

Association Between Chiropractic Spinal Manipulation
and Lumbar Discectomy in Adults with Lumbar Disc
Herniation and Radiculopathy: Retrospective
Cohort Study Using United States' DataThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: BMJ Open 2022 (Dec 16); 12 (12): e068262 ~ FULL TEXT
OPEN ACCESS Robert James Trager, Clinton J Daniels, Jaime A Perez, Regina M Casselberry, Jeffery A Dusek
Connor Whole Health,
University Hospitals Cleveland Medical Center,
Cleveland, Ohio, USA
Objectives: Chiropractic spinal manipulative therapy (CSMT) and lumbar discectomy are both used for lumbar disc herniation (LDH) and lumbosacral radiculopathy (LSR); however, limited research has examined the relationship between these therapies. We hypothesised that adults receiving CSMT for newly diagnosed LDH or LSR would have reduced odds of lumbar discectomy over 1-year and 2-year follow-up compared with those receiving other care.
Design: Retrospective cohort study.
Setting: 101 million patient US health records network (TriNetX), queried on 24 October 2022, yielding data from 2012 query.
Participants: Adults age 18-49 with newly diagnosed LDH/LSR (first date of diagnosis) were included. Exclusions were prior lumbar surgery, absolute indications for surgery, trauma, spondylolisthesis and scoliosis. Propensity score matching controlled for variables associated with the likelihood of discectomy (eg, demographics, medications).
Interventions: Patients were divided into cohorts according to receipt of CSMT.
Primary and secondary outcome measures: ORs for lumbar discectomy; calculated by dividing odds in the CSMT cohort by odds in the cohort receiving other care.
Results: After matching, there were 5,785 patients per cohort (mean age 36.9±8.2). The ORs (95% CI) for discectomy were significantly reduced in the CSMT cohort compared with the cohort receiving other care over 1-year (0.69 (0.52 to 0.90), p=0.006) and 2-year follow-up (0.77 (0.60 to 0.99), p=0.040). E-value sensitivity analysis estimated the strength in terms of risk ratio an unmeasured confounding variable would need to account for study results, yielding point estimates for each follow-up (1 year: 2.26; 2 years: 1.92), which no variables in the literature reached.
Conclusions: Our findings suggest receiving CSMT compared with other care for newly diagnosed LDH/LSR is associated with significantly reduced odds of discectomy over 2-year follow-up. Given socioeconomic variables were unavailable and an observational design precludes inferring causality, the efficacy of CSMT for LDH/LSR should be examined via randomised controlled trial to eliminate residual confounding.
Keywords: complementary medicine, rehabilitation medicine, surgery
Strengths and limitations of this study
This study was based on an a priori protocol developed by a multidisciplinary research team with the intention of reducing bias.
This study included patients with newly diagnosed lumbar disc herniation or lumbosacral radiculopathy and excluded those with absolute indications for surgery to make cohorts more comparable.
While an extensive propensity matching model was used to control for confounding variables, several variables were unavailable in the dataset including those relating to socioeconomic status, examination and imaging findings, pain severity and impact, catastrophising, self-efficacy and disability.
While this study examined a large population, only large, academically affiliated healthcare organisations in the US were included, thus results may not be broadly generalisable.
As this study is observational, a randomised controlled trial would be needed to eliminate possible residual confounding.
From the FULL TEXT Article:
Introduction
A lumbar disc herniation (LDH) is a focal displacement of intervertebral disc material beyond the normal limit of the disc margin, [1] which may compress one or more nerve roots, causing lumbosacral radiculopathy (LSR). The clinical features of LSR include radicular (radiating) lower extremity pain, predictable sensory disturbances, weakness and/or diminished muscle stretch reflexes. [2] LDH and LSR are common reasons for patients to receive chiropractic care or undergo surgery to remove LDH material, a procedure called discectomy. However, limited research has examined the association between chiropractic care and discectomy.
In the USA, chiropractors are portal-of-entry providers that often manage low back pain, including LDH/LSR. [3, 4] While chiropractors may use soft tissue or exercise therapies for these patients, [5] they most often employ chiropractic spinal manipulative therapy (CSMT). [4]
Prior studies have documented the benefits of CSMT for LDH/LSR, including randomised prospective studies. [6, 7] In a meta-analysis, spinal manipulation was found to be one of the most effective treatments for discogenic LSR. [8] Accordingly, US and international clinical practice guidelines have recommended spinal manipulation for low back pain and LSR. [9–13]
Prior studies examining the association between chiropractic care and lumbar spine surgery have examined a broader population and/or outcome. [14–20] Two studies identified a significant reduction in odds of lumbar surgery among individuals receiving early chiropractic care, with one examining surgical fusion or decompression among patients with an occupational back injury, [18] and another examining discectomy and fusion among patients with back pain. [14] The current study differs by examining a narrower range of LBP conditions (ie, LDH/LSR) with an outcome specific to discectomy.
Several factors may influence whether a patient undergoes a discectomy, including clinical features, patient preferences and the response to conservative care. [21–23] While the presence of severe or ‘red flag’ neurologic deficits and/or cauda equina syndrome (CES) are absolute indications for lumbar discectomy, continued pain despite conservative treatment that affects quality of life is considered a relative indication. [24] For patients without absolute indications, early discectomy can provide short-term benefits for LDH with LSR; however, long-term outcomes are similar at 1–2 years in those receiving conservative care. [25]
This study was conducted considering that CSMT and lumbar discectomy are both viable treatment options for LDH and LSR, yet there has been limited research examining the relationship between these care pathways.
Objectives
This study aimed to examine the association between receipt of CSMT for newly diagnosed LDH and/or LSR and odds of lumbar discectomy, with the hypothesis that adults receiving CSMT would have reduced odds of lumbar discectomy over 1–year and 2–year follow-up windows after index diagnosis compared with those receiving other care.
Methods
Study design
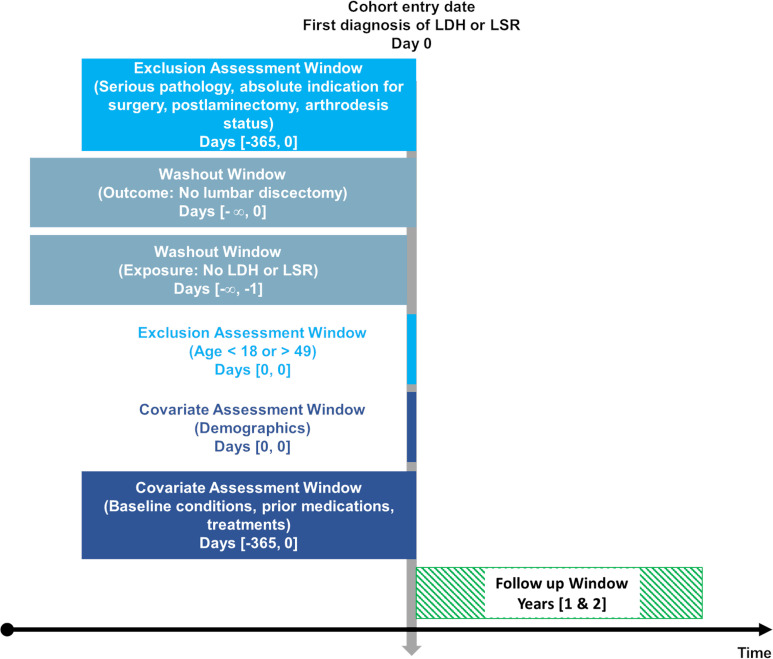
Figure 1 This study followed an a priori protocol registered with the Open Science Framework (https://osf.io/2gkcd), [26] and incorporated a retrospective, new user, active comparator design [27] to compare recipients and non-recipients of CSMT from age 18–49 of any sex (Figure 1). The study included patients meeting selection criteria from 24 October 2012 to 24 October 2020 to capture more recent data, considering the treatment of LDH and LSR may have changed over time. Strengthening the Reporting of Observational Studies in Epidemiology guideline structure was followed. [28]
This study used a 101 million patient’s population within the TriNetX US research network (TriNetX, Cambridge, Massachusetts, USA). [29] Data in this network is deidentified, aggregated and frequently updated from the health records of multiple healthcare organisations in the USA, which are typically large, academically affiliated health centres and their ambulatory offices. This network includes insured and uninsured patients. [30] The TriNetX dataset routinely undergoes automated and manual assessments to ensure data conformance, completeness and plausibility. [29, 31] One previous study estimated a completeness of at least 87% for medications in the TriNetX dataset [32]; however, the completeness of other variables has not been examined to our knowledge.
Queries of this dataset are performed using standardised nomenclatures such as the International Classification of Diseases (ICD-10) procedural classification system (ICD-10-PCS), current procedural terminology (CPT) and Veterans Health Administration National Drug File and others. ICD-10 codes may also be used, which are interconverted automatically to older ICD-9 codes using general equivalence mappings. [29] At University Hospitals of Cleveland, the Clinical Research Center manages all use of the TriNetX platform.
As of January 2022, there were 10 healthcare organisations within the TriNetX network that had providers administering CSMT. [33] In accordance with of privacy regulations, these institutions remain anonymous. Although this study only examined a fraction of US chiropractic providers, integration of chiropractors into hospitals is a growing trend, with 5% of US chiropractors reporting a hospital affiliation in 2019. [3] Integrated chiropractors are most often employed within physical medicine, rehabilitation or physical therapy settings and on average have 21–year experience in practice. [34]
Participants
Eligibility criteria This study identified patients with newly diagnosed LDH and/or LSR by querying the TriNetX dataset with a custom set of codes (online supplemental table 1). These patients were identified at the index date of diagnosis, which we defined as the first instance of LDH or LSR codes appearing in the medical record. This effectively required that patients had no previous instance of LDH or LSR diagnosis occurring over any time available in the dataset preceding the index date. As the length of time patients were available in the dataset prior to inclusion varied, this washout window also varied per patient. Patients were required to be represented in the dataset for at least 2 years after the index diagnosis date to be eligible.
Patients with diagnoses of lumbar or sacral radiculopathy or sciatica were included as these diagnoses often reflect underlying LDH or LSR, [35] and evidence suggested that these diagnosis codes are often used by clinicians. [36] The age bracket of 18–49 years was used as LDH is more common in younger patients aged 30–50. [37] Conversely, lumbar stenosis is a more prevalent cause of LSR in older patients. [38] Accordingly, the upper age cut-off was intended to exclude patients with lumbar stenosis from our study.
Patients with serious spine pathology or absolute indication for surgery, such as CES, signs of CES such as bowel or bladder incontinence, fracture, infection and malignant neoplasms were excluded over 365 days preceding and including the date of index diagnosis (online supplemental table 2). [39] Patients with conditions that could alter the CSMT or surgical approach and/or increase the odds of lumbar surgery were also excluded: lumbar fusion, arthrodesis or post-laminectomy syndrome, [40, 41] lumbar spine trauma [42] and degenerative lumbar scoliosis and spondylolisthesis. [43] As an additional measure of ensuring patients had no previous discectomy, we excluded patients with any instance of discectomy occurring over any time available in the dataset preceding and including the index date of diagnosis.
Diagnoses of lumbar spondylosis (eg, ICD-10: M47.26) were not used in our inclusion criteria, given these are not specific to LDH. In addition, codes specifying lumbar disc disorders with myelopathy (eg, ICD-10: M47.16) were not used as myelopathy has different clinical features and management strategies than LDH/LSR. Diagnosis codes specifying lumbar or lumbosacral disc degeneration were not included, as a strategy to create more uniformity between cohorts. Disc degeneration is not associated with radicular symptoms, unlike LDH, which has a strong association with radicular symptoms. [44]
Included patients were divided into two cohorts according to receipt of CSMT (online supplemental table 3). The CPT codes 98940, 98941 and 98 942 for CSMT were included in the ‘CSMT’ cohort and excluded in the ‘other care’ cohort. These 9894* codes are almost exclusively used by chiropractors in the USA. [45] Patients in the CSMT cohort were required to receive CSMT on the date of index date of diagnosis of LDH or LSR (ie, the first instance of the diagnosis in the medical record), while those in the cohort receiving other care could not receive CSMT on the index date of diagnosis.
Variables
Discectomy A definition for the outcome of lumbar discectomy was developed based on discussion among coauthors and comparison with previous publications (online supplemental table 4). [36, 39, 46, 47] This definition included multiple procedure codes for discectomy, as well as the ICD-10-PCS code 0SB4* which includes open, percutaneous and percutaneous endoscopic approaches to excise lumbosacral disc material, [48] and the Healthcare Common Procedure Coding System code C9757 for lumbar discectomy with implantation of an annular closure device. [47] Feasibility testing was conducted in June, 2021, to ensure these codes were represented in the TriNetX database. Two follow-up windows of 1 year and 2 years were used in this study to allow for comparisons to prior similar studies also using long-term endpoints. [16, 18]
Potential confounders Propensity score matching is a method of balancing confounding variables between cohorts to improve their comparability. [27] Based on previous recommendations, confounders were propensity matched when having evidence of an association with the outcome of interest (ie, lumbar discectomy). [49] Variables present within a 365–day window preceding the index diagnosis of LDH and/or LSR were eligible for propensity matching (online supplemental table 5).
Demographic variables associated with the likelihood of lumbar surgery were propensity matched including increasing age, [23, 50] male sex [23, 50, 51] and race. [50] Other factors associated with increased likelihood of lumbar surgery were matched including obesity, [23, 50] being a non-smoker, [23] psychological disorders, [50] a history of lumbar injections [23, 52] and prior treatment with opioids [42] or prescription pain medications. [23] Radicular symptoms or radiculopathy are also predictors of lumbar surgery in those with low back pain [23, 52] and were matched via the ICD-10 codes for LSR and sciatica.
Study size
A required sample size of 198 was calculated using G*Power [53] z-tests for logistic regression, with an alpha error 0.05, power of 0.95, probability of the outcome in the null hypothesis of 0.02 and OR of 0.18, assuming a normal distribution and a moderate interaction between covariates (R2=0.5). Probabilities were taken from a prior similar study that examined surgical rates in recipients vs non-recipients of chiropractic care. [16] This sample was deemed to be feasible given the large patient population within the TriNetX network.
Statistical methods
Statistical analysis was performed using built-in statistical functions available in the TriNetX software platform in real-time. Baseline characteristics were compared using a Pearson χ2 test for categorical variables and independent-samples t-test for continuous variables. We did not perform any imputations for missing data.
Propensity scores for each cohort were calculated using logistic regression. Propensity scores were matched 1:1 using a greedy nearest-neighbour algorithm and a calliper of 0.01 pooled SD. A visual diagnostic was used to assess the balance between cohorts following propensity score matching. Odds of discectomy in each cohort were calculated by dividing the number of patients undergoing discectomy by the number of patients not undergoing discectomy. ORs for discectomy for each follow-up window were calculated by dividing odds in the CSMT cohort by odds in the other care cohort.
A sensitivity analysis was conducted by computing E-values for both follow-up windows after propensity matching. [54] The E-value is defined as the minimum strength of association an unmeasured confounder would need to account for an association between the outcome (ie, CSMT) and exposure (lumbar discectomy). [55]
Patient and public involvement
No patient or public involvement.
Results
Participants

Table 1 Patients meeting selection criteria were identified from 70 healthcare organisations, 10 of which included CSMT services. A large sample size was identified for each cohort (Table 1). Before propensity matching, there were 5,785 patients in the CSMT cohort and 482,704 in the other care cohort. After propensity matching, which discarded non-matching patients in the larger other care cohort, there were 5,785 patients in each cohort (mean age 36.9±8.2 years).
Before matching, there were several differences between cohorts. Most notably, the CSMT cohort had a significantly lower percentage of patients who were Black/African American or Hispanic/Latino and significantly higher percentage of patients who were prescribed central nervous system medications. The frequency of LDH/LSR codes also varied between cohorts. All differences between cohorts were no longer statistically significant after propensity matching, aside from body mass index. However, this difference was minimal, varying only 0.5 kg/m˛ between cohorts.
Descriptive data
The average number of data points per patient was high in both cohorts (CSMT 2442, other care 1527). After propensity matching, the frequency of unknown demographic variables was the same both cohorts, with 15% having unknown race, 14% having unknown ethnicity and 0% having unknown sex or age. These findings suggested there was no difference between cohorts with respect to missing data. A visual propensity score density graph revealed that cohorts were comparable after propensity matching (see online supplemental figure 1).
Key results

Table 2 Discectomy was less frequent in the CSMT cohort throughout 1–year and 2–year follow-up windows before and after propensity matching. After matching, 1.5% of patients (CSMT) and 2.2% (other care) underwent discectomy over 1–year follow-up, while 1.9% (CSMT) and 2.4% (other care) underwent discectomy over 2 years (Table 2). After matching, odds of discectomy were significantly lower in the CSMT compared with other care cohort, with an OR (95% CI) of 0.69 (0.52 to 0.90; p=0.006) over 1–year and 0.77 (0.60 to 0.99; p=0.040) over 2–year follow-up from index diagnosis.
Sensitivity analysis
After propensity matching, ORs for the current study allowed calculation54 of an E-value for the point estimate of 2.26 with an E-value for the lower CI of 1.46 for the 1–year follow-up, and an E-value for the point estimate of 1.92 with an E-value for the lower CI of 1.11 for the 2–year follow-up.
While our protocol suggested patients have a small increase in likelihood of visiting a chiropractor if they have higher income (ie, risk ratio of 1.23), [56] this was based on data from the 1990s, [57, 28] which has been contradicted by more recent data. A more recent study found that income, education level and insurance coverage are not associated with patients’ initial choice of provider for spinal pain (ie, chiropractor, physical therapist or medical physician). [59] Regardless, the risk ratio from the earlier study suggesting income was a predictor is less than the E-value point estimates for our study (ie, 1.23, <1.92 and 2.26).
An unmeasured variable associated with both likelihood of visiting a chiropractor and likelihood of undergoing discectomy would require a risk ratio greater than the study E-value point estimates, 1.92 and 2.26, to fully explain away our results of a significant reduction in odds of discectomy from the 2–year and 1–year follow-up outcomes, respectively. [55] We are unaware of any socioeconomic or other variable that were not measured in the current study that could fully explain away our results based on the E-value estimates.
Discussion
This retrospective cohort study was the first to examine the association between receiving CSMT for newly diagnosed LDH and/or LSR and odds of lumbar discectomy and included a large US sample of over 3,000 patients per cohort after several exclusions and propensity matching to improve cohort comparability. These real-world results support our hypothesis that patients initially receiving CSMT for LDH/LSR have reduced odds of discectomy over 1–year and 2–year follow-up.
The frequency of discectomy in this study (ie, 1.5%–2.2% over 1 year) is comparable to previous studies, and suggestive that our methods of capturing this outcome were valid. One prior study which examined 2.5 million adults in the USA with low back and/or lower extremity pain and no red flag diagnosis found that 1.2% of patients underwent surgery over a 1–year follow-up period. [60] While smaller studies have reported a higher frequency of discectomy of 5% or greater, [44, 61–63] our study had a relatively young population and several exclusions, which could explain the frequency of discectomy being on the lower end of the range of prior studies. Further, most discectomies occurred in the first year of follow-up in our study, with only a small increase during the 2–year follow-up window. This is in agreement with a previous systematic review that reported the majority of patients undergo surgery within 2 and 12 months from onset of symptoms. [24]
The overall rate of surgery over 2–year follow-up including both cohorts combined in our study was 2.1%, whereas in previous similar studies examining CSMT this value was 5%14 and 9%. [18] The lower frequency of discectomy in our study could relate to a declining rate of lumbar surgery in the USA. [64] While our study included the most recent data, from 2012 to 2022, the 5% value derived from data from 2012 to 2018, [14] and 9% value derived from older data from 2002 to 2004. [18] Finally, it is possible that the final 2 years of our data included a lower frequency of discectomy related to the COVID-19 pandemic, as studies have reported delays and cancellations in elective spine surgeries during this time. [65, 66]
Previous studies have reported a reduction in surgery among patients receiving CSMT. In one study, the reduction in odds of lumbar spine surgery was of a greater magnitude than our study (ie, 0.22); however, this study focused on a population with occupational back injury.18 Another study examining a broader population identified a reduction in likelihood of surgery of greater magnitude than our study (ie, risk ratio of 0.30). [14] A third similar study found a reduction in surgery among CSMT recipients, which was not statistically significant, likely due to small sample size. [16] While the current study reinforces these previous findings, the smaller magnitude of our ORs could be explained by the extensive selection criteria, narrow age bracket, propensity matching methods and differences in patient population.
Our sensitivity analysis suggested that an unmeasured confounder associated with both CSMT and discectomy would require a risk ratio associated with patients’ initial choice of CSMT for LDH/LSR of a magnitude of 1.92 to 2.26 to fully explain our results at 2–year and 1–year follow-up, respectively. While we are unaware of any unmeasured confounder of this magnitude based on recent research on this topic, [59] it is possible that one will be elucidated in future studies. Although the data in the current study includes insured and uninsured patients, socioeconomic variables were not included in the dataset, which remain potentially important unmeasured confounders.
Considering the current study excluded absolute indications for surgery and serious pathology, we suggest our findings may be explained by pain relief afforded by CSMT. Previous studies have shown that LDH/LSR have good prognosis with at least half of patients experiencing significant relief in the first 3–12 months. [67, 68] As most patients will undergo surgery within 2–12 months of symptom onset, [24] we suggest initial pain relief afforded by CSMT could allow patients to avoid surgery during this early critical period.
Further research is needed to expand on the current study. Chiefly, a randomised controlled trial could eliminate residual sources of confounding such as socioeconomic variables. In such a study, several outcomes could be measured in tandem including pain severity, disability, cost of care and pain medication utilisation, in addition to the rate of lumbar discectomy. The current study provides preliminary data to justify such a study, which would be more costly and time-consuming to conduct yet provide a higher level of evidence. Further, given our selection criteria focused on younger adults undergoing discectomy for LDH/LSR, a follow-up study could examine the likelihood of lumbar fusion surgery among older adults with lumbar stenosis.
Limitations
First, because of its observational design, this study is unable to conclude that CSMT is causative in reducing the odds of lumbar discectomy. There are several variables unavailable in the TriNetX dataset that could lead to unmeasured confounding such as those relating to socioeconomic status, clinical examination findings, [22] detailed spinal imaging data such as measures of disc herniation, [69] self-reported pain severity and impact and measures of catastrophising, self-efficacy and disability.
Second, data entered into a patient medical record may not be accurate, leading to an information bias in the aggregated health records data. [70] Certain comorbidities, prior diagnoses, treatments, medications or other patient variables could be absent, incorrect or outdated, [71] which could affect propensity matching or impact a patient’s eligibility for the current study. We were also unable to examine data completeness for all variables at an individual patient level. It was not feasible to validate our query against a gold standard of chart review given data was deidentified and sourced from outside healthcare organisations.
Third, we are unable to determine the techniques of CSMT employed by chiropractors for each patient, which may have differing efficacy. [72] Knowledge of techniques performed such as mobilisation, low-force, or high-velocity, low-amplitude CSMT could allow us to standardise the CSMT cohort to include a more uniform treatment, or enable subgroup analysis according to technique (eg, flexion distraction, lumbar high-velocity, low-amplitude manipulation, instrument assisted, etc). In addition, the number of visits in which CSMT was used likely varied between patients in the CSMT cohort, and this variable cannot be tracked in the study dataset.
Fourth, we were unable to examine the likelihood of visiting a surgeon due to a lack of provider codes in the dataset. Previous research has found that patients who initiate care for low back pain with a chiropractor have significantly reduced odds of visiting a surgeon. [16] Accordingly, it is unclear if a difference in surgical visits between cohorts mediates the association observed in our study.
Finally, as the study results derived from large, academically affiliated healthcare institutions, they may not be generalisable to patients seeking chiropractic care in private facilities.73 These results also may not be generalisable to healthcare settings outside of the USA.
Conclusion
These findings suggest that patients receiving CSMT for newly diagnosed LDH and/or LSR without serious pathology, spinal deformity or absolute indications for surgery have significantly reduced odds of discectomy through 2–year follow-up after index diagnosis compared with those receiving other care. While socioeconomic variables were unavailable in the dataset, current data suggests these unmeasured variables would not completely explain our findings. However, given the possibility of residual confounding, the efficacy of CSMT for LDH/LSR should be explored further using a randomised controlled trial.
Supplementary Material
Reviewer comments. (233K, pdf)
Author's manuscript. (2.6M, pdf)
Supplementary Tacles and Figures. (2.6M, pdf)Contributors:
RJT, CJD, RMC, JAP and JAD conceived of and designed the study. RMC and JAP were responsible for data collection and management of the study software and database. RJT, CD, JAP and JAD were responsible for data analysis and interpretation. JAD provided supervision and mentorship. RJT drafted the manuscript, while all authors critically revised and approved the final manuscript. RJT was the guarantor of the study.
Funding:
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests:
RJT reports he has received book royalties as the author of two texts on the topic of sciatica.
Ethics approval
This study was determined Not Human Subjects Research by the University Hospitals Institutional Review Board (Cleveland, Ohio, USA; STUDY20220571).
References:
Fardon DF, Williams AL, Dohring EJ, et al..
Lumbar disc nomenclature: version 2.0: recommendations of the combined task forces
of the North American spine Society, the American Society of spine radiology
and the American Society of Neuroradiology.
Spine J 2014;14:2525–45.
10.1016/j.spinee.2014.04.022Tarulli AW, Raynor EM.
Lumbosacral radiculopathy.
Neurol Clin 2007;25:387–405.
10.1016/j.ncl.2007.01.008et alHimelfarb I, Hyland J, Ouzts N.
National Board of Chiropractic Examiners:
Practice Analysis of Chiropractic 2020
NBCE, 2020.Beliveau PJH, Wong JJ, Sutton DA, Simon NB, Bussieres AE, Mior SA, et al.
The Chiropractic Profession: A Scoping Review of Utilization Rates,
Reasons for Seeking Care, Patient Profiles,
and Care Provided
Chiropractic & Manual Therapies 2017 (Nov 22); 25: 35Lawrence DJ, Meeker W, Branson R, Bronfort G, Cates JR, Haas M, Haneline M et al.
Chiropractic Management of Low Back Pain and Low Back-Related Leg Complaints:
A Literature Synthesis
J Manipulative Physiol Ther 2008 (Nov); 31 (9): 659–674McMorland G, Suter E, Casha S, du Plessis SJ, Hurlbert RJ.
Manipulation or Microdiskectomy for Sciatica?
A Prospective Randomized Clinical Study
J Manipulative Physiol Ther. 2010 (Oct); 33 (8): 576–584Santilli V, Beghi E, Finucci S.
Chiropractic Manipulation in the Treatment of Acute Back Pain and Sciatica
with Disc Protrusion: A Randomized Double-blind Clinical Trial
of Active and Simulated Spinal Manipulations
Spine J. 2006 (Mar); 6 (2): 131—137Lewis RA, Williams NH, Sutton AJ, et al..
Comparative clinical effectiveness of management strategies for sciatica:
systematic review and network meta-analyses.
Spine J 2015;15:1461–77.
10.1016/j.spinee.2013.08.049Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530Van Wambeke P, Desomer A, Ailiet L.
Belgian health care knowledge centre KCE report 287Cs:
Low Back Pain and Radicular Pain:
Assessment and Management 2017Wong JJ, Côté P, Sutton DA, et al.
Clinical Practice Guidelines for the Noninvasive Management of
Low Back Pain: A Systematic Review by the Ontario Protocol
for Traffic Injury Management (OPTIMa) Collaboration
European J Pain 2017 (Feb); 21 (2): 201–216National Institute for Health and Care Excellence (NICE):
Low Back Pain and Sciatica in Over 16s: Assessment and Management (PDF)
NICE Guideline, No. 59 2016 (Nov): 1–1067Globe G, Farabaugh RJ, Hawk C, et al.
Clinical Practice Guideline:
Chiropractic Care for Low Back Pain
J Manipulative Physiol Ther 2016 (Jan); 39 (1): 1–22Anderson BR, McClellan SW.
Three Patterns of Spinal Manipulative Therapy for Back Pain
and Their Association With Imaging Studies, Injection
Procedures, and Surgery: A Cohort Study
of Insurance Claims
J Manipulative Physiol Ther 2021 (Nov); 44 (9): 683–689Anderson B.
A secondary analysis of insurance claims data to determine the association
between provider type and treatment escalation in musculoskeletal disorders.
Northern Illinois university, 2019
https://search.proquest.com/openview/da5d43e1ca5390f9afbcf53494d31bca/
1?pq-origsite=gscholar&cbl=18750&diss=yFritz JM, Kim J, Dorius J.
Importance of the Type of Provider Seen to Begin Health Care
for a New Episode Low Back Pain: Associations with
Future Utilization and Costs
J Eval Clin Pract. 2016 (Apr); 22 (2): 247–252Weeks, WB, Leininger, B, Whedon, JM et al.
The Association Between Use of Chiropractic Care and Costs of Care
Among Older Medicare Patients With Chronic Low Back Pain
and Multiple Comorbidities
J Manipulative Physiol Ther. 2016 (Feb); 39 (2): 63–75Keeney BJ, Fulton-Kehoe D, Turner JA, et al..
Early Predictors of Lumbar Spine Surgery After Occupational
Back Injury: Results From a Prospective Study
of Workers in Washington State
Spine (Phila Pa 1976). 2013 (May 15); 38 (11): 953–964Nelson CF, Metz RD, LaBrot T.
Effects of a Managed Chiropractic Benefit on the Use of
Specific Diagnostic and Therapeutic Procedures in the
Treatment of Low Back and Neck Pain
J Manipulative Physiol Ther 2005 (Oct); 28 (8): 564–569Legorreta, AP, Metz, RD, Nelson, CF, Ray, S, Chernicoff, HO, and Dinubile, NA.
Comparative Analysis of Individuals With and Without Chiropractic Coverage:
Patient Characteristics, Utilization, and Costs
Archives of Internal Medicine 2004 (Oct 11); 164 (18): 1985–1892Arts MP, Peul WC, Leiden-Hague Spine Intervention Prognostic Study Group .
Timing and minimal access surgery for sciatica:
a summary of two randomized trials.
Acta Neurochir 2011;153:967–74.
10.1007/s00701-011-0983-8Vroomen PC, de Krom MC, Knottnerus JA.
When does the patient with a disc herniation undergo lumbosacral discectomy?
J Neurol Neurosurg Psychiatry 2000;68:75–9.
10.1136/jnnp.68.1.75Boden LM, Boden SA, Premkumar A, et al.
Predicting likelihood of surgery before first visit in patients with back
and lower extremity symptoms: a simple mathematical model
based on more than 8,000 patients.
Spine 2018;43:1296–305.
10.1097/BRS.0000000000002603Sabnis AB, Diwan AD.
The timing of surgery in lumbar disc prolapse: a systematic review.
Indian J Orthop 2014;48:127.
10.4103/0019-5413.128740Jacobs WCH, van Tulder M, Arts M, et al.
Surgery versus conservative management of sciatica due to
a lumbar herniated disc: a systematic review.
Eur Spine J 2011;20:513–22.
10.1007/s00586-010-1603-7Trager RJ, Daniels CJ, Ravanpay AC.
The association between chiropractic spinal manipulation and
lumbar discectomy in adults: a retrospective cohort study protocol 2022Franklin JM, Schneeweiss S.
When and how can real world data analyses substitute
for randomized controlled trials?
Clin Pharmacol Ther 2017;102:924–33.
10.1002/cpt.857von Elm E, Altman DG, Egger M, et al.
The strengthening the reporting of observational studies in epidemiology
(STROBE) statement: guidelines for reporting observational studies.
Ann Intern Med 2007;147:573–7.
10.7326/0003-4819-147-8-200710160-00010Topaloglu U, Palchuk MB.
Using a federated network of real-world data to
optimize clinical trials operations.
JCO Clin Cancer Inform 2018;2:1–10.
10.1200/CCI.17.00067Stapff M, Stacey J.
How can real-world data support clinical trials and medical research?
Clin Res 2019;33.Pfaff ER, Girvin AT, Gabriel DL, et al.
Synergies between centralized and federated approaches to data quality:
a report from the National COVID cohort collaborative.
J Am Med Inform Assoc 2022;29:609–18.
10.1093/jamia/ocab217Evans L, London JW, Palchuk MB.
Assessing real-world medication data completeness.
J Biomed Inform 2021;119:103847.
10.1016/j.jbi.2021.103847Trager RJ, Anderson BR, Casselberry RM, et al.
Guideline-concordant utilization of magnetic resonance imaging in adults
receiving chiropractic manipulative therapy vs other care for
radicular low back pain: a retrospective cohort study.
BMC Musculoskelet Disord 2022;23:554.
10.1186/s12891-022-05462-ySalsbury SA, Goertz CM, Twist EJ, Lisi AJ.
Integration of Doctors of Chiropractic Into Private Sector
Health Care Facilities in the United States:
A Descriptive Survey
J Manipulative Physiol Ther. 2018 (Feb); 41 (2): 149–155Stynes S, Konstantinou K, Dunn KM.
Classification of patients with low back-related leg pain:
a systematic review.
BMC Musculoskelet Disord 2016;17:226.
10.1186/s12891-016-1074-zSabatino MJ, Burroughs PJ, Moore HG, et al.
Spine coding transition from ICD-9 to ICD-10:
not taking advantage of the specificity of a more granular system.
N Am Spine Soc J 2020;4:100035.
10.1016/j.xnsj.2020.100035Jönsson B, Strömqvist B.
Symptoms and signs in degeneration of the lumbar spine.
A prospective, consecutive study of 300 operated patients.
J Bone Joint Surg Br 1993;75:381–5.
10.1302/0301-620X.75B3.8496204Miyakoshi N, Hongo M, Kasukawa Y, et al.
Prevalence, spinal alignment, and mobility of lumbar spinal stenosis
with or without chronic low back pain: a community-dwelling study.
Pain Res Treat 2011;2011:340629.
10.1155/2011/340629Giardina JC, Cha T, Atlas SJ, et al.
Validation of an electronic coding algorithm to identify the primary
indication of orthopedic surgeries from administrative data.
BMC Med Inform Decis Mak 2020;20:1–10.
10.1186/s12911-020-01175-1Gandhi R, Perruccio AV, Rampersaud YR.
Predictors of willingness to undergo elective musculoskeletal surgery.
Patient Prefer Adherence 2013;7:191.
10.2147/PPA.S41852Pennington Z, Lubelski D, Tanenbaum J, et al.
Utility of patient-reported symptoms and health conditions for predicting
surgical Candidacy and utilization of surgery via an
outpatient spine clinic nomogram.
Clin Spine Surg 2019;32:E407–15.
10.1097/BSD.0000000000000838Webster BS, Verma SK, Gatchel RJ.
Relationship between early opioid prescribing for acute occupational
low back pain and disability duration, medical costs,
subsequent surgery and late opioid use.
Spine 2007;32:2127–32.
10.1097/BRS.0b013e318145a731Fukushima M, Oka H, Hara N, et al.
Prognostic factors associated with the surgical indication for lumbar
spinal stenosis patients less responsive to conservative treatments:
an investigator-initiated observational cohort study.
J Orthop Sci 2017;22:411–4.
10.1016/j.jos.2017.01.021Suri P, Carlson J, Rainville J.
Nonoperative treatment for lumbosacral radiculopathy: what factors
predict treatment failure?, Nonoperative treatment for lumbosacral
radiculopathy: what factors predict treatment failure?
Clin Orthop Relat Res Clin Orthop Relat Res 2015;473:1931–9.Whedon JM, Haldeman S, Petersen CL, et al.
Temporal trends and geographic variations in the supply of clinicians
who provide spinal manipulation to Medicare beneficiaries:
a serial cross-sectional study.
J Manipulative Physiol Ther 2021;44:177–85.
10.1016/j.jmpt.2021.02.002Castillo H, Chintapalli RTV, Boyajian HH, et al.
Lumbar discectomy is associated with higher rates of lumbar fusion.
Spine J 2019;19:487–92.
10.1016/j.spinee.2018.05.016Lorio M, Kim C, Araghi A, et al.
International Society for the advancement of spine surgery policy 2019-
Surgical treatment of lumbar disc herniation with radiculopathy.
Int J Spine Surg 2020;14:1–17.
10.14444/7001Association AM .
ICD-10-PCS 2020: The Complete Official Codebook.
American Medical Association, 2019.Bergstra SA, Sepriano A, Ramiro S, et al.
Three handy tips and a practical guide to improve your propensity score models.
RMD Open 2019;5:e000953.
10.1136/rmdopen-2019-000953Kardouni JR, Shing TL, Rhon DI.
Risk factors for low back pain and spine surgery:
a retrospective cohort study in soldiers.
Am J Prev Med 2016;51:e129–38.
10.1016/j.amepre.2016.06.005Babington JR, Edwards A, Wright AK.
Patient-Reported outcome measures: utility for predicting
spinal surgery in an integrated spine practice.
PM&R 2018;10:724–9.
10.1016/j.pmrj.2017.12.004Friedly J, Nishio I, Bishop MJ, et al.
The relationship between repeated epidural steroid injections
and subsequent opioid use and lumbar surgery.
Arch Phys Med Rehabil 2008;89:1011–5.
10.1016/j.apmr.2007.10.037Faul F. G*
Power. 1992.Mathur MB, Ding P, Riddell CA, et al.
Web site and R package for computing E-values.
Epidemiology 2018;29:e45–7.
10.1097/EDE.0000000000000864VanderWeele TJ, Ding P.
Sensitivity analysis in observational research:
introducing the E-value.
Ann Intern Med 2017;167:268–74.
10.7326/M16-2607Sharma R, Haas M, Stano M.
Patient Attitudes, Insurance, and Other Determinants of
Self-referral to Medical and Chiropractic Physicians
American J Public Health 2003 (Dec); 93 (12): 2111–2117Nyiendo J, Haas M, Goldberg B.
Pain, Disability, and Satisfaction Outcomes and Predictors of Outcomes:
A Practice-based Study hronic Low Back Pain Patients
Attending Primary Care and Chiropractic Physicians
J Manipulative Physiol Ther. 2001 (Sep); 24 (7): 433–439Nyiendo J, Haas M, Goldberg B, Sexton G.
Patient Characteristics and Physicians' Practice Activities for
Patients with Chronic Low Back Pain: A Practice-based Study
of Primary Care and Chiropractic Physicians
J Manipulative Physiol Ther 2001 (Feb); 24 (2): 92–100Chevan J, Riddle DL.
Factors associated with care seeking from physicians, physical therapists,
or chiropractors by persons with spinal pain:
a population-based study.
J Orthop Sports Phys Ther 2011;41:467–76.
10.2519/jospt.2011.3637Kim LH, Vail D, Azad TD, Bentley JP, Zhang Y, Ho AL, Faterni P, Feng A.
Expenditures and Health Care Utilization Among Adults
with Newly Diagnosed Low Back and Lower Extremity Pain
JAMA Network Open 2019 (May 3); 2 (5): e193676Mahmood TS, Saeid SA, Afsoun S.
Clinical results of 30 years surgery on 2026 patients
with lumbar disc herniation.
World Spin Column J 2012;3:80–6.Motiei-Langroudi R, Sadeghian H, Seddighi AS.
Clinical and magnetic resonance imaging factors which may
predict the need for surgery in lumbar disc herniation.
Asian Spine J 2014;8:446–52.
10.4184/asj.2014.8.4.446Gupta A, Upadhyaya S, Yeung CM, et al.
Does size matter? an analysis of the effect of lumbar disc
herniation size on the success of Nonoperative treatment.
Global Spine J 2020;10:881–7.
10.1177/2192568219880822Buser Z, Ortega B, D'Oro A, D’Oro A, et al..
Spine degenerative conditions and their treatments:
national trends in the United States of America.
Global Spine J 2018;8:57–67.
10.1177/2192568217696688Arnold PM, Owens L, Heary RF, et al.
Lumbar spine surgery and what we lost in the era of the coronavirus pandemic.
Clin Spine Surg 2021;34:E575–9.
10.1097/BSD.0000000000001235Norris ZA, Sissman E, O'Connell BK, et al.
COVID-19 pandemic and elective spinal surgery cancelations -
what happens to the patients?
Spine J 2021;21:2003–9.
10.1016/j.spinee.2021.07.019Vroomen PCAJ, de Krom MCTFM, Knottnerus JA, PCAJ V, de KM.
Predicting the outcome of sciatica at short-term follow-up.
Br J Gen Pract 2002;52:119–23.Haugen AJ, Grřvle L, Brox JI, et al.
Estimates of success in patients with sciatica due to
lumbar disc herniation depend upon outcome measure.
Eur Spine J 2011;20:1669–75.
10.1007/s00586-011-1809-3Gupta A, Upadhyaya S, Yeung CM, et al.
Caudal lumbar disc herniations are more likely to require surgery for symptom resolution.
Global Spine J 2021;11:359–64.
10.1177/2192568220905849Gokhale M, Stürmer T, Buse JB.
Real-World evidence: the devil is in the detail.
Diabetologia 2020;63:1694–705.
10.1007/s00125-020-05217-1Callahan A, Shah NH, Chen JH.
Research and reporting considerations for observational
studies using electronic health record data.
Ann Intern Med 2020;172:S79–84.
10.7326/M19-0873Schneider, M, Haas, M, Glick, R, Stevans, J, and Landsittel, D.
Comparison of Spinal Manipulation Methods and Usual Medical Care
for Acute and Subacute Low Back Pain:
A Randomized Clinical Trial
Spine (Phila Pa 1976). 2015 (Feb 15); 40 (4): 209–217Lubelski D, Williams SK, O'Rourke C, et al.
Differences in the surgical treatment of lower back pain
among spine surgeons in the United States.
Spine 2016;41:978–86.
10.1097/BRS.0000000000001396Schneeweiss S, Rassen JA, Brown JS, et al.
Graphical Depiction of longitudinal study designs in health care databases.
Ann Intern Med 2019;170:398–406. 10.7326/M18-3079
Return to LOW BACK PAIN
Return to RADICULOPATHY
Return to INITIAL PROVIDER/FIRST CONTACT
Since 2-15-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |