

The Role of Chiropractic Care in Providing Health Promotion
and Clinical Preventive Services for Adult Patients with
Musculoskeletal Pain: A Clinical Practice GuidelineThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Altern Complement Med 2021 (Oct); 27 (10): 850–867 ~ FULL TEXT
OPEN ACCESS Cheryl Hawk, Lyndon Amorin-Woods, Marion W Evans, James M Whedon, Clinton J Daniels, Ronald D Williams et. al
Texas Chiropractic College,
Pasadena, Texas, USA.
Objective: To develop evidence-based recommendations on best practices for delivery of clinical preventive services by chiropractors and to offer practical resources to empower provider applications in practice.
Design: Clinical practice guideline based on evidence-based recommendations of a panel of practitioners and experts on clinical preventive services. Methods: Synthesizing the results of a literature search for relevant clinical practice guidelines and systematic reviews, a multidisciplinary steering committee with training and experience in health promotion, clinical prevention, and/or evidence-based chiropractic practice drafted a set of recommendations. A Delphi panel of experienced practitioners and faculty, primarily but not exclusively chiropractors, rated the recommendations by using the formal consensus methodology established by the RAND Corporation/University of California.
Results: The Delphi consensus process was conducted during January-February 2021. The 65-member Delphi panel reached a high level of consensus on appropriate application of clinical preventive services for screening and health promotion counseling within the chiropractic scope of practice. Interprofessional collaboration for the successful delivery of clinical preventive services was emphasized. Recommendations were made on primary, secondary, tertiary, and quaternary prevention of musculoskeletal pain.
Conclusions: Application of this guideline in chiropractic practice may facilitate consistent and appropriate use of screening and preventive services and foster interprofessional collaboration to promote clinical preventive services and contribute to improved public health.
KEYWORDS: chiropractic; clinical practice guidelines; clinical preventive services; health promotion; musculoskeletal conditions; spinal manipulation
From the Full-Text Article:
Introduction
Over 30 years ago, the World Health Organization stated: “The role of the health sector must move increasingly in a health promotion direction, beyond its responsibility for providing clinical and curative services.” [1] However, this admonition has yet to be fully adopted by health care systems. For example, in the United States, more than 1 million annual deaths are attributed to preventable—usually health behavior-related—risk factors. [2] Using preventive care services as recommended could prevent more than 50,000 deaths per year and add 2 million healthy years of life. [2]
The importance of preventing disease is indisputable. A great deal is known about disease prevention and health promotion; changing health behavior is a key approach. Between 2014 and 2018, the number of guidelines listed for disease prevention in primary care medicine doubled in the U.S. National Guideline Clearinghouse of the Agency for Healthcare Research and Quality. [2] However, providers delivered guideline-recommended preventive services to fewer than 40% of at-risk patients. [2]
Interprofessional collaboration may address some of the shortfalls in health promotion and disease prevention by creating an overlap and sharing of the tasks among providers, especially for patients with multiple chronic conditions who often see several types of health professionals. [3-5]
Toward that end, this clinical practice guideline is designed to offer a practical model of interprofessional collaboration for chiropractors in the delivery of clinical preventive services — that is, services provided by health care providers that reduce risk factors and screen for early-stage disease [6] — to adult patients with musculoskeletal conditions. Utilizing the breadth of the available health care workforce, including chiropractors, would bolster at-risk patients' exposure to health promotion messages. Patients with musculoskeletal complaints are the primary patient population for the chiropractic profession. [7] They overlap with other health care providers, such as family physicians, thus increasing their exposure to health screening and counseling.
This guideline presents the spectrum of clinical preventive services as a context but focuses recommendations for services generally within the chiropractic scope of practice, which varies somewhat regionally and internationally, but generally includes non-drug, non-surgical approaches to patient care. [7] It also emphasizes the importance of practitioners developing collaborative referral networks to optimize patient care.
We also address two important barriers to the delivery of clinical preventive services: lack of time and providers' self-perceived lack of expertise in delivering preventive services. [2, 8] This guideline includes a “Resource Guide,” which will be housed on the Clinical Compass (CC) website (clinicalcompass.org) and regularly maintained and updated. It will offer current, readily accessed electronic resources for both doctors and patients to facilitate chiropractors' use of “best practices” for counseling patients on health behavior and assist them in following through on their recommendations.
This project used a Delphi consensus process with a panel of health care practitioners and academicians (n = 65) to develop a clinical guideline that provided evidence-based recommendations on best practices for delivery of clinical preventive services by chiropractors and to offer practical resources to empower provider applications in practice.
Methods
The purpose of this project was to develop an evidence- and consensus-based clinical practice guideline on the role of chiropractic care in providing health promotion and clinical preventive services for adult patients with musculoskeletal pain.
The development of recommendations followed steps based on those used in previous projects [9-12]:
Establish a multidisciplinary Steering Committee (SC) with training and experience in health promotion, clinical prevention, and/or evidence-based chiropractic practice.
Examine the most current clinical practice guidelines (CPGs) related to each aspect of management.
Identify gaps in the CPG(s) that may form barriers to best practices.
Perform targeted literature searches for the highest available evidence on the gap topics.
Make recommendations on chiropractic management, based on the best available evidence.
Conduct a Delphi consensus process with a panel of experienced practitioners and faculty.
Gather additional feedback from a public posting of the consensus statements. [10, 11]
Human subjects' considerations
Before establishing the Delphi panel, the lead institution obtained Institutional Review Board approval. Delphi panelists signed an informed consent that specified that their participation was voluntary and without compensation. They were provided with a consent form after the consensus process was completed in which they agreed to be acknowledged by name in the resulting publication after we obtained their signed form.
Project SC
The SC was composed of clinicians and academicians with many years of clinical and/or research experience representing multiple health professions. Its responsibilities were to examine and evaluate the evidence; develop recommendations based on the best available evidence; revise the recommendations based on the Delphi panelists' ratings and comments to reach a consensus; and contribute to the final manuscript.
Of the 15-member SC, 13 are Doctors of Chiropractic (DCs). The two non-DCs are PhDs (one in psychology and one in health promotion). To address topic expertise, three of the members have public-health related PhDs (Preventive Medicine or Health Promotion), three are Certified Health Education Specialists, one is a certified health and wellness coach, and one has an MPH.
Professions represented, including cross-trained DCs, are chiropractic, massage therapy, medicine, nursing, psychology, public health, and health promotion education. Nine are employed at health care training institutions, three at the Veterans Health Administration as clinicians, and three in private practice. To ensure stakeholder representation, seven of the DCs on the SC are in leadership positions of the CC, a chiropractic organization that represents U.S. state chiropractic associations as well as the U.S. chiropractic colleges and other chiropractic organizations. All but two of the SC members are located in the United States; two are located in Australia.
Literature search
A health sciences librarian, working with the SC, conducted literature searches in two stages. At least two investigators independently screened articles resulting from the searches for eligibility. Disagreements were resolved by discussion.
First stage search
To identify “seed documents” on which to base development of the initial set of seed recommendations, we conducted a search to identify the most recent clinical practice guidelines for clinical preventive services. We restricted the search to articles published from 2018 to 2020, because it has been recommended that CPGs be updated approximately every 3 years. [13]
Inclusion criteria for articles were:
Published January 2018–December 2020
English language
PubMed (It is unlikely that higher levels of evidence would be found in databases other than PubMed.)
Addressed non-pharmacological, non-surgical clinical preventive services in adults
Guidelines (clinical practice guidelines)
Exclusion criteria: Articles were excluded if they addressed:
Topics typically outside chiropractic scope of practice (e.g., managing specific non-musculoskeletal conditions or diseases; pharmacological preventive interventions)
Special populations (any other than non-pregnant adults)
Specific local populations or geographic areas only
Because chiropractic practice is predominantly concerned with the management of people with musculoskeletal conditions, we created search strategies for topics that might contribute to clarifying an appropriate role for chiropractic care in primary, secondary, and tertiary prevention.
These were:
Health promotion and disease prevention
Diet, physical activity, and obesity management
Tobacco cessation
Immune response related to manual therapy
Lifestyle factors related to immune system support
Hygiene for infectious disease prevention related to chiropractic practice
Details of the construction of these search strategies are provided in Supplementary Data. In addition, we used reference tracking and consulted topic experts on the SC to ensure that relevant papers were not missed. We also included evidence from our previous CPG on chiropractic management of patients with chronic musculoskeletal pain, which involves tertiary prevention. [11]
Second stage search
For topics on which no CPGs were identified, the search was extended to include systematic reviews and meta-analyses.
When there were gaps in or lack of detail for implementing guideline recommendations, we made additional targeted searches of specific preventive services/health promotion topics.
Evaluation of the quality of the evidence
The articles identified in our searches were then evaluated for quality. A Literature Review committee was formed to perform the evaluations. The project director developed an orientation manual for the committee members. It included a brief review of key aspects of study design and detailed notes for each evaluation instrument to standardize their application. At least two investigators rated each study and discussed differences in ratings until they reached agreement.

Table 1

Table 2

Table 3

Table 4 We evaluated CPGs by using the AGREE-Global Rating Scale (Table 1), which we have used in other studies. [11, 12, 14] We evaluated systematic reviews by using a modified Scottish Intercollegiate Guideline Network (SIGN) checklist, [15] which has been used in other studies (Table 2). [11, 12, 16–19] The SIGN checklist rates the studies as “high quality, low risk of bias,” “acceptable quality, moderate risk of bias,” “low quality, high risk of bias,” or “unacceptable” quality. We did not assess the quality of other types of studies, simply identifying their design and categorizing them as “lower level.” Articles rated as “high” or “acceptable” quality were used as primary evidence to support recommendations; lower-level studies were used to support details to aid in implementation.
We used the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system [20] to assess the overall quality of the evidence: www.essentialevidenceplus.com/product/ebm_loe.cfm?show=grade. (Table 3) Four investigators performed the GRADE assessment independently. They resolved disagreement by discussion. We used GRADE's recommended rubric for determining strength of recommendation, which is detailed in Table 4. [20, 21]
Seed statements development
A 2012 set of “best practices” recommendations on the role of chiropractic care in health promotion and disease prevention served as a seed document to inform the development of the seed statements for this project. [22] We also used our 2020 clinical practice guideline on chiropractic management of chronic musculoskeletal pain as a blueprint for the format of this project. [11] The content of the seed statements was based on the results of the literature search, focusing on recent relevant clinical practice guidelines and adapting their recommendations as appropriate to chiropractic scope of practice. The SC developed the seed statements, revising them for clarity and congruence with the literature, until they agreed that they were ready to be sent to the Delphi panel for rating.
Delphi consensus panel
We conducted a Delphi consensus process as per the RAND-UCLA methodology: This method “generally involves multiple rounds, in which a questionnaire is sent to a group of experts who answer the questions anonymously. The results of the survey are then tabulated and reported back to the group, and each person is asked to answer the questionnaire again. This iterative process continues until there is a convergence of opinion on the subject or no further substantial changes in the replies are elicited.” [23](p. 6) We have an established, broad-based panel of DCs and other health professionals who value and are familiar with the evidence base of chiropractic and who represent both practice and academic experience. Previous projects focused on the United States, due to its specific practice parameters and reimbursement issues. However, for the current topic of health promotion and disease prevention, we expanded the panel to include international representation.
We developed the current Delphi panel by (i) inviting those who participated in our previous consensus projects and (ii) nominations by the SC of experienced practitioners from the United States and other countries. Nominees submitted a practice characteristics form and their CV for the SC to review and after approval were invited to participate. Seventy-one were invited, and 65 accepted.
Delphi process
We sent the panelists a brief summary of the project that included relevant background literature and a document orienting them to the Delphi process. All communications, and the consensus process, were conducted via email by the project coordinator. Panelists were de-identified during the rating process, to avoid possible bias.
We followed the RAND-UCLA methodology, which uses a rating scale anchored by 1 (highly inappropriate) to 9 (highly appropriate), with “uncertain” placed over the middle of the scale. [23] In keeping with this methodology, we defined “appropriateness” to mean that the expected health benefit to the patient exceeds the expected negative consequences by a sufficiently wide margin that it is worth doing, exclusive of cost. [23] If panelists rated a statement as inappropriate (rating 1–3), they were asked to state a reason and provide a citation from the peer-reviewed literature to support it, if possible. Without a specific reason, the response was considered incomplete and no number was recorded. This procedure was used to facilitate creation of an appropriate, evidence-based revision that accurately represented the panelists' input as well as the available literature.
Data management and analysis
After each Delphi round, the project coordinator entered the ratings data into an SPSS (v. 25) database, and she and the project director computed medians and percentages of agreement. To maintain the rigor of the methodology, the threshold for consensus was 80% with a median rating of at least 7. We calculated agreement by categorizing ratings of 1–3 as “inappropriate” (disagreement with the statement); 4–6 as “uncertain”, and 7–9 as “appropriate” (agreement). We sorted the panelists' comments in a Word table by panelist ID, statement number, and rating to facilitate review. The SC reviewed the ratings and the deidentified comments. The SC revised any statements that did not reach at least 80% agreement, basing the revision on both the panelists' comments and the available literature. We recirculated the revised statements, along with all comments, and repeated the process until a consensus was attained.
Stakeholder engagement and external review: public comments
In keeping with recommendations by organizations such as the AGREE Enterprise, [24] we used several means to ensure both transparency and stakeholder involvement into developing this guideline. (i) Stakeholders were included in the broad-based Delphi panel. (ii) We invited public comments on the draft CPG after the conclusion of the Delphi process.
Public comments were solicited through methods we had established in previous projects. [10, 11] We used several routes to disseminate an invitation for comments on the draft CPG:
Email blast through MailChimp to the CC email list. This included the Clinical Compass Board, which includes U.S. state chiropractic organizations; a number of national chiropractic professional and academic organizations (a total of ~900 individuals); and vendors, which included interested laypersons.
ChiroCongress, a professional organization whose member associations represent more than 35,000 chiropractors.
CC Facebook and LinkedIn pages. These are available to both health professionals and interested laypeople.
Chiropractic Summit (https://www.chirosummit.org/) email list. The Chiropractic Summit is a U.S. organization composed of chiropractic groups and individuals.
These different dissemination routes overlapped to some extent, which provided reinforcement of the message. We sent a two-week reminder after the initial mailing. The comment period was 30 days.
The invitation sent to all groups contained a link to a dedicated page on the CC website. This site included several documents:(i) A repetition of the initial invitation for comments;
(ii) Background and introduction to the project;
(iii) Summary of the methodology, including the names and credentials of all project personnel to promote transparency;
(iv) Definitions of key terms and concepts for readers who were not familiar with health promotion and disease prevention terminology;
(v) The draft consensus statements; these included their references and also the percent agreement attained in the Delphi process; and finally,
(vi) A user-friendly comment form to facilitate responses and instructions to email the form directly to the project coordinator.The project director and the SC reviewed and decided how to respond to each comment. In the event that comments resulted in substantive change, the revised statements were to be recirculated in an additional Delphi round(s) until a consensus was reached.
Results

Figure 1

Table 5
Page 7

Figure 2

Table 6

Table 7
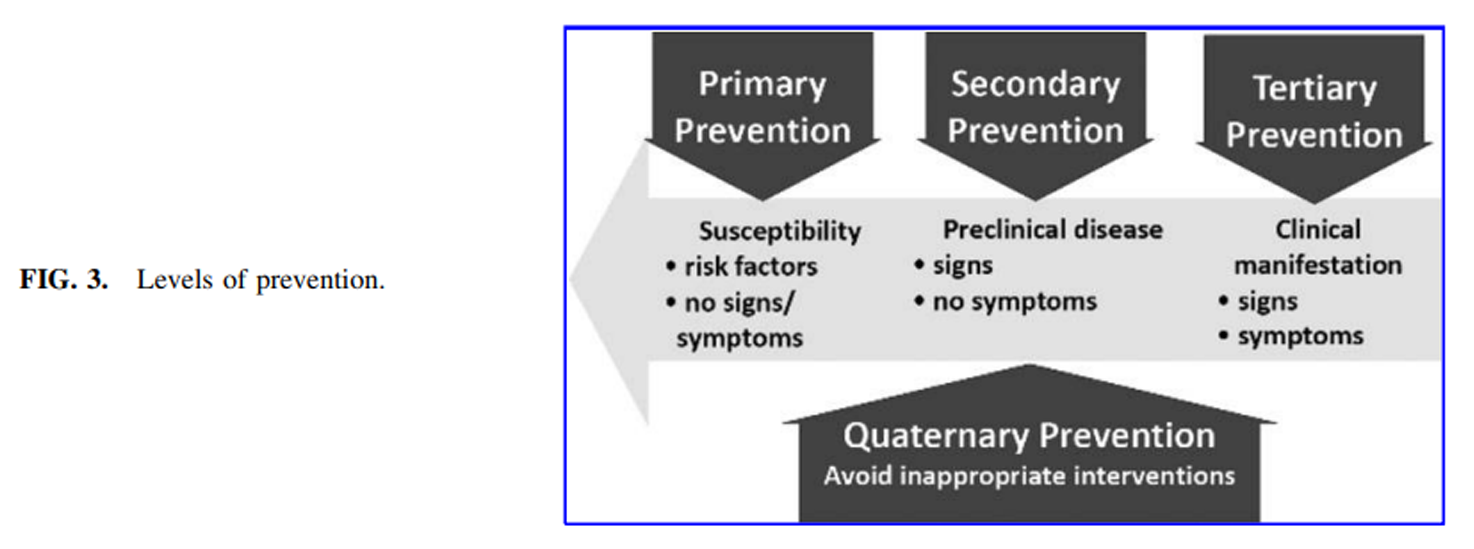
Figure 3 Literature search
First stage search: clinical practice guidelines Topics for which CPGs were identified were health promotion and disease prevention, diet, physical activity and obesity management, and tobacco cessation. Figure 1 shows the results of this search (2018–2020). Of 89 citations, 27 remained after screening for duplicates and eligibility (see Table 5 for list of articles). [12, 25–49] (Excluded studies are listed in Supplementary Data) We included several guidelines that were published before 2018 if there were no comparable guidelines published more recently.
Second stage search: systematic reviews Topics for which no CPGs were identified were effects on the immune system of spinal manipulation and lifestyle factors. The search for systematic reviews yielded 112 articles, as shown in Figure 2. After screening for eligibility and relevance, eight articles remained (shown in Table 6). [50–57] (Excluded studies are listed in Supplementary Data.)
Quality assessment
These 27 CPGs were all rated as high or acceptable. Table 5 lists the articles and quality rating for each. [12, 25–49, 58] The eight systematic reviews were all rated as high quality. Table 6 lists the articles and quality rating for each. [50–57]
Table 7 displays the rating of the quality of evidence and strength of recommendations for general topics. For screening and counseling on health behavior, infection control procedures for ambulatory care, and chiropractic management of tertiary prevention of pain, the evidence was strong, and there were no factors to lessen the strength of the recommendations in favor of these. For the effect of physical activity and environmental risk factors on the immune system, evidence was less robust, but because there are a few risks and multiple benefits of these, the recommendation in favor is strong.
For the effects of spinal manipulation on immune function, systematic reviews were high quality. However, the evidence they evaluated was low level and based on non-clinical studies. The strength of our recommendations varied. Although there is a low risk of side effects, the low-level evidence is outweighed by the possible delay or avoidance of interventions with more substantial evidence.
Public comments
After the 30-day public comment period, three comments were received. All were from chiropractors (one each from Florida, Oregon, and Australia). They were supportive of the project but wanted more details to be included about examinations and nutritional recommendations. Because of the defined scope of the project, the SC did not consider these comments to affect the validity of the consensus statements.
Delphi panel characteristics
The final panel composed of 65 individuals represented 6 health professions (acupuncture, chiropractic care, medicine, mental health counseling, nursing, and physical therapy). The distribution of professions was 94% DC, 3% MD, and 3% PT. The other professions listed were dual-trained DCs. The panelists were primarily male (78%) and Caucasian (85%). Other races/ethnicities reported were: other, unspecified (3), Hispanic (2), Asian/Pacific Islander (1), Black/African American (1), East Indian (1), Multiracial (1), and one missing response.
Delphi process
The list of key terms and concepts was provided to the panelists to be read before they began rating the statements, to be sure they were making decisions based on common terminology.
Definitions of key terms and conceptsClinical preventive services: Services provided by health care providers that
(1) prevent disease or injury by reducing risk factors and
(2) identify (screen for) disease at an early stage to reduce its impact. [6]According to the Guide to Clinical Preventive Services, [59] clinical preventive medicine interventions can be divided into the areas of screening, counseling, immunizations, and chemoprophylaxis.
Disease prevention: Interventions to avoid or minimize diseases and their associated risk factors. [60]
Disease prevention categories [60] (See Figure 3)Primary: remove the cause or risk factors for a condition/disease before it occurs
Secondary: detect a condition/disease at an early stage and reduce or prevent long-term effects (e.g., screening)
Tertiary: reduce the chronic effects of a condition/disease, minimizing sequelae (e.g., rehabilitation)
Quaternary: protect individuals from health care “interventions that are likely to cause more harm than good” [60](p. 106)Disease prevention model applied to pain management(developed by the Prevention of Acute and Chronic Pain Working Group of the U.S. Federal Pain Research Strategy) [61]
Primary prevention of pain: prevention of acute pain (example: injury prevention)
Secondary prevention of pain: prevention of transition of acute to chronic pain
Tertiary prevention of pain: reducing the effect of chronic pain on health and health-related quality of life.
E-Health: a type of medical informatics using electronic resources such as web-based technology and m-health (use of mobile devices, including wearable technologies) to monitor clinical signs, provide health information, and facilitate patient engagement in self-care for a healthier lifestyle and social support. [62–64]
Health promotion (WHO definition): the process of enabling people to increase control over, and to improve, their health, usually through addressing behavioral risk factors. [1]
Risk factor: Factors that increase the likelihood of people experiencing a health-related event.
Screening: Tests or procedures used to identify a disease at an early stage before it becomes symptomatic. Screening is a key component of secondary prevention. Because the individual is asymptomatic, the potential benefits of screening must outweigh the risks, and the individual must understand the risks and benefits.
Authoritative organizations such as the U.S. Preventive Services Task Force have conducted extensive evidence reviews and risk/benefit analyses on commonly used screening tests. [59]There were 60 statements for the panelists to rate in the first Delphi round. All 65 panelists responded to all Delphi rounds. All but two statements reached at least 80% consensus. Both statements were revised as per the comments and based on the evidence. One statement reached a consensus in Round 2 after being revised. The other required a third round and was rewritten as three statements before reaching a consensus. The following statements are the final product of the Delphi process.

Consensus Recommendations
Recommendations for general topics on health promotion and clinical prevention
Clinical preventive services, which include screening and counseling on health promotion and disease prevention, contribute to reducing current epidemic levels of chronic disease, chronic pain, obesity, and opioid use. [6]
Specific health behaviors are risk factors for most chronic conditions for which people seek health care. [6]
It is the responsibility of health care providers to identify these risk factors and facilitate health behavior change through providing appropriate evidence-based interventions or access to resources for such interventions. [6, 65, 66]
A biopsychosocial model is most appropriate for health promotion and disease prevention, particularly for typical chiropractic patients who present with chronic musculoskeletal pain and comorbidities/risk factors such as obesity, diabetes, cardiovascular disease, and other chronic conditions. [44, 67]
Interprofessional collaboration contributes to the successful delivery of clinical preventive services. [3–5]
Within their regulated scope of practice, chiropractors, similar to other health professionals, should follow established best-practice guidelines for disease prevention and health promotion, such as those recommended by the United States Preventive Services Task Force (USPSTF) and other recognized authorities. [11, 22, 68]
Use health promotion counseling strategies established for use in primary care settings that can be delivered as brief interventions (3–10 min, which may be spread over multiple visits) to facilitate health behavior change in patients with risk factors for or presence of chronic disease. Emphasize key principles [8]:
To encourage willing collaboration between patient and provider and gauge patient readiness to change, ask the patient for permission to discuss a behavioral issue directly related to the presenting complaint. [8]
Provide necessary information appropriate to the patient's level of health literacy.
Mutually agree on a specific behavior change, emphasizing its importance to the individual.
Provide readily accessed resources (ehealth/mhealth or conventional) so the patient can immediately take action. [62, 64, 69]
Follow up at subsequent visits with brief questions and encouragement.Address patients' cultural values as appropriate within the context of the specific health care topic on which you are counseling them. If these are not known, respectfully ask about their health beliefs and customs. [25]
Informed consent, risks, and benefits [12]
Chiropractic management should be consistent with the principles of evidence-based practice, which depend on: (i) the best available published scientific evidence combined with (ii) the clinician's experience and expertise and (iii) the patient's preferences and values.
Inform the patient about any serious potential risks and costs as well as the possible benefits of a proposed intervention.
The informed consent process involves active provider–patient communication. Explain all procedures, including diagnostic and treatment options (including no treatment and the natural history of spinal pain), in terms that are appropriate for the patient's level of health literacy. [11, 70] After answering the patient's questions and obtaining their signature, enter the informed consent into the health record.
Assess the patient for possible contraindications to manipulation or other procedures, particularly high-velocity, low-amplitude “thrust” maneuvers. [11, 12, 45]
Chiropractic-specific health promotion and disease prevention model
Health promotion and disease prevention in chiropractic care should be based on a biopsychosocial model encouraging patient empowerment and engagement in self-care practices. [22, 67]
Clinical preventive services within the chiropractic scope of practice are congruent with those of other providers and emphasize the following three components [22, 37]:
Screening for risk factors for disease, particularly lifestyle-related risk factors such as tobacco use, lack of physical activity, poor diet, and obesity.
Evidence-based health behavior counseling to promote health and prevent disease and injury, placing an emphasis on physical activity, dietary, and lifestyle factors that promote optimal function.
Manual procedures, including spinal manipulation, to enhance the patient's ability to engage in an active lifestyle. [11]The phases of prevention for chiropractic management of musculoskeletal pain may be appropriately applied as follows:
Primary prevention of pain: Chiropractic management that includes counseling on exercises or safety measures to decrease the risk of acute injury addresses primary prevention of pain. [61] However, clinical evidence does not currently exist to support the use of spinal manipulation alone for direct primary prevention of any condition or disease. [53]
Secondary prevention of pain: Chiropractic management that includes spinal manipulation, lifestyle counseling and other non-pharmaceutical approaches may contribute to secondary prevention of pain by shortening the duration of acute pain but little evidence supports spinal manipulation alone in preventing the transition from acute to chronic pain. [47, 61, 71]
Tertiary prevention of pain: Substantial evidence supports chiropractic management that includes spinal manipulation, lifestyle counseling, and other non-pharmaceutical approaches for tertiary prevention of pain. [11, 72–75]

Table 8
See p. 12Recommendations for primary prevention of disease and disability Overall screening and counseling Tobacco use, obesity, poor diet, and physical inactivity are key risk factors for chronic disease that are of paramount importance to the health of the public. Like all health care providers, DCs should screen for these risk factors and provide or refer for evidence-based resources and/or counseling. [22, 37] Table 8 summarizes all screening and counseling recommendations of the USPSTF. [29, 37, 76–78]
Tobacco cessation [41]
Determine the tobacco use status of all adolescent and adult patients and record it in the health record.
Offer tobacco users information and/or resources for cessation. At a minimum, offer him or her the national quit line number (U.S. 800-QUIT-NOW).
Offer patients readily accessed online cessation resources.
Base tobacco cessation counseling on the Ask, Advise, and Refer or 5 A's (Ask, Advise, Agree, Assist, Arrange) approach. [37, 49, 79]
Weight management [28]
Identify patients who are overweight or obese and ask permission to initiate a health-focused and person-centered discussion with them. [38]
Overweight patients with weight-related conditions (such as diabetes) and obese patients should be provided with a lifestyle program that includes (i) reducing calories; (ii) increasing physical activity; and (iii) interventions to support behavioral change. [37, 38, 80]
Provide patients with individualized follow-up feedback by using technology-based strategies. [38, 62–64, 81]
Nutrition/diet
Make nutrition recommendations for adults of all body sizes personally and culturally acceptable and affordable to the patient as well as nutritionally adequate to support long-term adherence. [38, 82]
Advise patients with risk factors for chronic disease or presence of chronic disease to adopt a diet emphasizing vegetables, fruits, whole grains, and unprocessed food and minimizing added sugar and salt. [32, 58]
Physical activity

Table 9
Advise currently sedentary patients to reduce sitting time and increase moderate-to-vigorous physical activity. [40, 83–86]
For currently sedentary patients, follow the updated screening recommendations of the American Academy of Sports Medicine for exercise participation (Table 9). [35]

Injury prevention
Fall prevention for older adults [31]
Advise older adults on balance, strength, and endurance exercises for fall prevention. [76, 87–89]
There is limited evidence directly supporting manual therapy to improve balance in older adults. [90, 91] However, spinal manipulation is supported for reducing chronic musculoskeletal pain and cervicogenic dizziness. [92, 93] In the presence of these conditions, a multimodal approach that includes spinal manipulation combined with an appropriate exercise regimen [76, 88] and resources for patients to correct home hazards [94] may be supportive to older adults at risk for falls.
Suicide prevention
Because chronic pain and opioid use are among a group of important risk factors for suicide, [95–97] establish and maintain a list of qualified counselors experienced in suicide risk assessment and/or treatment for at-risk patients.
Maintain readily accessible community resources for suicide prevention, such as the National Suicide Prevention Lifeline.
Firearm safety
For patients with indications of risk for self-harm or harm to others, in additional to referral for counseling, recommend resources on firearm safety when appropriate. [36, 98]
Infection control
Immunization is a well-established medical approach to primary prevention. Because it is not within the chiropractic scope of practice, refer patients who ask about vaccines to authoritative, evidence-based resources. [22]
No definitive clinical evidence supports a protective effect of spinal manipulation on immune system function or infectious disease prophylaxis. [52, 53, 56]
Provide office and clinical staff with an infection control protocol with training on hand hygiene, personal protective equipment, and environmental (surface) cleaning to prevent infection, consistent with evidence-based international or national guidelines such as those provided by the World Health Organization. [26, 99]
Base advice to patients on infectious disease, particularly COVID-19, on evidence-based international or national public health guidelines. [99]
Risk factor reduction, particularly increased physical activity, tobacco use cessation, achieving and maintaining a healthy weight, healthy food choices, and stress management may have a supportive effect on the immune system. [50, 51, 54, 55, 57]

Recommendations for secondary prevention of disease and disability
Provide patients with evidence-based screening procedures within the chiropractic scope of practice, such as the priority USPSTF-recommended procedures shown in Table 1. [100]
Develop a referral network of appropriate primary care and specialist practitioners for recommended screening procedures outside the scope of chiropractic practice. [100]
During routine physical inspection of the body, note the presence of any skin lesions that appear atypical according to the ABCDEs inspection (Asymmetrical; irregular Border; uneven/changed Color; Diameter >0.25 inch; Evolving in size, shape, or symptoms) and refer the patient to a dermatologist or their primary care physician for screening. [101]
Recommendations for tertiary prevention of disease and disability
Spine-related chronic pain
Patients' chronic musculoskeletal pain should not be expected to be “cured” within a specified time interval and/or number of treatment visits. Maintaining pain and function at optimal levels may be facilitated by planned treatment visits to prevent relapses and recurrences. [11, 102–105]
The goal of pain management is to facilitate the patient's ability to function optimally. This requires engaging the patient in self-care and lifestyle modifications to avoid physician dependence.
Consider multiple approaches that include both active and passive interventions as well as both physical and mind–body interventions. [11]
3a. Active interventions for spine-related chronic pain include [11]:
Rehabilitation exercise, including strengthening and flexibility
Decrease amount of time spent sitting
Weight management for obese patients
Tobacco cessation for users
Walking or other moderate aerobic exercise
Yoga and qigong
3b. Passive interventions should be focused on assisting the patient to become more active [11]:Spinal manipulation/mobilization
Massage
Acupuncture
Low-level laser therapy
Electrotherapies: Transcutaneous Electrical Nerve Stimulation or interferential current to manage pain and assist patients in becoming active.
3c. Mind–body approaches: Offer resources (online or by referral) for Cognitive-Behavioral Therapy and Mindfulness-Based Stress Reduction. [11]
Osteoarthritis
Active physical interventions for osteoarthritis include:
Exercise to support both achieving and maintaining healthy weight and for fitness, strength, and flexibility. [46, 48]
Decrease sedentary time.
Multifactorial weight management if overweight or obese. [46, 48, 106]Passive physical interventions include [48]:
Manual therapy, including manipulation, mobilization, and/or massage [107–110]
Acupuncture, using “high dose” (greater treatment frequency, at least 3 × week) [111, 112]
Low-level laser therapy [113, 114]Mind–body approaches [46, 48]: Offer resources (online or by referral) for mind–body interventions, such as Cognitive-Behavioral Therapy and Mindfulness-Based Stress Reduction.

Quaternary prevention of disease and disability
For older patients with spinal pain, provide spinal manipulation to reduce use of opioid analgesic therapy. [65, 66, 115–119]
For adults with low back pain, provide chiropractic care to reduce risk of outpatient adverse drug events. [120]
For adults with work-related back injuries, provide chiropractic care when appropriate to reduce likelihood of back surgery. [121]
For older adults with spinal pain and no red flags, chiropractic care, including spinal manipulation, may be provided without imaging. [122–124]
Take a thorough health history on all patients, including opioid and other medication use. Because the unintended consequences of opioid analgesic therapy may complicate patient care, DCs should work closely with the medical physicians of patients using opioids to ensure appropriate clinical management and reduce risk of adverse drug events. It is outside the chiropractic scope of practice in most locations to advise patients to discontinue use of prescription medications, including opioids, so it is important to collaborate with patients' providers with prescriptive authority to support reduction of opioid use. [65, 74]
Discussion
Previous studies show that chiropractors already advise patients on preventive health behavior. According to the 2020 Practice Analysis by the United States National Board of Chiropractic Examiners, 60% of DCs report making specific recommendations to patients on changing health behavior at least once a day and 68% make recommendations on disease prevention and early screening at least weekly. [7]
An analysis of U.S. National Health Interview Survey (NHIS) data indicated that for people who sought spinal manipulation as a part of complementary and alternative medical care in 2012, more than 40% reported using this care as a wellness or preventive measure. Eleven percent stated they used manipulation to improve immune function. [125] Further, another NHIS analysis found that a large majority (88%) of patients reported that they complied with health promotion advice, either from a DC or an MD. [126] Therefore, it is important to ensure that chiropractors are providing recommendations that are consistent with national and international evidence-based standards.
The volume of evidence available to clinicians presents a significant challenge, because it is not feasible for busy clinicians to routinely review primary research literature. [127] Guidelines may be considered “a convenient way of packaging evidence and presenting recommendations to healthcare decision-makers.”128 To further narrow the gap between recommendations and clinical implementation, we will augment this CPG by providing a Resource Guide with tools for common methods of implementation of preventive services. Further, because the nature of chiropractic practice requires a number of visits, particularly for patients with chronic conditions, chiropractors have multiple opportunities to deliver health promotion messages.
A limitation of this guideline is that for certain practices, such as spinal manipulation, evidence is scarce to make recommendations regarding its use for any purpose other than addressing tertiary and perhaps secondary prevention of pain. Another limitation is that, although we included some input from countries other than the United States, and based some recommendations on international guidelines, these recommendations primarily address U.S. stakeholders. We did achieve broad representation of these stakeholders, however, through the SC, the Delphi panel, and the wide dissemination to the public. Another limitation is that, despite making the draft document widely available, we received very few responses from the public and none from professional organizations.
We have produced this consensus guideline not to create a set of prescriptive rules, but rather to develop a resource to assist practitioners in their implementation of best practices. The CPGs are a guide, not a rulebook. The application of evidence-based guidelines must always be contextualized within the best interests of each individual patient and the experience and expertise of the practitioner [70] along with feasibility and availability. [4, 65]
Conclusions
Application of this guideline in chiropractic practice may facilitate consistent and appropriate use of screening and preventive services and foster interprofessional collaboration to promote clinical preventive services and contribute to improved public health.
SupplementAcknowledgments
The authors thank Cathy Evans for her exceptional coordination of the consensus process and achieving the high response rate.
They also thank the Delphi panelists for their essential role in the development of these recommendations: Wayne Bennett, DC, DABCO; Craig Benton, DC; Charles L. Blum, DC; Gina M. Bonavito-Larragoite, DC, FIAMA; Michael S. Calhoun, DC, DACBSP; Wayne H. Carr, DC, ACRB, CCSP, AFMCP; Jeffrey R. Cates, DC, MS; Kelsey L. Corcoran, DC; Matthew Coté, DC, MS; Thomas R. Cotter, DC, DACRB; Monica Curruchich, DC RN-BSN; John Curtin, MSS, DC, IANM; Vincent DeBono, DC; Mark D. Dehen, DC, FICC; Paul Ettlinger, DC; James E. Eubanks, MD, DC, MS; Jason T. Evans, DC, DIBCN, FIACN, ABIME, NASM; Drew Fogg, DC, MS, DACRB, Cert. MDT; David Folweiler, DC, DACRB; Margaret M. Freihaut, DC; Bill Gallagher, Jr., DC; Brian J. Gleberzon, DC, MHs; Jason Guben, BSc(N),DC; Gary Alan Jacob, DC, Lac, MPH; Brian L. James, MD; Jeffrey M. Johnson, DC; Valerie Johnson, DC, DABCI, DACBN; Louis A. Kazal, Jr., MD, FAAFP; Yasmeen Khan, DC, MS, MA; Robert E. Klein, DC, FACO; Charmaine Maria Korporaal, M Tech. (Chiropractic), CCSP, CCFC, ICSSD; Rick Louis LaMarche, DC; Lawrence Jason Larragoite, DC, FIAMA, CFMP; Robert A. Leach, DC, MS, MCHES; Duane T. Lowe, DC; Eric Luke, DC, MS; Peter McCann, MAppSc, BAppSc, DAppSc, FASLM, MACA, MANTA; Peter J. McGlynn, BAppSc (Chiropractic), MPH, PhD; Ralph C. Magnuson, DPT; Hans W. Mohrbeck, DC; Scott A. Mooring, DC, CCSP; Mark Mulak, DC, MBA, MS, DACRB; Marcus Nynas, DC, FICC; Juli Olson, DC, DACM; Colette Peabody, MS, DC; Mariangela Penna, DC; Tamara Glen Pooke, M Tech (Chiropractic), South Africa, PhD Radiology, Malaysia; Morgan R. Price, DC; Ranen Rambrij, M Tech (Chiropractic); Jeffrey W. Remsburg, DC, MS, DACRB; Vern A. Saboe, Jr. DC, FACO; Bruce Scott, DC; Chris Sherman, DC, MPH; Scott M. Siegel, DC, FIAMA; Charles Simpson, DC; Albert Stabile, Jr., DC; Neil Stakes, M Chiro, Singapore, SDCA, CKTP, FAKTR; Kevin Stemple, PT; James P. Stupak, DC; Lisa Thomson, DC; Jason Weber, DC, DACRB; Susan Wenberg, DC, MA; John S. Weyand, DC, DABCO; Clint J. Williamson, DC; and Morgan Young, DC.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
The NCMIC Foundation provided partial funding for the project director; the Clinical Compass provided funding for the project coordinator.
References:
World Health Organization.
Ottawa Charter for Health Promotion.
Geneva, Switzerland: World Health Organization, 1986.Taksler GB, Pfoh ER, Stange KC, Rothberg MB.
Association between number of preventive care guidelines
and preventive care utilization by patients.
Am J Prev Med 2018;55:1–10.Fowler T, Garr D, Mager NDP, Stanley J.
Enhancing primary care and preventive services
through interprofessional practice and education.
Isr J Health Policy Res 2020;9:12.Parkin-Smith GF, Davies SJ, Amorin-Woods LG.
Looking ahead: Chronic spinal pain management.
J Pain Res 2017; 10:2089–2095.Schor A, Bergovoy-Yellin L, Landsberger D, et al.
Multidisciplinary work promotes preventive medicine and
health education in primary care: A cross-sectional survey.
Isr J Health Policy Res 2019;8:50.Healthy People 2020.
Clinical Preventive Services.
Washington, DC: Office of Disease Prevention and Health Promotion, 2020.National Board of Chiropractic Examiners.
Practice Analysis of Chiropractic, 2020
Greeley, CO: National Board of Chiropractic Examiners, 2020.Searight HR.
Counseling patients in primary care:
Evidence-based strategies.
Am Fam Physician 2018;98: 719–728.Farabaugh RJ, Dehen MD, Hawk C.
Management of Chronic Spine-Related Conditions:
Consensus Recommendations of a Multidisciplinary Panel
J Manipulative Physiol Ther 2010 (Sep); 33 (7): 484–492Globe, G, Farabaugh, RJ, Hawk, C et al.
Clinical Practice Guideline: Chiropractic Care for Low Back Pain
J Manipulative Physiol Ther. 2016 (Jan); 39 (1): 1–22Hawk C, Whalen W, Farabaugh RJ, et al.
Best Practices for Chiropractic Management of Patients with
Chronic Musculoskeletal Pain: A Clinical Practice Guideline
J Altern Complement Med 2020 (Oct); 26 (10): 884–901Whalen W, Farabaugh RJ, Hawk C, et al.
Best-Practice Recommendations for Chiropractic Management
of Patients With Neck Pain
J Manipulative Physiol Ther. 2019 (Nov); 42 (9): 635–650Vernooij RW, Sanabria AJ, Sola I, et al.
Guidance for updating clinical practice guidelines:
A systematic review of methodological handbooks.
Implement Sci 2014;9:3.Brouwers MC, Kho ME, Browman GP, et al.
The Global Rating Scale complements the AGREE II in
advancing the quality of practice guidelines.
J Clin Epidemiol 2012;65: 526–534.Harbour R, Lowe G, Twaddle S.
Scottish intercollegiate guidelines network:
The first 15 years (1993–2008).
J R Coll Physicians Edinb 2011;41:163–168.Hawk C, Minkalis A, Webb C, et al.
Manual Interventions for Musculoskeletal Factors in Infants
with Suboptimal Breastfeeding: A Scoping Review
Evid Based Integr Med 2018 (Dec 12); 23: 1–12Hawk C, Minkalis AL, Khorsan R, et al.
Systematic Review of Nondrug, Nonsurgical Treatment of Shoulder Conditions
J Manipulative Physiol Ther 2017 (Jun); 40 (5): 293–319Weis CA, Pohlman K, Draper C, et al.
Chiropractic Care of Adults With Postpartum-Related Low Back,
Pelvic Girdle, or Combination Pain: A Systematic Review
J Manipulative Physiol Ther 2020 (Sep); 43 (7): 732–743Weis CA, Pohlman K, Draper C, et al.
Chiropractic Care for Adults With Pregnancy-Related Low Back,
Pelvic Girdle Pain, or Combination Pain: A Systematic Review
J Manipulative Physiol Ther 2020 (Sep); 43 (7): 714-731Guyatt GH, Oxman AD, Vist GE, et al.
GRADE: An Emerging Consensus on Rating Quality of Evidence
and Strength of Recommendations
British Medical Journal 2008 (Apr 26); 336 (7650): 924–926Guyatt GH, Oxman AD, Kunz R, et al.
Going from evidence to recommendations.
BMJ 2008;336:1049–1051.Hawk C, Schneider M, Evans MW Jr, Redwood D:
Consensus Process to Develop a Best-Practice Document on the
Role of Chiropractic Care in Health Promotion,
Disease Prevention, and Wellness
J Manipulative Physiol Ther. 2012 (Sep); 35 (7): 556–567Fitch K, Bernstein SJ, Aquilar MD, et al.
The RAND/UCLA Appropriateness Method User’s Manual.
Monica, CA: RAND Corporation, 2003.Brouwers MC, Kho ME, Browman GP, et al.
AGREE II: Advancing guideline development, reporting,
and evaluation in health care.
Prev Med 2010;51:421–424.Agency for Healthcare Research and Quality.
Health Literacy Universal Precautions Toolkit. 2nd Edition.
Rockville, MD: Agency for Healthcare Research and Quality, 2020.Boyce JM, Pittet D,
Healthcare Infection Control Practices Advisory Committee,
HIPAC/SHEA/APIC/IDSA Hand Hygiene Task Force.
Guideline for hand hygiene in health-care settings.
Recommendations of the Healthcare Infection Control
Practices Advisory Committee and the HIPAC/SHEA/
APIC/IDSA Hand Hygiene Task Force.
Am J Infect Control 2002;30:S1–46.Bull FC, Al-Ansari SS, Biddle S, et al.
World Health Organization 2020 Guidelines on
Physical Activity and Sedentary Behaviour
J Phys Act Health. 2021 (May 14); 18 (6): 631-637Curry SJ, Krist AH, Owens DK, et al.
Behavioral weight loss interventions to prevent obesity-related morbidity
and mortality in adults: US Preventive Services Task Force Recommendation Statement.
JAMA 2018;320:1163–1171.Force USPST, Curry SJ, Krist AH, et al.
Screening for intimate partner violence, elder abuse, and abuse of
vulnerable adults: US preventive services task force final recommendation statement.
JAMA 2018;320:1678–1687.Force USPST, Curry SJ, Krist AH, et al.
Screening and behavioral counseling interventions to reduce
unhealthy alcohol use in adolescents and adults:
US Preventive Services Task Force recommendation statement.
JAMA 2018;320:1899–1909.US Preventive Services Task Force, Grossman DC, Curry SJ, et al.
Interventions to prevent falls in communitydwelling older adults: US Preventive Services Task Force recommendation statement.
JAMA 2018;319:1696–1704.Health Canada.
Canada’s Dietary Guidelines for Health Professionals and Policy Makers.
Ottawa, Canada: Health Canada, 2019.Katzmarzyk PT, Powell KE, Jakicic JM, et al.
Sedentary behavior and health:
Update from the 2018 Physical Activity Guidelines Advisory Committee.
Med Sci Sports Exerc 2019;51:1227–1241.Lobelo F, Rohm Young D, Sallis R, et al.
Routine assessment and promotion of physical activity in
healthcare settings: A scientific statement from the
American Heart Association.
Circulation 2018;137:e495–e522.Riebe D, Franklin BA, Thompson PD, et al.
Updating ACSM’s recommendations for exercise preparticipation health screening.
Med Sci Sports Exerc 2015;47:2473–2479.Talley CL, Campbell BT, Jenkins DH, et al.
Recommendations from the American College of Surgeons Committee
on Trauma’s Firearm Strategy Team (FAST) Workgroup: Chicago Consensus I.
J Am Coll Surg 2019; 228:198–206.U.S. Preventive Services Task Force.
Clinical Preventive Services A and B Recommendations for Screening and Counseling Adults.
Bethesda, WA: USPSTF, 2020.Wharton S, Lau DCW, Vallis M, et al.
Obesity in adults: A clinical practice guideline.
CMAJ 2020;192:E875–E891.Force USPST, Grossman DC, Curry SJ, et al.
Behavioral counseling to prevent skin cancer:
US Preventive Services Task Force recommendation statement.
JAMA 2018;319: 1134–1142.U.S. Department of Health and Human Services.
Physical Activity Guidelines for Americans. 2nd Edition.
Washington, DC: U.S. Department of Health and Human Services, 2018.US Preventive Services Task Force.
Interventions for tobacco smoking cessation in adults, including
pregnant persons: US Preventive Services Task Force recommendation statement.
JAMA 2021;325:265–279.Force USPST, Krist AH, Davidson KW, et al.
Screening for unhealthy drug use:
US Preventive Services Task Force recommendation statement.
JAMA 2020;323:2301– 2309.Geenen R, Overman CL, Christensen R, et al.
EULAR recommendations for the health professional’s approach to
pain management in inflammatory arthritis and osteoarthritis.
Ann Rheum Dis 2018;77:797–807.Haldeman S., Johnson C.D., Chou R. et al.
The Global Spine Care Initiative:
Classification System for Spine-related Concerns
European Spine Journal 2018 (Sep); 27 (Suppl 6): 889–900Herman PM, Vernon H, Hurwitz EL, Shekelle PG, Whitley MD, Coulter ID.
Clinical Scenarios for Which Cervical Mobilization and Manipulation
Are Considered by an Expert Panel to Be Appropriate (and Inappropriate)
for Patients with Chronic Neck Pain
Clin J Pain 2020 (Apr); 36 (4): 273–280Kolasinski SL, Neogi T, Hochberg MC, et al.
2019 American College of Rheumatology/Arthritis Foundation guideline
for the management of osteoarthritis of the hand, hip, and knee.
Arthritis Rheumatol 2020;72:220–233.Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530Royal Australian College of General Practitioners.
Guideline for the management of knee and hip osteoarthritis. 2nd Edition.
East Melbourne, Australia: Royal Australian College of General Practioners, 2018.Van Schayck OCP, Williams S, Barchilon V, et al.
Treating tobacco dependence: Guidance for primary care on
life-saving interventions. Position statement of the IPCRG.
NPJ Prim Care Respir Med 2017;27:38.Booth A, Reed AB, Ponzo S, et al.
Population risk factors for severe disease and mortality
in COVID-19: A global systematic review and meta-analysis.
PLoS One 2021;16: e0247461.Chastin SFM, Abaraogu U, Bourgois JG, et al.
Effects of regular physical activity on the immune system,
vaccination and risk of community-acquired infectious
disease in the general population:
Systematic review and metaanalysis.
Sports Med 2021 [Epub ahead of print]; DOI: 10.1007/s40279-021-01466-1.Chow N, Hogg-Johnson S, Mior S, et al.
Assessment of studies evaluating spinal manipulative therapy and
infectious disease and immune system outcomes: A systematic review.
JAMA Netw Open 2021;4:e215493.Goncalves G, Le Scanff C, Leboeuf-Yde C.
Effect of chiropractic treatment on primary or early secondary
prevention: A systematic review with a pedagogic approach.
Chiropr Man Therap 2018;26:10.Jayawardena R, Sooriyaarachchi P, Chourdakis M, et al.
Enhancing immunity in viral infections, with special emphasis
on COVID-19: A review.
Diabetes Metab Syndr 2020;14:367–382.Patanavanich R, Glantz SA.
Smoking is associated with COVID-19 progression: A meta-analysis.
Nicotine Tob Res 2020;22:1653–1656.Picchiottino M, Leboeuf-Yde C, Gagey O, Hallman DM.
The acute effects of joint manipulative techniques on markers of autonomic
nervous system activity: A systematic review and meta-analysis
of randomized shamcontrolled trials.
Chiropr Man Therap 2019;27:17.Schakel L, Veldhuijzen DS, Crompvoets PI, et al.
Effectiveness of stress-reducing interventions on the response
to challenges to the immune system: A meta-analytic review.
Psychother Psychosom 2019;88:274–286.U.S. Department of Health and Human Services.
Dietary Guidelines for Americans 2015–2020.
Washington, DC: USDHHS, 2015.U. S. Preventive Services Task Force.
The Guide to Clinical Preventive Services 2014:
Recommendations of the U.S. Preventive Services Task Force.
Rockville, MD: U.S. Preventive Services Task Force, 2014.Martins C, Godycki-Cwirko M, Heleno B, Brodersen J.
Quaternary prevention: Reviewing the concept.
Eur J Gen Pract 2018;24:106–111.Gatchel RJ, Reuben DB, Dagenais S, et al.
Research agenda for the prevention of pain and its impact:
Report of the work group on the prevention of acute and
chronic pain of the federal pain research strategy.
J Pain 2018;19: 837–851.Brørs G, Pettersen TR, Hansen TB, et al.
Modes of e-Health delivery in secondary prevention programmes
for patients with coronary artery disease: A systematic review.
BMC Health Serv Res 2019;19:364.Villarreal V, Berbey-Alvarez A.
Evaluation of mHealth applications related to
cardiovascular diseases: A systematic review.
Acta Inform Med 2020;28:130–137.Debon R, Coleone JD, Bellei EA, De Marchi ACB.
Mobile health applications for chronic diseases:
A systematic review of features for lifestyle improvement.
Diabetes Metab Syndr 2019;13:2507–2512.Parkin-Smith G, Amorin-Woods L, Shobbrook M, Losco B.
Chiropractors and the opioid epidemic: Strategies to mitigate
harm and promote evidence-based care (part 2: Summary).
Chiropr J Aust 2020;47:18–28.Shobbrook M, Amorin-Woods L, Parkin-Smith GF.
Mitigating the opioid crisis: An Australian perspective
on the role of chiropractors (part I).
Chiropr J Aust 2020;47: 4–17.Green BN, Johnson CD, Haldeman S, et al.
A Scoping Review of Biopsychosocial Risk Factors
and Co-morbidities for Common Spinal Disorders
PLoS One. 2018 (Jun 1); 13 (6) :e0197987Whedon JM, Bezdjian S, Dennis P, et al.
Cost Comparison of Two Approaches to Chiropractic Care for Patients
with Acute and Sub-acute Low Back Pain Care Episodes: A Cohort Study
Chiropractic & Manual Therapies 2020 (Dec 14); 28 (1): 68Gordon NP, Crouch E.
Digital information technology use and patient preferences for internet-based
health education modalities: Cross-sectional survey study of middle-aged
and older adults with chronic health conditions.
JMIR Aging 2019;2:e12243.Amorin-Woods LG, Losco BE.
‘PICO-D management’; a decision-aid for evidence-based
chiropractic education and clinical practice.
Chiropr Man Therap 2016;24:49.Stevans JM, Delitto A, Khoja SS, et al.
Risk Factors Associated With Transition From Acute to Chronic
Low Back Pain in US Patients Seeking Primary Care
JAMA Netw Open 2021 (Feb 1); 4 (2): e2037371Agency for Healthcare Research and Quality.
Noninvasive Nonpharmacological Treatment for Chronic Pain:
A Systematic Review Update
Comparative Effectiveness Review Number 227
Rockville (MD): Agency for Healthcare Research and Quality (2020)Skelly AC, Chou R, Dettori JR, et al.
Noninvasive Nonpharmacological Treatment for Chronic Pain:
A Systematic Review
Comparative Effectiveness Review no. 209
Agency for Healthcare Research and Quality (US), Rockville (MD) (2018)Hawk C, Schneider MJ, Haas M, Katz P, Dougherty P, Gleberzon B, et al.
Best Practices for Chiropractic Care for Older Adults:
A Systematic Review and Consensus Update
J Manipulative Physiol Ther 2017 (May); 40 (4): 217–229Weeks, WB, Leininger, B, Whedon, JM et al.
The Association Between Use of Chiropractic Care and Costs
of Care Among Older Medicare Patients With Chronic
Low Back Pain and Multiple Comorbidities
J Manipulative Physiol Ther. 2016 (Feb); 39 (2): 63–75Sherrington C, Michaleff ZA, Fairhall N, et al.
Exercise to prevent falls in older adults:
An updated systematic review and meta-analysis.
Br J Sports Med 2017;51:1750–1758.Smith PC, Schmidt SM, Allensworth-Davies D, Saitz R.
Primary care validation of a single-question alcohol screening test.
J Gen Intern Med 2009;24:783–788.U.S. Preventive Services Task Force, Curry SJ, Krist AH, et al.
Behavioral weight loss interventions to prevent obesity-related morbidity
and mortality in adults: US Preventive Services Task Force recommendation statement.
JAMA 2018;320:1163–1171.Buettner-Schmidt K, Maack B, Larson M, et al.
Systems change to improve tobacco use identification and
referral in the chiropractic setting: A pilot study.
Chiropr Man Therap 2018;26:45.Semlitsch T, Stigler FL, Jeitler K, et al.
Management of overweight and obesity in primary care-
A systematic overview of international evidence-based guidelines.
Obes Rev 2019;20:1218–1230.Dounavi K, Tsoumani O.
Mobile health applications in weight management:
A systematic literature review.
Am J Prev Med 2019;56:894–903.Lee MK, Amorin-Woods L, Cascioli V, Adams J.
The use of nutritional guidance within chiropractic patient management:
A survey of 333 chiropractors from the ACORN practice-based research network.
Chiropr Man Therap 2018;26:7.Piercy KL, Troiano RP.
Physical activity guidelines for americans from the
US Department of Health and Human Services.
Circ Cardiovasc Qual Outcomes 2018;11: e005263.Piercy KL, Troiano RP, Ballard RM, et al.
The physical activity guidelines for Americans.
JAMA 2018;320:2020–2028.Powell KE, King AC, Buchner DM, et al.
The scientific foundation for the physical activity guidelines for Americans, 2nd edition.
J Phys Act Health 2018:1–11.Brown WJ BA, Bull FC, Burton NW.
Development of Evidence-based Physical Activity Recommendations for Adults (18–64 Years).
Canberra, ACT, Australia: Australian Government Department of Health, 2013.Rodrigues IB, Ponzano M, Giangregorio LM.
Practical tips for prescribing exercise for fall prevention.
Osteoporos Int 2019;30:1953–1960.Sherrington C, Fairhall N, Wallbank G, et al.
Exercise for preventing falls in older people living in the community:
An abridged Cochrane systematic review.
Br J Sports Med 2020;54:885–891.Yitayeh A, Teshome A.
The effectiveness of physiotherapy treatment on balance dysfunction
and postural instability in persons with Parkinson’s disease:
A systematic review and meta-analysis.
BMC Sports Sci Med Rehabil 2016;8:17.Holt KR, Haavik H, Elley CR.
The effects of manual therapy on balance and falls: A systematic review.
J Manipulative Physiol Ther 2012;35:227–234.Holt, KR, Haavik, H, Lee, ACL, Murphy, B, and Elley, CR.
Effectiveness of Chiropractic Care to Improve Sensorimotor Function Associated with
Falls Risk in Older People: A Randomized Controlled Trial
J Manipulative Physiol Ther. 2016 (May); (39) 4: 267–278Clar C, Tsertsvadze A, Court R, Hundt G, Clarke A, Sutcliffe P.
Clinical Effectiveness of Manual Therapy for the Management of
Musculoskeletal and Non-Musculoskeletal Conditions:
Systematic Review and Update of UK Evidence Report
Chiropractic & Manual Therapies 2014 (Mar 28); 22 (1): 12Rubinstein SM, de Zoete A, van Middelkoop M, et al.
Benefits and Harms of Spinal Manipulative Therapy for the Treatment
of Chronic Low Back Pain: Systematic Review and Meta-analysis
of Randomised Controlled Trials
British Medical Journal 2019 (Mar 13); 364: l689Moreland B, Kakara R, Henry A.
Trends in nonfatal falls and fall-related injuries among adults
aged ‡65 years-United States, 2012–2018.
MMWR Morb Mortal Wkly Rep 2020;69:875–881.Petrosky E, Harpaz R, Fowler KA, et al.
Chronic pain among suicide decedents, 2003 to 2014:
Findings from the national violent death reporting system.
Ann Intern Med 2018;169:448–455.Braden JB, Edlund MJ, Sullivan MD.
Suicide deaths with opioid poisoning in the United States: 1999–2014.
Am J Public Health 2017;107:421–426.Campbell G, Bruno R, Darke S, et al.
Prevalence and correlates of suicidal thoughts and suicide attempts
in people prescribed pharmaceutical opioids for chronic pain.
Clin J Pain 2016;32:292–301.Sexton SM, Lin KW, Weiss BD, et al.
Preventing gun violence: The role of family physicians.
Am Fam Physician 2018;98:560–568.Evans MW, Jr., Ramcharan M, Floyd R, et al.
A proposed protocol for hand and table sanitizing in
chiropractic clinics and education institutions.
J Chiropr Med 2009;8: 38–47.Maciosek MV, LaFrance AB, Dehmer SP, et al.
Updated priorities among effective clinical preventive services.
Ann Fam Med. 2017;15:14–22.Brunssen A, Waldmann A, Eisemann N, Katalinic A.
Impact of skin cancer screening and secondary prevention campaigns
on skin cancer incidence and mortality: A systematic review.
J Am Acad Dermatol 2017;76:129–139 e110.Eklund A, Hagberg J, Jensen I, Leboeuf-Yde C, Kongsted A, Lovgren P, et al.
The Nordic Maintenance Care Program: Maintenance Care Reduces the Number
of Days With Pain in Acute Episodes and Increases the Length of Pain Free
Periods for Dysfunctional Patients With Recurrent and Persistent Low Back Pain -
A Secondary Analysis of a Pragmatic Randomized Controlled Tial
Chiropractic & Manual Therapies 2020 (Apr 21); 28: 19Eklund, A., I. Jensen, M. Lohela-Karlsson, J. Hagberg, C. Leboeuf-Yde, et al. (2018).
The Nordic Maintenance Care Program: Effectiveness of Chiropractic Maintenance Care
Versus Symptom-guided Treatment for Recurrent and Persistent Low Back Pain -
A Pragmatic Randomized Controlled Trial
PLoS One. 2018 (Sep 12); 13 (9): e0203029Iben A, Lise H, Charlotte LY.
Chiropractic Maintenance Care - What’s New?
A Systematic Review of the Literature
Chiropractic & Manual Therapies 2019 (Nov 21); 27: 63Herman P, Edgington S, Ryan G, Coulter I.
Prevalence and Characteristics of Chronic Spinal Pain Patients
with Different Hopes (Treatment Goals) for Ongoing Chiropractic Care
J Alternative and Complementary Medicine 2019 (Oct 1); 25 (10): 1015-1025Reyes C, Leyland KM, Peat G, et al.
Association between overweight and obesity and risk of clinically
diagnosed knee, hip, and hand osteoarthritis: A population-based cohort study.
Arthritis Rheumatol 2016;68:1869–1875.Nelson NL, Churilla JR.
Massage therapy for pain and function in patients with arthritis:
A systematic review of randomized controlled trials.
Am J Phys Med Rehabil 2017;96:665–672.Perlman A, Fogerite SG, Glass O, et al.
Efficacy and safety of massage for osteoarthritis of the knee:
A randomized clinical trial.
J Gen Intern Med 2019;34:379–386.Anwer S, Alghadir A, Zafar H, Brismee JM.
Effects of orthopaedic manual therapy in knee osteoarthritis:
A systematic review and meta-analysis.
Physiotherapy 2018; 104:264–276.Ceballos-Laita L, Estebanez-de-Miguel E, Martin-Nieto G, et al.
Effects of non-pharmacological conservative treatment on pain, range of
motion and physical function in patients with mild to moderate hip osteoarthritis.
A systematic review.
Complement Ther Med 2019;42: 214–222.Gong Z, Liu R, Yu W, et al.
Acutherapy for knee osteoarthritis relief in the elderly:
A systematic review and meta-analysis.
Evid Based Complement Alternat Med 2019;2019:1868107.Sun N, Tu JF, Lin LL, et al.
Correlation between acupuncture dose and effectiveness in
the treatment of knee osteoarthritis: A systematic review.
Acupunct Med 2019; 37:261–267.Stausholm MB, Naterstad IFM, Joensen J, et al.
Efficacy of low-level laser therapy on pain and disability in knee
osteoarthritis: Systematic review and meta-analysis
of randomised placebo-controlled trials.
BMJ Open 2019;9: e031142.Wyszynska J, Bal-Bochenska M.
Efficacy of highintensity laser therapy in treating
knee osteoarthritis: A first systematic review.
Photomed Laser Surg 2018;36: 343–353.Corcoran KL, Bastian LA, Gunderson CG, et al.
Association Between Chiropractic Use and Opioid Receipt Among
Patients with Spinal Pain: A Systematic Review and Meta-analysis
Pain Medicine 2020 (Feb 1); 21 (2): e139–e145Kazis LE, Ameli O, Rothendler J, et al.
Observational retrospective study of the association of initial
healthcare provider for new-onset low back pain with early
and longterm opioid use.
BMJ Open 2019;9:e028633.Lisi AJ, Corcoran KL, DeRycke EC, et al.
Opioid Use Among Veterans of Recent Wars Receiving
Veterans Affairs Chiropractic Care
Pain Med. 2018 (Sep 1); 19 (suppl_1): S54–S60Whedon JM, Toler AWJ, Goehl JM, Kazal LA.
Association Between Utilization of Chiropractic Services for
Treatment of Low-Back Pain and Use of Prescription Opioids
J Altern Complement Med. 2018 (Jun); 24 (6): 552–556Whedon JM, Toler AWJ, Kazal LA, Bezdjian S, Goehl JM, Greenstein J.
Impact of Chiropractic Care on Use of Prescription
Opioids in Patients with Spinal Pain
Pain Medicine 2020 (Dec 25); 21 (12): 3567–3573
There are more like this at: SPINAL PAIN MANAGEMENTWhedon JM, Toler AWJ, Goehl JM, Kazal LA.
Association Between Utilization of Chiropractic Services for
Treatment of Low-Back Pain and Use of Prescription Opioids
J Altern Complement Med. 2018 (Jun); 24 (6): 552–556Keeney BJ, Fulton-Kehoe D, Turner JA, et al.
Early Predictors of Lumbar Spine Surgery After Occupational
Back Injury: Results From a Prospective Study
of Workers in Washington State
Spine (Phila Pa 1976). 2013 (May 15); 38 (11): 953–964Davis MA, Yakusheva O, Liu H, et al.
Access to Chiropractic Care and the Cost of Spine Conditions Among Older Adults
American Journal of Managed Care 2019 (Aug); 25 (8): e230–e236Whedon JM, Toler AWJ, Bezdjian S, et al.
Implementation of the Primary Spine Care Model in a Multi-Clinician
Primary Care Setting: An Observational Cohort Study
J Manipulative Physiol Ther 2020 (Sep); 43 (7): 667–674Powell AC, Rogstad TL, Elliott SW, et al.
Health care utilization and pain outcomes following
early imaging for low back pain in older adults.
J Am Board Fam Med 2019; 32:773–780.Hawk C, Ndetan H, Evans MW, Jr.
Potential role of complementary and alternative health care providers
in chronic disease prevention and health promotion:
An analysis of National Health Interview Survey data.
Prev Med 2012;54:18–22.Ndetan H, Evans MW, Jr., Bae S, et al.
The health care provider’s role and patient compliance to
health promotion advice from the user’s perspective:
Analysis of the 2006 National Health Interview Survey data.
J Manipulative Physiol Ther 2010;33:413–418.Greenhalgh T, Howick J, Maskrey N,
Evidence Based Medicine Renaissance Group.
Evidence based medicine: A movement in crisis?
BMJ 2014;348:g3725.Treweek S, Oxman AD, Alderson P, et al.
Developing and evaluating communication strategies to support informed
decisions and practice based on evidence (DECIDE): Protocol and preliminary results.
Implement Sci 2013;8:6.GRADE (Grading of Recommendations Assessment, Development and Evaluation)
Working Group 2007 (modified by the EBM Guidelines Editorial Team).
www.essentialevidenceplus.com/product/ebm_loe.cfm?show= grade
Accessed April 7, 2021.
Return to BEST PRACTICES
Return to MUSCULOSKELETAL PAIN GUIDELINES
Since 9-12-2021


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |