Initial Choice of Spinal Manipulation Reduces
Escalation of Care for Chronic Low Back Pain
Among Older Medicare BeneficiariesThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Spine (Phila Pa 1976) 2022 (Feb 15); 47 (4): E142E148 ~ FULL TEXT
OPEN ACCESS James M Whedon, DC, MS Anupama Kizhakkeveettil, BAMS (Ayurveda), MAOM, PhD
Andrew WJ Toler, MS Serena Bezdjian, PhD Daniel Rossi Sarah Uptmor, DC
Todd A. MacKenzie, PhD Jon D Lurie, MD, MS Eric L. Hurwitz, DC, MS, PhD
Ian Coulter, PhD Scott Haldeman, DC, MD, PhD
Southern California University of Health Sciences,
Whittier, CA, USA
Geisel School of Medicine at Dartmouth,
Hanover, NH, USA.
Study design: We combined elements of cohort and crossover-cohort design.
Objective: The objective of this study was to compare long-term outcomes for Spinal Manipulative Therapy (SMT) and Opioid Analgesic Therapy (OAT) regarding escalation of care for patients with chronic low back pain (cLBP).
Summary of background data : Current evidence-based guidelines for clinical management of cLBP include both OAT and SMT. For long-term care of older adults, the efficiency and value of continuing either OAT or SMT are uncertain.
Methods: We examined Medicare claims data spanning a five-year period. We included older Medicare beneficiaries with an episode of cLBP beginning in 2013. All patients were continuously enrolled under Medicare Parts A, B, and D. We analyzed the cumulative frequency of encounters indicative of an escalation of care for cLBP, including hospitalizations, emergency department visits, advanced diagnostic imaging, specialist visits, lumbosacral surgery, interventional pain medicine techniques, and encounters for potential complications of cLBP.
Results: SMT was associated with lower rates of escalation of care as compared to OAT. The adjusted rate of escalated care encounters was approximately 2.5 times higher for initial choice of OAT vs. initial choice of SMT (with weighted propensity scoring: rate ratio 2.67, 95% CI 2.64-2.69, p < .0001).
There is more like this @ our:
MEDICARE Section and the:
NON-PHARMACOLOGIC THERAPY SectionConclusions: Among older Medicare beneficiaries who initiated long-term care for cLBP with opioid analgesic therapy, the adjusted rate of escalated care encounters was significantly higher as compared to those who initiated care with spinal manipulative therapy.
Level of Evidence: 3.
From the FULL TEXT Article:
INTRODUCTION
Chronic low back pain (cLBP) can be a major disabling health condition for older adults. [1] A systematic review that included over 135,000 individuals in 35 studies found that 70% to 85% of the elderly population experience an episode of LBP in their lifetime, and 90% have more than one episode. [2] In a nationally representative sample of 9,665 United States (US) adults with LBP, 19.3% were aged 65 years and older. [3] LBP can limit the ability of older adults to perform everyday tasks of walking, lifting, stooping, and other basic activities of daily life. [4] Compounding the human burden is the high cost of treating spinal pain. Among 154 medical conditions in 2016, the highest amount of healthcare spending was for spinal pain, at $134.5 billion, 30.3% of which was for patients aged 65 or older. [5] Increases in the prevalence of LBP among Medicare beneficiaries have been accompanied by dramatic increases in costs. [6] and increased expenditure for spine care interventions have not correlated with improved outcomes. [7] For many invasive and expensive spine care procedures there is insufficient evidence to justify their use. [8, 9] Efficiency in healthcare is recognized as one of six domains of health care quality. [10] In the management of cLBP, healthcare resources are often overutilized, [6] and in such cases, the care of cLBP may be described as unnecessarily escalated and therefore inefficient.
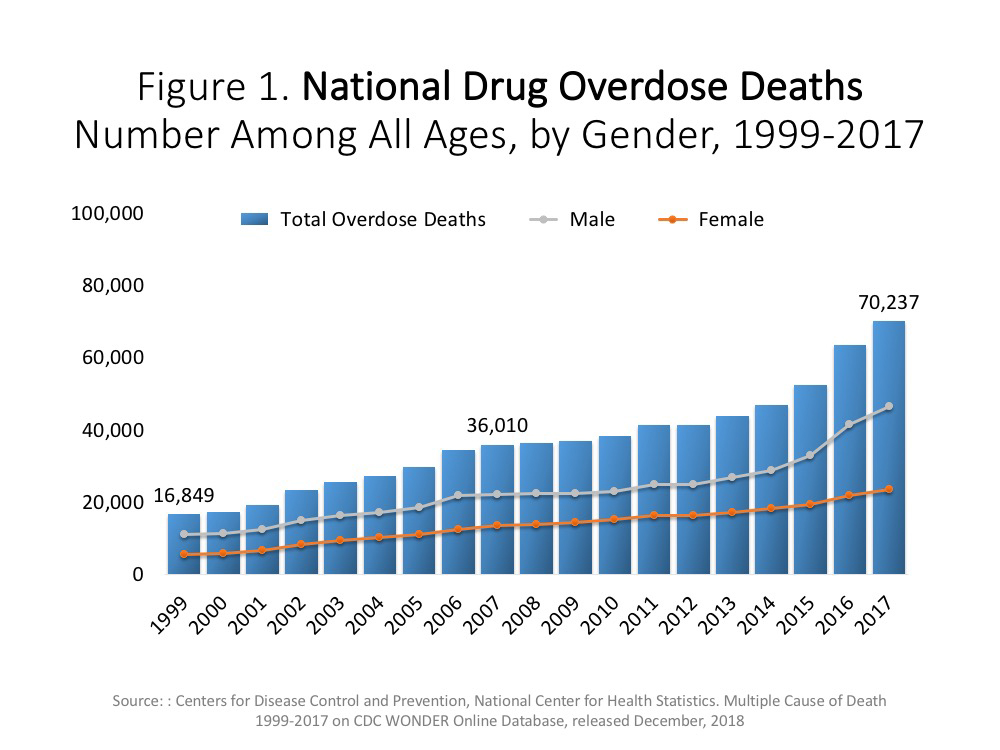
Current evidence-based guidelines for clinical management of cLBP include both pharmacological and non-pharmacological approaches. [11] Both Opioid Analgesic Therapy (OAT) [12] and Spinal Manipulative Therapy (SMT) [13] are provided to older adults with cLBP. The crisis of opioid overprescribing and the hazards of opioid use and misuse have been exhaustively documented. [14, 15] Compounding concerns about the safety of the long-term use of opioids, it is uncertain how utilization of OAT affects the escalation of care of cLBP [16] and thus the efficiency of clinical management. Similar concerns have been expressed about SMT. Although SMT is established as an evidence-based treatment for cLBP, [17, 18] a series of government reports found that frequent unnecessary SMT under Medicare resulted in excessive costs, particularly for maintenance care, in which SMT is provided on an ongoing long-term basis to prevent spinal problems from recurring or worsening. [1921]
Thus, for long-term care of cLBP, the efficiency and value of continuing either OAT or SMT are uncertain. The objective of this study was to compare long-term outcomes for SMT and OAT regarding escalation of care for patients with cLBP. We hypothesized that among older Medicare beneficiaries with cLBP, recipients of OAT have higher rates of escalated care for LBP, as compared with recipients of SMT.
METHODS
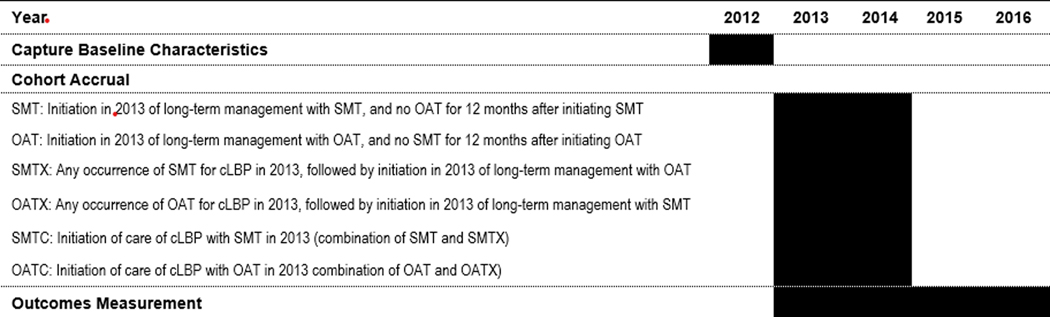
Figure 1 To test our hypothesis, we conducted a retrospective study using nationally representative samples (100% Parts A and B and 40% part D) of fee-for-service claims data spanning a five-year study period (20122016). We combined elements of cohort and crossover-cohort design to evaluate for comparative rates of selected healthcare outcomes. The study population included non-institutionalized Medicare beneficiaries enrolled in Parts A, B, and D, aged 6584 years and residing in a US state or the District of Columbia. We restricted the sample to persons with an episode of cLBP beginning in 2013. All included patients received long term management of cLBP with SMT or OAT. For OAT, we defined long-term management as 6 or more standard 30-day supply prescription fills in a 12-month period. [22, 23] For SMT, we defined long-term management as ?12 office visits for spinal manipulation for LBP in any 12-month period, including at least one visit per month. [21, 24-26] We assembled primary cohorts and crossover cohorts, and for purposes of analysis, combined cohorts based upon the patients first choice of treatment. [Figure 1]
As measures of lower socioeconomic status, we captured eligibility for Medicare Part D low-income subsidy and dual eligibility for both Medicare and Medicaid. We calculated Charlson comorbidity scores and collected data on diagnosis of comorbid chronic conditions that may confound the indication for opioids or affect prognosis for older adults with cLBP. For persons who received OAT, we also collected data on class of opioid prescribed at the time of cohort accrual. From the index date through 2016, we analyzed the cumulative frequency of encounters indicative of an escalation of care for cLBP. We also analyzed for encounters for potential complications of cLBP and spinal injuries, which may rarely occur as a complication of SMT of the lower back.
We tried to estimate the causal difference between initial choice of the two approaches to treatment. To estimate the adjusted incidence rate ratio, we conducted a comparison of outcomes between cohorts OATC and SMTC using Poisson regression with robust standard errors, controlling for individual characteristics and measures of health status including age, sex, race, state of residence, Charlson comorbidity index, LBP diagnostic category, and the presence of specific comorbidities such as hip or knee arthritis, depression, or fibromyalgia. We repeated this comparison using a propensity score approach. In the first step, we derived a model for the propensity of OAT vs SMT using a flexible logistic regression in terms of the covariates listed above. Next, we compared outcomes between OAT and SMT using both inverse weighted propensities and binned propensities (i.e., controlling for the categorical variable created by taking deciles of the propensity). A more detailed description of the methods may be viewed in the Appendix.
RESULTS

Table 1 Table 1 displays demographic characteristics and measures of health status by cohort. The overall study sample included 28,160 individuals: 4,998 individuals (18%) in cohort SMT, 20,947 (74%) in cohort OAT, 1,431 (5%) in cohort SMTX, 784 (3%) in cohort OATX, 6,429 individuals in cohort SMTC and 21,731 individuals in cohort OATC. Within all cohorts, average age at cohort accrual ranged between 72.6 and 73.1 years; approximately two thirds of persons were 74 years of age or younger. Females outnumbered males by approximately 3:1 within all cohorts. Persons who identified as White greatly outnumbered other racial/ethnic groups within all cohorts. The proportion of individuals with lower socioeconomic status was approximately five times higher in the OAT cohort, as compared to the SMT cohort. Comorbidity scores were also higher in the OAT cohort, with more than twice the proportion of patients with scores of 2, 3, or 4 in the OAT cohort as compared to the SMT cohort.
Most cases were categorized as non-specific LBP. There were higher proportions of individuals diagnosed with radiculopathy and spinal stenosis among patients who received only OAT, as compared to those who received only SMT. Cases of herniated disc and spondylolisthesis were also higher in the OAT cohort, while in the other three cohorts, the frequency of cases was so low that data suppression was required. Diagnosis of sprain/strain occurred infrequently, and frequency data in this category were suppressed for the crossover cohorts. Multiple comorbidities, including musculoskeletal conditions, were common among included persons and may have impacted their use of opioids.
Higher proportions of patients in the OAT cohort were diagnosed with depressive disorder and osteoarthritis of the hip or knee, as compared to the SMT cohort. Among the combined cohorts, choice of OAT as initial treatment was associated with indications of lower socioeconomic status, higher comorbidity scores, and higher rates of depressive disorder and osteoarthritis of the hip and knee.

Table 2

Table 3 As in the primary and crossover cohorts, most patients in the combined cohorts had non-specific LBP. Diagnoses of radiculopathy, spondylolisthesis and spinal stenosis were higher among patients who chose OAT as the initial approach to treatment. Most patients (8182%) who initially chose OAT were prescribed a schedule 2 opioid; approximately 3% were prescribed schedule 3, and 15% were prescribed a schedule 4 drug.
Table 2 displays the proportion by cohort of patients with at least one escalated care encounter. Escalated care encounters occurred in all cohorts, but in general, such encounters occurred most frequently in the OAT and OATC cohorts, in which patients chose OAT as the initial approach to care. The single exception to this pattern was the occurrence of spinal injury, which was more than 50% higher among patients who chose SMT as the initial approach to care. Spinal surgeries occurred infrequently, requiring suppression of rates in all cohorts. For cohort OATC vs. cohort SMTC, the adjusted rate of any escalated care encounter was 2.43 times higher with binned propensity scoring, and 2.67 times higher with weighted propensity scoring. [Table 3].
DISCUSSION
For long-term care of cLBP, the efficiency and value of continuing either OAT or SMT are uncertain. The objective of this study was to compare long-term outcomes for SMT and OAT regarding escalation of care for patients with cLBP. The results support our hypothesis that among older Medicare beneficiaries with cLBP, recipients of OAT have higher rates of escalated care for LBP, as compared with recipients of SMT. The results impact all included demographic groups, but predominately white women aged 6574. In their evaluation of propensity scoring methods for studies of Medicare claims, Weeks et al. found that the method of inverse weighting offered the advantage of maintaining sample size and preserving external validity. [27] Therefore, the better of the two estimates resulting from our regression analyses may be the higher rate ratio of 2.67, indicating that the rate of escalated care encounters was more than 2.5 times higher for patients who initiated care with OAT as compared to SMT. Higher rates of escalation of care suggest that care pathways for patients who initially choose OAT involve less efficient utilization of clinical resources.
Previous studies have reported reductions in clinical resource utilization for patients who saw a chiropractor first (CMS claims data on chiropractic services are equivalent to data on SMT, because SMT is the only chiropractic service covered under Medicare). [13] Keeney et al. reported that among patients with work-related back injuries, less than 2% of workers who first saw a chiropractor for their injury underwent surgery, as compared to 42% who first consulted a surgeon. [28] Several large-scale studies have found that utilization of chiropractic care is associated with decreased opioid use, [2931] and that early use of spinal manipulation may reduce unnecessary escalation of care, with greater efficiency and lower costs. [3234]
Pain, loss of function, and the adverse effects of pain medications can all put older patients with cLBP at risk of a fall, which can result in serious injury. Krebs et al. conducted a nine-year longitudinal cohort study of more than 2,900 men aged 65+ with persistent back, hip, or knee pain. They found no significant correlation between opioid use and increased risk of falls or fractures. [35] By contrast, the results of this study indicate that among patients who used SMT or initiated care with SMT, rates of a same-level fall with associated hip fracture or head injury were less than half those for the OAT cohort. When these results are considered along with the risk of abuse, overdose, and death associated with use of OAT, SMT appears to offer a more efficient and safer treatment alternative for older patients with cLBP. This inference may need to be tempered, however, considering the higher rates of spinal injury observed among recipients of SMT.
Spinal injury was the single exception to the pattern of higher rates of escalated care for OAT as compared to SMT. The rationale for investigating rates of spinal injury was the possibility of iatrogenic injury due to SMT: because manipulation involves the delivery of physical force to the body, it is reasonable to hypothesize that SMT may carry a risk of injury. However, the results contrast sharply with those of an observational study of more than 6.6 million Medicare beneficiaries, which found that the adjusted risk of physical injury following a chiropractic office was much lower at 7 days than that following a visit to a primary care physician (hazard ratio, 0.24; 95% confidence interval, 0.230.25). [36] The higher rates reported here likely reflect the large difference in the period of outcomes measurement (up to 48 months for the current study vs. 7 days for the previous study). Future research should explicitly estimate the causal difference in risk of acute injury due to SMT as compared to other treatment approaches.
Our findings are generally consistent with previous findings regarding overall care for LBP, and offer new insights into differences in outcomes for OAT vs. SMT:
We found higher rates of hospitalization for OAT as compared to SMT. Most patients with back pain do not require hospitalization. Martin et al. found that from 1997 to 2006, the proportion of US adults with spine problems who had any hospitalization decreased from 3.5 to 2.6%. [37] and in 2012 Waterman et al. estimated that only 1.2% of US LBP patients required hospital admission. [38]
Manchikanti et al. found that between 2009 and 2018, utilization of interventional techniques for Medicare patients with chronic pain declined by 6.7%. [39] In the context of this overall decline, we found that the proportion of patients who received injections and other interventional procedures for LBP was nearly five times greater for the OAT cohort as compared to SMT.
Not inconsistent with the findings of Kim et al., who reported that only 1.2% of adults with a new diagnosis of LBP or lower extremity pain between 2008 and 2015 received surgery, [40] we found that that rates of spinal surgery were too low to report under CMS data suppression rules.
We found that recipients of OAT were more likely to receive advanced spinal imaging than recipients of SMT. Imaging for LBP is often unnecessary and is associated with increased costs and other potentially unnecessary procedures. [4143] In a recent analysis of Medicare data, Davis et al. found that increased beneficiary access to chiropractic care was correlated with a significant decrease in spending on spinal imaging and testing. [44]
We found a significantly higher risk of specialist visits for patients receiving OAT as compared to SMT. Chenot et al. found that consulting a specialist for LBP was associated with increased use of imaging and therapeutic interventions. [45]
We found that recipients of OAT were much more likely to seek emergency department care than recipients of SMT. Patients presenting with LBP can impose a significant burden on emergency department resources: Edwards et al. estimated the prevalence of LBP in emergency settings to be 4.39%. [46]
Implications for Practice and Policy
Chiropractors provide 94% of all SMT services in the US. [47] The reduced escalation of care associated with SMT should equate with lower costs, but a series of reports by the Office of Inspector General (OIG), found chiropractic care provided under Medicare to be excessively costly. However, the OIG did not compare costs for chiropractic with other approaches to spine care, and did not correlate costs with outcomes. [1921]
By contrast, Weeks et al. found that under Medicare, chiropractic costs for care of patients with cLBP were significantly lower than those for conventional medical care. [33] More recently, Davis and colleagues concluded that increased access to chiropractic services correlated with reduced costs of spine care for older Medicare beneficiaries. [44]
Nevertheless, coverage for spinal manipulation as provided by chiropractors under Medicare remains tightly restricted; Medicare does not cover physical examinations performed by chiropractors, or any service other than spinal manipulation. [13]
Increased patient access to chiropractic services may enhance the capacity of the Medicare workforce to care for the growing population of older adults with spinal pain. Medicare policy makers should consider expansion of Medicare coverage for chiropractic services. [48]
Limitations
The general limitations of using health claims data for research include inconsistencies in billing practices and coding of procedures and diagnoses. For example, we identified SMT by CPT codes that are specific for spinal manipulation and commonly used by chiropractors, but some clinicians may code SMT with other procedure codes that denote manipulative and physical medicine procedures. Other limitations of this study include a lack of an indication of pain severity, and lack of diagnoses in pharmacy claims data, and the retrospective design, which required us to rely upon CMS for accurate recordkeeping and prevented us from controlling exposures and the assessment of outcomes.
With this study there is potential for confounding by indication; while the different rates of escalation of care may be associated with worse outcomes leading to the escalations, they may instead be related to underlying differences in the patients that lead to their choice of treatment cohort in the first place. However, we controlled for comorbid chronic conditions (knee or hip osteoarthritis) that might confound the results, and for fibromyalgia and depressive disorder, which can impact prognosis of patients with cLBP.
Because selection bias can influence the results of observational research, we employed robust approaches to propensity scoring intended to minimize the risk of selection bias in this study. Despite these measures, we were unable to consider all confounding variables, the inherent limitations of observational design inhibit causal inference, and explicit assessment of changes in patients underlying health status were not possible.
Claims data lack sufficient clinical granularity to completely adjust for clinical level differences in populations. Unmeasured confounders (factors that affect treatment selection but are not part of the dataset) may affect patient perceptions regarding treatments, the capacity to benefit from those treatments, and clinician decisions regarding whether such interventions are indicated. However, the analysis of large multi-year claims datasets allows cost-efficient conduct of long-term evaluations, and sensitive detection of events that are uncommon or may take extended time in treatment to develop.
Conclusion
Among older Medicare beneficiaries who initiated long-term care for chronic low back pain with opioid analgesic therapy, the adjusted rate of escalated care encounters was significantly higher as compared to those who initiated care with spinal manipulative therapy.
APPENDIX - DETAILED METHODS
Overview
To test our hypothesis, we conducted a retrospective study using nationally representative samples of fee-for-service (FFS) claims data spanning a five-year study period (20122016). We combined elements of cohort and crossover-cohort design to evaluate for comparative rates of selected healthcare outcomes. The study population included non-institutionalized Medicare beneficiaries aged 6584 years and residing in a US state or the District of Columbia. We excluded subjects over the age of 84 at baseline due to age-related reduction in the utilization of spinal manipulation; we also excluded subjects with a primary diagnosis of cancer or use of hospice care during the study period. All patients were continuously enrolled throughout the study period under Medicare Parts A (inpatient), B (outpatient), and D (pharmacy). Thus, all patients had prescription drug coverage throughout the period of outcomes measurement. We restricted the sample to subjects with an episode of cLBP beginning in 2013. Because cLBP lasts three months or longer,1 we defined an episode of cLBP as occurring with the recording of two paid claims with primary diagnosis of LBP at least 90 days but less than 180 days apart. Claims were restricted to outpatient office visits as defined by Place of Service code 11. LBP was identified by ICD-9 or ICD-10 diagnosis code.
This study was conducted in accordance with a data use agreement with the Centers for Medicare and Medicaid Services (CMS), which allowed access to Medicare administrative data for research purposes. In accordance with CMS rules for analysis of health claims, cells with n<11 were suppressed to prevent disclosure of protected health information. The research methods were reviewed and approved by the principal investigators institutional review board.
This study was conducted in the context of a multi-aim NIH-funded investigation of the comparative value of OAT vs. SMT for long-term care of older Medicare beneficiaries with cLBP. Thus, aspects of the methods used for sampling and cohort assembly are identical to those described in reports on other aims of this research project.2
Cohort Definitions
All included patients received long term management of cLBP with SMT or OAT. SMT was identified in clinical claims data by Current Procedural Terminology (CPT) code 98940, 98941, or 98942. OAT was identified as opioid analgesics or analgesic medications containing opioids, identified by drug code 3 and obtained by prescription through an outpatient pharmacy. For OAT, we defined long-term management as 6 or more standard 30-day supply prescription fills in a 12-month period.4,5 For SMT, we defined long-term management as ?12 office visits for spinal manipulation for LBP in any 12-month period, including at least one visit per month.1,6,7,8
We assembled the included patients into cohorts. The date of accrual (index date) for patients into each cohort was the date of the first office visit associated with an episode of cLBP. For subjects with more than one episode of cLBP, only the first episode was counted for purposes of cohort accrual. A look-back period, defined as the 12-month period ending with the index date, allowed exercise of population inclusion and exclusion criteria and capture of patient characteristics including comorbidity scores. We assembled primary cohorts and crossover cohorts, and for purposes of analysis, combined cohorts based upon the patients first choice of treatment. [Figure 1]
Measurement of Patient Characteristics
Subject age in years at index date was categorized as 6569, 7074, 7579, and 8084. Sex as a biological variable was collected as male or female. Race and ethnicity data are multiply categorized in CMS data, but adherence to data suppression rules required aggregating these data to only two categories: White and Other / Unknown. As measures of lower socioeconomic status, we captured eligibility for Medicare Part D low-income subsidy and dual eligibility for both Medicare and Medicaid. As measures of health status, we calculated Charlson comorbidity scores, and collected data on diagnosis of comorbid chronic conditions (osteoarthritis of the hip or knee, which may confound the indication for opioids, and fibromyalgia and depressive disorder, which may affect prognosis for older adults with cLBP). Diagnostic codes for LBP were categorized as non-specific LBP, radiculopathy, herniated disc, spondylolisthesis, sprain/strain, or spinal stenosis. For subjects who received OAT, we also collected data on class of opioid prescribed at time of cohort accrual.
Outcomes Measurement and Statistical Analysis
From index date through 2016, we analyzed the cumulative frequency of encounters indicative of an escalation of care for cLBP. We measured by Current Procedural Terminology (CPT) code for secondary care encounters for LBP, including hospitalizations, emergency department visits, advanced diagnostic imaging, specialist visits, lumbosacral surgery, and interventional pain medicine techniques (including epidural injections, adhesiolysis procedures, facet joint interventions, discography, disc decompression, sacroiliac joint blocks, and other nerve blocks). We also analyzed for encounters for potential complications of cLBP: same level fall (identified by E-code) resulting in hip fracture or head injury, and spinal injuries (lumbosacral sprain, dislocation, or fracture) which may rarely occur as a complication of SMT of the lower back.
We generated descriptive statistics on subject characteristics and on the frequency of outcomes by cohort and analyzed to estimate the causal difference between initial choice of the two approaches to treatment. Previous studies have found that initial choice of treatment for LBP can significantly affect outcomes.9,10 We accounted for selection bias by modeling of the outcome by covariates and by propensity scoring. To estimate the adjusted incidence rate ratio using a multivariable model (e.g., ratio of average count) we conducted a comparison of outcomes between cohorts OATC and SMTC using Poisson regression with robust (sandwich) standard errors, controlling for age, sex, race, beneficiary residence ZIP code, Part D low-income subsidy, dual eligibility status, LBP diagnostic category, Charlson comorbidity score, and comorbid chronic conditions (osteoarthritis of the hip or knee, fibromyalgia, and depressive disorder). We repeated this comparison using a propensity score approach. In the first step, we derived a model for the propensity of OAT vs SMT using a flexible logistic regression (e.g., non-parametric regression including interactions) in terms of the covariates above. Next, we compared outcomes between OAT and SMT using both inverse weighted propensities and binned propensities (i.e., controlling for the categorical variable created by taking deciles of the propensity). All statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, NC).
Propensity Models
An iterative statistical process was undertaken for the development and fitness testing of the propensity models. The following is a list of the variables examined for inclusion along with their descriptions:zipcode residence of subject in the analysis year
age five categories: 6569, 7074, 7579, 8084, exclusion category 85 years & above
sex m/f
race two categories: White and Other
Charlson Summary of 2013 Charlson comorbidity score in 5 categories: 0, 1, 2, 3 and 4+
lics Any Low-income Subsidy in 2013, inferred from Medicare Part D claims
dual_elig - Flag for beneficiary Dual Eligibility (Medicare/Medicaid) in 2013
chronic_cat - Chronic Condition 1: Osteoarthritis of the Hip
Chronic Condition 2: Osteoarthritis of the Knee
Chronic Condition 3: Fibromyalgia
Chronic Condition 4: Depressive Disorder
severity LBP diagnostic categories 1, 3, 4, 6, 11, 12 (non-specific low back pain, radiculopathy, herniated disc, spondylolisthesis, sprain/strain, & spinal stenosis, respectively)The process included step-by-step identification of correct covariates to include in the models removing the ones (e.g., zipcode, LBP severity categories) that led to misspecification or nonconvergence of the model and adding in the ones that were integral to the study (such as sex of the patient and geographic unit Census data).
The primary (or most important) covariates were identified using the following SAS command and criteria: variable importance >1 by GLMSELECT method, corroborated by lasso and random forest methods. This process led to the inclusion of the following variables: age (5 categories); race (2 categories); Charlson comorbidity score (5 categories); low income subsidy in 2013; chronic condition (Osteoarthritis of the Knee and Depressive Disorder); and diagnostic severity of lbp (severity category 1). This process also identified key interaction terms to include in the model as well as identified variables to remove from the model (low back pain, severity category 11).
As a result of this iterative process of covariate selection, the final model included the following variables covariates: census division (geographic units); age; sex; race; Charlson score; low income subsidy; Osteoarthrities of the knee & Depressive Disorder; and LBP diagnostic severity category. The final model also included the following interaction terms: Depressive Disorder*Charlson score; low income subsidy*age; low income subsidy*Osteoarthritus; low income subsidy*Depressive Disorder; lbp severity category1*Charlson score; lbp severity category1*Depressive Disorder; and lbp severity category1*race.
APPENDIX References:
R.A. Deyo, S.F. Dworkin, D. Amtmann, G. Andersson, et al.,
Report of the NIH Task Force on Research Standards
for Chronic Low Back Pain
Journal of Pain 2014 (Jun); 15 (6): 5695851R15AT010035-01
Spinal Manipulation Services vs. Prescription Drug Therapy for Long-Term Care of Aged Medicare Beneficiaries with Chronic Low Back Pain
U.S. Department of Health and Human Services, 2018. (Accessed October 20, 2020, at
https://projectreporter.nih.gov/project_info_description.cfm?aid=9589519&icde=52242383&ddparam=&ddvalue=&ddsub=&cr=6&csb=default&cs=ASC&pball=National Drug Codes List -
The complete repository of National Drug Codes Information.
NDC List, 2020. (Accessed June 20, 2020, at
https://ndclist.com/Chou R, Turner JA, Devine EB, et al.
The Effectiveness and Risks of Long-Term Opioid Treatment of Chronic Pain
Evidence Report/Technology Assessment Number 218
Agency for Healthcare Research and Quality
Rockville, MD 20850
AHRQ Publication No. 14-E005-EF September 2014Morden NE, Munson JC, Colla CH, et al.
Prescription opioid use among disabled Medicare beneficiaries:
intensity, trends, and regional variation.
Med Care 2014;52:8529Office Of Inspector General
Hundreds of Millions in Medicare Payments for Chiropractic Services
Did Not Comply with Medicare Requirements
Washington, DC: Office of Inspector General,
Department of Health and Human Services; 2016.Weigel PA, Hockenberry JM, Wolinsky FD.
Chiropractic Use in the Medicare Population: Prevalence, Patterns,
and Associations With 1-year Changes in Health
and Satisfaction With Care
J Manipulative Physiol Ther 2014 (Mar); 37 (8): 542-551Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, et al.
Noninvasive Treatments for Low Back Pain
Comparative Effectiveness Review no. 169
Agency for Healthcare Research and Quality; (February 2016)Keeney BJ, Fulton-Kehoe D, Turner JA, et al.
Early Predictors of Lumbar Spine Surgery After Occupational Back Injury:
Results From a Prospective Study of Workers in Washington State
Spine (Phila Pa 1976). 2013 (May 15); 38 (11): 953964Liliedahl RL, Finch MD, Axene DV, Goertz CM.
Cost of Care for Common Back Pain Conditions Initiated With Chiropractic
Doctor vs Medical Doctor/Doctor of Osteopathy as First Physician:
Experience of One Tennessee-Based General Health Insurer
J Manipulative Physiol Ther 2010 (Nov); 33 (9): 640643
Acknowledgements
This study was conducted in accordance with data use agreement # DUA: RSCH-2019-52662 with the Centers for Medicare and Medicaid Services. The authors gratefully acknowledge the valuable contributions of student researchers Maria Bangash and Kayla Sagester.
The manuscript submitted does not contain information about medical device(s)/drug(s).
This research was supported by the National Center for Complementary and Integrative Health (NCCIH) of the National Institutes of Health (award number 1R15AT010035).
Relevant financial activities outside the submitted work: board membership, consultancy, grants, royalties, travel/accommodations/meeting expenses.
References:
Wong AY, Karppinen J, Samartzis D.
Low back pain in older adults: risk factors, management options
and future directions.
Scoliosis Spinal Disord 2017;12:14de Souza IMB, Sakaguchi TF, Yuan SLK, et al.
Prevalence of Low Back Pain in the Elderly Population:
A Systematic Review
Clinics (Sao Paulo) 2019 (Oct 28); 74: e789Ghildayal N, Johnson PJ, Evans RL, Kreitzer MJ.
Complementary and alternative medicine use in
the US adult low back pain population.
Glob Adv Health Med 2016;5:6978Weigel, P.A., Hockenberry, J., Bentler, S.E., Wolinsky, F.D., 2014.
The Comparative Effect of Episodes of Chiropractic and
Medical Treatment on the Health of Older Adults
J Manipulative Physiol Ther 2014 (Mar); 37 (3): 143154Dieleman JL, Cao J, Chapin A, et al.
US Health Care Spending by Payer and Health Condition, 1996-2016
JAMA 2020 (Mar 3); 323 (9): 863884Weiner DK, Kim YS, Bonino P, Wang T.
Low back pain in older adults: are we utilizing healthcare resources wisely?
Pain Med. 2006;7:14350Deyo RA, Mirza SK, Turner JA, Martin BI.
Overtreating Chronic Back Pain: Time to Back Off?
J Am Board Fam Med. 2009 (Jan); 22 (1): 6268Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, et al.
Nonpharmacologic Therapies for Low Back Pain: A Systematic Review
for an American College of Physicians Clinical Practice Guideline
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 493505Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, et al.
Prevention and Treatment of Low Back Pain:
Evidence, Challenges, and Promising Directions
Lancet. 2018 (Jun 9); 391 (10137): 23682383
This is the third of 4 articles in the remarkable Lancet Series on Low Back PainInstitute of Medicine Committee on Quality of Health Care in America.
Crossing the Quality Chasm: A New Health System for the 21st Century
Washington, DC: National Academies Press; 2001Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514530Jones MR, Ehrhardt KP, Ripoll JG, et al.
Pain in the Elderly.
Current pain and headache reports 2016;20:23Whedon JM, Goertz CM, Lurie JD, Stason WB.
Beyond Spinal Manipulation: Should Medicare Expand Coverage
for Chiropractic Services? A Review and Commentary
on the Challenges for Policy Makers
J Chiropractic Humanities 2013 (Aug 28); 20 (1): 918Hagemeier NE.
Introduction to the opioid epidemic: the economic burden
on the healthcare system and impact on quality of life.
Am J Manag Care 2018;24:S200S6Wilson N, Kariisa M, Seth P, Smith Ht, Davis NL.
Drug and Opioid-Involved Overdose Deaths - United States, 20172018.
MMWR Morb Mortal Wkly Rep 2020;69:2907Deyo RA, Von Korff M, Duhrkoop D.
Opioids for low back pain.
BMJ 2015; 350:g6380.: 10.1136/bmj.g6380Coulter ID, Crawford C, Hurwitz EL, et al.
Manipulation and Mobilization for Treating Chronic Low Back Pain:
A Systematic Review and Meta-analysis
Spine J. 2018 (May); 18 (5): 866879Rubinstein SM, De Zoete A, Van Middelkoop M, Assendelft WJJ, De Boer MR, Van Tulder MW.
Benefits and Harms of Spinal Manipulative Therapy for the Treatment of
Chronic Low Back Pain: Systematic Review and Meta-analysis
of Randomised Controlled Trials
British Medical Journal 2019 (Mar 13); 364: 1689Office Of Inspector General
Chiropractic Services in the Medicare Program: Patient Vulnerability Analysis
Washington, D.C: Office of Inspector General,
Department of Health and Human ServicesOffice Of Inspector General
Inappropriate Medicare Payments for Chiropractic Services
Washington, DC: Office of Inspector General,
Department of Health and Human Services; 2009.Office Of Inspector General
Hundreds of Millions in Medicare Payments for Chiropractic Services
Did Not Comply with Medicare Requirements
Washington, DC: Office of Inspector General,
Department of Health and Human Services; 2016.Chou R, Turner JA, Devine EB, et al.
The Effectiveness and Risks of Long-Term Opioid Treatment of Chronic Pain
Evidence Report/Technology Assessment Number 218
Agency for Healthcare Research and Quality
Rockville, MD 20850
AHRQ Publication No. 14-E005-EF September 2014Morden NE, Munson JC, Colla CH, et al.
Prescription opioid use among disabled Medicare beneficiaries:
intensity, trends, and regional variation.
Med Care 2014;52:8529R.A. Deyo, S.F. Dworkin, D. Amtmann, G. Andersson, et al.,
Report of the NIH Task Force on Research Standards
for Chronic Low Back Pain
Journal of Pain 2014 (Jun); 15 (6): 569585Weigel PA, Hockenberry JM, Wolinsky FD.
Chiropractic Use in the Medicare Population: Prevalence, Patterns,
and Associations With 1-year Changes in Health
and Satisfaction With Care
J Manipulative Physiol Ther 2014 (Mar); 37 (8): 542-551Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, et al.
Noninvasive Treatments for Low Back Pain
Comparative Effectiveness Review no. 169
Agency for Healthcare Research and Quality; (February 2016)Weeks WB, Tosteson TD, Whedon JM, et al.
Comparing Propensity Score Methods for Creating Comparable Cohorts
of Chiropractic Users and Nonusers in Older, Multiply Comorbid
Medicare Patients With Chronic Low Back Pain.
J Manipulative Physiol Ther 2015;38:6208Keeney BJ, Fulton-Kehoe D, Turner JA, et al.
Early Predictors of Lumbar Spine Surgery After Occupational Back Injury:
Results From a Prospective Study of Workers in Washington State
Spine (Phila Pa 1976). 2013 (May 15); 38 (11): 953964Corcoran KL, Bastian LA, Gunderson CG, et al.
Association Between Chiropractic Use and Opioid Receipt Among
Patients with Spinal Pain: A Systematic Review and Meta-analysis
Pain Medicine 2020 (Feb 1); 21 (2): e139e145Kazis LE, Ameli O, Rothendler J, et al.
Observational Retrospective Study of the Association of Initial
Healthcare Provider for New-onset Low Back Pain with
Early and Long-term Opioid Use
BMJ Open. 2019 (Sep 20); 9 (9): e028633Whedon JM, Toler AWJ, Kazal LA, Bezdjian S, Goehl JM, Greenstein J.
Impact of Chiropractic Care on Use of
Prescription Opioids in Patients with Spinal Pain
Pain Medicine 2020 (Dec 25); 21 (12): 35673573
There are more like this at: SPINAL PAIN MANAGEMENTLiliedahl RL, Finch MD, Axene DV, Goertz CM.
Cost of Care for Common Back Pain Conditions Initiated With Chiropractic
Doctor vs Medical Doctor/Doctor of Osteopathy as First Physician:
Experience of One Tennessee-Based General Health Insurer
J Manipulative Physiol Ther 2010 (Nov); 33 (9): 640643Weeks, WB, Leininger, B, Whedon, JM et al.
The Association Between Use of Chiropractic Care and Costs of Care Among Older
Medicare Patients With Chronic Low Back Pain and Multiple Comorbidities
J Manipulative Physiol Ther. 2016 (Feb); 39 (2): 6375Weeks WB, Pike J, Donath J, Fiacco P, Justice BD.
Conservative Spine Care Pathway Implementation is Associated with Reduced
Health Care Expenditures in a Controlled, Before-After Observational Study
J General Internal Medicine 2019 (Aug); 34 (8): 13811382Krebs EE, Paudel M, Taylor BC, et al.
Association of Opioids with Falls, Fractures, and Physical Performance
among Older Men with Persistent Musculoskeletal Pain.
Journal of general internal medicine 2016;31:4639Whedon, JM, Mackenzie, TA, Phillips, RB, and Lurie, JD.
Risk of Traumatic Injury Associated with Chiropractic Spinal Manipulation
in Medicare Part B Beneficiaries Aged 66-99
Spine (Phila Pa 1976) 2015 (Feb 15); 40 (4): 264270 doi: 10.1016/S0140-6736(16)30970-9.Martin BI, Turner JA, Mirza SK, et al.
Trends in Health Care Expenditures, Utilization, and Health Status
Among US Adults With Spine Problems, 1997-2006
Spine (Phila Pa 1976). 2009 (Sep 1); 34 (19): 20772084Waterman BR, Belmont PJ, Jr., Schoenfeld AJ.
Low back pain in the United States: incidence and risk factors
for presentation in the emergency setting.
Spine J 2012;12:6370Manchikanti L, Sanapati MR, Pampati V, Boswell MV, Kaye AD, Hirsch JA.
Update on Reversal and Decline of Growth of Utilization of
Interventional Techniques In Managing Chronic Pain in
the Medicare Population from 2000 to 2018.
Pain Physician 2019;22:52136Kim LH, Vail D, Azad TD, Bentley JP, Zhang Y, Ho AL, Faterni P, Feng A.
Expenditures and Health Care Utilization Among Adults
with Newly Diagnosed Low Back and Lower Extremity Pain
JAMA Network Open 2019 (May 3); 2 (5): e193676Lemmers GPG, van Lankveld W, Westert GP, van der Wees PJ, Staal JB.
Imaging versus no imaging for low back pain: a systematic review,
measuring costs, healthcare utilization and absence from work.
Eur Spine J 2019;28:93750Powell AC, Rogstad TL, Elliott SW, et al.
Health Care Utilization and Pain Outcomes Following
Early Imaging for Low Back Pain in Older Adults.
J Am Board Fam Med 2019;32:77380Webster BS, Choi Y, Bauer AZ, Cifuentes M, Pransky G.
The cascade of medical services and associated longitudinal costs
due to nonadherent magnetic resonance imaging for low back pain.
Spine (Phila Pa) 2014;39:143340Davis AY, O, Liu H, Tootoo J, Titler MG, Bynum JPW.
Access to Chiropractic Care and the Cost
of Spine Conditions Among Older Adults
American J Managed Care 2019 (Aug); 25 (8): e230e236Chenot JF, Leonhardt C, Keller S, et al.
The impact of specialist care for low back pain on health service
utilization in primary care patients: a prospective cohort study.
Eur J Pain 2008;12:27583Edwards J, Hayden J, Asbridge M, Gregoire B, Magee K.
Prevalence of low back pain in emergency settings:
a systematic review and meta-analysis.
BMC Musculoskelet Disord 2017;18:143Shekelle PG, Adams AH, Chassin MR, Hurwitz EL, Brook RH.
Spinal manipulation for low-back pain.
Ann Intern Med 1992;117:5908Medicare: Patient Access to Chiropractic.
American Chiropractic Association, 2020. (Accessed October 15, 2020, at
https://www.acatoday.org/Advocacy/Legislative-Regulatory-Policy/Medicare/HR3654-Resources
Return to MEDICARE
Return to LOW BACK PAIN
Return to OPIOID EPIDEMIC
Return NON-PHARMACOLOGIC THERAPY
Return to INITIAL PROVIDER/FIRST CONTACT
Since 9-09-2021


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |