

Clinical Practice Guideline for Best Practice Management
of Pediatric Patients by Chiropractors:
Results of a Delphi Consensus ProcessThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Integr Complement Med 2024 (Mar); 30 (3): 216–232 ~ FULL TEXT
OPEN ACCESS Genevieve Keating, BAppSc (Chiro), PhD • Cheryl Hawk, DC, LMT, PhD
Lyndon Amorin-Woods, BAppSc (Chiropractic), MPH
Deisy Amorin-Woods, BAPsych, DipEd, BSW
Sharon Vallone, DC, et al.
Fielding Graduate University,
Santa Barbara, CA, USA.

Objective: To build upon existing recommendations on best practices for chiropractic management of children by conducting a formal consensus process and best evidence synthesis.
Design: Best practice guide based on recommendations from current best available evidence and formal consensus of a panel of experienced practitioners, consumers, and experts for chiropractic management of pediatric patients.
Methods: Synthesis of results of a literature search to inform the development of recommendations from a multidisciplinary steering committee, including experts in pediatrics, followed by a formal Delphi panel consensus process.
Results: The consensus process was conducted June to August 2022. All 60 panelists completed the process and reached at least 80% consensus on all recommendations after three Delphi rounds. Recommendations for best practices for chiropractic care for children addressed these aspects of the clinical encounter: patient communication, including informed consent; appropriate clinical history, including health habits; appropriate physical examination procedures; red flags/contraindications to chiropractic care and/or spinal manipulation; aspects of chiropractic management of pediatric patients, including infants; modifications of spinal manipulation and other manual procedures for pediatric patients; appropriate referral and comanagement; and appropriate health promotion and disease prevention practices.
Conclusion: This set of recommendations represents a general framework for an evidence-informed and reasonable approach to the management of pediatric patients by chiropractors.
Keywords: adolescent; child; chiropractic; infant; manipulation; mobilization; pediatrics; spinal; spine.
From the Full-Text Article:
Introduction
Chiropractors are concerned with the assessment, diagnosis, treatment, and prevention of disorders of the neuromusculoskeletal system and the potential effects of these disorders on general health for people of all ages. [1, 2] Although other types of health care providers, such as physical therapists, treat musculoskeletal symptoms in children (patients3] chiropractic is the most common complementary and integrative medicine practice used by children in the United States [4] and is also commonly used by children around the world, including in Australia. [5] In Australia, the best estimates are that chiropractors provide care to more than 30,000 child patients (0–18 years old) every week. [6] According to a 2017 scoping review, ~8% of chiropractic patients are 18 years of age and under. [7] Manual care for children is most often sought for the treatment of musculoskeletal (MSK) conditions. [8]
In 2019, in Victoria, Australia, a state government inquiry into chiropractic care of children under 12 was conducted by Safer Care Victoria (SCV). [9] SCV sought input from consumers and received 22,043 responses from parents who had accessed chiropractic care for their child(ren) under 12 years of age. While most respondents sought chiropractic care for musculoskeletal conditions, up to 40% were related to developmental concerns. [10] Most of the children who presented to chiropractors were also under the care of other health professionals for their presenting concerns. The other health professionals consulted were primarily general (medical) practitioners, maternal and child health nurses, and medical specialists. Over 99% of parents of children consulting chiropractors in the report felt well informed and involved in the decisions about the care. According to the parents, 98.4% said they had noticed, or their child had reported, an improvement after the care was provided. [11]
Another major part of the SVC inquiry was the commission of a Cochrane Collaboration review of the efficacy and safety of chiropractic spinal manipulation for children. [12] This Cochrane Review was not published in a scientific journal but played a key role in determining the SCV recommendations. [13] The review, in common with other reviews, noted that adverse events (AEs) are very rare in children receiving chiropractic manipulation. [8, 12, 14] A 2023 retrospective analysis of 54,846 patients, involving 960,140 chiropractic treatment visits, found that none of the 39 AEs reported occurred in children; the median patient age of those with AEs being 50.8 years. [15]
However, because of the lack of definitive evidence of efficacy and effectiveness for various conditions, the Cochrane review concluded that spinal manipulation is not recommended for children under 12, for a number of conditions, or for general wellness. [12, 13] It is important to note that the Cochrane review defined “spinal manipulation” as “any technique delivered by any health professional that involves a high-velocity, low-amplitude (HVLA) thrust beyond the physiological range of motion, impacting the spine, within the limits of anatomical integrity.”1 [12](p.4) The SCV report refers to a statement by the authors of one of the primary source documents cited by the Cochrane Collaboration that chiropractors who treat children modify both biomechanical force and speed to accommodate the child's age and physical development so they are often not using an HVLA thrust. [16] Quite apart from the recommendations of SCV, chiropractors have also acknowledged the pressing need for research on chiropractic care for children. [17, 18]
Chiropractic, in common with other manual care professions, is responsible for ethical and safe practice, which requires cultivating and mastering both an academic foundation and clinical expertise. [1] Chiropractic undergraduate education involves the study of the unique anatomy and physiology of the child as well as the modification of evaluative and therapeutic procedures as applied to this unique population when addressing neuromusculoskeletal problems and the potential effect on overall health and wellbeing. In Australia, chiropractic education specifically requires graduates to adapt practice according to varying patient needs across the human lifespan, including the need for care and management options to be tailored for individuals. [19](p.13)
By nature of training and scope, chiropractors also address public health issues and supportive measures for healthy human development during the clinical encounter. [20] These may include advice regarding injury prevention, healthy diet, physical activity needs, sleep advice, reduced screen time (including mobile/cell phone use), healthy social relationships, and vigilance around childhood trauma. [21–23] It has been found that, in general, children with a decreased health-related quality of life have higher utilization of complementary and integrative medicine. [24, 25]
In 2009 and 2016, Hawk et al. performed consensus processes, gathering expert opinion on best practices for the chiropractic care of children. [21, 22] The resulting documents have helped provide practitioners with guidelines. They have also been helpful to other providers, the public, and third-party payers in demonstrating that the chiropractic profession has high standards for the care of children. However, the most recent of these documents were based on the literature published before 2015, so in keeping with recommendations for guidelines [26, 27] and to address a key recommendation of the SCV regarding the safety of chiropractic care, we conducted this project.
Aims and Purpose
This project aimed to build upon the existing recommendations on best practices for the chiropractic management of children by conducting a formal Delphi consensus process and best evidence synthesis. Our new emphases were on providing the safest possible chiropractic care for children and providing appropriate health promotion and disease prevention practices. The process was based on the 2016 best practices [22] recommendations and the findings of the SCV Cochrane review with a brief update of the SCV's review of the safety of spinal manipulation for children.
Methods
Human subject considerations
No data were collected from any patients or parents of patients. The only personal data collected were from the Delphi consensus panel experts. The project was approved by the Institutional Review Board of the Project Director's (C.H.) institution before collection of any information from these individuals. As part of this process, the panelists signed a consent form confirming their voluntary and uncompensated participation. They also signed a permission-to-acknowledge form before submission of the article for publication.
Steering committee
The steering committee (SC) was composed of experienced clinicians and academics from health professions involved in the care of children, and several also represented chiropractic organization stakeholders.
The SC's role in the project was to provide input on evidence, contribute to drafting the seed recommendations, revise the recommendations based on the Delphi panel's comments and ratings to achieve consensus, and contribute to the development of the final article.

Table 1 Table 1 summarizes the expertise and affiliations of the SC. Of the 16 members, 13 are chiropractors; of those, 2 are also cross-trained as medical physicians (1 Medical Pediatrician); other professions in which the chiropractors are cross-trained are health education, lactation consulting, massage therapy, and public health.
Those SC members who are not chiropractors represent family therapy, psychology, social work (1), midwifery/lactation consulting (1), and nursing (1). Five of the SC members have PhDs; topics for these PhDs are Early Childhood Development; Musculoskeletal Health of the Infant; Preventive Medicine; Midwifery, Maternal, and Child Health; and Nursing. Four are faculty at chiropractic institutions.
Eight members have advanced training/certification in pediatrics. For purposes of stakeholder representation, these chiropractic organizations are represented by SC members: Australian Chiropractors Association (Aus-ACA), American Chiropractic Association (U.S.-ACA), U.S. Clinical Compass, and International Chiropractors Association (ICA). Two nonchiropractic SC members represented the consumer perspective.
Approach to the literature search
We began the project with two seed documents. First was the 2016 set of recommendations on best practices for chiropractic care for children, which had been itself an update of recommendations published in 2009. [21, 22] We used this set of recommendations as a starting point for this project and included updates and expansion based on current evidence and issues.
The second document was the 2019 systematic review prepared by Cochrane Australia for SCV. [12] Although this rapid review of the effectiveness, efficacy, and safety of spinal manipulation for children was not published in a peer-reviewed journal, as an official government publication, we used its findings as a primary resource for developing our recommendations. The Cochrane Australia Review concluded that, although AEs were rare, they could not draw conclusions about the safety and effectiveness of spinal manipulation for children under 12 because of the paucity of studies and lack of specific treatment information. [12]
For this reason, we decided that until more definitive research is available, it is still premature to make recommendations on the treatment of specific conditions in children. Therefore, because studies on the effectiveness and efficacy of even the most common conditions for which children seek chiropractic care are likely to remain sparse in the immediate future, we made the decision to focus our evidence-based recommendations on ensuring that chiropractic care is delivered as safely as possible.
Primary search strategy
We conducted a literature search to update the evidence on safety obtained from the Cochrane Australia Review, which ended in June 2019. Our research question was: “What are the adverse events associated with chiropractic care, including spinal manipulation among children (<18 years of age)?” [22] To not be redundant with the results of the Cochrane Australia Review, we used a start date after that study's search ended. Since similar searches we have used in the past have found that high-quality articles were not missed in PubMed, we did not include other databases in the search. In February 2022, we searched PubMed from July 1, 2019 to January 31, 2022 using these terms: (“Manipulation, Spinal” OR “Manipulation, Chiropractic” OR Chiropractic OR “manual therapy” OR “manual therapies”) AND (pediatric OR pediatrics OR child OR infant OR adolescent OR newborn) AND (safety OR “adverse effects” OR “adverse events”)
Eligibility criteria for articles on AEs and safetyInclusion criteria were:
Exclusion criteria were:
- Published July 1, 2019 to January 31, 2022
- Human subjects
- English language
- Chiropractic spinal manipulation was the treatment/intervention
- Study population was children (<18 years)
- Included information on AEs/safety
- Commentaries/editorials/letters
- Nonpeer-reviewed publications
- Study protocols with no results
- Surveys and other cross-sectional studies
- Conference abstracts
At least two investigators screened the search results for eligibility.
Secondary (targeted) searches
As we developed the seed statements, which addressed each component of the clinical encounter, we conducted targeted searches for documentation. These were not formal and exhaustive searchers; we asked topic experts in our SC to also consult their personal libraries, using the same eligibility criteria as the previous search. We added an expanded section on health promotion and disease prevention practices recommended for all health professionals to this set of recommendations; thus, we searched recognized organizations, including the U.S. Preventive Services Task Force (USPSTF) and the U.S. Centers for Disease Control and Prevention (CDC), as well as a recently published clinical practice guideline (CPG) developed specifically for the role of chiropractic in health promotion and disease prevention for adults with musculoskeletal pain.20,28,29
Evaluation of the quality of the evidence
In keeping with the precedent used by the Cochrane Australia Review, we did not assess the quality of the studies from the search for AEs related to spinal manipulative therapy (SMT). For evidence supporting recommendations on “best practices” for chiropractors treating children (which were identified through targeted searches and SC recommendations), we evaluated the quality of CPGs, systematic reviews/meta-analyses, randomized controlled trials (RCTs), and narrative reviews. Other types of articles were categorized as “lower level” quality of evidence and were not formally rated. Although rapid reviews are an increasingly popular method of assessing the literature, [30] there is not yet agreement on the best set of quality assessment considerations, so we did not formally assess the quality of rapid reviews.

Table 2

Table 3

Table 4

Table 5 We evaluated CPGs using the AGREE-GRS (Global Rating Scale) (Table 2).31 We evaluated systematic reviews (Table 3) and RCTs (Table 4) using modified SIGN (Scottish Intercollegiate Guideline Network) checklists. [32] We evaluated narrative reviews (Table 5) using SANRA (scale for the quality assessment of narrative review articles). [33]
At least two investigators (C.H., L.A.-W., D.A.-W., A.S.) rated each article; differences in ratings were resolved by discussion.
Seed statement development
The SC used the 2016 best practices for chiropractic care for children document as a starting point to develop the seed statements. [22] For this project, we expanded the brief section in the 2016 article on health promotion and disease prevention. We used the literature search results to inform the process of developing draft seed statements. Using an iterative process, the SC continued drafting the seed statements to achieve clarity and incorporate the best evidence to support them. When they reached agreement, the statements were then ready for the Delphi process.
Delphi panel
All members of the SC were consulted to nominate Delphi panelists, taking into consideration a number of factors: (1) balancing experienced Delphi panelists with new panelists; (2) representing chiropractic and other professionals involved in health care for children; (3) representing both practitioners who specialize in chiropractic pediatrics and “generalist” practitioners; (4) including experts in research and academics as well as practitioners. Panelists were based on their practice characteristics (provided in a form accompanying their nomination as a panelist) and their Curriculum Vitae; they were invited to participate after approval by the SC.
Rating of seed statements in modified Delphi process
We used the RAND/University of California at Los Angeles (RAND-UCLA) methodology for modified Delphi processes for rating the appropriateness of the described procedure. [34] It “generally involves multiple rounds, in which a questionnaire is sent to a group of experts who answer the questions anonymously. The results of the survey are then tabulated and reported back to the group, and each person is asked to answer the questionnaire again. This iterative process continues until there is a convergence of opinion on the subject or no further substantial changes in the replies are elicited.” [34](p. 6)
As per the standard methodology, panelists rated each seed statement using an ordinal scale of 1–9 (highly inappropriate to highly appropriate). [34] Instructions were to rate the statements as [34]:
“Appropriateness” is defined by the RAND-UCLA methodology as meaning that the patient's expected health benefit is greater than any expected negative consequences by a sufficiently wide margin that it is worth doing, without considering cost. [34] If panelists intended to rate a statement as inappropriate (rating 1–3), we required them to provide a reason and, if possible, cite peer-reviewed articles in support. We considered this necessary for the SC to make an evidence-informed revision of the statement and accurately represent the panel's input. If the panelist did not supply a reason, we considered the response a missing value. Delphi panelists were provided with all supporting citations; upon request, they were provided with the full-text documents.
Modified Delphi rounds, rating system, and data analysis
The project coordinator entered all numerical response data into an SPSS file for analysis (median and percent agreement). She entered text data (comments) into a Word table, organized by panelist identification number (ID), statement ID, and rating. All data, both numeric and text, were identified only by a code number when circulated to the panelists and the SC. The project director collapsed the 1–9 scale into three categories, “inappropriate” (1–3), “undecided” (4–6), and “appropriate (7–9), and analyzed this frequency data for the median rating and percent agreement. Statements not reaching 80% agreement for appropriateness (i.e., ratings 7–9) were revised by the SC, based upon the panelists' comments, and were recirculated until the panel reached at least 80%
Results
Literature search
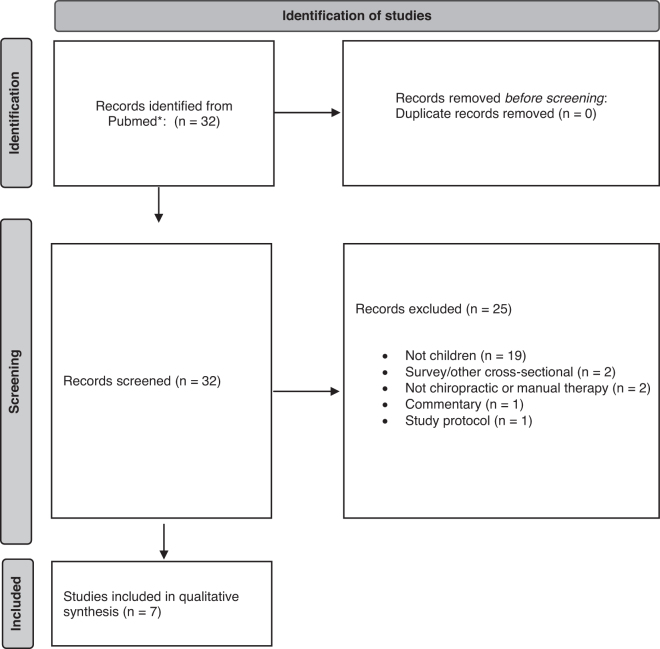
Figure 1
page 7

Table 6
page 8

Table 7
page 9Safety literature search The PubMed safety search (covering the period July 1st 2019–January 31st 2022) yielded 32 studies, with 25 excluded, as detailed in Figure 1 (excluded studies are listed in Supplementary materials) The remaining seven studies are detailed in Table 6. [8, 35–40]
Quality assessment
Table 7 lists the CPGs, systematic reviews, and narrative reviews rated for quality. Other study designs were considered lower-level evidence and were not rated. Seven of the eight guidelines were rated as high quality [41–47]; one was not rated because two of the investigators on this project were authors, and it was used as a seed document for information about health promotion and disease prevention. [20] Of the four systematic reviews, three were rated as high quality [48–50] and one as acceptable. [12] Of the four narrative reviews, three were rated as high quality [16, 48, 51] and one as acceptable. [52]
Delphi panel characteristics
Of the 60 panelists, 65% (39) were female, and 35% (21) were male. All but two were of white/Caucasian ethnicity; one reported as Asian/Pacific Islander, and one multi/biracial. All 60 were chiropractors; 1 was also a physiotherapist, and 1 was also a massage therapist. Five had additional Master's degrees, and 4 also had PhDs. The mean years practicing in their profession was 22 (range, 1–53 years). In terms of geography, 55% (33) were from Australia (6 of 6 states: NSW, QLD, SA, TAS, WA, VIC); 28% (17) were from the U.S. (13 of 50 states: AZ, CA, FL, IA, IL, MO, MS, MN, NY, OK, OR, TX, WA); and 17% (10) were from countries other than Australia and the U.S.: Denmark, England, Ireland, Malaysia, New Zealand, and South Africa. Nine panelists were faculty at a chiropractic institution, 3 at a nonchiropractic institution, and four at a chiropractic program within a nonchiropractic institution. Fifty-five percent (33) had some type of postgraduate certification in pediatrics.
For the 53 panelists who are practicing clinicians, their mean years in practice was 22 (range, 1–43 years); the mean number of estimated pre-COVID (coronavirus disease 2019) patients per week was 89 (range, 0–280); and mean estimated percent of those patients who were under age 18 was 39% (range, 0%–100%).
Delphi process
The Delphi process was conducted June to August 2022. In the first round, 66 of the 70 seed statements reached at least 80% consensus. In the second round, 2 of the 4 revised statements from Round 1 reached 80% consensus. In the third round, the last two statements reached consensus. All 60 panelists participated in each of the 3 rounds, although 3 declined to be acknowledged.
Seed statements
The following are the recommendations for best practices for chiropractic care for childrenIntroduction
In1. The purpose of these recommendations is to ensure the health and safety of chiropractic patients under 18 years of age by identifying the components of the most appropriate clinical approach to chiropractic care in the pediatric age group.
In2. Weigh the potential benefits of an intervention against potential health risks and financial and/or time costs. [53–55]
In3. Consider the anatomical, physiological, developmental, social, and psychological differences between children and adults to determine the application and appropriateness of health care evaluation and interventions. [22, 56, 57]
Patient communicationCO1. Gather relevant clinical information during the case history of a child using a flexible approach to establish rapport while collecting information. [22, 56, 58]
CO2. Communicate in an age- and developmentally appropriate manner to help a child actively engage in the clinical encounter [56, 58] as much as possible, incorporating relevant strategies and use of resources (using words, signs, or toys) to help a child feel at ease. [4, 59–61]
CO3. During treatment, be sensitive to the child's cues when they communicate feelings (examples: fear, pleasure) or sensations (examples: ticklish, pain). [59, 60]
CO4. In pediatric practice it is important to establish trust and rapport with both parents/caregivers and the child during the clinical encounter in a safe, inclusive, and nonjudgmental environment. [62] This requires not only sensitivity to the language being used but also the nonverbal elements of the exchange. [56, 59, 60]
CO5. Be sensitive to cultural, religious, and gender considerations in patient dialog to optimize reaching an appropriate diagnosis, designing an effective and safe treatment plan and gaining consent for the mutually agreed plan. [63]
Informed consentIC1. Ensure that an informed consent process is completed with the parent/guardian and the child if age- and developmentally appropriate before initiating any assessment, examination, or treatment. Obtain a signed informed consent form from the parent or legal guardian and document it in the patient's record. The informed consent process consists of explaining the recommended care, including benefits, potential risks, and alternative treatment options. [56]
IC2. Explain procedures in clear and simple terms; answer both the parent/guardian's and child's questions, to ensure that their consent is fully informed and voluntary.56
IC3. Obtain verbal consent from the child, if developmentally appropriate. [61]
IC4. Explain the diagnosis and prognosis to the parent/guardian and child in age-appropriate, understandable wording. [56]
IC5. Explain the proposed management/treatment plan and any possible risks, benefits, financial costs, and alternative treatment options (including natural history).51 When suggesting treatments for which current evidence is not definitive, refer to the “Chiropractic Management of Pediatric Patients” section below for specific language to explain such to parents/guardian. [8, 56]
IC6. Consent should be freely given without coercion or pressure. [64]
IC7. Explain that the patient, parent, or guardian may withdraw consent at any time.
IC8. Provide the patient/parents with opportunities to ask questions at all stages of the informed consent, discussion of treatment options, assessment/examination, and treatment.
Clinical historyHE1*. In a comprehensive case history at the initial visit, include a review of systems, developmental milestones, family history, health care history, concurrent health care and medication use. [56, 58] Specific items include [65]:
Onset of pain/symptoms
Mechanism of injury or trauma
Symptom parameters (timing, location, quality, frequency, intensity, duration, and radiation)
Family history of relevant conditions
Social/behavioral health history (such as activities, social/emotional stress, conflicts or abuse; depression, including suicidal ideation; gender identity) [63]
Intellectual and/or behavioral difficulties, including presence of learning difficulties, attention-deficit/hyperactivity disorder (ADHD/ADD) and autism spectrum traits. Determine the relevance and effect of these difficulties on consent, history taking, delivery of treatment, and the type/style of treatment
Growth, physical development, and milestones
Health care history, including current and previous treatment for presenting complaint
HE2*. Elicit information on general health habits, including breastfeeding, diet, and dietary issues such as eating disorders, [66] sleep, physical activity, and injuries.
HE3*. Review relevant prenatal events, including the health of the mother, as well as a review of the birth history (e.g., gestational age, birthweight, perinatal complications). [56]
HE4*. Obtain case history information from the child, if possible, to assist in developing an appropriate management plan. [61]
Physical examinationPE1. Use clinically relevant and valid examination procedures to move from a working diagnosis, which is based on the history, to a short list of differential diagnoses. [22, 56, 58, 65]
PE2. Assess vital signs pertinent to their health and chief complaints in an age-appropriate manner as part of the initial examination and at reassessment intervals. [56, 58]
PE3. Be familiar with the World Health Organization (WHO) growth charts (for children up to age 2) and CDC growth charts (children 2 years and older) and use when clinically applicable to monitor growth.
PE4. Refer any necessary diagnostic or examination procedures outside the chiropractors' clinical skills, scope of practice, or experience to an appropriately qualified health professional with whom to coordinate care. [1]
PE5. The neuromusculoskeletal examination should include [65]:
Inspection and palpation for lesions, pain source, or masses
Developmentally appropriate assessment of movement and gait
Range of motion assessment of the spine and extremities, as relevant
Assessment of joint motion as relevant Orthopedic and neurologic evaluation
Postural assessment
Assessment of organ systems when indicated such as eyes, ears, nose, throat, heart, lungs, and abdomen.
PE6. Conduct an age-appropriate developmental assessment, which, depending on clinical relevance, may include: balance and gait, fundamental developmental milestones, cranial nerve examination, [22, 56, 58, 65, 67] muscle tone, primitive reflexes, postural reflexes, and gross and fine motor development. [68]
PE7. Refer children with possible developmental delay for further assessment as necessary. [69]
Red flags in pediatric patients

Table 8
page 10RF1. If the history and/or examination reveal “red flags” indicating serious conditions, refer the child to an appropriate provider for further diagnosis and/or care (Table 8). [22, 56, 58, 65]

Diagnostic imagingDI1. Consider referral for radiographic examination in the presence of a history of trauma, suspicion of serious pathology, and/or positive results of screening assessment of scoliosis. [52, 65]
DI2. In the absence of red flags, do not use routine or repeat radiographs for the evaluation of the structure and function of the spine. [52, 70]
DI3. Where there are indicators of pathology or conditions that warrant further investigation, appropriate referral for assessment should be made in a timely manner. [65]
Chiropractic management of pediatric patients
(See specific recommendations for infants below)C1. There are four basic chiropractic management approaches to the care of a child: (1) sole management by a chiropractor, (2) independent concurrent care by a chiropractor and other provider(s), (3) comanagement with other appropriate health care providers, and (4) referral to another registered/licensed or certified health care provider/specialist. [1, 22, 42]
C2. Follow the principles of evidence-based practice, which are to make clinical judgments based on the best available evidence combined with clinical experience and the patient's preferences. [22, 56, 71, 72]
C3. Children may present to chiropractic practices with various conditions and developmental concerns not directly related to the neuromusculoskeletal system. There is a paucity of high-level research evidence for the effectiveness of spinal manipulation and/or chiropractic care for such conditions. [8, 12, 48, 49, 73] However, the absence of research evidence does not equate to evidence of absence and subsequent denial of care. [74]
C4. In the presence of concurrent neuromusculoskeletal issues, consider a therapeutic trial of chiropractic care, using treatment that has been widely and safely used [8, 16, 51, 75, 76] even when high-level research evidence is currently unavailable.C4a. Provide parents with the information they need for fully informed consent, including an explanation of supportive measures and collaboration with other health care providers to improve overall health and wellbeing.

Infant (children <1 year of age) assessment and treatment—
in addition to practices common to all childrenIA1. Assess or refer for assessment of the infant's ability to feed by breast or bottle by mother's report. It may include musculoskeletal assessment of cranial symmetry, temporomandibular and/or cervical joint and soft tissue function, as well as any distal site that could refer pain and may affect the infant's ability to feed. [77]
IA1a. Measure and record any cranial asymmetry as treatment plan progresses. [77, 78]
IA1b. Observe feeding or the infant's suckling to assess the integrity of oral motor function and make appropriate referrals as necessary for further intervention or neuromuscular reeducation. [79]IA2. Provide evidence-based advice and information about nutrition (breastfeeding or breast milk substitute). [80]
IA3. Support and encourage parent/infant bonding while providing assessment and treatment because early bonding and attachment are important for development and long-term health. [79, 81–83]
IA4. Provide evidence-based advice on safe sleeping for infants. [84]
IA5. Communicate with, comanage with and/or refer infants with disabilities to appropriate providers for more extensive treatment and comanagement. [1]
Manual procedures
There are special considerations for use of spinal manipulation and other manual procedures with children. [1, 8, 16, 51, 75, 76]SO. Modify manipulative and/or mobilization and soft tissue techniques as appropriate for the child's age and developmental stage. [12, 16]
SO. Patient preferences: Adapt manipulation and soft tissue procedures for the individual child's needs and comfort.
Sa. Patient size: Modify biomechanical force in proportion to the age and developmental stage of the child.
Sb. Structural development: Modify manual procedures to ensure the safety of the developing skeleton.
Sc. Flexibility of joints: Take into account the greater flexibility and lesser muscle mass of children, using gentler and lighter manual procedures.

Co-management and referralCM1. Establish communication and, if possible, collaborative relationships with the child's other healthcare providers in order to effectively and safely co-manage pediatric complaints. [1]
CM2. Establish co-management with other health care providers as appropriate, including but not restricted to: [1, 25]
CM2a. The child is not showing clinically significant improvement after an initial trial of chiropractic care.
CM2b. The parents of the child request such a co-management approach.
CM2c. There are significant co-morbidities that are outside the scope of chiropractic practice.
CM2d. When ordering diagnostic imaging or laboratory studies, forward copies of the results to the child's primary provider for coordination of care, if requested/authorized by the parent/caregiver.
CM2e. Consider co-management of non-musculoskeletal conditions with the child's primary care provider and/or other providers.
CM2f. Immediately refer to the appropriate medical specialist when the case history or examination reveal any “red flags” suggestive of serious pathology. A list of these red flags is shown in Figure 1, end of document.

Health promotion and disease preventionPrimary prevention
PP1. Well child visits are an established aspect of pediatric health care and may be indicated for the purpose of health promotion and clinical assessment of asymptomatic pediatric patients. [22]
PP2. Emphasize disease prevention and health promotion through counseling on physical activity, nutrition, injury prevention, and a generally healthy lifestyle. [20] These health promotion principles may be addressed through the course of care, and include but are not limited to:
Adequate age-appropriate physical activity
Adequate sleep
Decreased screen time, such as television, mobile/cell phones, electronic games, and computer use
Healthy diet
Healthy social relationships
Injury prevention
Substance use or abuse prevention (such as caffeinated beverages, alcohol, tobacco, [44] vaping, marijuana, steroids, and other prescription or illicit drugs). Provide and discuss age-appropriate, readily accessible cessation materials.
PP3. Screen children ages 2–18 years for obesity and offer them lifestyle and dietary advice or consider referring them to a qualified provider for appropriate interventions. [46, 85]
PP4. If parents ask about sun exposure for their children, provide them with information from authoritative sources on minimizing exposure to ultraviolet (UV) radiation while maintaining safe exposure for the desirable benefits related to Vitamin D. [45, 86, 87]
PP5. If parents ask for advice or information about childhood vaccinations, explain that they have the right to make their own health decisions. They should be adequately informed about the benefits and risks to both their child and the broader community associated with these decisions. Consider referral to a health professional whose scope of practice includes vaccinations to address patient questions or concerns. [20] (See Chiropractic Board of Australia position statement).
Secondary prevention—screeningSP1. If parents ask, or if relevant to presenting complaint, provide them with access to resources on correct use of seat belts, car seats, and infant seats, such as those provided by local and national public health agencies. [88, 89]
SP2. Any tests or procedures used for public screenings should be based on recognized evidence of their benefit for disease prevention and health promotion. [28]
Adolescent idiopathic scoliosisAI1. Screen children for scoliosis; idiopathic scoliosis is more commonly discovered during a child's growth spurt (10 to 15 years old) using established tests, including forward bend test, Scoliometer, Humpometer, plumb line test, or Moiré topography. [41, 43, 90]
AI2. Refer patients with positive results of scoliosis screening for appropriate imaging examination. [52, 65]
AI3. Although there is currently no evidence for effectiveness of spinal manipulation (SMT) on progression or improvement in curvature, evidence is insufficient but favorable for its effectiveness for pain for some adolescents (ages 13–17) with scoliosis. Therefore, consider the risks and benefits of a therapeutic trial of SMT. [50]
Recognition of family and domestic violence, including child abuse and neglectFV1. Be alert for signs of family and domestic violence (FDV), including possible child abuse or neglect. These include but are not limited to physical injury, chronic pain, depression, and posttraumatic stress disorder. [47, 56, 58, 91, 92]
FV2. Pay particular attention to injuries in various stages of healing and explanations for the injuries being either lacking or incongruous. [56, 58, 93]
FV3. Where FDV is suspected affecting the welfare of a child, it is necessary to notify the appropriate services. [56, 58, 93]
FV4. If warranted, refer the family to an appropriately trained mental health practitioner and/or provide access to a resource kit with a list of information and support services. [56, 58, 93]
Discussion
The media and fringe medical advocates have sometimes presented the impression that chiropractic care of children, especially infants, has serious safety concerns and an absence of effectiveness. [94] Indeed, the impetus for this Delphi project was recommendation 6 (p7) of a government inquiry conducted in the Australian state of Victoria in 2019 as a result of media interest.
Consequently, an international, interdisciplinary team, including many with prior experience in formulating best practice guidelines was convened with logistical and financial support from several peak bodies representing the chiropractic profession. This comprehensive Delphi process spanned over 2 years.
The 2009 and updated 2016 recommendations constituted a logical launching point for the project. Due to the robust nature of the original documents, there was little substantive change in many statements with the exception of the sections on health promotion, secondary prevention, and recognition of FDV. Since the SCV inquiry was precipitated around concerns of safety of SMT with children under 12, this review included a deep search for reports of AEs associated with manual care of pediatric patients. Consistent with the SCV inquiry, this study confirmed the rarity of published examples of AEs associated with SMT and manual care.
This Delphi consensus process followed standard methodology by forming an interdisciplinary SC, which included consumers consistent with best practice protocols to evaluate the contemporary literature. The volume of evidence available to clinicians presents a significant challenge since it is not feasible for busy clinicians to review primary research literature routinely. [95] Thus, CPGs and best practice documents communicate “preprocessed” evidence-based recommendations to clinicians. Where insufficient evidence is available to give graded recommendations, guidelines may offer “consensus-based” recommendations. [96, 97]
The guidance statements in this document can primarily form the basis of written information for parents, advising them of proposed benefits and potential risks of intended care. Regulators, practicing chiropractors who treat children, other health care providers, educators, third-party payers, and the general public will also find the content informative and instructive.
These best practices serve also as a scaffold for practitioners who wish to acquire additional knowledge to appropriately care for pediatric subgroups by progressing to postgraduate advanced training or continuing education coursework.
Other health care providers who care for children in collaboration with chiropractors will benefit through enhanced understanding of the nature, scope, and expectations of the pediatric chiropractic encounter. This can lay a foundation for mutual referral and cooperation in the best interest of the children who consult chiropractors.
Health insurers and third-party payers increasingly seek evidence to inform decisions about their medical policies and benefits. Often lacking in this process are the resources and skills needed to synthesize the scientific literature and to gather input from the providers and consumers most affected by their policy decisions. This document represents such a resource.
Strengths and limitations
A strength of this international project was the involvement of consumers from the initial phase of design through to publication. Approaches that give consumers specific roles or engage them in a formal structure such as a SC [98] or that enable consumers to set the agenda, develop a shared mission and purpose statements and participate in most stages of the planning, administration, and evaluation make consumer participants feel comfortable with the team and process, maintain consumer involvement throughout the process, and improve the quality of outcomes. [98–104]
We had unprecedented input from consumers through the SC, and we were also able to draw on the consumer submissions that formed an important part of the SCV report. The SC had interdisciplinary expertise from medicine, medical pediatrics, nursing, lactation consultancy, massage, social work, psychology, family therapy, mental health, academics, researchers, and clinicians on both the SC and Delphi panels.
Limitations
Due to the continuing substantial gaps in the evidence for the effectiveness of SMT care of children, it was important to develop a set of evidence-informed recommendations that are the result of expert opinion achieved through a rigorous consensus process. However, the gaps in the evidence base still represent a limitation to these recommendations because expert consensus is a lower form of evidence to be relied on principally when higher levels of evidence are lacking. It is possible that our limited literature search may have missed relevant citations; however, it is noteworthy that most clinical interventions lack high-quality supportive evidence. [105]
Our recommendations primarily deal with the “typical” patient care journey through history, examination, and management and are not designed to exhaustively cover all possible services chiropractic practitioners may provide for children. We also provided only limited recommendations related to specific childhood age groups; although we discussed infants as a subsection, it was beyond our scope to provide specific guidance for other pediatric age groups (such as toddlers, elementary school, or adolescents).
Another limitation of a study based on consensus is that it is possible that the panelists do not fully represent the general population of chiropractic experts. We did not conduct searches on effectiveness for individual childhood conditions as we adopted the position that delivery of care should be defendable rather than decisive. [13] Lastly, we did not seek formal input from organizational stakeholders representing educators, third-party payers, legislative bodies, or nonmanual care pediatric organizations. We did not provide any specific recommendations about age-appropriate treatment dosage, frequency, and duration, which were beyond this project's scope.
Acknowledgements
The authors want to thank Cathy Evans for her superlative work as project coordinator. They thank Nathan Hinkeldey, DC, for his valuable assistance in rating the quality of the evidence. The authors would also like to thank all the Delphi panelists for so generously contributing their expertise and time to the arduous work of the Delphi process: Cassie Atkinson-Quinton, BHSc(Chiro), MClinChiro, DACNB; Laura Baffes, BS, DC, CCSP; Charles L. Blum, DC; Jennifer Brocker, DC, DICCP; Jerrilyn Cambron, DC, PhD; Beth Carleo, BS, DC; Elizabeth Conlon, BHSc(Chiro), MClinChiro; Rachel Cripps, BSc(Hons), MSc(Chiro), MSc(Ped); Rachael Davie, BHSc, BAppSc(Chiro); Jason d'Hotman de Villers, MTech(Chiro), MSc(Chiro), MSc(Ped); Mark Dehen, DC, FICC; Kerri Elston Doherty, BA(Hons), DC; Matthew Doyle, MSc(Ped), MSc(Chiro), BAppSc, BChiroSc, BSc, Fellow Pediatric Chiropractor (AICE); Susan Ferguson, BAppSc(Chiro), Pediatric Chiropractor (AICE); Christian J. Fludder, BChiroSc, MChiro; Karen Forsyth, BAppSc(Clin), BChiroSc, MSc(Ped), Pediatric Chiropractor (AICE); Adoni Fotopoulos, BSc, MChiro; Pamela S. Gindl, DC, DICCP; Olivia Gleeson, BAppSc(Clin), BChiroSc; Paul J. Greteman, DC, DICCP; Samantha Haitsma, BChiro; Jan Hartvigsen, DC, PhD; Navine Haworth, DC, DICCP, GCTTL, PhD; Lise Hestbaek, DC, PhD; Elise G. Hewitt, DC, DICCP, FICC; Rosemary Keating, BAppSc(Chiro), MChiroSc(Ped), Pediatric Chiropractor (AICE); Braden Keil, BAppSc(Chiro), MChiroSc(Ped); Lauren Kinnane, BHSc(Chiro), MClinChiro; Charmaine Korporaal, MTech(Chiro), CCFC, CCSP, ICSSD; Ann Langford, DC, DICCP; Monique Lawless, BHSc(Chiro), MClinChiro; Chiara Layton, BHSc(Chiro) BAppSc(Chiro); Robert Leach, DC, MS, MCHES; Twink Lim, DC; Glenn Maginness, BAppSc(Chiro), MChiroSc(Ped); Haley Maginness, BHSc(Chiro), MClinChiro; Mike Marinus, MTech(Chiro), MSc(Ped); Troy Miles, BChiroSc, BAppSc(Clin); Rory Murphy, BChiroSc; Kenneth Parker, BAppSc(Chiro); Katie Pritchard, BSc, BChiro; Melinda Ricci, BSc(Chiro), BChiro(Hons); Joanne Sexton, BAppSc(Clin), BChiroSc; Vassilios Stathoulis, BSc, MChiro, Pediatric Chiropractor (AICE); Troy Sturgill, DC, MS; Mary Unger-Boyd, DC, DICS, CACCP; Michelle Van Doorn, BSc(Neuro), BSc(Chiro), BChiro; Meghan Van Loon, PT, DC, DICCP; Carla Vescio, BHSc(Chiro), MClinChiro; Susan Wenberg, DC, MA; Polly Wilkie, BSc(Anatomy), MChiro, Grad. Dip Exercise and Sports Sciences, Adv. Dip Nutritional Medicine; Kaitlin Williams, BAppSc(Clin), BChiroSc; Steve Williams, DC, DICS, FICS, FRCC(Ped), FBCA; Mikaela Wilson, BHSc(Chiro), BAppSc(Chiro); Beau L. Woods, BChiroSc, MPH; Alison Young, BChiroSc, BAppSc(Chiro), MSc(Ped); Morgan Young, DC.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
This project was supported in part by the Aus-ACA, the American Chiropractic Association (Council on Chiropractic Pediatrics), and the Clinical Compass. Also represented were the Australasian Institute of Chiropractic Education (AICE) and the ICA. One SC member (R.T.) has a private lactation consultancy. The project director (C.H.) was partially supported by the Aus-ACA, the American Chiropractors Association, the Clinical Compass, Texas Chiropractic College, and the NCMIC Foundation. However, the funding sources of the project had no influence on any aspect of the study beyond representation on the SC or Delphi Panel. The research reported in this study is the sole responsibility of the authors and reflects the independent ideas of the authors as the SC and the Delphi panelists. None of the organizations listed requested access, approved, or influenced any part of the deliberations, including the final version of the statements or any draft of the article before publication.
Disclaimer:
References:
Vallone SA, Miller J, Larsdotter A, et al..
Chiropractic Approach to the Management of Children
Chiropractic & Osteopathy 2010 (Jun 2); 18: 16Adams J, Peng W, Cramer H, et al..
The Prevalence, Patterns, and Predictors of Chiropractic Use Among
US Adults: Results From the 2012 National Health Interview Survey
Spine (Phila Pa 1976) 2017 (Dec 1); 42 (23): 1810–1816Dice JL, Dendy D, Sizer PS, et al..
Manual therapy in preadolescent children: A delphi investigation
of physical therapists in the United States.
Phys Ther 2021;101(4):pzab027;
doi: 10.1093/ptj/pzab027Black LI, Clarke TC, Barnes PM, et al..
Use of complementary health approaches among children aged
4–17 years in the United States: National Health
Interview Survey, 2007–2012.
Natl Health Stat Report 2015;78:1–19Adams J, Peng W, Steel A, et al..
A cross-sectional examination of the profile of chiropractors recruited
to the Australian Chiropractic Research Network (ACORN):
A sustainable resource for future chiropractic research.
BMJ Open 2017;7(9):e015830;
doi: 10.1136/bmjopen-2017-015830ABS. 4364.0.55.002
Health Service Usage and Health Related Actions, Australia, 2014–2015.
In: Statistics ABS. Commonwealth of Australia:
Canberra; 2017; https://shorturl.at/cegyVBeliveau PJH, Wong JJ, Sutton DA, et al..
The Chiropractic Profession: A Scoping Review of Utilization Rates,
Reasons for Seeking Care, Patient Profiles, and Care Provided
Chiropractic & Manual Therapies 2017 (Nov 22); 25: 35Corso M, Cancelliere C, Mior S, et al..
The safety of spinal manipulative therapy in children under 10 years:
A rapid review.
Chiropr Man Ther 2020;28(1):12;
doi: 10.1186/s12998-020-0299-ySafer Care Victoria.
Chiropractic Spinal Manipulation of Children Under 12. 2019. Available from: https://www.bettersafercare.vic.gov.au/report
s-and-publications/chiropractic-spinal-manipulation-of-children-under-12 [Last accessed: August 22, 2020].Keating GM.
Parent reports of chiropractic care for children:
A preliminary report from 22,043 parents in Australia
J Clinical Chiropractic Pediatrics 2021; 20 (1): 1731–1732Keating GM.
Do Children in Australia Benefit from Chiropractic Care?
[Dissertation]. 2021.
ProQuest: The School of Psychology.
Fielding Graduate University: Santa Barbara, CA;
https://shorturl.at/blNW2Green S, McDonald S, Murano M, et al..
Systematic Review of Spinal Manipulation in Children.
In: Cochrane Australia for Safer Care Victoria:
Victoria, Australia; 2019; https://shorturl.at/grJK7Keating GM, Amorin-Woods LG.
Commentary on the 2019 Safer Care Victoria review of
chiropractic spinal manipulation of children under 12 years
Chiropr J Aust 2023; 50 (1): 1–28Swait G, Finch R.
What Are the Risks of Manual Treatment of the Spine?
A Scoping Review for Clinicians
Chiropractic & Manual Therapies 2017 (Dec 7); 25: 37Chu EC, Trager RJ, Lee LY, et al..
A retrospective analysis of the incidence of severe adverse events
among recipients of chiropractic spinal manipulative therapy.
Sci Rep 2023;13(1):1254;
doi: 10.1038/s41598-023-28520-4Todd AJ, Carroll MT, Mitchell EKL.
Forces of Commonly Used Chiropractic Techniques
for Children: A Review of the Literature
J Manipulative Physiol Ther. 2016 (Jul); 39 (6): 401–410Amorin-Woods LG, Woods BL, Moore CS, et al..
Research priorities of the Australian chiropractic profession:
A cross-sectional survey of academics and practitioners.
J Manipulative Physiol Ther 2022;45(1):73–89;
doi: 10.1016/j.jmpt.2022.03.015Amorin-Woods LG. Parkin-Smith GF, Woods BL, et al.
Show Me The Money! Personal perspectives, capacity and research funding
within the Australian chiropractic profession:
Results of a nationwide survey.
J Contemp Chiropr. 2022;5(1):114–129;
https://journal.parker.edu/index.php/jcc/article/view/208CCEA. CCEA Accreditation and Competency Standards 2017.
Available from:
https://static1.squarespace.com/static/619ad68aad4524745de58b0d/t/
61b68e4f58b763415445f387/1639353947256/CCEA_Accreditation_and_
Competency_Standards_2017.pdf
[Last accessed: November 23, 2019].Hawk C, Amorin-Woods LG, Evans MwJr., et al..
The Role of Chiropractic Care in Providing Health Promotion
and Clinical Preventive Services for Adult Patients with
Musculoskeletal Pain: A Clinical Practice Guideline
J Altern Complement Med 2021 (Oct); 27 (10): 850–867Hawk, C, Schneider, M, Ferrance, RJ, Hewitt, E, Van Loon, M, and Tanis, L.
Best Practices Recommendations for Chiropractic Care for Infants,
Children, and Adolescents: Results of a Consensus Process
J Manipulative Physiol Ther. 2009 (Oct); 32 (8): 639–647Hawk C, Schneider M, Vallone S, Hewitt E.
Best Practices for Chiropractic Care of Children:
A Consensus Update
J Manipulative Physiol Ther. 2016 (Mar); 39 (3): 158–168Moore KM, Amorin-Woods D, Amorin-Woods LG, et al..
A cross-sectional study of Australian chiropractors' and students' readiness
to identify and support patients experiencing intimate partner violence.
J Chiropract Educ 2023;37(1):71–81;
doi: 10.7899/JCE-21-45Alcantara J, Ohm J, Kunz D.
The Safety and Effectiveness of Pediatric Chiropractic:
A Survey of Chiropractors and Parents in a
Practice-based Research Network
Explore (NY) 2009 (Sep–Oct); 5 (5): 290–295April KT, Feldman DE, Zunzunegui MV, et al..
Complementary and alternative health care use in young children with
physical disabilities waiting for rehabilitation services in Canada.
Disabil Rehabil 2009;31(25):2111–2117; doi: 10.3109/09638280902937407Becker M, Neugebauer EA, Eikermann M.
Partial updating of clinical practice guidelines often makes more sense
than full updating: A systematic review on methods
and the development of an updating procedure.
J Clin Epidemiol 2014;67(1):33–45;
doi: 10.1016/j.jclinepi.2013.06.021Shekelle P, Woolf S, Grimshaw JM, at al.
Developing clinical practice guidelines: Reviewing, reporting, and publishing
guidelines; updating guidelines; and the emerging issues of enhancing
guideline implementability and accounting for comorbid
conditions in guideline development.
Implement Sci 2012;7:62;
doi: 10.1186/1748-5908-7-62U. S. Preventive Services Task Force.
A and B Recommendations. USPSTF;
Rockville, MD; 2022; https://shorturl.at/uBL67CDC.
Health Topics A-Z.
Atlanta, GA, USA; 2022;
https://www.cdc.gov/health-topics.html.Speckemeier C, Krabbe L, Schwenke S, et al..
Discrete choice experiment to determine preferences of decision-makers
in healthcare for different formats of rapid reviews.
Syst Rev 2021;10(1):121;
doi: 10.1186/s13643-021-01647-zBrouwers MC, Kho ME, Browman GP, et al..
The Global Rating Scale complements the AGREE II in
advancing the quality of practice guidelines.
J Clin Epidemiol 2012;65(5):526–534;
doi: 10.1016/j.jclinepi.2011.10.008Harbour R, Lowe G, Twaddle S.
Scottish Intercollegiate Guidelines Network:
The first 15 years (1993–2008).
J R Coll Physicians Edinb 2011;41(2):163–168;
doi: 10.4997/JRCPE.2011.209Baethge C, Goldbeck-Wood S, Mertens S.
SANRA—A scale for the quality assessment of narrative review articles.
Res Integr Peer Rev 2019;4(1):5;
doi: 10.1186/s41073-019-0064-8Fitch K, Bernstein S, Aquilar MS, et al..
The RAND/UCLA Appropriateness Method User's Manual
RAND Corporation: Santa Monica, CA; 2003;Ellwood J, Draper-Rodi J, Carnes D.
Comparison of common interventions for the treatment of infantile colic:
A systematic review of reviews and guidelines.
BMJ Open 2020;10(2):e035405;
doi: 10.1136/bmjopen-2019-035405Ellwood J, Draper-Rodi J, Carnes D.
The effectiveness and safety of conservative interventions for positional
plagiocephaly and congenital muscular torticollis:
A synthesis of systematic reviews and guidance.
Chiropr Man Therap 2020;28(1):31;
doi: 10.1186/s12998-020-00321-wGhanim MT, Bergmann S, Turner RD, et al..
Recurrent stroke in a child with atlantoaxial instability
following chiropractic manipulation.
J Pediatr Hematol Oncol 2020;42(6):e518–e520;
doi: 10.1097/MPH.0000000000001559Paknejad MS, Motaharifard MS, Barimani S, et al..
Traditional, complementary and alternative medicine in
children constipation: A systematic review.
Daru 2019;27(2):811–826;
doi: 10.1007/s40199-019-00297-wPohlman KA, Carroll L, Tsuyuki RT, et al..
Comparison of active versus passive surveillance adverse event reporting
in a paediatric ambulatory chiropractic care setting:
A cluster randomised controlled trial.
BMJ Open Qual 2020;9(4):e000972;
doi: 10.1136/bmjoq-2020-000972Vos B, Rake JP, Vlieger A.
Adverse events associated with pediatric complementary and
alternative medicine in the Netherlands:
A national surveillance study.
Eur J Pediatr 2021;180(7):2165–2171;
doi: 10.1007/s00431-020-03899-8Grossman DC, Curry SJ, Owens DK, et al..
Screening for adolescent idiopathic scoliosis: US preventive
services task force recommendation statement.
JAMA 2018;319(2):165–172;
doi: 10.1001/jama.2017.19342Haldeman S, Johnson CD, Chou R, et al..
The Global Spine Care Initiative: Care Pathway
for People With Spine-related Concerns
European Spine Journal 2018 (Sep); 27 (Suppl 6): 901–914Negrini S, Donzelli S, Aulisa AG, et al..
2016 SOSORT guidelines: Orthopaedic and rehabilitation
treatment of idiopathic scoliosis during growth.
Scoliosis Spinal Disord 2018;13:3;
doi: 10.1186/s13013-017-0145-8Sargent JD, Unger JB, Leventhal AM.
Recommendations from the USPSTF for prevention and cessation
of tobacco use in children and adolescents.
JAMA 2020;323(16):1563–1564;
doi: 10.1001/jama.2019.22312U. S. Preventive Services Task Force, Grossman DC, Curry SJ, et al.
Behavioral counseling to prevent skin cancer:
US preventive services task force recommendation statement.
JAMA 2018;319(11):1134–1142;
doi: 10.1001/jama.2018.1623US Preventive Services Task Force.
Screening for Obesity in Children and Adolescents:
US Preventive Services Task Force Recommendation Statement.
JAMA 2017;317(23):2417–2426;
doi: 10.1001/jama.2017.6803WHO.
Preventing Child Maltreatment: A Guide to Taking Action
and Generating Evidence.
Geneva; 2006;
https://apps.who.int/iris/handle/10665/43499Driehuis F, Hoogeboom TJ, Nijhuis-van der Sanden MWG, et al..
Spinal manual therapy in infants, children and adolescents:
A systematic review and meta-analysis on treatment
indication, technique and outcomes.
PLoS One 2019;14(6):e0218940;
doi: 10.1371/journal.pone.0218940Parnell Prevost C, Gleberzon B, Carleo B, et al..
Manual Therapy for the Pediatric Population:
A Systematic Review
BMC Complement Altern Med. 2019 (Mar 13); 19 (1): 60Théroux J, Stomski N, Losco CD, et al..
Spinal Manipulative Therapy for Adolescent Idiopathic Scoliosis:
A Systematic Review
J Manipulative Physiol Ther. 2017 (Jul); 40 (6): 452–458Todd AJ, Carroll MT, Robinson A, et al..
Adverse Events Due to Chiropractic and Other Manual Therapies
for Infants and Children: A Review of the Literature
J Manipulative Physiol Ther. 2015 (Nov); 38 (9): 699–712Jenkins HJ, Downie AS, Moore CS, et al..
Current evidence for spinal X-ray use in the
chiropractic profession: A narrative review.
Chiropr Man Ther 2018;26:48;
doi: 10.1186/s12998-018-0217-8Brozek JL, Akl EA, Alonso-Coello P, et al..
Grading quality of evidence and strength of recommendations in clinical
practice guidelines. Part 1 of 3. An overview of the GRADE approach
and grading quality of evidence about interventions.
Allergy 2009;64(5):669–677;
doi: 10.1111/j.1398-9995.2009.01973.xGuyatt GH, Oxman AD, Kunz R, et al..
Going from evidence to recommendations.
BMJ 2008;336(7652):1049–1051;
doi: 10.1136/bmj.39493.646875.AEGuyatt GH, Oxman AD, Vist GE, et al..
GRADE: An Emerging Consensus on Rating Quality of Evidence
and Strength of Recommendations
British Medical Journal 2008 (Apr 26); 336 (7650): 924–926Davies NJ.
Chiropractic Pediatrics.
Churchill Livingstone Elsevier:
Edinburgh; 2010.Huelke DF.
An overview of anatomical considerations of infants and
children in the adult world of automobile safety design.
Annu Proc Assoc Adv Automot Med 1998;42:93–113;Zitelli BJ, Nowalk MAJ.
Atlas of Pediatric Physical Diagnosis. 7th ed.
Elsevier: Philadelphia, PA; 2018.Bari A, Khan RA, Jabeen U, et al..
Analyzing communication skills of Pediatric Postgraduate
Residents in Clinical Encounter by using video recordings.
Pak J Med Sci 2017;33(6):1312–1317;
doi: 10.12669/pjms.336.13481Schnaith A, Schifsky J, Schifsky T, et al..
Communication strategies for patients who are nonverbal.
Pediatrics 2021;148(3):e2021051867;
doi: 10.1542/peds.2021-051867O'Reilly L, Dolan P.
The voice of the child in social work assessments:
Age-appropriate communication with children.
Br J Soc Work 2016;46(5):1191–1207;
doi: 10.1093/bjsw/bcv040Porges SW.
Polyvagal theory: A science of safety.
Front Integr Neurosci 2022;16:871227;
doi: 10.3389/fnint.2022.871227Townsend M, Clark BA.
Universal gender screening: A simple strategy to enhance
primary care for transgender and gender diverse people.
Fam Pract 2022;39(5):985–987;
doi: 10.1093/fampra/cmab176Australian Charter of Healthcare Rights, 2nd ed.
In. Sydney NSW Australia: ACSQHC; 2023;
https://www.safetyandquality.gov.au/our-work/partnering-
consumers/australian-charter-healthcare-rights/australian-
charter-healthcare-rights-second-editionKentar Y, Schwarze M, Pepke W, et al..
Pediatric back pain-diagnostic algorithm.
Orthopade 2022;51(1):36–43;
doi: 10.1007/s00132-021-04189-3Lebow J, Narr C, Mattke A, et al..
Engaging primary care providers in managing pediatric
eating disorders: A mixed methods study.
J Eating Disord 2021;9(1):11;
doi: 10.1186/s40337-020-00363-8Fasher M.
The 6 week check.
Aust Fam Phys 2012;41:288–290;
https://www.racgp.org.au/afp/2012/may/the-6-week-checkDuderstadt K.
Pediatric Physical Examination, 3rd Ed.
Elsevier: St, Louis, MO; 2018.National Center on Birth Defects and Developmental Disabilities.
Developmental Monitoring and Screening.
Centers for Disease Control and Prevention:
Atlanta, GA, USA; 2022.Corso M, Cancelliere C, Mior S, et al..
The clinical utility of routine spinal radiographs by
chiropractors: A rapid review of the literature.
Chiropr Man Ther. 2020;28(1):33;
doi: 10.1186/s12998-020-00323-8Johnson C.
Highlights of the basic components of evidence-based practice.
J Manipulative Physiol Ther 2008;31(2):91–92;
doi: 10.1016/j.jmpt.2008.01.001Sackett DL, Rosenberg WM, Gray JA, et al..
Evidence-Based Medicine: What It Is and What It Isn't
British Medical Journal 1996 (Jan 13); 312 (7023): 71–72DeMarsh S, Huntzinger A, Gehred A, et al..
Pediatric osteopathic manipulative medicine:
A scoping review.
Pediatrics 2021;147(2):e2020016162;
doi: 10.1542/peds.2020-016162Alderson P.
Absence of evidence is not evidence of absence.
BMJ 2004;328(7438):476–477;
doi: 10.1136/bmj.328.7438.476Marchand AM.
A Proposed Model With Possible Implications for Safety and
Technique Adaptations for Chiropractic Spinal Manipulative
Therapy for Infants and Children
J Manipulative Physiol Ther 2015 (Nov); 38 (9): 713–726Triano JJ, Lester S, Starmer D, et al..
Manipulation peak forces across spinal regions for
children using mannequin simulators.
J Manipulative Physiol Ther 2017;40(3):139–146;
doi: 10.1016/j.jmpt.2017.01.001Vallone SA.
Evaluation and Treatment of Breastfeeding Difficulties
Associated with Cervicocranial Dysfunction:
A Chiropractic Perspective
J Clinical Chiropractic Pediatrics 2016 (Dec); 15 (3): 1301Pastor-Pons I, Lucha-López MO, Barrau-Lalmolda M, et al..
Interrater and intrarater reliability of cranial
anthropometric measurements in infants with positional plagiocephaly.
Children 2020;7(12):306;
doi: 10.3390/children7120306Tow J, Vallone S.
Development of an integrative relationship in the care of the
breastfeeding newborn: Lactation consultant and chiropractor.
J Clin Chiropr Pediatr 2009;10:626–632;
https://shorturl.at/fk128World Health Organization.
Counseling for Maternal and Newborn Health Care.
World Health Organization: Geneva; 2013;
https://apps.who.int/iris/handle/10665/44016Phuma-Ngaiyaye E, Welcome Kalembo F.
Supporting mothers to bond with their newborn babies: Strategies used
in a neonatal intensive care unit at a tertiary hospital in Malawi.
Internat J Nurs Sci 2016;3(4):362–366;
10.1016/j.ijnss.2016.10.001 [CrossRef]Sullivan R, Perry R, Sloan A, et al..
Infant bonding and attachment to the caregiver:
Insights from basic and clinical science.
Clin Perinatol 2011;38(4):643–655;
doi: 10.1016/j.clp.2011.08.011Winston R, Chicot R.
The importance of early bonding on the long-term
mental health and resilience of children.
London J Prim Care 2016;8(1):12–14;
doi: 10.1080/17571472.2015.1133012Paavonen EJ, Saarenpää-Heikkilä O, Morales-Munoz I, et al..
Normal sleep development in infants:
Findings from two large birth cohorts.
Sleep Med 2020;69:145–154;
doi: 10.1016/j.sleep.2020.01.009Skinner AC, Ravanbakht SN, Skelton JA, et al..
Prevalence of obesity and severe obesity in US children, 1999–2016.
Pediatrics 2018;141(3):e20173459;
doi: 10.1542/peds.2017-3459Malacova E, Cheang PR, Dunlop E, et al..
Prevalence and predictors of vitamin D deficiency in a nationally representative sample of adults participating
in the 2011–2013 Australian Health Survey.
Br J Nutr 2019;121(8):894–904;
doi: 10.1017/S0007114519000151National Cancer Council of Australia.
Sun exposure and vitamin D—Risks and benefits.
National Cancer Council: Australia; 2016;
https://wiki.cancer.org.au/policy/
Position_statement_-_Risks_and_benefits_of_sun_exposureNeuroscience Research Australia and Kidsafe Australia.
Best Practice Guidelines for the Safe Restraint
of Children Travelling in Motor Vehicles, 2nd Ed.
Neuroscience Research Australia and Kidsafe Australia:
Sydney, Australia; 2020; https://shorturl.at/tyGL0Parab A, Whyte T, Albanese B, et al..
Can age or height define appropriate thresholds for transition to
adult seat belts? An analysis of observed seat belt fit
in children aged 7–12 years.
Int J Environ Res Public Health 2022;19(3):1524;
doi: 10.3390/ijerph19031524Oetgen ME, Heyer JH, Kelly SM.
Scoliosis screening.
J Am Acad Orthop Surg 2021;29(9):370–379;
doi: 10.5435/JAAOS-D-20-00356RACGP.
Abuse and Violence: Working with Our Patients in General Practice, 4th ed.
The Royal Australian College of General Practitioners:
Melbourne; 2014; https://shorturl.at/mvBX2Broaddus-Shea ET, Scott K, Reijnders M, et al..
A review of the literature on good practice considerations for initial
health system response to child and adolescent sexual abuse.
Child Abuse Negl 2021;116(Pt 1):104225;
doi: 10.1016/j.chiabu.2019.104225Danaher F, Vandeven A, Blanchard A, et al..
Recognizing, diagnosing, and preventing child maltreatment:
An update for pediatric clinicians.
Curr Opin Pediatr 2018;30(4):582–590;
doi: 10.1097/MOP.0000000000000648Lewis M.
De-legitimising complementary medicine: Framings of the Friends
of Science in Medicine-CAM debate in Australian media reports.
Sociol Health Illness 2019;41(5):831–851;
doi: 10.1111/1467-9566.12865Greenhalgh T, Howick J, Maskrey N.
Evidence based medicine: A movement in crisis?
BMJ 2014;348:g3725;
doi: 10.1136/bmj.g3725Djulbegovic B, Guyatt GH.
Progress in evidence-based medicine: A quarter century on.
Lancet 2017;390(10092):415–423; doi: 10.1016/S0140-6736(16)31592-6Venus C, Jamrozik E.
Evidence-poor medicine: Just how evidence-based
are Australian clinical practice guidelines?
Intern Med J 2020;50(1):30–37;
doi: 10.1111/imj.14466Macdonell K, Christie K, Robson K, et al..
Implementing family-integrated care in the NICU: Engaging
veteran parents in program design and delivery.
Adv Neonatal Care 2013;13(4):262–269, quiz 270–261;
doi: 10.1097/ANC.0b013e31829d8319Berg RC, Gamst A, Said M, et al..
True user involvement by people living with HIV is possible:
Description of a user-driven HIV clinic in Norway.
J Assoc Nurses AIDS Care 2015;26(6):732–742;
doi: 10.1016/j.jana.2015.07.002Coad J, Flay J, Aspinall M, et al..
Evaluating the impact of involving young people in
developing children's services in an acute hospital trust.
J Clin Nurs 2008;17(23):3115–3122;
doi: 10.1111/j.1365-2702.2008.02634.xElwell R.
Developing a nurse-led integrated ‘red legs' service.
Br J Commun Nurs 2014;19(1):12, 14–19;
doi: 10.12968/bjcn.2014.19.1.12Todd S, Felce D, Beyer S, et al..
Strategic planning and progress under the All Wales Strategy:
Reflecting the perceptions of stakeholders.
J Intellect Disabil Res 2000;44 (Pt 1):31–44;
doi: 10.1046/j.1365-2788.2000.00248.xTooke J.
Involving people with dementia in the work of an organisation:
Service User Review Panels.
Qual Ageing Older Adults 2013;14:56–65;
10.1108/14717791311311111 [CrossRef]Weinstein J.
Involving mental health service users in quality assurance.
Health Expect 2006;9(2):98–109;
doi: 10.1111/j.1369-7625.2006.00377.xHowick J, Koletsi D, Ioannidis JPA, et al..
Most healthcare interventions tested in Cochrane Reviews
are not effective according to high quality evidence:
A systematic review and meta-analysis.
J Clin Epidemiol 2022;148:160–169;
doi: 10.1016/j.jclinepi.2022.04.017US Preventive Services Task Force.
Behavioral Counseling to Prevent Skin Cancer:
US Preventive Services Task Force Recommendation Statement.
JAMA 2018;319(11):1134–1142;
doi: 10.1001/jama.2018.1623Owens DK, Davidson KW, Krist AH, et al..
Primary care interventions for prevention and cessation of tobacco use
in children and adolescents: US preventive services
task force recommendation statement.
JAMA 2020;323(16):1590–1598;
doi: 10.1001/jama.2020.4679
Return to PEDIATRICS
Return to BEST PRACTICES
Return to PEDIATRICS GUIDELINES
Since 6-21-2024


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |