2002;46(4):215–220.Peters R.
The Subluxation – Historical Perspectives Part II
Chiropractic Journal of Australia 2009 (Dec); 39 (4): 143–150Rome PL.
Chiropractic hospital appointments in Australia –
An international comparison.
Chiropr J Aust. 2016;44(2):142-63.Vernon H.
Historic overview and update on subluxation theories.
J Chiropr Humanit. 2010;17(1)Wenban AB.
Subluxation research: a survey of peer-reviewed
chiropractic scientific journals [review].
Chiropr J Aust. 2003;33(4):122-30Yochum TR, Rowe LJ.
Essentials of skeletal radiology. 2e. Vol 1.
Baltimore: Williams and Wilkins; 1987:162Medicare.gov.
Chiropractic services.
https://www.medicare.gov/coverage/chiropractic-services.htmlhttps://www.chiroindex.org/? action=doSearch&advanced_search=1&search1=
subluxation&type1=article&bool1=AND&search2&type2=all&bool2=
AND&search3&ty pe3=all&journalId&year1&year2
&peer=peer&ptId#resultsWilliams PL, Warwick R.
Gray’s Anatomy 36th Edn.
New York: Churchill Livingstone;1980;477ICD-10.
World Health Organisation
http://www.who.int/classifations/apps/icd/icd10online/Rome PL.
Medical evidence recognising the vertebral subluxation.
Chiropr J Aust. 2016;44(4):303-7Rome PL.
A basis for the theory of a central chiropractic principle:
The vertebral subluxation.
Chiropr J Aust. 2013;43(1):2-13Rome PL.
Terminology relating to the vertebral subluxation complex
and the manipulative sciences. (Part 1)
Chiropr J Aust. 2017;45(2):73-89Rome PL.
Terminology relating to the vertebral subluxation complex
and the manipulative sciences. (Part 2)
Chiropr J Aust. 2017;45(2):90-130Rome PL.
Usage of chiropractic terminology in the literature:
296 ways to say “subluxation”. Complex issues
of the vertebral subluxation.
Chiro Tech. 1996;8(2):49-60Holt K, Russell D, Cooperstein R, et al.
Interexaminer Reliability of a Multidimensional Battery
of Tests Used to Assess for Vertebral Subluxations
Chiropractic Journal of Australia 2016; 46 (1): 100–117Burk JM, Rhudy TR, Ratliff CR.
Inter- and intra-examiner agreement using Gonstead line marking method.
Am J Chiropr Med. 1990;3:114-7Cooperstein R, Young M.
The Reliability of Spinal Motion Palpation Determination of
the Location of the Stiffest Spinal Site is Influenced by
Confidence Eatings: A Secondary Snalysis of Three Studies
Chiropractic & Manual Therapies 2016 (Dec 20); 24: 50Fingleton CP, Dempsey L, Smart K, Doody CM.
Intra-examiner and interexaminer reliability of manual palpation and
pressure algometry of the lower limb nerves in asymptomatic subjects.
J Manipulative Physiol Ther. 2014;37(2):97-104Arab AM, Abdollahi I, Joqhataei MT, Golafshani Z, Kazemnejad A.
Inter- and intra-examiner reliability of single and composites of
selected motion palpation and pain provocation tests for sacroiliac joint.
Man Ther. 2009;14(2):213-21Bridging the brain-mind gap.
ABC Radio National May 9, 2018
http://www.abc.net.au/radionational/programs/bigideas/
bridging-thebrain-mind-gap/9719956Dvorsky G.
Why anaesthesia is one of the greatest medical mysteries of our time.
April 29, 2016
https://www.gizmodo.com.au/ 2016/04/why-anaesthesia-is-one-
of-the-greatest-medical-mysteries-of-our-time/Nelson C.
The subluxation question.
J Chiropr Humanit. 1997;7:46-55Lehmpfuhl W.
Kopfschmerz bis zur atlantoaxialen subluxation
[Headache to atlanto-axial subluxation.]
Ther Ggw. 1951 May;90(5):175-9Lehmpfuhl W.
Die behandlung des subluxations - koptschmerzes.
[Therapy of the subluxation--headaches.]
Dtsch Med Wochenschr/ 1950 Dec 29;75(52):1747-48Figar S, Krausova L, Lewit K.
[Plethysmographic investigations in the chirotherapy of vertebral disorders.]
Acta Neuroveg (Wein). 1967;29(4):618-23Rychlíková E.
[Vertebrogenic functional disturbances with chronic ischemic heart disease.]
Vertebragene functionelle Störungen bei chronischer ischämischer Herzkrankheit.
Münchner Medizinische Wochenschrift 1975;117:127. (Cited in:
Lewit K. Manipulative therapy in rehabilitation of the locomotor system.
3e. Oxford: Butterworth Heinemann;1999:283-284.)
(See also MMW Munch Med Wochenschr 1975;117(4):127-30Seuss W.
Therapie des bluthochdrucks durch chiropractic.
(Therapy for high blood pressure through chiropractic.
Heilkunst 1960;73.
(As cited in Weiant CW, Goldschmidt S.
Medicine and chiropractic. Self Published, New York.1966:123Simonenko VB, Tesiq AN, Shirokov EA, Davydov OV.
[Some features of coronary artery disease combined with vertebrogenic thoracoalgias.]
(Incls vertebrogenous cardiomyalgia)
Klin Med (Mosk). 2007;85(1):61-63.
(Article in Russian – Pubmed abstract in English.)Falkenau HA.
[Chiropractic management of the cervical syndrome in oto-rhino-laryngology (Author’s translation)]
HNO. 1977;25(8):269-272. (German) (Abstract Only).Falkenau HA.
[The pathogenesis and chiropractic management of cervical dysphagia)
Author’s translation.)]
Laryngol Rhinol Otol (Stuttg). 1977;56(5)467-469. (German)Na H-J, Chang S-G.
A diagnostic imaging case of cervical spinal subluxation
for chuna manual therapy: cervical malposition with OPLL.
J Korean Med. 2016;37(4):45-48.Gutmann G.
Das atlas-blockierungs-syndrom des säuglings und des kleinkindes.
[The atlas fixation syndrome of the infant and toddler.]
Manuelle Medizin. 1987;25:5-10
http://icpa4kids.org/Chiropractic-Research/the-atlas-fixation-syndrome-
in-the-baby-and-infant-germantitle-das-atlas-blockierungs-syndrom-
des-sauglings-und-des-kleinkindes.htmlWarbasse JP.
Subluxation of vertebrae.
In: Surgical treatment. a practical treatise on the therapy of surgical
diseases for the use of practitioners and students of surgery.
Vol 1.WB Saunders Co, Phil. 1918:623Finneson BE.
Low back pain.2e.
Philadelphia: JB Lippincott Co. 1980; 251-259Schmorl G, Junghanns H.
The human spine in health and disease. 2e.
New York. Grune & Stratton. 1971;185-242White AA, Panjabi MM.
Clinical biomechanics of the spine.
Philadelphia: JB Lippincott Co. 1978.Hadley LA.
Anatomico-roentgenographic studies of the spine.
Springfield. Charles C Thomas.1976;127-149,430-8Epstein BS.
The spine – a radiological text and atlas. 4th edn.
Philadelphia: Lea & Febiger. 1976:30,557-9Keats TE, Anderson MW.
The neck. Chapter 3.
In: Atlas of normal roentgen variants that may simulate disease.
7e. St Louis: Mosby Inc.2001:66Murtagh J.
General practice. 5e.
North Ryde. 2012Murtagh J.
John Murtagh’s general practice. e6 Chapter 24.
Spinal dysfunction
https://murtagh.mhmedical.com/content.aspx? sectionid=116026062&bookid=1522Lewit K.
Manipulative therapy in rehabilitation of the locomotor system.
3e. Oxford: Butterworth Heinemann; 1999:33,282-7Maigne R.
Functional disturbances.
In: Orthopaedic medicine: A new approach to vertebral manipulations.
Springfield: Charles C Thomas; 1972.164,192-209, 390Greenman PE.
Somatic dysfunction: somatic screening exam introduction.
An osteopathic approach to diagnosis and treatment.
Undated.
American Academy of Manual Medicine
http://www.webmanmed.com/somdysfunc.htmlSmale S, Rayner A.
Chain reaction – the neurophysiological mechanism of manual therapy
http://www.raynersmale.com/blog/ 2015/7/10/chain-reaction-
the-neurophysiological-mechanism-of-manual-therapyhttps://downloads.cms.gov/medicare-coverage-database/lcd_attachments/
31862_17/Chiropractic_FactSheet09.18.14.pdfhttps://qualityindicators.ahrq.gov/Downloads/Modules/PSI/
V70/TechSpecs/PSI_Appendix_G.pdfhttps://www.guideline.gov/summaries/summary/47342/
subluxation-chiropractic-practice?q=chiropractichttps://www.chirobase.org/15News/vacomments.pdf
International Academy of Veterinary Chiropractic.
Freetz, Germany. Oct 28-31, 2014
https://ivca.de/wp-content/uploads/2014/09/
Course-Registration-Advanced-Animal-Chiropractic-Course.pdfInman WL.
Veterinary orthopaedic manipulation
www.oakwoodhillsanimalhospital.com/refId,60104/refDownload.pm.Maler MM.
Overview of veterinary chiropractic and its use in paediatric exotic patients.
Vet Clin Exot Anim 2012;15:299-310
https:// www.vetexotic.theclinics.com/article/S1094-9194(12)00008-4/pdfVertebral subluxation complexes.
International Academy of Veterinary Chiropractic. (Germany)
https://www.i-a-v-c.com/index.php/animal-chiropractic.htmlDoctors shouldn’t be robbed of the language of our craft.
Medical Observer April 20 2017.
https://www.medicalobserver.com.au/ professional-news/
doctors-shouldnt-be-robbed-of-the-language-of-our-craftHart J.
Analysis and Adjustment of Vertebral Subluxation as a Separate and
Distinct Identity for the Chiropractic Profession: A Commentary
J Chiropractic Humanities 2016 (Oct 25); 23 (1): 46–52Huijbregts PA.
The chiropractic subluxation: implications for manual medicine.
[Editorial] J Man Manip Ther. 2005;13(3):139-14Sato A. Sato Y, Schmidt RF.
The impact of somatosensory input on autonomic functions.
Rev Physiol Biochem Pharmacol. Berlin, Springer, 1997;328ppsSato A.
Neural mechanisms of autonomic responses elicited by somatic sensory stimulation.
Neurosci Behav Physiol. 1997;27(5):610-21World Health Organisation’s publication,
World Classification of Diseases (ICD-10) 2017/18
http://www.icd10data.com/search?s=cervicogenicThe International classification of headache disorders, 3rd edn. 2013.
Cephalalgia. 2013;33(9):629-808.
http://www.ihs-headache.org/ binary_data/1437_ichd-iii-beta-
cephalalgia-issue-9-2013.pdfCailliet R.
Subluxations of the cervical spine including the “whiplash” syndrome.
In: Neck and arm pain.
Philadelphia. FA Davis Co. 1964:60-85Butler S.
Headaches a real pain-in-the-neck.
Sydney Telegraph. August 27th 1970 pp7.Gliedt JA, Hawk C, Anderson M, Ahmad K, Bunn D, Cambron J, et al.
Chiropractic Identity, Role and Future:
A Survey of North American Chiropractic Students
Chiropractic & Manual Therapies 2015 (Feb 2); 23 (1): 4Rome P. Waterhouse JD.
Neurodynamics of vertebrogenic somatosensory activation and
Autonomic Reflexes - a review: Part 7 The Cervicogenic Factor.
Asia-Pacific Chiropr J. 2021;1.4
apcj.net/papers-issue-2-4/#RomeWaterhousePart7CervicogenicRome P. Waterhouse JD.
Neurodynamics of vertebrogenic somatosensory activation and
Autonomic Reflexes - a review: Part 9 Cervicogenic headaches.
AsiaVanáskova E, Dolina J, Hep A.
Swallowing disorders related to vertebrogenic dysfunctions.
In: Brzozowski T (Ed). New advances in the basic and clinical gastroenterology.
Chapter 8. 2012:175-184
https://www.intechopen.com/books/new-advances-in-the-basic-and-
clinicalgastroenterology/swallowing-disorders-related-to-
vertebrogenic-dysfunctions.Vanáskova E, Hep A, Lewit K, et al.
Cervical dysfunction and disturbed oesophageal motility – scintigraphic assessment.
J Orthop Med. 2001;23(1):9-11
https://doi.org/10.1080/1355297X.2001.11736122Rome P. Waterhouse JD.
A neurological evidence base for the Vertebrogenic Dyspepsia Syndrome:
A somatosensory link to visceral dysfunction.
Asia-Pacific Chiropr J. 2022;2.6
apcj.net/papers-issue-2-6/#RomeWaterhouseDyspepsiaRome PL, Waterhouse JD, Maginness G, Ebrall P.
Medical management of infantile colic with spinal manipulation:
A narrative review of the European medical literature [review].
J Contempt Chiropr. 2019;2:60-74Rome P. Waterhouse JD.
Neurodynamics of vertebrogenic somatosensory activation and Autonomic Reflexes -
a review: Part 6 International medical literature and its clinical
application of the somatovisceral model.
Asia-Pacific Chiropr J. 2021;1.4
apcj.net/ papers-issue-2-4/#RomeWaterhouseIntMedLit6.
Return to SUBLUXATION THEORY
Since 1-05-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |