

Patient Willingness to Pay for Reductions in
Chronic Low Back Pain and Chronic Neck PainThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Pain 2019 (Nov); 20 (11): 1317–1327 ~ FULL TEXT
OPEN ACCESS Patricia M Herman, Jill E Luoto, Mallika Kommareddi, Melony E Sorbero, Ian D Coulter
RAND Health, RAND Corporation,
Santa Monica, California
Many recommended nonpharmacologic therapies for patients with chronic spinal pain require visits to providers such as acupuncturists and chiropractors. Little information is available to inform third-party payers' coverage policies regarding ongoing use of these therapies. This study offers contingent valuation-based estimates of patient willingness to pay (WTP) for pain reductions from a large (n = 1,583) sample of patients using ongoing chiropractic care to manage their chronic low back and neck pain. Average WTP estimates were $45.98 (45.8) per month per 1-point reduction in current pain for chronic low back pain and $37.32 (38.0) for chronic neck pain. These estimates met a variety of validity checks including that individuals' values define a downward-sloping demand curve for these services. Comparing these WTP estimates with patients' actual use of chiropractic care over the next 3 months indicates that these patients are likely "buying" perceived pain reductions from what they believe their pain would have been if they didn't see their chiropractor-that is, they value maintenance of their current mild pain levels.
These results provide some evidence for copay levels and their relationship to patient demand, but call into question ongoing coverage policies that require the documentation of continued improvement or of experienced clinical deterioration with treatment withdrawal.
PERSPECTIVE: This study provides estimates of reported WTP for pain reduction from a large sample of patients using chiropractic care to manage their chronic spinal pain and compares these estimates to what these patients do for care over the next 3 months, to inform coverage policies for ongoing care.
Keywords: Chronic low back pain; chiropractic care; chronic neck pain; willingness to pay.
From the FULL TEXT Article:
Introduction
Over 40 percent of adults in the US experience chronic pain, often chronic spinal (back and neck) pain, [30, 31] and this pain is expensive to the healthcare system [32] and to employers. [43] Recently a number of nonpharmacologic interventions have been found to be safe and effective, and included in treatment guidelines for chronic spinal pain. [7, 38, 44, 45] The lists of recommended interventions include therapies that require ongoing visits to providers such as acupuncturists, physical therapists, and chiropractors.
At present healthcare payer plans provide limited coverage for these therapies, usually with substantial co-payments and/or limits on the number of visits when coverage is offered at all. [27] Guidelines contain some information about ongoing treatment plans for patients with chronic low-back pain (hereafter, back pain) and chronic neck pain (hereafter, neck pain), [4, 5, 10, 11, 21, 23, 24] but the underlying evidence base is slim to non-existent. Care beyond the initial course of treatment usually requires documentation of continued improvement, [10, 11, 21, 23, 24] or of clinical deterioration with treatment withdrawal. [21] Given the chronic (i.e., long-term) nature of back and neck pain, the likely necessity for some type of ongoing care, and the substantial out-of-pocket and other costs patients face in seeing these providers, policy makers could benefit from information on how current patients are making decisions regarding their use of these providers for long-term chronic pain management.
One aspect of patients’ decisions is the value they place on chronic pain reduction. There are several ways to put a monetary value on a health benefit, [19] pp215–241 yet very little is known about patient willingness-to-pay (WTP) to manage chronic spinal pain. While WTP estimates have been criticized as providing only “hypothetical answers,” they can help inform policy on appropriate out-of-pocket expenses for care when estimates reflect plausible real-life situations [42] — e.g., when obtaining WTP estimates from chronic spinal pain patients already in care and facing ongoing decisions as to whether further care is worthwhile.
One small Canadian study of patients with chronic pain used a discrete choice experiment to estimate a patient WTP of $1,428 per month to completely reduce pain and associated morbidity. [8] However, because the discrete choice scenarios included extremely severe symptoms and high out-of-pocket costs, this pain clinic-based study may not be applicable to the long-term use of providers of the recommended nonpharmacologic therapies by patients with moderate back pain. WTP estimates are needed for patients who have been managing their chronic spinal pain using providers of recommended nonpharmacologic therapies.
It would also be useful to “market test” the WTP estimates [35] by comparing what patients said regarding the value they placed on their symptom improvement to their behavior in terms of continued treatment over time. Roughly 30 percent of those with spinal pain have visited a chiropractor, [33] and many of these patients are under long-term chiropractic care to manage chronic pain. [12, 15, 26, 28, 37] Given the substantial out-of-pocket expenditures, [27] as well as other (e.g., time, travel) costs, associated with chiropractic visits, these patients are obviously willing to pay for this care. But what are they “buying”? Under long-term care some of these patients may have reached a symptom plateau, [10, 11, 21, 23, 24] and then continued care to keep their previous symptoms from returning. This information is important to inform ongoing coverage policies.
This study utilizes data collected from a large sample of chiropractic patients with back pain and/or neck pain to provide information regarding the care decision processes of patients who are using ongoing chiropractic care to manage their chronic spinal pain. We will provide estimates of patients’ reported WTP to reduce their chronic pain, and compare these to their revealed WTP as evidence of what patients’ are “buying” when they obtain chiropractic care.
Methods
This study uses longitudinal data collected from a US sample of patients under chiropractic treatment for non-specific back pain and/or neck pain. These data were collected as part of a larger project focused on the appropriateness of spinal manipulation and mobilization for chiropractic patients presenting with various subtypes of these conditions. The project used multistage systematic stratified sampling to capture 3 months of data on patients being seen at chiropractic clinics and their providers in six regions and metropolitan areas: San Diego, California; Tampa, Florida; Minneapolis, Minnesota; Seneca Falls/Upstate, New York: Portland, Oregon; and Dallas, Texas.
The goal of the sampling design was to recruit 20 chiropractors (clinics) per region and 7 back pain and 7 neck pain cases from each clinic. Each participating clinic was given an iPad and staff were trained to make the iPad’s short prescreening questionnaire available to every patient who visited the clinic during a 4-week period. The questionnaire established initial inclusion criteria (i.e., >21 years of age, English proficient, no present personal injury or workers compensation litigation, have back or neck pain). Those who met these criteria and provided an email address were invited to the study and sent a link to a longer screening questionnaire to determine whether they met the criteria for chronic back pain and/or neck pain (i.e., pain for at least 3 months before seeing the chiropractor and/or self-report of chronicity).
If they met these criteria they were consented, asked additional questions including on WTP, and then immediately sent a series of 7 more questionnaires over the next 3 months: a longer baseline questionnaire, 5 shorter biweekly questionnaires, and a final longer questionnaire at 3 months. This study used responses to WTP questions in the screening questionnaire, patient characteristics collected at baseline, and measures of pain, function, and healthcare utilization collected in each of the 7 questionnaires following the screening survey.
More detail on the overall project [13, 14] and more detail on data collection methods and sample characteristics [26] can be found elsewhere. It turned out that the patients in the sample have been in treatment for an average of 11 years, [26] thus they are likely all in some sort of ongoing care and continually making decisions about that care.
Measures
Our primary outcome measure, WTP was measured separately for each type of chronic pain. For patients with both back pain and neck pain, WTP information was collected only for the pain that they reported as worse at screening. Each patient was given two open-ended questions: one asking for their WTP to reduce pain to zero and one for pain reductions to half their present level. Following best practice for WTP elicitation, patients were reminded of their budget constraint before they responded, and the questions were developed and pre-tested during a pilot study. [42] The WTP questions asked, “Thinking about what you can afford to pay on a monthly basis, how much would you be willing and able to pay out-of-pocket per month for your pain to be reduced by half? (to go to zero?).” The two questions allowed a test of the validity of the WTP responses. We expect reports of higher WTP for greater levels of pain reduction. WTP values from open-ended questions, such as we used, are known to be unbiased, and although values for public goods (e.g., open park space) from open-ended questions have been found to be widely varying, imprecise and plagued by non-response, [19] opened-ended values for private goods such as healthcare have been shown to be valid. [2, 41]
At each data collection point all patients reported their average pain levels over the past 7 days (pain numerical rating scale or NRS [29]), and their present function using the 10-item Neck Disability Index (NDI) [47] for those with neck pain and the 10-item Oswestry Disability Index (ODI) [20] for those with back pain. These measures are all recommended for use in their respective populations and have a substantial literature on their validity and reliability
pain NRS [3, 6, 18, 36, 40],
NDI [9, 34, 46, 48],
ODI [17, 22, 25].
Using similar pain scales, we also asked patients what their pain levels would have been (i.e., their projected pain) for back pain and neck pain if they had not continued in chiropractic treatment. These questions were added after focus groups and piloting found that some patients reported zero levels of pain, and that many patients viewed their ongoing chiropractic treatments as a means to manage their pain. Patients’ expected increase in (return of) pain if chiropractic care ended was calculated as projected pain minus actual pain.
In the screener questionnaire participants were asked whether their health insurance covered any of the cost of their chiropractic visits. Those with any coverage were then asked their average out-of-pocket costs per chiropractic visit. We used the chiropractor’s reported full cost per visit for those without chiropractic coverage. On every questionnaire after baseline participants reported the number of chiropractic visits since the last data collection point. Other variables captured patients’ income level, years with pain, and whether they had both back pain and neck pain, worked full or part-time, and had depression according to the 4-item depression scale from the PROMIS-29 (scores >52.5). [1]
Analysis
We descriptively examined patients’ pain, function, visit costs and frequency, and patient characteristics between three samples of participants who reported WTP for back or neck pain. We used ANOVA (continuous), and χ2 or Fisher’s exact tests (categorical) to examine the comparability between the Full Sample (all those who provided an estimate of WTP at screening), Revealed WTP Sample (those who stated a WTP at screening and had chiropractic visits afterwards), and the Pain Reduction Sample (those who had a reduction in both actual pain and projected pain by the end of the study).
After trimming WTP values above the 99th percentile, we averaged respondents’ WTP to reduce either their back or neck pain to zero or by half and tested the reasonableness of these estimates in several ways. First, we compared the reduce-to-zero to the reduce-by-half estimates; the reduce to zero values should be larger. Next, we construct demand curves for pain reduction; that is, graphed the proportion of the sample willing to pay any given price for a given pain reduction. These curves allowed us to examine the full distribution – not just mean – of the WTP estimates. Finally, we examine the relationships between WTP and the variables that should be related — e.g., income and pain levels. Because WTP tends to be right-skewed, we used ordinary least squares (OLS) estimation on logtransformed WTP. In base models for back pain and neck pain we included as predictive variables patient actual pain and projected pain, as well as demographic information including income, employment status, and years of experienced pain. Errors were clustered at the level of clinics to account for unobserved correlations within clinics. We then estimated more sophisticated versions of this model by including additional patient variables (age, sex, presence of depression, and level of education), as well as clinic fixed effects to control for any unobserved time-invariant clinic-level attributes affecting patient WTP. With the log transformation for WTP, coefficients in these models represent the percentage change in WTP from a one-unit change in the covariate of interest.
Because their pain levels differed, different patients were referencing different amounts of pain reduction when asked for their WTP. Therefore, we put the WTP estimates on a per-unit-of-pain-reduced basis. Since it is unclear if patient stated WTP relates to reductions in their current experienced pain or projected pain in the absence of regular chiropractic care, we calculated individuals’ stated WTP per point reduction of each — i.e., stated WTP for a reduction to zero divided by actual pain, stated WTP for a reduction to zero divided by projected pain, stated WTP for a reduction by half divided by half of actual pain, and stated WTP for a reduction by half divided by half of projected pain,.
Revealed WTP per month was calculated for each patient in the Revealed WTP Sample as each participants’ average number of chiropractic visits per month over the next 3 months multiplied by the amount paid out-of-pocket for each visit. Only those in the Full Sample who had visits after baseline were included in the Revealed WTP Sample. The estimate of costs per month was then put on a per-point-reduction-in-pain basis by dividing by each of three versions of the pain reduction these patients could be “buying”: reductions in actual pain over the month, reductions in projected pain over the month, and the average “reduction” in pain experienced with every visit — i.e., the expected reduction from projected pain to actual pain. Reductions in actual pain and in projected pain over the month are estimated based on each patients’ slope (change by weeks since baseline) estimated using hierarchical linear modeling with fixed effects and person-level random intercepts and slopes. Only those in the Revealed WTP Sample who experienced reductions in these measures of pain were included in the Pain Reduction Sample.
Our comparison of ex ante stated WTP and ex post reported actual behaviors (revealed WTP) served as another robustness check on the stated WTP results. Given the salience of regular expenditures on chiropractic care for these patients, we would expect stated WTP to be roughly equal to revealed WTP (out-of-pocket chiropractic visit costs). However, it could also be somewhat higher or lower. It could be higher because stated WTP may include more than patient out-of-pocket chiropractic visit costs — e.g., patients’ time and transportation costs or costs of any non-chiropractic visits. Stated WTP could also be higher due to stated preference bias — i.e., respondents may overstate WTP because they are not held liable to actually pay these amounts. Stated WTP could also be lower than revealed WTP if patients are obtaining something of value other than simple pain reduction from these visits — e.g., functional improvement, or exercise and lifestyle advice. Nevertheless, we can use comparisons between stated and revealed WTP to help understand what patients are “buying” with their out-of-pocket chiropractic visit costs.
All analyses were performed in R 3.4.4. [39] This study was approved by the RAND Human Subjects Protection Committee and each participant gave consent before answering any of the questionnaires.
Results
Of the 2,024 participants in the baseline survey,26 1,708 had non-specific back or neck pain, and 1,583 (92.7%) of those answered the WTP questions — 865 about reducing low-back pain and 718 about reducing neck pain. We trimmed WTP values above the 99th percentile for back pain to $1000 for reducing pain to zero and $536 for reducing pain by half. Maximum WTP values reported for back pain were $10,000 per month for reducing their pain to zero and $2,000 per month for reducing pain by half. Trimming WTP values above the 99th percentile for neck pain reduced those values to $1000 for reducing pain to zero and $500 for reducing pain by half. Maximum WTP values reported for neck pain were $1,000,000 per month for reducing their pain to zero or by half.

Table 1

Table 2 Table 1 presents descriptive socioeconomic statistics for each primary pain type for the Full Sample and the two subsamples. The average age was over 48 years for patients with back pain and almost 46 years for neck pain. Females were in the majority of all samples, but especially in the neck pain sample of which they comprised more than 80%. Almost half of all samples had chronic pain for over 10 years. Differences in income and other patient characteristics between the samples were small and generally non-significant.
Table 2 shows the estimates of patients’ WTP for pain reduction using different measures of pain. As expected estimates of WTP for pain reduced to zero were higher than WTP estimates for reducing pain by half. The differences in these estimates were small and not statistically significant across the full and subsamples for back pain and neck pain patients. If patients were thinking about their current level of experienced pain when reporting on their WTP for their pain to be reduced to zero, their WTP was almost $46 per month per 1-point reduction for the full back pain sample and just over $37 for the full neck pain sample. If patients were thinking about projected pain when making their WTP estimates, because projected pain was higher than current pain, WTP estimates per month per 1-point reduction were lower: almost $26 for back pain and just over $21 for neck pain. Overall, back pain patients were willing to pay more than neck pain patients, and estimates of WTP per month per 1-point reduction were higher when based on the estimates given for WTP when pain was reduced by half than when based on estimates for pain reduced to zero. This may indicate that initial pain reductions are worth more than later reductions as pain approaches zero. The Pain Reduction Sample had significantly lower pain scores resulting in their WTP per 1-point reduction to be slightly (but significantly in the case of back pain) higher.
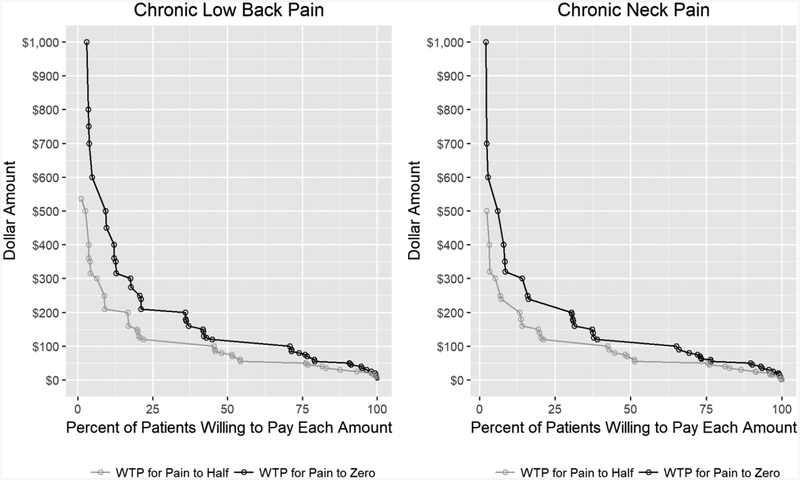
Figure 1 Figure 1 shows demand curves for pain reduction based on reported WTP for patients with back pain and neck pain. These curves illustrate the full distribution of stated WTP and demonstrate that the share of patients willing to pay for pain reduction decreases as price increases. These graphs also demonstrate that the proportion of patients willing to pay for complete pain reduction (i.e., to zero) was everywhere higher than the proportion willing to pay for reductions in pain levels by half. This evidence of everywhere downward-sloping demand curves based on the stated WTP data lends credibility to our collected estimates. We also see high rates of dispersion in WTP among our samples. For example, over 70% of those with back pain have WTP of at least $100 per month for full pain reduction but less than 25% have WTP of more than $200 per month. We see a similarly range in WTP for pain reductions for the neck pain sample across the $100-$200 price range – about 65% of the sample is willing to pay up to $100 monthly for complete pain reduction in neck pain but just over 30% are willing to pay $200 or more.

Table 3 Table 3 presents the results of regression models examining the predictors of stated WTP for our back pain and neck pain Full Samples. As expected, patients experiencing higher levels of pain reported higher WTP to have their pain reduced to zero. A 1-point increase in pain was associated with a 6% increase in WTP for those with back pain, and with a 7% increase in WTP for those with neck pain. The difference between patients’ current pain and what they report that their pain would have been if they did not see the chiropractor (an estimate of patients’ expected pain increase if chiropractic care ended) was significantly associated with higher WTP for neck pain, but not back pain patients. Also, as expected, income is positively associated with WTP. Although only the $100,000 to $199,000 income category coefficients tend to be statistically significant, estimated coefficients generally increase across income categories. The inclusion of additional explanatory variables in the full models caused little change in the coefficients estimated, but added the information that women reported 16% lower WTP than men and those aged 65 years or more reported 43% lower WTP than those less than age 30 for reductions in lowback pain.
Table 4 shows inputs to and the resulting estimates of patients’ out-of-pocket expenditures (revealed WTP) per 1-point reduction in three different measures of pain. Patients report an average of just over 12 chiropractic visits in the 6 months before baseline (i.e., biweekly visits on average), and those who go on to continue care (Revealed WTP Sample) report a consistent 6 to 7 visits over the next 3 months. There were no statistically significant differences between the three samples in these estimates, nor in their reported out-of pocket costs per visit or over the 3 months. Patients reported an average cost per visit of $43 to $45 overall, but those with insurance coverage paid less and those without coverage paid about $30 more. The average total out-of-pocket cost for chiropractic over the 3-month study period was just over $300, or about $100 per month. Over the 3-month study period, patients in the Pain Reduction Sample had small average reductions in actual pain of three-quarters of a point (one-quarter point per month) and average reductions in projected pain of almost one point (one-third point per month). If either of these pain reductions were what these patients were “buying” with their out-of-pocket investment in chiropractic visits, they were paying roughly $700 to $800 per 1-point reduction — an amount more than ten times their stated WTP. One other measure of pain reduction was what patients thought they experienced with every chiropractic visit – the difference between current pain and what patients believed their pain would have been if they did not see their chiropractor. This reduction averaged about 3 points across samples. If this was the pain reduction patients were “buying” their revealed WTP per 1-point reduction was then about $36 for back pain and about $42 for neck pain—amounts much closer to their stated WTP.
Discussion
Our stated WTP estimates, while subject to the same pitfalls as any stated preference measure, show remarkable consistency across pain types and subsamples. They also demonstrate several reasonable qualities: estimates for full reductions in pain that were higher than for half reductions, and downward sloping demand curves where the curves for full pain reduction were everywhere higher than those for half reductions. The regression results agree with intuitions that income is positively correlated with WTP (i.e., those with higher income can afford to pay more), and that pain levels are positively correlated with WTP (i.e., reducing higher pain levels to zero should be worth more than reducing lower levels). Finally, these estimates stand up to scrutiny when compared to “revealed” estimates of WTP based on what patients subsequently pay for treatment over the ensuing months—at least in terms of one set of revealed estimates.
Beyond the WTP estimates themselves, which may be useful to coverage policy regarding patient out-of-pocket payments (e.g., co-pays), their comparison to revealed WTP can also provide evidence regarding the version of pain reduction these patients are “buying” when they pay to visit their chiropractor. Based on our results, it does not seem that patients are buying reductions in their actual pain. Those reductions were so small over the study period that it would mean patients were paying $700 to $800 per month per 1-point reduction, numbers that stand in stark contrast to our consistent WTP estimates of $20 to $56 per month per 1-point reduction in pain across several samples, levels of pain reduction (reduce to zero or by half), pain measures (actual pain and projected pain), and types of pain (back pain and neck pain). Instead, it seems that patients are buying (i.e., making their day-to-day decisions based on) the difference between their current pain and projected pain if they did not see their chiropractor. Under this assumption, back pain patients are paying $36 per month per 1-point reduction in pain from what it would have been, and neck pain patients are paying about $42, values well within the range of what patients state they are willing to pay.
If patients are valuing and making ongoing treatment decisions based on their ability to maintain their current pain levels and to avoid what they believe their pain would be without treatment, this has implications for coverage policy. Coverage policies that require documentation of continued improvement with treatment, or experienced and documented deterioration without treatment, for each extension of coverage are inconsistent with patients’ values and decision making regarding ongoing care for their chronic conditions.
We are aware of one other study that used another survey-based method (a discrete choice experiment) to estimate patients’ WTP for reductions in chronic pain and pain-related disability. [8] The participants (n=78) were all patients in a pain clinic and their estimated WTP for complete symptom relief was $1,428 out-of-pocket per month. As can be seen, their estimate was approximately 7 to 9 times higher than our monthly Full Sample WTP estimates for pain reduced to zero of $184 for back pain patients and $158 for patients with neck pain. There are several reasons for these large differences.
First, the $1,428 per month estimate was the value for patients to go from excruciating pain and total disability to mild pain and disability. Our sample’s pain and disability scores under chiropractic care put them near mild pain and disability already. Second, our WTP was only for pain reduction, whereas, these patients’ WTP incorporated reductions in both pain and disability. Third, these patients were primed with higher estimates of out-of-pocket costs than experienced by our sample: $100 to $1000 per month. Finally, discrete choice experiment methods often find higher WTP than does open-ended, contingent valuation methods. [2, 16] This study’s WTP estimate for a one-category drop in pain (from excruciating to severe) was $225, a number much closer to our estimates.
Our study benefits from large samples of patients with chronic low-back and neck pain who have been using chiropractic care long-term to manage their symptoms, but it also has limitations. Our study is observational and depends on patients’ reports of their WTP for something likely not possible: reduction of their pain to zero. Therefore, it is subject to all the challenges of stated preference bias. Our estimates of WTP were made by individuals who were in ongoing chiropractic care often for many years and regularly making decisions regarding their WTP, and who had just been reminded of what they were currently paying. These conditions likely contributed to the fact that our estimates have good consistency and validity, but they should still be interpreted with caution. For example, our estimates would not apply to patients who have never used or are just beginning chiropractic care. In addition, since our sample was of current chiropractic patients, our estimates represent WTP for those who choose and can afford to pay for these services. This study offers little information on what WTP would be for those who could benefit from chiropractic care but can’t afford it. It is also unclear as to whether these estimates provide any information for coverage policies for other therapies or for use of chiropractic for other conditions.
Patients with back pain and neck pain under ongoing chiropractic care report an average WTP of between $20 and $55 per month per 1-point reduction in pain. Based on this, it is clear that these patients are willing to pay some level of out-of-pocket costs for this care. The demand curves show that the number of patients willing to pay each dollar amount for this pain reduction decreases as the price increases and there is wide dispersion in response, therefore, demand for these services can be somewhat controlled through the amount patients are required to pay out-of-pocket. However, if the use of chiropractic or other of the recommended nonpharmacologic therapies is to be promoted, some reduction in out-of-pocket costs should be considered, especially for those with lower incomes and higher levels of pain. These patients also seem to make their care decisions based on the difference between their current pain and what they believe their pain would be if they didn’t receive chiropractic care. Therefore, coverage decisions that require continued improvement or documentation clinical deterioration with treatment withdrawal are inconsistent with successful pain management. Future studies that examine the impact of lower out-of-pocket costs on the use of providers of nonpharmacologic therapies by those with lower incomes, and studies that consider successful symptom management as a criterion for ongoing coverage are warranted.
Highlights
Willingness to pay for a 1-point reduction in chronic back pain was $45.98 per month.
Willingness to pay for a 1-point reduction in chronic neck pain was $37.32 per month.
These estimates met a variety of validity checks including downward-sloping demand.
Patients reported that their pain would be higher without chiropractic visits.
Comparing stated WTP to visit costs indicates patients pay to avoid this higher pain.
Funding:
This work was supported by the National Center for Complementary and Integrative Health of the National Institutes of Health [grant number 1U19AT007912–01]
Conflicts of Interest:
The authors declare that they have none.
References:
Amtmann D, Kim J, Chung H, Bamer AM, Askew RL, Wu S, Cook KF, Johnson KL.
Comparing CESD-10, PHQ-9, and PROMIS depression instruments
in individuals with multiple sclerosis.
Rehabil. Psychol 59:220, 2014Balistreri E, McClelland G, Poe G, Schulze W.
Can hypothetical questions reveal true values? A laboratory comparison
of dichotomous choice and open-ended contingent values with auction values.
Environ. Resource Econ 18:275–292, 2001Bijur PE, Latimer CT, Gallagher EJ.
Validation of a verbally administered numerical rating scale
of acute pain for use in the emergency department.
Academic emergency medicine. 10:390–392, 2003California Division of Workers’ Compensation.
Medical Treatment Utilization Schedule (MTUS)
Chronic Pain Guideline
Medical Treatment Guidelines State of California,
Sacramento, CA, 2017Canadian Chiropractic Association and
Canadian Federation of Chiropractic Regulatory Boards
Chiropractic Clinical Practice Guideline:
Evidence-based Treatment of Adult Neck Pain Not Due to Whiplash
J Canadian Chiro Assoc 2005 (Sep); 49 (3): 158–209Childs JD, Piva SR, Fritz JM.
Responsiveness of the numeric pain rating scale in patients with low back pain.
Spine. 30:1331, 2005Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, et al.
Nonpharmacologic Therapies for Low Back Pain: A Systematic Review
for an American College of Physicians Clinical Practice Guideline
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 493–505Chuck A, Adamowicz W, Jacobs P, Ohinmaa A, Dick B, Rashiq S.
The willingness to pay for reducing pain and pain-related disability.
Value Health. 12:498–506, 2009Cleland JA, Fritz JM, Whitman JM, Palmer JA.
The reliability and construct validity of the Neck Disability Index
and patient specific functional scale in patients with cervical radiculopathy.
Spine. 31:598–602, 2006Colorado Division of Workers’ Compensation.
Cervical Spine Injury Medical Treatment Guidelines
Denver, CO, Revised: February 3, 2014Colorado Division of Workers’ Compensation.
Low Back Pain Medical Treatment Guidelines
Denver, CO, Revised: February 3, 2014Cooper RA, McKee HJ.
Chiropractic in the United States: trends and issues.
Milbank Q. 81:107–138, 2003Coulter ID, Herman PM, Ryan GW, Hays RD, Hilton LG, Whitley MD.
Researching the Appropriateness of Care in the Complementary
and Integrative Health Professions: Part I
J Manipulative Physiol Ther. 2018 (Nov); 41 (9): 800–806Coulter ID, Herman PM, Ryan GW, Hays RD, Hilton LJ, CERC Team.
The Challenge of Determining Appropriate Care in the Era of
Patient-Centered Care and Rising Health Care Costs.
J. Health Serv. Res. Policy [in press], 2018Coulter ID, Shekelle PG.
Chiropractic in North America: a descriptive analysis.
J Manip Physiol Ther. 28:83–89, 2005Danyliv A, Pavlova M, Gryga I, Groot W.
Willingness to pay for physician services: Comparing estimates
from a discrete choice experiment and contingent valuation.
Society and Economy. 34:339–357, 2012Davidson M, Keating JL.
A Comparison of Five Low Back Disability Questionnaires:
Reliability and Responsiveness
Physical Therapy 2002 (Jan); 82 (1): 8–24Downie W, Leatham P, Rhind V, Wright V, Branco J, Anderson J.
Studies with pain rating scales.
Annals of the Rheumatic Diseases. 37:378–381, 1978Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL:
Methods for the Economic Evaluation of Health Care Programmes.
3rd edition, Oxford University Press, Oxford, 2005.Fairbank J, Couper J, Davies J, O’brien J.
The Oswestry low back pain disability questionnaire.
Physiotherapy. 66:271–273, 1980Farabaugh RJ, Dehen MD, Hawk C.
Management of Chronic Spine-Related Conditions:
Consensus Recommendations of a Multidisciplinary Panel
J Manipulative Physiol Ther 2010 (Sep); 33 (7): 484–492Fisher K, Johnston M.
Validation of the Oswestry low back pain disability questionnaire,
its sensitivity as a measure of change following treatment and
its relationship with other aspects of the chronic pain experience.
Physiotherapy theory and practice. 13:67–80, 1997Globe, G, Farabaugh, RJ, Hawk, C et al.
Clinical Practice Guideline:
Chiropractic Care for Low Back Pain
J Manipulative Physiol Ther. 2016 (Jan); 39 (1): 1–22Globe GA, Morris CE, Whalen WM, et al.
Chiropractic Management of Low Back Disorders:
Report From a Consensus Process
J Manipulative Physiol Ther 2008 (Nov); 31 (9): 651–658Grönblad M, Hupli M, Wennerstrand P, Järvinen E, Lukinmaa A, Kouri J-P, Karaharju EO.
Inter-correlation and test-retest reliability of the pain disability index (PDI)
and the Oswestry disability questionnaire (ODQ) and their correlation
with pain intensity in low back pain patients.
The Clinical journal of pain. 9:189–195, 1993Herman P, Hilton L, Sorbero ME, et al
Characteristics of Chiropractic Patients Being Treated
for Chronic Low Back and Neck Pain
J Manipulative Physiol Ther. 2018; 41: 445–455Heyward J , Jones CM , Compton WM , et al .
Coverage of Nonpharmacologic Treatments for Low Back Pain
Among US Public and Private Insurer
JAMA Network Open 2018 (Oct 5); 1 (6): e183044Hurwitz, EL.
Epidemiology: Spinal Manipulation Utilization
J Electromyogr Kinesiol. 2012 (Oct); 22 (5): 648–654Huskisson E
Measurement of pain.
The Lancet. 304:1127–1131, 1974Institute of Medicine (IOM)
Relieving Pain in America: A Blueprint for Transforming Prevention,
Care, Education, and Research
Washington, DC: The National Academies Press, 2011.Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH.
The prevalence of chronic pain in United States adults:
results of an Internet-based survey.
J Pain. 11:1230–1239, 2010Martin, BI, Deyo, RA, Mirza, SK et al.
Expenditures and Health Status Among Adults With Back and Neck Problems
JAMA 2008 (Feb 13); 299 (6): 656–664Martin, BI, Gerkovich, MM, Deyo, RA et al.
The Association of Complementary and Alternative Medicine Use
and Health Care Expenditures for Back and Neck Problems
Medical Care 2012 (Dec); 50 (12): 1029–1036McCarthy MJH, Grevitt M, Silcocks P, Hobbs G.
The Reliability of the Vernon and Mior Neck Disability Index,
and its Validity Compared With the Short Form-36
Health Survey Questionnaire
European Spine Journal 2007 (Dec); 16 (12): 2111–2117Olsen JA, Smith RD.
Theory versus practice: a review of ‘willingness-to-pay’
in health and health care.
Health Economics. 10:39–52, 2001Paice JA, Cohen FL.
Validity of a verbally administered numeric rating scale
to measure cancer pain intensity.
Cancer nursing. 20:88–93, 1997Posner J, Glew C.
Neck Pain.
Ann. Intern. Med 136:758–759, 2002Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530R Core Team: R:
A language and environment for statistical computing,
R Foundation for Statistical Computing, Vienna, Austria, 2018Salaffi F, Stancati A, Silvestri CA, Ciapetti A, Grassi W.
Minimal clinically important changes in chronic musculoskeletal
pain intensity measured on a numerical rating scale.
European journal of pain. 8:283–291, 2004Smith RD.
The discrete-choice willingness-to-pay question format in
health economics: should we adopt environmental guidelines?
Medical Decision Making. 20:194–206, 2000Smith RD.
Construction of the contingent valuation market in health care: a critical assessment.
Health Economics. 12:609–628, 2003Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R.
Lost Productive Time and Cost Due to Common Pain Conditions in the US Workforce
JAMA 2003 (Nov 12); 290 (18): 2443–2454The Diagnosis and Treatment of Low Back Pain Work Group.
VA/DoD Clinical Practice Guideline for Diagnosis and Treatment of Low Back Pain PDF
Washington, DC: The Office of Quality, Safety and Value, VA, &
Office of Evidence Based Practice, U.S. Army MedicalCommand, 2017, Version 2.0.The Joint Commission.
Non-pharmacologic and Non-opioid Solutions for Pain Management
Quick Safety Issue 44 | August 2018Vernon H
The Neck Disability Index: State-of-the-Art, 1991-2008
J Manipulative Physiol Ther 2008 (Sep); 31 (7): 491–502Vernon H, Mior S
The Neck Disability Index: A Study of Reliability and Validity
J Manipulative Physiol Ther 1991 (Sep); 14 (7): 409–415Wheeler AH, Goolkasian P, Baird AC, Darden BV.
Development of the Neck Pain and Disability Scale:
item analysis, face, and criterion-related validity.
Spine. 24:1290, 1999
Return to LOW BACK PAIN
Since 1-04-2022


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |
