

The Effect of Reduced Access to Chiropractic Care
on Medical Service Use for Spine Conditions
Among Older AdultsThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Manipulative Physiol Ther 2021 (Jun); 44 (5): 353–362 ~ FULL TEXT
Matthew Davis • Olga Yakusheva • Haiyin Liu
Brian Anderson • Julie Bynum
University of Michigan,
400 North Ingalls, Room 4347,
Ann Arbor, MI 48109
FROM: Keeney ~ Spine 2013 (May 15)Objective: The purpose of this study was to examine the extent to which access to chiropractic care affects medical service use among older adults with spine conditions.
Methods: We used Medicare claims data to identify a cohort of 39,278 older adult chiropractic care users who relocated during 2010-2014 and thus experienced a change in geographic access to chiropractic care. National Plan and Provider Enumeration System data were used to determine chiropractor per population ratios across the United States. A reduction in access to chiropractic care was defined as decreasing 1 quintile or more in chiropractor per population ratio after relocation. Using a difference-in-difference analysis (before versus after relocation), we compared the use of medical services among those who experienced a reduction in access to chiropractic care versus those who did not.
Results: Among those who experienced a reduction in access to chiropractic care (versus those who did not), we observed an increase in the rate of visits to primary care physicians for spine conditions (an annual increase of 32.3 visits, 95% CI: 1.4-63.1 per 1,000) and rate of spine surgeries (an annual increase of 5.5 surgeries, 95% CI: 1.3-9.8 per 1,000). Considering the mean cost of a visit to a primary care physician and spine surgery, a reduction in access to chiropractic care was associated with an additional cost of $114,967 per 1,000 beneficiaries on medical services ($391 million nationally).
Conclusions: Among older adults, reduced access to chiropractic care is associated with an increase in the use of some medical services for spine conditions.
Keywords: Back Pain; Chiropractic; Health Services Accessibility.
From the Full-Text Article:
Introduction
At any given point, approximately 30% of older adults are experiencing back pain and 16% have neck pain. [1, 2] Compared with younger counterparts for whom musculoskeletal conditions are often self-limiting, older adults who experience back pain are more likely to have future recurrences1, [3] that can lead to long-term functional limitations. [4] The high prevalence coupled with back pain being among the leading causes of disability is contributing to excessive national healthcare costs. Among older adults, $28.8 billion was spent on back and neck pain each year in the United States. [5] Most back pain is not caused by any serious underlying pathology. [6, 7] Thus, established guidelines by the American Pain Society and American College of Physicians recommend nonpharmacological and conservative measures for back pain. [8] Back pain is among the most frequent reasons older Americans visit medical physicians [9, 10] and there continues to be overreliance on opioid analgesics, medical specialists, and unwarranted diagnostic imaging. [11-14]
Chiropractic care is among the most common nonmedical services used by Americans to treat spine conditions, most of which are back and/or neck pain. [15] Since the 1970s, chiropractic care has been included in Medicare as a benefit used by approximately 7.0% of beneficiaries. [16] Among older adults with known spine conditions, approximately 35% use chiropractic care. [17] The Centers for Medicare and Medicaid Services (CMS) spends between $400 and $500 million on the chiropractic care benefit. [18, 19] Several reports by the Office of the Inspector General [18-21] that examined the benefit have underscored the high relative payout. Missing from the debate regarding the Medicare benefit is a clear understanding of how chiropractic care affects the use of conventional medical services. A prior study uncovered an association between higher accessibility of chiropractic care and lower reliance on primary care services, suggesting chiropractic care may substitute for medical visits.22 Further, a more recent report found associations between higher access to chiropractic care and lower spending on diagnostic services [23] —services that should be reserved for patients needing more invasive care such as surgery.6 Therefore, it is conceivable that the CMS is recapturing at least part of the payout for chiropractic care by a reduction in the use of conventional medical services. However, the indirect effects of chiropractic care on medical service use have not been rigorously examined.
The purpose of this study was to examine how access to chiropractic care affects the use of medical services for spine conditions among older adults. We hypothesized that access to chiropractic care may reduce dependency on medical services for spine conditions by providing an alternative point of access to the healthcare system. Previous work has shown that a loss in access to health services has a more immediate effect on use, whereas an increase in access takes years to change how individuals use health services. [24] Therefore, we examined how reduced access to chiropractic care (as a proxy for removal of CMS's chiropractic care benefit) affects visits to medical physicians, diagnostic services, and medical treatment for spine conditions.
Methods
We conducted a retrospective cohort study to examine the association between reduced access to chiropractic care and medical service use among older adults with spine conditions. We used data from 2010 to 2014 to geocode Medicare beneficiaries and identified a cohort that relocated once. Local accessibility of chiropractic care was estimated using the Variable Distance Enhanced Two-Step Floating Catchment Area—a method that accounts for local drive time. This study received an expedited review by the University of Michigan Health and Behavioral Sciences Institutional Review Board (HUM00105363).
Study Population
Medicare is the national health insurance program for older adults in the United States that is administered by the CMS. Administrative claims from Medicare were used to identify the cohort of older adults for our study. We used the Medicare Master Beneficiary Summary Files to identify all older adults (age 65 or older) who, in addition to coverage of hospital services (Part A), were continually enrolled in coverage of doctor's visits and outpatient services (Part B) from 2010 to 2014. Across the country, there are 306 Hospital Referral Regions that represent different healthcare markets. Medicare beneficiaries who relocated once from 2010 to 2014 were identified by a change in Hospital Referral Regions. This resulted in the identification of 887,917 older adults (Appendix).
Next, we identified chiropractic care users by linking all Medicare beneficiaries who relocated to their respective healthcare claims. We identified those with evidence of using chiropractic care before they moved based on 1 or more claims to a chiropractor. Further restricting the sample to those who had a minimum of 2 years of data before and after relocation resulted in 42,842 older adult chiropractic users. We removed those in the lowest quintile of access to chiropractic care before relocation, because those individuals by definition could only relocate to the same level or increase access following relocation. Our final sample consisted of 39,278 older adult chiropractic users (Appendix, Fig 1).
Access to Chiropractic Care
Historic versions of the National Plan and Provider Enumeration System that include the addresses of all US Medicare providers were used to identify the practice location of chiropractors from 2010 to 2014. Provider specialty code 35 in the National Plan and Provider Enumeration System was used to identity chiropractors. [25] Each chiropractor was linked to Medicare claims in the 20% Carrier files. Those that did not submit at least one Medicare claim were assumed to be inactive and removed from our analyses. For each Zone Improvement Plan Code Tabulation Area (ZCTA), we estimated chiropractic care accessibility using an enhanced version of the 2-step floating catchment area method first developed by Luo and Wang [26] and modified by others. [27] This approach has a distinct advantage over “bucketing” approaches, because it provides a higher resolution and is less sensitive to the inherent issues of data aggregation into artificial units. Detailed methods regarding this measure of access can be found elsewhere. [23, 28]
We identified older adults who experienced a reduction in access to chiropractic care after relocation based on access in their respective ZCTA at baseline versus after relocation. Both before and after relocation, the distribution of chiropractor per population ratios across US ZCTAs were separated into quintiles. Older adults who relocated to a ZCTA in a lower quintile relative to their baseline were identified as the group that experienced reduced access, versus those who did not experience a reduction (ie, relocated to a ZCTA in the same or higher quintile relative to the baseline). In this way, a reduction in access to chiropractic care after relocating served as a proxy for loss of the chiropractic care service.
Medical Services for Spine ConditionsVisits to Medical Providers We were interested in differentiating among several different types of visits for spine conditions to conventional medical providers. First, using administrative claims for all ambulatory visits, we identified those for either back and/or neck pain. To do so, we used an established list of International Classification of Diseases, Ninth Edition, Clinical Modification codes to identify spine conditions. [29, 30] Using the provider specialty codes [25] associated with claims for spine conditions, we identified visits to chiropractors, primary care physicians (family practice, internal medicine, general practice, and geriatricians), medical specialists who commonly treat spine conditions (neurologists and physiatrists), and spine surgeons (orthopedic and neurosurgeons).
Diagnostic Exam Services Diagnostic imaging for spine conditions were identified using a collection of Healthcare Common Procedure Coding System codes among ambulatory claims. [31] We separated plain film spine diagnostic exams from advanced imaging that included computed tomography and magnetic resonance imaging for spine conditions.
Treatment (Opioids and Surgeries) To determine whether access to chiropractic care affects medical treatment in meaningful ways, we examined prescription opioid use and spine surgeries. Medicare Part D files were used to identify the number of prescriptions for opioid analgesics before and after relocation using a list of established National Drug Codes. [32] Spine surgeries were identified using a list of Current Procedural Terminology codes used by others. [31]Covariates
Several sociodemographic characteristics were used to adjust for differences between the groups. Age, sex, and race/ethnicity were obtained from the Master Beneficiary Summary File. We used diagnosis codes in the Medicare Provider Analysis and Review, Carrier, and Outpatient files to calculate a comorbidity score using the Charlson-Deyo Comorbidity Index. [33] This comorbidity measure was used to control for differences in health status. In the 2 years before relocation, beneficiaries were identified as having the respective comorbidity if he or she had evidence of inpatient hospitalization with the comorbidity. To avoid potential misidentification of individuals who received a single inaccurate diagnosis, we required at least 2 ambulatory claims (in the Carrier and/or Outpatient files) to classify the existence of comorbidity. We also adjusted for the calendar year in which the move occurred.
National Cost Estimates
To make estimates of how potential differences in the utilization of medical services may affect national spending, we estimated the mean cost for spine visits to physicians and spine surgeries using data from the Medical Expenditure Panel Survey for 2012 (the midyear of our study time period). The Medical Expenditure Panel Survey is one of the largest sources of data on US healthcare spending from which national estimates can be made using complex survey design methods. Among all adults 65 and older, we estimated the mean cost of physician visits for a spine condition and spine surgery.
The estimated cost (across all payers) for a spine visit to a physician was $250 and $19,435 for spine surgery. Approximately 7.0% of older adults use chiropractic care [16] — we extrapolated our cost estimates to this population of 3.4 million older adults. We express our estimates as the number of services per 1,000 beneficiaries. Using the effect of reduced access to chiropractic care, we estimate nationally what the effect would be if all 3.4 million older adult chiropractic care users lost access. We make national cost estimates by multiplying total services by the aforementioned cost estimates.
Statistical Analyses
We used data from 2 years before and after relocation (referred to as baseline and post-relocation herein). Using a difference-in-difference design, we compared the rate of service use 2 years before versus 2 years after relocation (first difference) between those who experienced a decrease in access to chiropractic care versus those who did not (second difference). Endpoints for all health services were at the population level (ie, the rate of service use per 1,000 older adults) averaged over the 2 years before (and after). We display unadjusted rates for the 2 years before versus after relocation for endpoints. To examine the association between a decrease in access to chiropractic care and medical service use, we used generalized linear models of the endpoints as the dependent variables on the primary exposure modeled as a 2-way interaction term (baseline/post-relocation × reduced access/ same or increased access) and adjusted for age, sex, race, baseline comorbidity, and year in which the move occurred. A 2-sided p value of less than 0.05 was considered statistically significant. Geospatial analyses were conducted using ArcGIS version 10.5 (Redlands, California), and analysis of claims data was conducted using SAS version 9.4 (Cary, North Carolina).
Results
Characteristics of Study Population

Table 1

Table 2
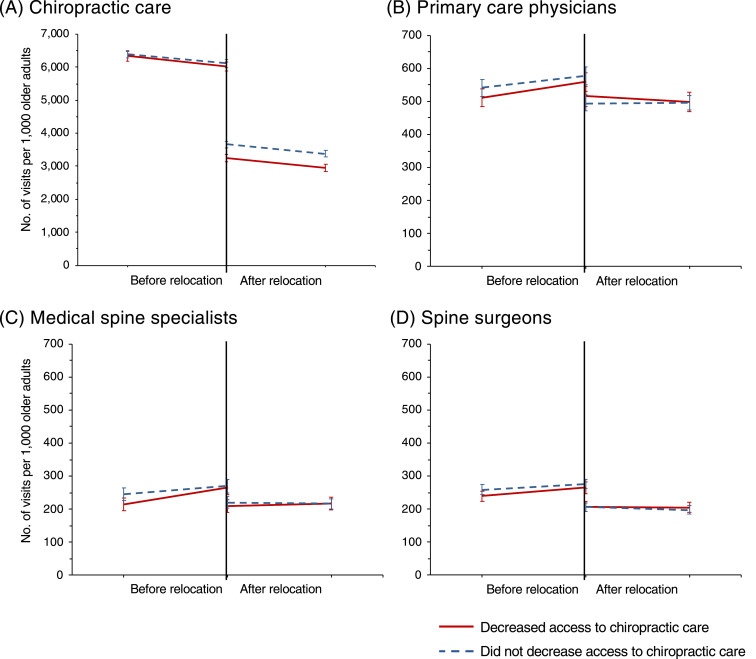
Figure 1
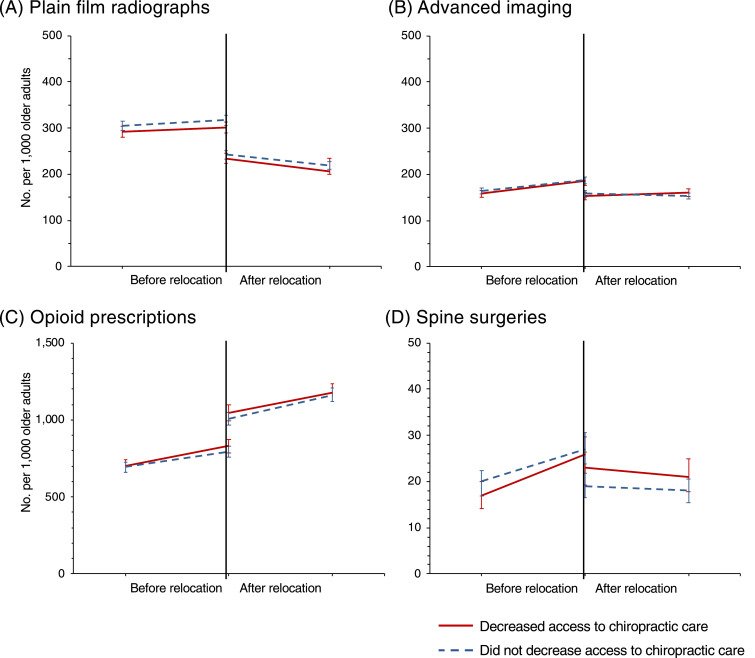
Figure 2 Among the 39,278 older adults who relocated within the 5-year period, 16,121 (41.0%) experienced a reduction in access to chiropractic care after relocation (Table 1). Overall, older adults who experienced a reduction in access to chiropractic care were similar to those who did not experience a decrease in access. Those who experienced a decrease in access were slightly younger (mean age of 75.1 versus 75.4 years) and less racially diverse. In utilization of spine services at baseline, those who experienced a decrease in access had fewer plain film radiographs (296.8 versus 311.0 per 1,000, p value 0.02).
Change in Access to Chiropractic Care and Medical Spine Services
Older adults who experienced reduced access to chiropractic care were less likely to visit chiropractors after they moved. Decreasing 1 quintile of chiropractic care access was associated with an annual reduction of 309.4 visits to chiropractors per 1,000 older adults (95% CI: 104.3-514.5), p value < 0.01 (Table 2 and Fig 1). However, a reduction of 1 quintile of access to chiropractic care was associated with an increase of 32.3 visits to primary care physicians for spine conditions per 1,000 older adults (95% CI: 1.4-63.1). Statistically significant associations were not observed for visits to spine surgeons and/or medical spine specialists.
Among diagnostic imaging (ie, plain film radiographs and advanced imaging) and treatment measures (ie, opioids and surgeries) for spine conditions, the only statistically significant association was for the rate of spine surgeries. A reduction in access to chiropractic care by 1 quintile was associated with an increase of 5.5. surgeries per 1,000 older adults (95% CI 1.3-9.8), p value 0.01.
Considering the cost of medical services for spine conditions, a reduction in access to chiropractic care was associated with an additional cost of $8,075 per 1,000 beneficiaries on primary care visits and $106,892 on spine surgeries. Extrapolating the effect of reduced access to chiropractic care to the entire Medicare population (to estimate the national effect of eliminating the chiropractic care benefit to all 3.4 million chiropractic care users in Medicare), reduced access to chiropractic care would result in an additional 110 million visits to primary care physicians (annual cost of $27.5 million) and 19,000 additional spine surgeries (annual cost of $363.4 million). (annual cost $390.9 million).
Discussion
This study is among the first to utilize a rigorous methodology to examine the indirect effects of access to chiropractic care on medical services use. We used a combination of administrative healthcare data and a difference-in-difference methodology to examine the effects of reducing access to chiropractic care on service use for spine conditions. Each individual served as his or her own control, and a reduction in access to chiropractic care after relocation served as a proxy for loss of the chiropractic care benefit. At the population level, we found statistically significant increases in both spinal surgeries and primary care visits among older adult chiropractic users who experienced a reduction in access to chiropractic care after relocating (versus those who did not experience reduced access). Translating the observed increase of 5.5 spine surgeries per 1,000 older adults owing to reduced access to chiropractic care to the entire Medicare population (ie, 3.4 million chiropractic users) results in 19,000 additional spine surgeries nationally at an annual cost of $363.4 million. Likewise, an additional 110 million visits to primary care physicians for spine conditions was associated with reduced access to chiropractic care at an annual cost of $27.5 million to CMS. In sum, this amounts to $391 million annually—a sizeable proportion of the CMS's payout for the service.18,19
Prior studies that examined the relationship between access to chiropractic care and primary care service use have been limited to ecological study designs. Davis et al. found an inverse association between the regional supply of chiropractors and the number of visits to primary care physicians for spine conditions22—residing in areas of the highest chiropractic supply was associated with an 8% reduction in visits for spine conditions to primary care physicians (including family and internal medicine). Our study suggests that this association may translate to differences in healthcare utilization at the patient level. If indeed access to chiropractic care reduces the burden on primary care physicians (ie, treatment of spine conditions that are common in primary care), it has important implications for healthcare policy considering potential limits on Medicare coverage for chiropractic services and the anticipated shortfall of primary care physicians nationally.34
We also found an association between a reduction in chiropractic care availability and higher rates of spine surgeries. Our study aligns with an observational study by Nelson et al. that found that insurance plans with a chiropractic benefit resulted in a 14% reduction in back surgery.35 At the episode level, Fritz et al.36 found that individuals with back pain initiating care with a chiropractor experienced an 87% reduction in spine surgery visits. Although surgery is indicated for a small number of patients with spine conditions, current treatment guidelines advocate for conservative management for most cases. Our results provide some modest evidence that access to chiropractic care may disrupt treatment escalation, leading to surgery. We did not find statistically significant associations with imaging services. The increased utilization of plain film radiography following reduced access to chiropractic care was only marginally statistically significant (p = 0.10). Other reports23,35,36 have found associations between chiropractic care use and decreased utilization of imaging services.
A recent meta-analysis37 concluded that chiropractic users had 64% lower odds of receiving an opioid medication than nonusers for treatment of spine conditions. Specific to the Medicare population, a strong inverse correlation was found between the per-capita supply of chiropractors and the proportion of older adults filling opioid prescriptions.38 This is particularly timely given the rate at which opioid abuse and overdose have grown over the past decade.39 This was evident in our analyses as both groups increased in opioid use over time. However, we did not identify a statistically significant association between reduced access to chiropractic care and prescription opioid use
Limitations
In our analyses, each individual served as his or her control (by comparing before versus after relocation), making the observed effects internally valid. Yet, older adults who relocated once during the study period may not be generalizable to the entire population of older Americans. Second, the 2-year window (particularly after relocation) used to calculate the difference in health care utilization may not be adequate to capture long-term behavior change. Recent work shows that 2 years is reasonable to identify immediate effects of reduced access to health services24; however, health service use could be different over longer periods. Third, this study used nonexperimental data; thus, residual confounding cannot completely be ruled out. However, the difference-in-difference approach minimizes confounding to a greater degree compared to conventional observational studies. Lastly, it was not possible to determine the degree to which health service use was appropriate and/or concordant with existing practice guidelines in our analyses. Although most patients would benefit from a conservative approach, a small number require rapid medical intervention owing to the severity of disease.
Future Studies
Most studies to date that have evaluated the CMS's chiropractic care benefit are observational designs that have inherent limitations. Future studies should apply more rigorous natural experimental designs that are being used by a growing number of health researchers to make causal inferences from nonexperimental data. Furthermore, more research is needed to determine the impacts of access to chiropractic care beyond that of health service use and cost. For instance, studies should examine how access at the population level affects quality of care (ie, the degree to which care is concordant with current practice guidelines) at the level of the episode and among specific spine conditions.
Conclusion
Individuals seeking chiropractic care have a high degree of confidence in the ability of chiropractors to improve their symptoms40 and have a strong preference for the service.17 Health services do not operate within a vacuum. Studies evaluating the service tend to neglect considering how the CMS's chiropractic care benefit affects the healthcare system at large. We found modest evidence of increased spine surgeries and primary care visits among older adults who lost access to chiropractic care after moving. This suggests that the chiropractic care benefit in Medicare may have an indirect effect on the use of other services for spine conditions. This has important implications for health policy decisions, because it suggests that CMS may be recapturing a sizeable proportion of the payout for the chiropractic care benefit through a reduction in medical service use.
Supplementary Information
Appendix (PDF)
Funding Sources and Conflicts of Interest
This study was funded by R01AT009003 from the National Center for Complementary & Integrative Medicine at the NIH. Davis receives consulting fees for serving as a statistical reviewer for Regional Anesthesia and Pain Medicine. Otherwise, no other conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): M.D., O.Y., H.L., B.A., J.B.
Design (planned the methods to generate the results): M.D., O.Y. Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): M.D.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): M.D., O.Y., H.L. Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): M.D., O.Y., H.L., B.A., J.B.
Literature search (performed the literature search): M.D., B.A. Writing (responsible for writing a substantive part of the manuscript): M.D.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): M.D., O.Y., H.L., B.A., J.B.References:
Docking RE Fleming J Brayne C Zhao J Macfarlane GJ Jones GT.
Epidemiology of back pain in older adults: prevalence and risk factors for back pain onset.
Rheumatology (Oxford). 2011; 50: 1645-1653Patel KV Guralnik JM Dansie EJ Turk DC.
Prevalence and impact of pain among older adults in the United States:
findings from the 2011 National Health and Aging Trends Study.
Pain. 2013; 154: 2649-2657Dunn KM Hestbaek L Cassidy JD.
Low back pain across the life course.
Best Pract Res Clin Rheumatol. 2013; 27: 591-600Murray CJ, Atkinson C, Bhalla K, et al;
The State of US Health, 1990-2010: Burden of Diseases, Injuries, and Risk Factors
JAMA 2013 (Aug 14); 310 (6): 591–608Dieleman JL, Baral R, Birger M, et al.
US Spending on Personal Health Care and Public Health, 1996-2013
JAMA 2016 (Dec 27); 316 (24): 2627-2646Deyo RA Jarvik JG Chou R.
Low back pain in primary care.
BMJ. 2014; 349: g4266Srinivas SV Deyo RA Berger ZD.
Application of “less is more” to low back pain.
Arch Intern Med. 2012; 172: 1016-1020Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530Deyo RA Mirza SK Martin BI.
Back pain prevalence and visit rates: estimates from U.S. national surveys, 2002.
Spine (Phila Pa 1976). 2006; 31: 2724-2727Hart LG Deyo RA Cherkin DC.
Physician office visits for low back pain. Frequency, clinical evaluation,
and treatment patterns from a U.S. national survey.
Spine (Phila Pa 1976). 1995; 20: 11-19Mafi JN McCarthy EP Davis RB Landon BE.
Worsening trends in the management and treatment of back pain.
JAMA Intern Med. 2013; 173: 1573-1581Vogt MT Kwoh CK Cope DK Osial TA Culyba M Starz TW.
Analgesic usage for low back pain: impact on health care costs and service use.
Spine (Phila Pa 1976). 2005; 30: 1075-1081Webster BS Cifuentes M Verma S Pransky G.
Geographic variation in opioid prescribing for acute, work-related,
low back pain and associated factors: a multilevel analysis.
Am J Ind Med. 2009; 52: 162-171Ivanova JI Birnbaum HG Schiller M Kantor E Johnstone BM Swindle RW.
Real-world practice patterns, health-care utilization, and costs in patients
with low back pain: the long road to guideline-concordant care.
Spine J. 2011; 11: 622-632Davis, MA, Sirovich, BE, and Weeks, WB.
Utilization and Expenditures on Chiropractic Care
in the United States from 1997 to 2006
Health Serv Res. 2010 (Jun); 45 (3): 748-761Whedon JM, Song Y, Davis MA.
Trends in the Use and Cost of Chiropractic Spinal Manipulation Under Medicare Part B
Spine J. 2013 (Nov); 13 (11): 1449–1454Weigel, PA, Hockenberry, JM, and Wolinsky, FD.
Chiropractic Use in the Medicare Population: Prevalence, Patterns, and Associations
With 1-Year Changes in Health and Satisfaction With Care
J Manipulative Physiol Ther. 2014 (Oct); 37 (8): 542-551U.S. Department of Health and Human Services,
Office of the Inspector General
Chiropractic services in the Medicare Program: payment vulnerability analysis
(OEI-09-02-00530). 2005Office of the Inspector General.
Inappropriate Medicare Payments for Chiropractic Service PDF
Washington, DC: US Department of Health and Human Services; 2009U.S. Department of Health and Human Services,
Office of the Inspector General
Hundreds of millions in Medicare payments for chiropractic services did not comply with Medicare requirements
A-09-14-02033). 2016Whedon JM, Goertz CM, Lurie JD, Stason WB.
Beyond Spinal Manipulation: Should Medicare Expand Coverage for Chiropractic Services?
A Review and Commentary on the Challenges for Policy Makers
Journal of Chiropractic Humanities 2013 (Aug 28); 20 (1): 9–18Davis, MA, Yakusheva, O, Gottlieb, DJ, and Bynum, JP.
Regional Supply of Chiropractic Care and Visits to
Primary Care Physicians for Back and Neck Pain
J American Board of Family Medicine. 2015 (Jul); 28 (4): 481–490Davis MA, Yakusheva O, Liu H, et al.
Access to Chiropractic Care and the Cost of Spine Conditions Among Older Adults
American Journal of Managed Care 2019 (Aug); 25 (8): e230–e236Cher BAY Yakusheva O Liu H Bynum JPW Davis MA.
The effect of healthcare provider availability on spine spending.
J Gen Intern Med. 2021; 36: 654-661Center for Medicaid and Medicare Services,
Center for Program Integrity, Provider Enrollment Oversight Group.
Crosswalk Medicare provider/supplier to healthcare provider taxonomy.
2017 (Available at:)
https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/
MedicareProviderSupEnroll/Downloads/TaxonomyCrosswalk.pdf
Date accessed: February 7, 2021Luo W Wang F.
Measures of spatial accessibility to health care in a GIS environment:
synthesis and a case study in the Chicago region.
Environ Plann B. 2003; 30: 865-884McGrail MR.
Spatial accessibility of primary health care utilising the two step
floating catchment area method: an assessment of recent improvements.
Int J Health Geogr. 2012; 11: 50Naylor KB Tootoo J Yakusheva O Shipman SA Bynum JPW Davis MA.
Geographic variation in spatial accessibility of U.S. healthcare providers.
PLoS One. 2019; 14e0215016Cherkin DC Deyo RA Volinn E Loeser JD.
Use of the International Classification of Diseases (ICD-9-CM) to identify
hospitalizations for mechanical low back problems in administrative databases.
Spine (Phila Pa 1976). 1992; 17: 817-825Martin, BI, Deyo, RA, Mirza, SK et al.
Expenditures and Health Status Among Adults With Back and Neck Problems
JAMA 2008 (Feb 13); 299 (6): 656–664Lurie JD Birkmeyer NJ Weinstein JN.
Rates of advanced spinal imaging and spine surgery.
Spine (Phila Pa 1976). 2003; 28: 616-620Centers for Disease Control and Prevention
Analyzing prescription data and morphine milligram equivalents. 2016 (Available at:)
https://www.cdc.gov/drugoverdose/resources/data.html
Date accessed: February 7, 2020Deyo RA Cherkin DC Ciol MA.
Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases.
J Clin Epidemiol. 1992; 45: 613-619Association of American Medical Colleges.
The complexities of physician supply and demand: projections from 2018 to 2033. Available at:
https://www.aamc.org/system/files/2020-06/stratcomm-aamc-physician-
workforce-projections-june-2020.pdf
Accessed February 7, 2021.Nelson CF Metz RD LaBrot T.
Effects of a Managed Chiropractic Benefit on the Use of Specific Diagnostic
and Therapeutic Procedures in the Treatment of Low Back and Neck Pain
J Manipulative Physiol Ther 2005 (Oct); 28 (8): 564–569Fritz JM, Kim J, Dorius J.
Importance of the Type of Provider Seen to Begin Health Care for a New Episode
Low Back Pain: Associations with Future Utilization and Costs
J Eval Clin Pract. 2016 (Apr); 22 (2): 247–252Corcoran KL, Bastian LA, Gunderson CG, et al.
Association Between Chiropractic Use and Opioid Receipt Among Patients with Spinal Pain:
A Systematic Review and Meta-analysis
Pain Medicine 2020 (Feb 1); 21 (2): e139–e145Weeks WB, Goertz CM.
Cross-Sectional Analysis of Per Capita Supply of Doctors of Chiropractic
and Opioid Use in Younger Medicare Beneficiaries
J Manipulative Physiol Ther 2016 (May); 39 (4): 263–266Center for Disease Control and Prevention.
Annual surveillance report of drug-related risks and outcomes,
United States 2019. Available at:
https://www.cdc.gov/drugoverdose/pdf/pubs/2019-cdc-drug-surveillance-report.pdf
Accessed February 7, 2021.Allen H Wright M Craig T et al.
Tracking Low Back Problems in a Major Self-Insured Workforce:
Toward Improvement in the Patient's Journey
J Occupational and Environmental Medicine 2014 (Jun); 56 (6): 604–620
Return to MEDICARE
Return to COST-EFFECTIVENESS
Since 1-22-2021


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |