|
Beauty Parlor Stroke Syndrome
A Chiro.Org article collection
If you think chiropractic adjustments can cause stroke, please review this series of abstracts. Extension and rotational stressors, on an already–diseased Vertebral Artery, is the real culprit. There has been less reporting of “Beauty Parlor Stroke” than there has been for chiropractic–related strokes, but it is likely it occurs much more frequently.
|

|
Bow Hunter's Stroke
A Chiro.Org article collection
Another instance of extension and rotational stresses leading to stroke.
|

|
Iatrogenic Vertebral Artery Injury
A Chiro.Org article collection
Vertebral Arteries are also injured during a wide variety of medical procedures and surgeries.
|

|
Stroke & Essential Fatty Acids
A Chiro.Org article collection
Stroke is the third leading cause of death in the US. Fortunately, diagnostic imaging for stroke risk and stroke-prevention strategies have advanced greatly in recent years. It is now possible to reduce the artery-clogging plaque that leads to stroke, offering hope that this debilitating condition can be prevented.
|

|
A Workout to Remember: CrossFit-Induced
Vertebral Artery Dissection
Cureus 2023 (Jun 30); 15 (6): e41211 ~ FULL TEXT
Vertebral artery dissection (VAD) is a cause of brain stem stroke in the younger population and is commonly associated with trauma, sudden neck movement, or chiropractic manipulations. In this case, a 28–year-old male with a non-significant past medical history who recently started a CrossFit boot camp presented to the emergency department with right-sided neck pain, dysarthria, mild right gaze paresis, right dysmetria, and right facial droop with symptoms of Horner's syndrome. Imaging results revealed an age-indeterminate left lateral cerebellar infarct with right VAD. The goal of management is to prevent stroke, which is done with anticoagulation and potentially thrombolytic therapy if there are no contraindications. The patient received thrombolytic therapy and was treated with conservative management. The prognosis is good for patients who survive the initial dissection and are treated in this manner. It is important to obtain a thorough history of young and healthy patients who present with concerning neurologic symptoms so that precipitating activities are not missed.
|

|
An Adult Patient With Acute Ischemic Stroke and
Carotid Stenosis Presenting to a Chiropractor:
A Case Report
Cureus 2023 (Apr 6); 15 (4): e37209 ~ FULL TEXT
A 59-year-old male, with a recent history of acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pneumonia, presented to a chiropractor with a one-week history of numbness in the right upper and lower extremity that was triggered by neck movement, and lightheadedness/dizziness. On examination, the chiropractor noted limited, painful cervical spine range of motion, right upper extremity weakness, patellar hyperreflexia, positive Hoffman's and Trömner's signs bilaterally, nystagmus, a sluggish right pupillary light reflex, and carotid bruit. Cervical radiographs were suggestive of Klippel-Feil syndrome. The chiropractor suspected a vascular cause such as a transient ischemic attack and referred the patient to the emergency department, which the patient visited the following day. The patient was admitted, and MRI revealed multiple tiny acute to subacute cortical infarcts of the left frontal and parietal lobes while sonography demonstrated left internal carotid artery stenosis. The patient was treated with anticoagulant and antiplatelet medications and carotid endarterectomy with a positive outcome. Given the overlap between symptoms of stroke and those of the cervical spine, chiropractors should be prepared to recognize potential stroke patients and refer them for emergent medical management.
|

|
Effects of Manual Versus Instrumental Spinal Manipulation
on Blood Flow of the Vertebral and Internal Carotid
Arteries in Participants With Chronic Nonspecific
Neck Pain: A Single-Blind, Randomized Study
J Chiropractic Medicine 2023 (Mar); 22 (1): 1–10 ~ FULL TEXT
Intragroup analysis exhibited no statistically significant difference between the manual spinal manipulation (MSM) and instrumental spinal manipulation (ISM) groups in terms of of peak systolic velocity (PSV), end-diastolic velocity, resistive index of ipsilateral and contralateral ICA and VA, in addition to volume flow of both VAs preintervention and postintervention (P > .05). Within the intergroup analysis, there was a significant difference in ipsilateral ICA PSV (P = .031) (preintervention vs postintervention difference was –7.9 ± 17.2 cm/s [95% confidence interval, –17.4 to 1.6] in the ISM group and 8.7 ± 22.5 cm/s [95% confidence interval, –3.6 to 21.2]) in the MSM group (P < .05). Other parameters did not show any significant difference (P > .05). Conclusion Manual and instrumental spinal manipulations applied to the upper cervical spine in participants with chronic NNP did not appear to alter blood flow parameters of the VAs and ICAs.
|

|
Association Between Cervical Artery Dissection and
Spinal Manipulative Therapy -
A Medicare Claims Analysis
BMC Geriatrics 2022 (Nov 29); 22 (1): 917 ~ FULL TEXT
Among Medicare beneficiaries aged 65 and older who received cervical spine manipulation, the association with cervical artery dissection is no greater than that among the control groups, and CSM does not appear to be a significant risk factor for cervical artery dissection (CeAD) in this population group.
|

|
Vertebral Arteries Do Not Experience Tensile Force
During Manual Cervical Spine Manipulation
Applied to Human Cadavers
J Man Manip Ther 2022 (Nov 15); 1–9 ~ FULL TEXT
Measured in arbitrary in-situ head/neck positions, VA were slack. It appears that this slack must be taken up prior to VA experiencing tensile force. During cervical spine manipulations (using cervical spine extension and rotation), arterial length changes remained below that slack length, suggesting that VA elongated but were not stretched during the manipulation. However, in order to answer the question if cervical spine manipulation is safe from a mechanical perspective, the testing performed here needs to be repeated using a defined in-situ head/neck position and take into consideration other structures (e.g. carotid arteries).
|

|
Chiropractic Management of Neck Pain Complicated by
Symptomatic Vertebral Artery Stenosis and Dizziness
American Journal of Case Reports (Sep 14) 2022 [Epub] ~ FULL TEXT
This case highlights a patient with neck pain and concurrent
VBI, with confirmed VBI on imaging related to vertebral artery
stenosis that responded positively to thoracic SMT and soft tissue manipulation. Four cases were reported in the literature in which chiropractors either avoided manual cervical SMT altogether or modified it to reduce or avoid cervical rotation as a safety precaution when treating neck pain among patients with VBI, yielding a positive outcome. However, as there is insufficient evidence that cervical SMT is safe for patients with VBI, this therapy should be avoided in these patients. As illustrated in the present case and supported by recent esearch, thoracic SMT or soft tissue manipulation may provide alternative means of alleviating neck pain in those with VBI. Practitioners considering these treatments should do so in collaboration with medical specialists and on a case-by-case basis.
|

|
The Effects of 4 Weeks of Chiropractic Spinal Adjustments
on Motor Function in People with Stroke:
A Randomized Controlled Trial
Brain Sciences 2021 (May 21); 11 (6): 676 ~ FULL TEXT
Improvements in motor function were observed when chiropractic care was added to 4 weeks of physical therapy care in people with subacute or chronic stroke. These improvements were statistically significant and a post-hoc responder analysis suggested they were also likely to be clinically significant. Chiropractic spinal adjustments may therefore be beneficial for people with motor impairments associated with subacute or chronic stroke. Further research, involving larger group sizes and longer-term follow-up and intervention periods, is required to corroborate these findings and further investigate the impacts of chiropractic care on motor function in people with stroke.
|

|
A Risk-benefit Assessment Strategy to Exclude Cervical
Artery Dissection in Spinal Manual-therapy:
A Comprehensive Review
Annals of Medicine 2019 (Mar 19): 51 (2): 118–127 ~ FULL TEXT
Cervical artery dissection refers to a tear in the internal carotid or the vertebral artery that results in an intramural haematoma and/or an aneurysmal dilatation. Although cervical artery dissection is thought to occur spontaneously, physical trauma to the neck, especially hyperextension and rotation, has been reported as a trigger. Headache and/or neck pain is the most common initial symptom of cervical artery dissection. Other symptoms include Horner's syndrome and lower cranial nerve palsy. Both headache and/or neck pain are common symptoms and leading causes of disability, while cervical artery dissection is rare. Patients often consult their general practitioner for headache and/or neck pain, and because manual-therapy interventions can alleviate headache and/or neck pain, many patients seek manual therapists, such as chiropractors and physiotherapists. Cervical mobilization and manipulation are two interventions that manual therapists use. Both interventions have been suspected of being able to trigger cervical artery dissection as an adverse event. The aim of this review is to provide an updated step-by-step risk-benefit assessment strategy regarding manual therapy and to provide tools for clinicians to exclude cervical artery dissection.
|

|
The Effects of a Single Session of Chiropractic Care on
Strength, Cortical Drive, and Spinal Excitability
in Stroke Patients
Scientific Reports 2019 (Feb 25); 9 (1): 2673 ~ FULL TEXT
In this group of stroke patients, with plantar flexor muscle weakness, a single session of chiropractic care resulted in increased plantar flexor muscle strength and cortical drive to the affected limb. Further research is required to investigate the longer term and potential functional effects of chiropractic care in stroke recovery.
|

|
Spontaneous Cervical Artery Dissection:
A Fluoroquinolone Induced Connective Tissue Disorder?
Chiropractic & Manual Therapies 2018 (Jul 9); 26: 22 ~ FULL TEXT
Spontaneous cervical artery dissections more often manifest in young people and have been associated with catastrophic consequences. Some indeterminate risk factors have been identified, making the diagnosis of developing dissections quite difficult. Fluoroquinolone antibiotics have been recognized for their degradative effects on connective tissue. Recent studies have implicated fluoroquinolones in the genesis of aortic artery aneurysms. It is the purpose of this paper to provide reasoning for a testable hypothesis of whether fluoroquinolones constitute a risk factor associated with cervical artery dissections. A causal relationship of fluoroquinolone antibiotics to cervical artery dissection is plausible. The suppositions developed in this paper are insufficient to suggest that fluoroquinolones currently represent an established risk factor in the development of cervical artery dissections. Fluoroquinolones may indeed be a novel and previously unrecognized cause of cervical artery dissections.
|

|
Risk of Carotid Stroke after Chiropractic Care:
A Population-Based Case-Crossover Study
J Stroke Cerebrovasc Dis. 2017 (Apr); 26 (4): 842–850 ~ FULL TEXT
We compared 15,523 cases to 62,092 control periods using exposure windows of 1, 3, 7, and 14 days prior to the stroke. Positive associations were found for both chiropractic and PCP visits and subsequent stroke in patients less than 45 years of age. These associations tended to increase when analyses were limited to visits for neck pain and headache-related diagnoses. There was no significant difference between chiropractic and PCP risk estimates. We found no association between chiropractic visits and stroke in those 45 years of age or older. We found no excess risk of carotid artery stroke after chiropractic care. Associations between chiropractic and PCP visits and stroke were similar and likely due to patients with early dissection-related symptoms seeking care prior to developing their strokes.
|

|
Chiropractic Response to a Spontaneous
Vertebral Artery Dissection
J Chiropractic Medicine 2015 (Sep); 14 (3): 183–190 ~ FULL TEXT
The patient was not treated on the initial visit but was advised of the possibility of a vertebral artery or carotid artery dissection and was recommended to the emergency department for immediate evaluation. The patient declined but later was convinced by her chiropractor to present to the emergency department. A magnetic resonance angiogram of the neck and carotid arteries was performed showing that the left vertebral artery was hypoplastic and appeared to terminate at the left posterior inferior cerebellar artery. There was an abrupt moderately long segment of narrowing involving the right vertebral artery beginning near the junction of the V1 and V2 segments. The radiologist noted a concern regarding right vertebral artery dissection. Symptoms resolved and the patient was cleared of any medications but advised that if symptoms reoccurred she was to go for emergency care immediately.
|

|
Risk of Stroke After Chiropractic Spinal Manipulation
in Medicare B Beneficiaries Aged 66 to 99 Years
With Neck Pain
J Manipulative Physiol Ther. 2015 (Feb); 38 (2): 93–101 ~ FULL TEXT
The proportion of subjects with stroke of any type in the chiropractic cohort was 1.2 per 1000 at 7 days and 5.1 per 1000 at 30 days. In the primary care cohort, the proportion of subjects with stroke of any type was 1.4 per 1000 at 7 days and 2.8 per 1000 at 30 days. In the chiropractic cohort, the adjusted risk of stroke was significantly lower at 7 days as compared to the primary care cohort (hazard ratio, 0.39; 95% confidence interval, 0.33-0.45), but at 30 days, a slight elevation in risk was observed for the chiropractic cohort (hazard ratio, 1.10; 95% confidence interval, 1.01-1.19). Among Medicare B beneficiaries aged 66 to 99 years with neck pain, incidence of vertebrobasilar stroke was extremely low. Small differences in risk between patients who saw a chiropractor and those who saw a primary care physician are probably not clinically significant.
|

|
Risk of Traumatic Injury Associated with Chiropractic Spinal
Manipulation in Medicare Part B Beneficiaries Aged 66-99
Spine (Phila Pa 1976) 2015 (Feb 15); 40 (4): 264–270
Among Medicare beneficiaries aged 66-99 with an office visit risk for a neuromusculoskeletal problem, risk of injury to the head, neck or trunk within 7 days was 76% lower among subjects with a chiropractic office visit as compared to those who saw a primary care physician.
|

|
Recognition of Spontaneous Vertebral Artery Dissection
Preempting Spinal Manipulative Therapy: A Patient
Presenting With Neck Pain and Headache
for Chiropractic Care
J Chiropractic Medicine 2014 (Jun); 13 (2): 90–95 ~ FULL TEXT
This case highlights the potential for patients with vertebral artery dissection to present with nonspecific musculoskeletal complaints. Neurological symptoms may not manifest initially, but their sudden onset indicates the possibility of an ischemic cerebrovascular event. We suggest that early recognition and emergent referral for this patient avoided potential exacerbation of an evolving pre-existing condition and resulted in timely anticoagulation treatment.
|

|
Elongated Styloid Processes and Calcified Stylohyoid
Ligaments in a Patient With Neck Pain:
Implications for Manual Therapy Practice
J Chiropractic Medicine 2014 (Jun); 13 (2): 128–133 ~ FULL TEXT
Neck pain in the presence of elongated styloid processes (ESPs) and calcified stylohyoid ligaments (CSLs) can be associated with Eagle syndrome, which can include ipsilateral head and neck pain, odynophagia, dysphagia, and cerebrovascular symptoms. This case, initially thought to be Eagle syndrome, highlights proper diagnostic workup for this condition and presents potential contraindications to consider with regard to cervical spine manipulation in such patients. Manual therapy precautions pertaining to cervical spine manipulation may be appropriate in cases involving ESPs and calcified stylohyoid ligaments.
|

|
Vertebral Artery Dissection as a Cause
of Cervical Radiculopathy
Asian Spine J. 2013 (Dec); 7 (4): 335–338 ~ FULL TEXT
We describe a case of vertebral artery dissection presenting as cervical radiculopathy in a previously healthy 43-year-old woman who presented with proximal left arm weakness and neck pain aggravated by movement. Cervical magnetic resonance imaging (MRI) and angiography revealed dissection of the left vertebral artery with an intramural hematoma compressing the left C5 and C6 nerve roots.
|

|
WARNING:
Conducting an Orchestra Can Cause Vertebral
Artery Dissection: "Ostrich Sign" Indicates
Bilateral Vertebral Artery Dissection
Journal of Stroke and Cerebrovascular Diseases 2012 (Nov); 21 (8): 903. e1–2
Vertebral artery dissections (VADs) comprise about 2% of ischemic strokes and can be associated with trauma, chiropractic manipulation, motor vehicle collisions, whiplash, amusement park rides, golfing, and other motion-induced injuries to the neck. We present a case of bilateral extracranial VAD as a complication of conducting an orchestra. To our knowledge, this has not been documented in the literature. Conceivably, vigorous neck twisting in an inexperienced, amateur conductor may place excessive rotational forces upon mobile portions of the verterbral arteries, tear the intima, deposit subintimal blood that extends longitudinally, and cause neck pain and/or posterior fossa ischemic symptoms.
|

|
Risk Factors and Clinical Presentation of Craniocervical
Arterial Dissection: A Prospective Study
BMC Musculoskelet Disord. 2012 (Sep 3); 13: 164 ~ FULL TEXT
This study will provide descriptive and comparative data on intrinsic and extrinsic risk factors for craniocervical arterial dissection and outline the typical clinical presentation, including the nature of early presenting features which might assist practitioners to identify those patients for whom vigorous manual therapy of the neck is inappropriate and alert them to those for whom immediate urgent medical care should be sought.
|

|
Recognition of Perinatal Stroke in a Chiropractic
Practice: Case Report and Clinical Challenges
Related to a Late Diagnosis
J Clinical Chiropractic Pediatrics 2012 (Jun); 13 (1): 958–967 ~ FULL TEXT
In recent years, improvements in medical techniques and technology have enabled primary health care practitioners to diagnose perinatal strokes in infants far earlier than ever before. This new technology can also support chiropractors, especially those working with pediatric patients, in order to validate their diagnosis when they recognize these initial symptoms.
|

|
Vertebral Artery Dissection in a Patient
Practicing Self-manipulation of the Neck
J Chiropractic Medicine 2011 (Dec); 10 (4): 283–287 ~ FULL TEXT
The purpose of this case report is to describe a patient who regularly practiced self-manipulation of her neck who presented with shoulder and neck pain and was undergoing a vertebral artery dissection.
|

|
The Safety of Cervical Manipulation:
Putting Stroke Risk in Perspective
Dynamic Chiropractic 2011 (May 20); 29 (11): 29, 43, 45 ~ FULL TEXT
Several studies have attempted to link chiropractic manipulation to adverse events, the most serious and widely studied being strokes following dissections of the vertebral artery. [1–6] To begin to shed light on this problem, several retrospective studies against large population bases have been conducted. As shown in Table 1, [7–15] a large sampling of such studies indicates that the number of serious complications or cerebrovascular accidents (CVAs), as established by researchers from both the chiropractic and medical professions, ranges from one case per 400,000 manipulations to zero in 5 million.
|

|
A Population-Based Case-Series of Ontario Patients Who Develop a
Vertebrobasilar Artery Stroke After Seeing a Chiropractor
J Manipulative Physiol Ther 2011 (Jan); 34 (1): 15–22 ~ FULL TEXT
Ninety-three VBA stroke cases consulted a chiropractor during the year before their stroke. The mean age was 57.6 years (SD, 16.1), and 50% were female. Most cases had consulted a medical doctor during the year before their stroke, and 75.3% of patients had at least one cerebrovascular comorbidity. The 3 most common comorbidities were neck pain and headache (prevalence, 66.7%; 95% confidence interval [CI], 57.0%-76.3%), diseases of the circulatory system (prevalence, 63.4%; 95% CI, 54.8%-74.2%), and diseases of the nervous system and sense organs (prevalence, 47.3%; 95% CI, 38.7%-58.1%). Our population-based analysis suggests that VBA stroke patients who consulted a chiropractor the year before their stroke are older than previously documented in clinical case series. We did not find that women were more commonly affected than men. Moreover, we found that most patients had at least one cardio- or cerebrovascular comorbidity. Our analysis suggests that relying on case series or surveys of health care professionals may provide a biased view of who develops a VBA stroke.
|

|
Patients With Symptoms and Signs of Stroke
Presenting to a Rural Chiropractic Practice
J Manipulative Physiol Ther 2010 (Jan); 33 (1): 62–69 ~ FULL TEXT
Patients with symptoms and signs of stroke may infrequently present to chiropractic physicians for evaluation and treatment, regardless of the interval since the last prior chiropractic treatment. Several prehospital stroke recognition instruments were introduced in the mid-1990s, including the Los Angeles Paramedic Stroke Scale, the Cincinnati Prehospital Stroke Scale, and in the United Kingdom the Face Arm Speech Test (FAST), a modification of the Cincinnati scale. [37] The FAST seems particularly well suited as a tool for chiropractic physicians, their staff, and for patient education; indeed, this tool is already being used by health educators and nurses to train persons for rapid stroke recognition (Table 4). [5]
Table 4. The Face Arm Speech Test, also known as FAST [5]
|
F
|
Face: Ask person to smile. Does one side of the face droop?
|
|
A
|
Arm: Ask person to raise both arms. Does one arm drift downward?
|
|
S
|
Speech: Ask the person to say their name or a simple sentence. Is the speech slurred or unusual?
|
|
T
|
Time: If any of these signs, call 911 or get to the nearest stroke center or hospital immediately.
|
|

|
Examining Vertebrobasilar Artery Stroke
in Two Canadian Provinces
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S170–175 ~ FULL TEXT
Under the assumption that chiropractic manipulation to the cervical spine is a risk factor for VBA stroke, it is possible that the increase in incidence may have been related to an increase in the utilization of chiropractic services. However, 2 observations do not support this hypothesis. First, we found that the incidence rate of VBA strokes was similar in Saskatchewan and Ontario even though chiropractic utilization was 10 times higher in Saskatchewan than in Ontario. Second, the sharp increase in the rate of VBA stroke occurred despite a decrease in chiropractic utilization in Ontario. In Saskatchewan, the sharp increase in the incidence of VBA strokes occurred whereas the chiropractic utilization remained fairly stable. These findings are in agreement with the results of Cassidy et al who found that there was no significant added risk associated with antecedent exposure to a chiropractor before VBA compared against the risk associated with exposure to a primary care physician in the ambulatory setting. [7]
|

|
Safety of Chiropractic Manipulation of the Cervical Spine:
A Prospective National Survey
Spine (Phila Pa 1976). 2007 (Oct 1); 32 (21): 2375–2378 ~ FULL TEXT
Data were obtained from 28,807 treatment consultations and 50,276 cervical spine manipulations. There were no reports of serious adverse events. This translates to an estimated risk of a serious adverse event of, at worse approximately 1 per 10,000 treatment consultations immediately after cervical spine manipulation, approximately 2 per 10,000 treatment consultations up to 7 days after treatment and approximately 6 per 100,000 cervical spine manipulations. Minor side effects with a possible neurologic involvement were more common. The highest risk immediately after treatment was fainting/dizziness/light-headedness in, at worse approximately 16 per 1000 treatment consultations.
|

|
Cervical Spine Adjusting and the Vertebral Artery (PowerPoint)
Association of Chiropractic Colleges ~ 11-07-2007
Thanks to the Association of Chiropractic Colleges and Gerard Clum, D.C., President of Life Chiropractic College West, for supplying us with these 73 educational slides for your review.
|

|
Putting Risk into Perspective
ACAnews ~ September 2007 ~ FULL TEXT
Over the last three years, doctors of chiropractic in the state of Connecticut have been subject to a rash of anti-chiropractic advertisements conspicuously placed on rolling and static billboards, and in well-read statewide newspapers. Most recently, doctors saw a spate of unprecedented anti-chiropractic legislation aimed to mandate informed consent in chiropractic offices and require open access to chiropractic malpractice records.
|

|
The Etiology of Cervical Artery Dissection
J Chiropractic Medicine 2007 (Summer); 6 (3): 110–120 ~ FULL TEXT
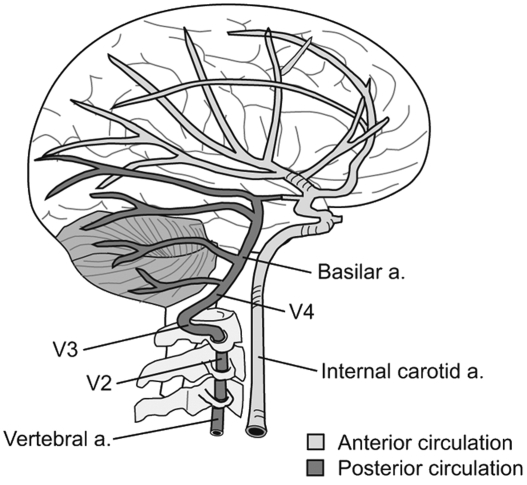
The etiology of cervical artery dissection (CAD) is unclear, although a number of risk factors have been reported to be associated with the condition. On rare occasions, patients experience CAD after cervical spine manipulation, making knowledge about the cervical arteries, the predisposing factors, and the pathogenesis of the condition of interest to chiropractors. This commentary reports on the relevant anatomy of the cervical arteries, developmental features of CAD, epidemiology of the condition, and mechanisms of dissection.
|

|
The Benefits Outweigh the Risks for Patients
Undergoing Chiropractic Care for Neck Pain:
A Prospective, Multicenter, Cohort Study
J Manipulative Physiol Ther 2007 (Jul); 30 (6): 408–418 ~ FULL TEXT
In contrast to clinical trials of prescription medication, researchers in the area of conservative care for musculoskeletal complaints have focused their attention on treatment effectiveness and, to a much lesser degree, on adverse events. This study, consisting of patients treated in a wide variety of chiropractic practices and settings, describes both positive and negative, and short- and long-term clinical outcomes for a relatively large study population with neck pain.
Although many of the subjects (in this study) had chronic, recurrent neck pain and had undergone prior care for this complaint, many patients experienced benefit from the treatment (based upon diminished pain and disability, the percentage of patients recovered and percentage satisfied with care). Furthermore, many responded relatively quickly to treatment (48% were recovered at the fourth visit).
|

|
Inappropriate Use of the Title Chiropractor and Term
Chiropractic Manipulation in the Peer-reviewed
Biomedical Literature
Chiropractic & Osteopathy 2006 (Aug 22); 14 (1): 16 ~ FULL TEXT
The results of this year-long prospective review suggests that the words chiropractor and chiropractic manipulation are often used inappropriately by European biomedical researchers when reporting apparent associations between cervical spine manipulation and symptoms suggestive of traumatic injury. Furthermore, in those cases reported here, the spurious use of terminology seems to have passed through the peer-review process without correction. Additionally, these findings provide further preliminary evidence, beyond that already provided by Terrett, that the inappropriate use of the title chiropractor and term chiropractic manipulation may be a significant source of over-reporting of the link between the care provided by chiropractors and injury.
You may also want to read this Editorial Comment by the author.
|

|
Are German Orthopedic Surgeons
Killing People With Chiropractic?
Journal of Neurology 2006 (Jun); 253 (6): 724–730 ~ FULL TEXT
Editorial Commentary:
I present for your review an abstract from the Journal of Neurology. This abstract blatantly conceals the facts stated in the body of the paper when it claims that “we describe 36 patients with vertebral artery dissections and prior chiropractic neck manipulation”. When I read that sentence, I am led to believe that “real-live chiropractors” (meaning licensed Doctors of Chiropractic, who received their training at a CCE/WCCE accredited schools) were the ones to provide the “chiropractic neck manipulation”. Unfortunately, that couldn't be further from the truth!
|

|
Cerebrovascular Accident Without Chiropractic Manipulation:
A Case Report
J Manipulative Physiol Ther 2006 (May); 29 (4): 330–335 ~ FULL TEXT
A 49-year-old man with non-traumatic chronic episodic head and neck pain presented for care. Examination and plain film radiographs were unremarkable, suggesting a mechanical origin for the symptoms; however, information in the case history raised concerns. The patient was examined and not manipulated by the doctor of chiropractic but referred back to his general practitioner for a second opinion. The following week, the patient was admitted to hospital having had a cerebrovascular accident. The possible indication of the prodrome to a stroke may lie in the case history rather than the examination findings and provocative testing.
|

|
Is It Time To Stop Functional Pre-manipulation Testing
of the Cervical Spine?
Manual Therapy 2005 (May); 10 (2): 154–158 ~ FULL TEXT
The combined extended and rotated cervical spine position has been postulated to affect vertebral artery blood flow by primarily causing a narrowing of the vessel lumen, usually within the artery contralateral to the side of head rotation. The production of brainstem symptoms during the manoeuvre has generally been considered to be a positive test result. As a consequence, functional pre-manipulation testing of the cervical spine has been part of clinical screening undertaken by chiropractors and other manual practitioners to rule out the risk of possible injury to the vertebral artery.
|

|
Current Concepts: Spinal Manipulation and
Cervical Arterial Incidents (2005)
NCMIC ~ Executive Summary (8 pages) ~ FULL TEXT
There is a growing concern and awareness of an association between chiropractic manipulation and cerebrovascular accidents (CVAs). Unfortunately, opinion rather than fact has tended to dominate discussions regarding CVAs and chiropractic, even though there has been no definitive evidence that chiropractic adjustments (actually) cause strokes. The good news is that this monograph notes that a causative relationship between chiropractic manipulation and stroke is unlikely. There is an associative relationship between the two because people may go to chiropractors for relief of stroke-related symptoms.
|

|
Identification of Internal Carotid Artery Dissection
in Chiropractic Practice
J Can Chiropr Assoc. 2004 (Sep); 48 (3): 206–210 ~ FULL TEXT
The problem any chiropractic physician faces in identifying ICAD patients is that the condition may present without any symptoms or the symptoms may appear benign (e.g., headache, neck pain or cervicogenic dizziness). Consequently, it may be impossible to identify some ICAD patients, especially in the early stages of the pathology. As the ICAD progresses and neural blood flow is compromised, the symptom picture typically manifests more completely. The chiropractic physician must be alert to characteristic findings of a progressing ICAD, since an immediate referral to a medical specialist may be required.
|

|
How Common Are Side Effects of Spinal Manipulation
And Can These Side Effects Be Predicted?
Manual Therapy 2004 (Aug); 9 (3): 151–156
Little scientific support is available concerning usual and unusual reactions after spinal manipulation although such reactions are very common in clinical practice. Fifty-nine manipulative therapists were requested to enroll 15 consecutive patients attending for their first visit to receive spinal manipulation. These patients were asked to complete a questionnaire after this first visit that asked for possible risk factors for spinal manipulation and asked about any side effects after the manipulation. The participating practitioners were asked to note medical diagnosis, manipulated spinal region, number of treated areas and type of additional treatment. Four hundred and sixty five valuable responses were analysed. Two hundred and eighty three patients (60.9%) reported at least one post-manipulative reaction. The most common were headache (19.8%), stiffness (19.5%), local discomfort (15.2%), radiating discomfort (12.1%) and fatigue (12.1%).
|

|
The Stroke Issue: Paucity of Valid Data,
Plethora of Unsubstantiated Conjecture
J Manipulative Physiol Ther 2004 (June); 27 (5): 368–372 ~ FULL TEXT
Chiropractic can be proud of its exemplary standards in the areas of informed consent and the allocation of funding for research to study issues of safety. As a responsible, ethical, and caring profession, chiropractic must continue to look into the issue regarding the potential risk of chiropractic adjustment. At this time, it cannot be scientifically stated that there is no risk of VBA dissection from chiropractic cervical adjustment. It can, and in my opinion must, be scientifically stated that there is neither valid evidence of a causal relationship between chiropractic cervical adjustment and VBA dissection nor any valid data to estimate a risk of VBA dissection associated with chiropractic cervical adjustment. It can also be stated that the data that are available regarding the total number of adjustments performed each year, the total number of VBA dissections and occlusions that occur in the absence of chiropractic adjustment each year, and the data that indicate a chiropractic cervical adjustment represents less force to the vertebral artery than movement within the normal range of motion make it more logical to assume a temporal rather than causal link between these 2 events.
|

|
Homocysteine Levels and CVAs: Cause?
Indicator of Risk?
Foundation for Chiropractic Education and Research News Release ~ FULL TEXT
March 10, 2004
 Norwalk, Iowa — The Foundation for Chiropractic Education and Research’s (FCER) Director of Research, Anthony L. Rosner, Ph.D., has authored a commentary on the possible relationship between elevated homocysteine levels and increased risk of spontaneous cervical artery dissections (sCAD).
Norwalk, Iowa — The Foundation for Chiropractic Education and Research’s (FCER) Director of Research, Anthony L. Rosner, Ph.D., has authored a commentary on the possible relationship between elevated homocysteine levels and increased risk of spontaneous cervical artery dissections (sCAD).
|

|
Spontaneous Cervical Artery Dissections and
Implications for Homocysteine
J Manipulative Physiol Ther 2004 (Feb); 27 (2): 124–132 ~ FULL TEXT
As shown in Table 1, the annual incidence of spontaneous VADs in hospital settings has been estimated to occur at the rate of 1 to 1.5 per 100,000 patients. [15] The corresponding VAD incidence rate in community settings has been reported to be twice as high. [16, 17] Using an estimated value of 10 from the literature to represent an average number of manipulations per patient per episode, [23] it becomes apparent that the proposed exposure rate for CVAs attributed to spinal manipulation is equivalent to the spontaneous rates for cervical arterial dissections as reported. [15–17] If the threat of stroke or stroke-like symptoms is to be properly assessed, therefore, at least half our attention needs to be directed toward the spontaneous events instead of primarily or solely on spinal manipulation.
|

|
Motor Vehicle Accidents: The Most Common Cause
of Traumatic Vertebrobasilar Ischemia
Can J Neurol Sci 2003 (Nov); 30 (4): 320–325
There were 80 patients whose vertebrobasilar ischemia was attributed to neck trauma. Five were diagnosed as due to chiropractic manipulation, but the commonest attributed cause was motor vehicle accidents (MVAs), which accounted for 70 cases; one was a sports injury, and five were industrial accidents. In some cases neck pain from an MVA led to chiropractic manipulation, so the cause may have been compounded. In most vehicular cases the diagnosis had been missed, even denied, by the neurologists and neurosurgeons initially involved. The longest delay between the injury and the onset of delayed symptoms was five years.
|

|
Vertebrobasilar Ischemia and Spinal Manipulation
J Manipulative Physiol Ther 2003 (Sep); 26 (7): 443–447 ~ FULL TEXT
This pratitioner examine(d) cerebral arterial blood flow in 2 patients exhibiting signs of vertebrobasilar arterial ischemia (VBI) before and after spinal manipulative therapy. Improvements in arterial flow following spinal adjusting led the author to surmise: “Spinal manipulation may have a normalizing effect on the sympathetic nervous system, allowing for a change in vasospastic cerebral vascular arteries”.
|

|
Cerebrovascular Accidents:
The Rest of The Story
 Anthony L. Rosner, PhD., Research Director for FCER ~ June 20, 2003 ~ FULL TEXT
Anthony L. Rosner, PhD., Research Director for FCER ~ June 20, 2003 ~ FULL TEXT
During the past decade, the issues of cerebrovascular accidents [CVAs] and spinal manipulation have become linked in a debate of ever-increasing intensity. A copious number of studies have investigated spinal manipulation as a putative causative factor of CVAs; however, a common theme among these is the failure to adequately explore the possibility that the majority of CVAs may be spontaneous, cumulative, or caused by factors other than spinal manipulation itself. The problem is only exacerbated by the sometimes hysterical reactions apparent in the mass media over the past three years in reaction to the flawed investigations. This paper was presented Friday June 20, 2003 at the International Spinal Trauma Conference in Chicago, IL. Thanks to Dr. Rosner and the FCER for permission to reproduce this FULL TEXT article exclusively at Chiro.Org!
You may also enjoy his recent articles: Stroke Revisisted: The “Chinatown” Syndrome
and his article Informed Consent: If You Come to a Fork in the Road, Take It.
|

|
Response to Vertebral Artery Dissection Study:
Synopsis Paper by Smith et al.
Published in May 13, 2003 Issue of Neurology
 ~ May 18, 2003 ~ May 18, 2003
The recent publication by Smith et al. in Neurology addressing vertebral artery dissection represents another episode of regrettable studies which, despite serious flaws which raise substantial questions as to their internal validity, go at great lengths to selectively disparage the advisability of performing cervical manipulations as a means of patient care while obscuring the larger picture.
|

|
Association of Internal Carotid Artery Dissection
and Chiropractic Manipulation
Neurologist 2003 (Jan); 9 (1): 35–44
In reviewing the cases of internal carotid dissection potentially related to CMT, there were many confounding factors, such as connective tissue aberrations, underlying arteriopathy, or coexistent infection, that obscured any obvious cause-and-effect relationship. To date there are only 13 reported cases of ICAD temporally related to CMT. Most ICADs seem to occur spontaneously and progress from local symptoms of headache and neck pain to cortical ischemic signs. Approximately one third of the reported cases were manipulated by practitioners other than chiropractic physicians, and because of the differential risk related to major differences in training and practice between practitioners who manipulate the spine, it would be inappropriate to compare adverse outcomes between practitioner groups.
|

|
VAD Following Cervical Manipulation: D.C. vs M.D.
Experiences Affect Perception of Risk
 ~ January 13, 2003 ~ January 13, 2003
Examination of the database of the Canadian Chiropractic Protective Association (CCPA, which provides malpractice insurance for 83% of chiropractors in Canada) for the period 1988 to 1997 found 23 cases of VAD. Retrospective review of these cases and a survey of chiropractors suggests an estimated 134,466,765 cervical manipulations were performed during the 10-year period. Records from these reported VAD cases indicates that in a 30 year practice, only one in 48 chiropractors would be aware of a vascular incident following cervical manipulation. In contrast, examination of the records show that these 23 VAD patients saw a total of 216 physicians, including 69 neurologists.
|

|
International Expert Debunks Stroke Consortium
Chief's Claims About Link Between Stroke
and Neck Adjustment
Canada Newswire; Nov 18, 2002
ORONTO, Nov 18, 2002 (Canada NewsWire via COMTEX) -- A leading world expert on scientific methodology and research, Dr. David Sackett, an officer of the Order of Canada and member of the Canadian Medical Hall of Fame, today described Dr. John Norris, former Chair of the Canadian Stroke Consortium, as “incompetent” in scientific research and “irresponsible” with regard to the Consortium's work attributing strokes to neck adjustment.
|

|
Is Cervical Spinal Manipulation Dangerous?
J Manipulative Physiol Ther 2003 (Jan); 26 (1): 48–52 ~ FULL TEXT
It appears that the risk of cerebrovascular accidents after cervical manipulation is low, considering the enormous number of treatments given each year, and very much lower than the risk of serious complications associated with generally accepted surgery. Provided there is a solid indication for cervical manipulation, we believe that the risk involved is acceptably low and that the fear of serious complications is greatly exaggerated.
|

|
The Mechanics of Neck Manipulation With Special
Consideration of the Vertebral Artery
J Can Chiropr Assoc. 2002 (Sep); 46 (3): 134–136 ~ FULL TEXT
Before this paper was published by Herzog and Symons, the chiropractic community accepted the belief that mechanical injury to the vertebral artery was possible, but it was very, very rare occurrence; but nevertheless, accepted. And all this without a shred of scientific evidence about the mechanics of the vertebral artery during cervical manipulation. All that began to change as this group of researchers continued studying the tensile strains that occur to the vertebral artery during normal range of motion and spinal manipulation, as well as testing of the failure limits of those tissues.
|

|
Clinical Perceptions of the Risk of Vertebral Artery
Dissection After Cervical Manipulation:
The Effect of Referral Bias
Spine J 2002 (Sep); 2 (5): 334–342
For the 10-year period 1988 to 1997, there were 23 cases of vertebral artery dissection after cervical manipulation reported to the CCPA that represents 83% of practicing chiropractors in Canada. Based on the survey, an estimated 134,466,765 cervical manipulations were performed during this 10-year period. This gave a calculated rate of vertebral artery dissection after manipulation of 1 in every 5,846,381 cervical manipulations. Based on the number of practicing chiropractors and neurologists during the period of this study, 1 of every 48 chiropractors and one of every two neurologists would have been made aware of a vascular complication from cervical manipulation that was reported to the CCPA during their practice lifetime.
 You may also enjoy an in-depth review of this article by the
FCER.
You may also enjoy an in-depth review of this article by the
FCER.
|

|
Uneventful Upper Cervical Manipulation in the
Presence of a Damaged Vertebral Artery
J Manipulative Physiol Ther 2002 (Sept); 25 (7): 472–483 ~ FULL TEXT
This case report demonstrates that vigorous manipulation of the upper cervical spine is possible without injuring an already damaged vertebral artery. It is suggested that the line of drive used during the single manipulation, almost pure lateral flexion with slight rotation, was responsible for the apparent innocuous response. Guidelines for the evaluation and management of vertebral artery dissection are reviewed. Because it is currently impossible to identify patients at risk of having a dissected vertebral artery with standard in-office examination procedures, rotational manipulation of the upper cervical spine should be abandoned by all practitioners, and schools should remove such techniques from their curriculums.
|

|
Manipulation of the Neck and Stroke:
Time for More Rigorous Evidence
Medical Journal of Australia 2002 (Apr 15); 176 (8): 376–380
In this issue of the Journal, Ernst (page 376) reviews case reports of serious adverse events associated with cervical spine manipulation. Although Ernst acknowledges the considerable doubt about a causal relationship between the manipulation and the adverse event, he is inconsistent in suggesting that the anecdotal and uncontrolled evidence of the case reports favours the adverse events, often strokes, being an effect of manipulation. Elucidating a causal relationship calls for greater clarity, less ambivalence and generally better science in the present evidence-based climate. Thus, the important question to be answered in the light of Ernst's article is whether the association between neck manipulation and stroke is actually causal and, if so, in what direction?
|

|
Unpredictability of Cerebrovascular Ischemia Associated
with Cervical Spine Manipulation Therapy: A Review of
Sixty-four Cases After Cervical Spine Manipulation
Spine 2002 (Jan 1); 27 (1):49–55
This study was unable to identify factors from the clinical history and physical examination of the patient that would assist a physician attempting to isolate the patient at risk of cerebral ischemia after cervical manipulation. Cerebrovascular accidents after manipulation appear to be unpredictable and should be considered an inherent, idiosyncratic, and rare complication of this treatment approach.
|

|
Scientific Evidence Over-Rides the False Claimsn
in Canadian Stroke Case
Joel Alcantara, D.C., Director of Research for the ICPA ~ FULL TEXT
The Lana Lewis inquest in Canada is well known to Canadian chiropractors as it has and will affect the practice of chiropractic in that country and possibly the world. The following is a summary from one of the expert witnesses called by the chiropractic profession, Dr. David Sackett. To some, the name may be familiar, particularly since its synonymous with the words “evidenced-based medicine”.
|

|
New Study Puts Stroke From Neck Adjustment at
Less than 1 in 5 Million Adjustments
 Toronto, October 12, 2001— A new Canadian study, reported in the October 2, 2001 issue of the Canadian Medical Association Journal (CMAJ), puts the risk of stroke following neck adjustment at 1 in every 5.85 million adjustments. The study, which is based on patient medical files and malpractice data from the Canadian Chiropractic Protective Association, evaluated all claims of stroke following chiropractic care for a ten year period between 1988 and 1997.
Toronto, October 12, 2001— A new Canadian study, reported in the October 2, 2001 issue of the Canadian Medical Association Journal (CMAJ), puts the risk of stroke following neck adjustment at 1 in every 5.85 million adjustments. The study, which is based on patient medical files and malpractice data from the Canadian Chiropractic Protective Association, evaluated all claims of stroke following chiropractic care for a ten year period between 1988 and 1997.
|

|
Chiropractic Manipulation and Stroke
Stroke 2001 (Sep); 32 (9): 2207—2208
 This is the response to this
Rothwell et al. article by Anthony Rosner, PhD of the FCER.
This is the response to this
Rothwell et al. article by Anthony Rosner, PhD of the FCER.
|

|
A Case Study of Misrepresentation of the
Scientific Literature: Recent Reviews
of Chiropractic
J Altern Complement Med 2001 (Feb); 7 (1): 65-78 ~ FULL TEXT
Accurate use of published data and references is a cornerstone of the peer-review process. Statements, inferences, and conclusions based upon these references should logically ensue from the data they contain. When journal articles and textbook chapters summarizing the safety and efficacy of particular therapies or interventions use references inaccurately or with apparent intent to mislead, the integrity of scientific reporting is fundamentally compromised. Ernst et al.'s publication on chiropractic include repeated misuse of references, misleading statements, highly selective use of certain published papers, failure to refer to relevant literature, inaccurate reporting of the contents of published work, and errors in citation. Meticulous analysis of some influential negative reviews has been carried out to determine the objectivity of the data reported. The misrepresentation that became evident deserves full debate and raises serious questions about the integrity of the peer-review process and the nature of academic misconduct.
|

|
Consequences of Neck Manipulation Performed by a Non-professional
Spinal Cord 2001 (Feb); 39 (2): 112–113
A 30-year-old man who fainted after neck manipulation by a barber and developed spinal cord and brainstem dysfunction. His MRI revealed an extramedullary, intradural dumbbell shaped mass on the right side at C1 and C2 level compressing the spinal cord.
|

|
Vertebral Artery Dissection: Warning Symptoms,
Clinical Features and Prognosis in 26 Patients
Can J Neurol Sci 2000 (Nov); 27 (4): 292–296 ~ FULL TEXT
Headache and/or neck pain followed by vertigo or unilateral facial paresthesia is an important warning sign that may precede onset of stroke by several days.
 Please review this detailed response by FCER's Anthony L. Rosner, Ph.D.
Please review this detailed response by FCER's Anthony L. Rosner, Ph.D.
|

|
Vertebral Artery Dissection and Migraine Headaches in Children
J Child Neurol 2000 (Oct); 15 (10): 694–696
Risk factors for vertebral artery dissection are reviewed, with emphasis on association with migraine headaches. A review of imaging studies for the diagnosis of dissection is also presented. This case demonstrates the importance of considering arterial wall dissection in pediatric patients with a history of atypical migraines associated with new neurologic findings.
|

|
Vertebral Artery Dissection Causing Stroke in Sport
J Clin Neurosci 2000 (Jul); 7 (4): 298–300
Stroke in sport, although uncommon, is predominantly due to arterial dissection in either the vertebral or carotid arteries. Physicians involved in athlete care need to be aware of this diagnosis.
|

|
Sudden Neck Movement and Cervical Artery Dissection
Canadian Medical Association Journal 2000 (Jul 11); 163: 38–40 ~ FULL TEXT
During the past year the Canadian Stroke Consortium, a national network of stroke physicians, has been prospectively collecting detailed information on cases of dissection of the cervical arteries. Seventy-four patients have been studied so far: their age range was 16-87 years (mean 44 years), 60% were male, and there was a predominance of vertebrobasilar artery dissections compared with carotid artery dissections (72% v. 28%). Most (81%) of the dissections were associated with sudden neck movement, ranging from therapeutic neck manipulation to a vigorous game of volleyball, but some occurred during mild exertion such as lifting a pet dog or during a bout of coughing.
|

|
Is There a Role for Premanipulative Testing
Before Cervical Manipulation?
J Manipulative Physiol Ther 2000 (Mar); 23 (3): 175–179 ~ FULL TEXT
It appears that a positive premanipulative test is not an absolute contraindication to manipulation of the cervical spine. If the test is able to identify patients at risk for cerebrovascular accidents, we suggest patients with a reproducible positive test should be referred for a duplex examination of the vertebral artery flow. If duplex flow is normal, the patient should be eligible for cervical manipulation despite the positive premanipulative test.
|

|
Effect of Premanipulative Tests on Vertebral Artery and
Internal Carotid Artery Blood Flow: A Pilot Study
J Manipulative Physiol Ther 1999 (Jul); 22 (6): 368–375 ~ FULL TEXT
Screening procedures that use rotation and extension may be useful tests of the adequacy of collateral circulation. A larger study is needed to determine whether subjects testing positive significantly differ from those testing negative.
|

|
Risk Factors and Precipitating Neck Movements Causing
Vertebrobasilar Artery Dissection After Cervical
Trauma and Spinal Manipulation
Spine 1999 (Apr 15); 24 (8): 785–794
The literature does not assist in the identification of the offending mechanical trauma, neck movement, or type of manipulation precipitating vertebrobasilar artery dissection or the identification of the patient at risk. Thus, given the current status of the literature, it is impossible to advise patients or physicians about how to avoid vertebrobasilar artery dissection when considering cervical manipulation or about specific sports or exercises that result in neck movement or trauma.
|

|
Perspectives: An Overview of Comparative Considerations
of Cerebrovascular Accidents
Chiropractic Journal of Australia 1999; 29 (3): 87—102 ~ FULL TEXT
This paper seeks to contrast reports concerning major adverse side effects, viz. cerebrovascular accidents (CVAs) attributed to cervical spine manipulation, within a broad perspective of medical procedures. It also seeks to correlate the incidence rates of other adverse events and medical procedures with the general incidence rate of CVAs. On analysis, an accurate position would indicate that cervical spinal manipulation is one of the more conservative, least invasive and safest of procedures in the provision of human health care services. The paper also alludes to the political connotations on the subject.
Thanks to the Chiropractic Journal of Australia for permission to reproduce this FULL TEXT article exclusively at Chiro.Org!
|

|
Risk Assessment of Neurological and/or Vertebrobasilar
Complications in the Pediatric Chiropractic Patient
J Vertebral Subluxation Research (JVSR) 1998; 2 (2): 73–78
The estimate of risk due to the pediatric chiropractic patient in this category of complication was estimated to be 4.0 x 10 -7 % of all visits. Stated otherwise, there would be a chance of approximately 1 in 250 million pediatric visits that a N/VB complication would result. While some pre-existing conditions may predispose a pediatric patient to a higher incidence of such complications, the estimates derived in the present study are considered applicable to the general pediatric population.
|

|
Efficacy and Risks of Chiropractic Manipulation:
What Does the Evidence Suggest?
Integrative Medicine 1998; 1: 61–66
This review article drew upon the appropriateness studies conducted at RAND, which indicated efficacy of manipulation for acute or sub-acute low back pain, neck pain, and muscle-tension-type headaches. The article also reported the low risk of serious complications from lumbar and cervical manipulations. According to the literature review, the estimated risk for serious complications from cervical manipulation is 6.39 per 10 million manipulations. For lumbar manipulation, it is 1 per 100 million manipulations. These estimates compare favorably to other forms of therapy, such as cervical spine surgery or nonsteroidal anti-inflammatory drugs (NSAIDS). The risk from manipulation is low and compares favorably to other forms of therapy for the same conditions (e.g., 15.6 complications per 1000 cervical spine surgeries, 3.2 per 1000 subjects for nonsteroidal anti-inflammatory drugs)
|

|
Tissue Plasminogen Activator in a Vertebral Artery Dissection
Can J. Neurol Sci 1997 (May); 24 (2): 151–154
We report a 49-year-old woman who presented with the rapidly progressing basilar artery syndrome who was given an intravenous dose of tissue plasminogen activator seven hours after the onset of first symptoms. Thirty minutes after the injection, a dramatic recovery of the patient's consciousness and neurological signs was noted.
|

|
Safety in Chiropractic Practice Part II: Treatment to the
Upper Neck and the Rate of Cerebrovascular Incidents
J Manipulative Physiol Ther 1996 (Nov); 19 (9): 563–569
Retrospective data were collected from questionnaires covering the period 1978-1988 inclusive; in a second survey, chiropractors provided information obtained through inspection of their own case records.
|

|
Manipulation and Mobilization of the Cervical Spine.
A Systematic Review of the Literature
Spine 1996 (Aug 1); 21 (15): 1746–1760
The combination of three of the randomized controlled trials comparing spinal manipulation with other therapies for patients with subacute or chronic neck pain showed an improvement on a 100-mm visual analogue scale of pain at 3 weeks of 12.6 mm (93% confidence interval, -0.15, 25.5) for manipulation compared with muscle relaxants or usual medical care. The highest quality randomized controlled trial demonstrated that spinal manipulation provided short-term relief for patients with tension-type headache. The complication rate for cervical spine manipulation is estimated to be between 5 and 10 per 10 million manipulations.
|

|
Safety in Chiropractic Practice, Part I: The Occurrence
of Cerebrovascular Accidents After Manipulation
to the Neck in Denmark from 1978–1988
J Manipulative Physiol Ther 1996 (Jul); 19 (6): 371–377
Although the incidence of CVA after chiropractic SMT was confirmed to be low, there seems to be sufficient evidence to justify a firm policy statement cautioning against upper cervical rotation as a technique of first choice.
|

|
The Validity of the Extension-rotation Test as a
Clinical Screening Procedure Before Neck Manipulation:
A Secondary Analysis
J Manipulative Physiol Ther 1996 (Mar); 19 (3): 159–164
We were unable to demonstrate that the extension-rotation test is a valid clinical screening procedure to detect decreased blood flow in the vertebral artery. The value of this test for screening patients at risk of stroke after cervical manipulation is questionable.
|

|
A Risk Assessment of Cervical Manipulation vs.
NSAIDs for the Treatment of Neck Pain
J Manipulative Physiol Ther 1995 (Oct); 18 (8): 530–536
As for comparative safety, the best available evidence indicates that NSAID use poses a significantly greater risk of serious complications and death than the use of cervical manipulation for comparable conditions. In conclusion,
the best evidence indicates that cervical manipulation for neck pain is much safer than the use of NSAIDs, by as much as a factor of several hundred times. There is no evidence that indicates NSAID use is any more effective than cervical manipulation for neck pain.
|

|
Misuse of the Literature by Medical Authors
in Discussing Spinal Manipulative Therapy Injury
J Manipulative Physiol Ther 1995 (May); 18 (4): 203–210 ~ FULL TEXT
The words chiropractic and chiropractor have been incorrectly used in numerous publications dealing with SMT injury by medical authors, respected medical journals and medical organizations. In many cases, this is not accidental; the authors had access to original reports that identified the practitioner involved as a non–chiropractor. The true incidence of such reporting cannot be determined. Such reporting adversely affects the reader's opinion of chiropractic and chiropractors.
|

|
Letter to the Editor, The New York Times, Regarding
the Jane Brody article of April 3, 2001
 Anthony L. Rosner, Ph.D. ~ FULL TEXT
Anthony L. Rosner, Ph.D. ~ FULL TEXT
Jane Brody's recent article [“When Simple Actions Ravage Arteries”, 04/03/01] is an unfortunate and careless portrayal of a healthcare intervention which was specifically designed to avoid the more serious and often irreversible sequelae of the more invasive tools of orthodox medicine: drugs and surgery. Emphasizing the body's own capacity to heal, chiropractic management of patients is based upon the diagnosis, treatment and prevention of disorders of the musculoskeletal system and how they are reflected upon general health through the nervous system.
|

|
A Review of the Significant Shortcomings in the Reporting
of Stroke Associated with Cervical Manipulation
Clinical Practice Guidelines, Chapter 9: Patient Safety
In the case of strokes purportedly associated with manipulation, the panel noted significant shortcomings in the literature. A summary of the relevant literature follows. For example: “In a letter to the editor of the Journal of Manipulative and Physiological Therapeutics, Myler(9) wrote, I was curious how the risk of fatal stroke after cervical manipulation, placed at 0.00023%(10) compared with the risk of (fatal) stroke in the general population of the United States. According to data obtained from the National Center for Health Statistics, the mortality rate from stroke in the general population was calculated to be 0.00057%. If these data are correct, the risk of a fatal stroke following cervical manipulation is less than half the risk of fatal stroke in the general population.”
|

|
The Benefits and Risks of Spinal Manipulation
Chiropractic in the United States: Training, Practice and Research
Agency for Health Care Policy and Research
Chapter 11 of AHCPR Publication No. 98–N002
This chapter summarizes what has been learned from clinical trials about the benefits of spinal manipulation for specific problems and from case reports about the risks of spinal manipulation. In addition, findings of studies examining the ability of spinal manipulation to increase patient satisfaction, decrease cost, or increase cost-effectiveness of care are summarized.
|

|
What are the Risk of Chiropractic Neck Treatments?
William J. Lauretti, DC ~ FULL TEXT
J Manipulative and Physiological Therapeutics (October, 1995)
Every published study which has estimated the incidence of stroke (CVA) from cervical manipulation has agreed that the risk is 1 to 3 incidents per million treatments. Dvorak, [1] in a survey of 203 practitioners of manual medicine in Switzerland, found a rate of one serious complication per 400,000 cervical manipulations, without any reported deaths, among an estimated 1.5 million cervical manipulations. Jaskoviak [2] reported approximately 5 million cervical manipulations from 1965 to 1980 at The National College of Chiropractic Clinic in Chicago, without a single case of vertebral artery stroke or serious injury.
|

|
Response to Vertebral Artery Dissection Study:
Canadian Journal of Neurological Sciences
 FCER & Anthony L. Rosner, Ph.D. (December 22, 2000) ~ FULL TEXT
FCER & Anthony L. Rosner, Ph.D. (December 22, 2000) ~ FULL TEXT
A recent publication addressing vertebral artery dissection in The Canadian Journal of Neurological Sciences [1] is surprisingly anecdotal and sketchy in its depiction of both the possible causes and etiology of the subject it is intended to discuss. As such, it is laden with severe methodological deficiencies which severely undercut its credibility and create misleading impressions of vertebral artery dissection and raise more fundamental questions as to how retrospective studies should be conducted. There are at least five critical issues which need to be brought into consideration in order to more fully understand this particular study in a broader perspective.
|

|
Acupuncture and Stroke Recovery
Johansson et al (1993) investigated the effectiveness of acupuncture as a supplement to physical therapy in recovery from stroke. Pang (1994) investigated two particular scalp acupuncture techniques in order to compare their effectiveness in treating apoplexy following stroke.
|

|
A Review of the Reported Complications
from Spinal Manipulation
John J. Triano, D.C., Ph.D.
In general, chiropractic treatment has little associated risk. Table TX5 displays the complications of spinal manipulation that have been reported [Haldeman, Haldeman, LeBoeuf-Yve]. Nearly all reactions to manipulation are mild and self-limiting, lasting less than 24 hours. Rarely, significant injury can result from injudicious or inappropriate use. The incidence of serious complication is less than 1:1,000,000.
|

|
Claims of Risk From Chiropractic Care For Neck Pain Are
Exaggerated Say Experts At The Texas Back Institute
Plano, TX – May 10, 2000 -- Periodic claims posed in the public and professional media that Chiropractic treatment to the neck poses a high risk for stroke are unwarranted say the experts at the Texas Back Institute.
|

|
Stroke Prevention Guidelines Issued
“Stroke is... killing about 160,000 Americans each year,” Dr. Ralph Sacco of the departments of neurology and public health at Columbia University in New York told reporters at a telephone
press conference on Thursday. “About 700,000 people will have a new or recurrent stroke each year,” he added, “and stroke incidence seems to be on the rise”. To reduce risk of stroke,
the NSA offers these basic recommendations.
|

|
Kinematics of the Head and Associated Vertebral Artery
Length Changes During High-velocity, Low-amplitude
Cervical Spine Manipulation
Chiropractic & Manual Therapies 2022 (Jun 1); 30 (1): 28 ~ FULL TEXT
Mean head angular displacements and VA length changes were small during CSM thrusts. Of the four different CSM measured, mean VA length changes were largest during rotation procedures. This suggests that if clinicians wish to limit VA length changes during the thrust phase of CSM, consideration should be given to the type of CSM used.
|

|
Effect of Cervical Manipulation on Vertebral Artery
and Cerebral Haemodynamics in Patients with
Chronic Neck Pain: A Crossover Randomised
Controlled Trial
BMJ Open 2019 (May 28); 9 (5) :e025219 ~ FULL TEXT
Our results are in accordance with previous work, which has shown a decrease in blood flow and velocity in the contralateral vertebral artery with head rotation. This may explain why we also observed a decrease in blood velocity with manipulation because it involves neck rotation. Our work is the first to show that cervical manipulation does not result in brain perfusion changes compared with a neutral neck position or maximal neck rotation. The changes observed were found to not be clinically meaningful and suggests that cervical manipulation may not increase the risk of cerebrovascular events through a haemodynamic mechanism.
|

|
Systematic Review and Meta-analysis of Chiropractic Care
and Cervical Artery Dissection:
No Evidence for Causation
Cureus. 2016 (Feb 16); 8 (2): e498 ~ FULL TEXT
The quality of the published literature on the relationship between chiropractic manipulation and CAD is very low. Our analysis shows a small association between chiropractic neck manipulation and cervical artery dissection. This relationship may be explained by the high risk of bias and confounding in the available studies, and in particular by the known association of neck pain with CAD and with chiropractic manipulation. There is no convincing evidence to support a causal link between chiropractic manipulation and CAD. Belief in a causal link may have significant negative consequences such as numerous episodes of litigation.
|

|
Internal Carotid Artery Strains During High-Speed,
Low-Amplitude Spinal Manipulations of the Neck
J Manipulative Physiol Ther. 2015 (Nov); 38 (9): 664–671 ~ FULL TEXT
This study showed that maximal Internal Carotid Artery (ICA) strains imparted by cervical spinal manipulative treatments were well within the normal ROM. Chiropractic manipulation of the neck did not cause strains to the ICA in excess of those experienced during normal everyday movements. Therefore, cervical spinal manipulative therapy as performed by the trained clinicians in this study, did not appear to place undue strain on the ICA and thus does not seem to be a factor in ICA injuries.
|

|
Chiropractic Care and the Risk of Vertebrobasilar Stroke:
Results of a Case-control Study in U.S. Commercial
and Medicare Advantage Populations
Chiropractic & Manual Therapies 2015 (Jun 16); 23: 19 ~ FULL TEXT
We found no significant association between exposure to chiropractic care and the risk of VBA stroke. We conclude that manipulation is an unlikely cause of VBA stroke. The positive association between PCP visits and VBA stroke is most likely due to patient decisions to seek care for the symptoms (headache and neck pain) of arterial dissection. We further conclude that using chiropractic visits as a measure of exposure to manipulation may result in unreliable estimates of the strength of association with the occurrence of VBA stroke.
|

|
Quantifying Strain in the Vertebral Artery With
Simultaneous Motion Analysis of the Head and Neck:
A Preliminary Investigation
Clin Biomech (Bristol, Avon) 2014 (Dec); 29 (10): 1099–1107 ~ FULL TEXT
The results of this study suggest that the strains on the VA during global head and neck movements, including SM, do not exceed published failure strains. Furthermore, this study supports previous evidence that the greatest amount of strain in the VA occurs during rotation (Herzog et al., 2012). This study provides new evidence that peak strain in the VA may not actually occur at the end range of motion, but rather at some point when the end range has not been reached yet. This finding leads to the conclusion that sVAD, due to global head and neck movements, is not predictable unless achieving large amounts of strain causing global failure, which was never observed in the current study.
|

|
Cervical Arterial Dissections and Association With Cervical
Manipulative Therapy A Statement for Healthcare
Professionals from the American Heart Association
and the American Stroke Association
Stroke. 2014 (Oct); 45 (10): 3155–3174 ~ FULL TEXT
Cervical artery dissections (CDs) is an important cause of ischemic stroke in young and middle-aged patients. CD is most prevalent in the upper cervical spine and can involve the internal carotid artery or vertebral artery. Although current biomechanical evidence is insufficient to establish the claim that CMT causes CD, clinical reports suggest that mechanical forces play a role in a considerable number of CDs and most population controlled studies have found an association between CMT and VAD stroke in young patients. Although the incidence of CMT-associated CD in patients who have previously received CMT is not well established, and probably low, practitioners should strongly consider the possibility of CD as a presenting symptom, and patients should be informed of the statistical association between CD and CMT prior to undergoing manipulation of the cervical spine.
|

|
Changes in Vertebral Artery Blood Flow Following Various
Head Positions and Cervical Spine Manipulation
J Manipulative Physiol Ther. 2014 (Jan); 37 (1): 22–31 ~ FULL TEXT
This paper examined the quality of literature describing an association between cSMT and CAD. Case reports represented the majority of this literature. Since these In a neutral head position, physiologic measures of VA blood flow and velocity at the C1–2 spinal level were obtained using phase-contrast magnetic resonance imaging after 3 different head positions and a chiropractic upper cervical spinal manipulation. A total of 30 flow-encoded phase-contrast images were collected over the cardiac cycle, in each of the 4 conditions, and were used to provide a blood flow profile for one complete cardiac cycle. Differences between flow (in milliliters per second) and velocity (in centimeters per second) variables were evaluated using repeated-measures analysis of variance.
RESULTS: The side-to-side difference between ipsilateral and contralateral VA velocities was not significant for either velocities (P = .14) or flows (P = .19) throughout the conditions. There were no other interactions or trends toward a difference for any of the other blood flow or velocity variables.
CONCLUSIONS: There were no significant changes in blood flow or velocity in the vertebral arteries of healthy young male adults after various head positions and cervical spine manipulations.
|

|
Chiropractic and Stroke: Association or Causation?
Int J Clin Pract. 2013 (Sep); 67 (9): 825–833 ~ FULL TEXT
Serious complications following spinal manipulative therapy (SMT) of the cervical spine, including stroke, are relatively rare. Estimates vary between 1:400,000 cervical spine manipulations and 1:5.6 million. [1, 2] However, there is controversy on how frequent events such as stroke are, and whether there is a causal relationship with SMT. Even more controversy can be found specifically relating to chiropractic SMT and whether this has a higher risk than other types of SMT. Both sides of the debate appear to have extremists with a biased perspective. Previous articles have not provided a comprehensive review of the evidence for and against chiropractic. A recent article noted several weaknesses or inconsistencies in some articles discussing chiropractic treatment and stroke. [3] A critical review of a paper previously published in the International Journal of Clinical Practice has been conducted to provide evidence for the alternative theories regarding the safety of chiropractic SMT and whether there is a causal relationship with the stroke. [4] A critical review of the current literature will also help to assess any misconceptions or distortion of the results of studies on chiropractic and stroke.
|

|
The Quality of Reports on Cervical Arterial
Dissection Following Cervical Spinal Manipulation
PLoS ONE 2013 (Mar 20); 8 (3): e59170 ~ FULL TEXT
This paper examined the quality of literature describing an association between cSMT and CAD. Case reports represented the majority of this literature. Since these reports may contribute to further understanding CADs as they relate to manual therapy, it is important that they are of the highest quality. This study has demonstrated that the literature infrequently reports useful data toward understanding the association between cSMT, CADs and stroke. As a result, the value of these reports toward informing our understanding of the relation between cSMT and CAD is minimal. We suggest that through the systematic collection of data features presented in this paper, a clearer clinical picture of the association between cSMT and CAD would be possible. This study lays the groundwork for developing a universal reporting tool for adverse events related to cSMT.
|

|
Vertebral Artery Strains During High-speed,
Low Amplitude Cervical Spinal Manipulation
J Electromyogr Kinesiol. 2012 (Oct); 22 (5): 740–746 ~ FULL TEXT
Spinal manipulative therapy (SMT) has been recognized as an effective treatment modality for many back, neck and musculoskeletal problems. One of the major issues of the use of SMT is its safety, especially with regards to neck manipulation and the risk of stroke. The vast majority of these accidents involve the vertebro-basilar system, specifically the vertebral artery (VA) between C2/C1. However, the mechanics of this region of the VA during SMT are unexplored. Here, we present first ever data on the mechanics of this region during cervical SMT performed by clinicians. VA strains obtained during SMT are significantly smaller than those obtained during diagnostic and range of motion testing, and are much smaller than failure strains. We conclude from this work that cervical SMT performed by trained clinicians does not appear to place undue strain on VA, and thus does not seem to be a factor in vertebro-basilar injuries.
|

|
Current Understanding of the Relationship Between
Cervical Manipulation and Stroke: What Does
It Mean for the Chiropractic Profession?
Chiropractic & Osteopathy 2010 (Aug 3); 18 (1): 1–9 ~ FULL TEXT
The understanding of the relationship between cervical manipulative therapy (CMT) and vertebral artery dissection and stroke (VADS) has evolved considerably over the years. In the beginning the relationship was seen as simple cause-effect, in which CMT was seen to cause VADS in certain susceptible individuals. This was perceived as extremely rare by chiropractic physicians, but as far more common by neurologists and others. Recent evidence has clarified the relationship considerably, and suggests that the relationship is not causal, but that patients with VADS often have initial symptoms which cause them to seek care from a chiropractic physician and have a stroke some time after, independent of the chiropractic visit. This new understanding has shifted the focus for the chiropractic physician from one of attempting to “screen” for “risk of complication to manipulation” to one of recognizing the patient who may be having VADS so that early diagnosis and intervention can be pursued. In addition, this new understanding presents the chiropractic profession with an opportunity to change the conversation about CMT and VADS by taking a proactive, public health approach to this uncommon but potentially devastating disorder.
|

|
Preliminary Report: Biomechanics of Vertebral Artery
Segments C1–C6 During Cervical Spinal Manipulation
J Manipulative Physiol Ther. 2010 (May); 33 (4): 273–278 ~ FULL TEXT
The results of this study suggest complex and nonintuitive strain patterns of the VA within the cervical transverse foramina. Consistent (for 2 chiropractors) and repeatable (for 3 repeat measurements for each chiropractor) elongation and shortening of adjacent VA segments were observed simultaneously and could not be explained with a simple model of neck movement. We hypothesized that they were caused by variations in the location and stiffness of the VA fascial attachments to the vertebral foramina and by coupled movements of the cervical vertebrae. However, in agreement with previous work on VA strains proximal and distal to the cervical transverse foramina, strains for cervical spinal manipulations were consistently lower than those obtained for cervical rotation.
|

|
Microstructural Damage in Arterial Tissue
Exposed to Repeated Tensile Strains
J Manipulative Physiol Ther 2010 (Jan); 33 (1): 14–19 ~ FULL TEXT
Twenty-four test specimens from cadaveric rabbit ascending aorta were divided into 2 control groups (n = 12) and 2 experimental groups (n = 6 each). Specimens were exposed to 1000 strain cycles of 0.06 and 0.30 of their in situ length. A pathologist, blinded to the experimental groups, assessed microstructural changes in the arteries using quantitative histology. Pearson χ2 analysis (a = .05) was used to assess differences in tissue microstructure between groups. Cadaveric arterial tissues of New Zealand white rabbit with similar size, structure, and mechanical properties of human vertebral artery did not exhibit histologically identifiable microdamage when exposed to repeated mechanical loading equivalent to the strains observed in human vertebral artery during chiropractic cervical spine manipulative therapy.
|

|
Risk of Vertebrobasilar Stroke and Chiropractic Care:
Results of a Population-based Case-control
and Case-crossover Study
Spine 2008 (Feb 15); 33 (4 Suppl): S176–183 ~ FULL TEXT
VBA stroke is a very rare event in the population. There was an association between chiropractic services and subsequent vertebrobasilar artery stroke in persons under 45 years of age, but a similar association was also observed among patients receiving general practitioner services. This is likely explained by patients with vertebrobasilar artery dissection-related neck pain or headache seeking care before having their stroke.
|

|
An Analysis of the Etiology of Cervical
Artery Dissections: 1994 to 2003
J Manipulative Physiol Ther 2005 (Oct); 28 (8): 617–622 ~ FULL TEXT
The case series that were reviewed in this article indicated that most CADs reported in the previous decade were spontaneous but that some were associated with trauma/trivial trauma, and a minority with cervical spine manipulation. This etiologic breakdown of CAD does not differ significantly from what has been portrayed by most other authors.
|

|
Cervical Artery Dissection A Comparison of
Highly Dynamic Mechanisms: Manipulation
Versus Motor Vehicle Collision
J Manipulative Physiol Ther 2005 (Jan); 28 (1): 57–63 ~ FULL TEXT
This recent review of the literature finds: “Additionally, long-lasting abnormalities of blood flow velocity within the vertebral artery have been reported in patients following common whiplash injuries, whereas no significant changes in vertebral artery peak flow velocity were observed following cervical chiropractic manipulative therapy”. and concludes that: “The direct evidence suggests that the healthy vertebral artery is not at risk from properly performed chiropractic manipulative procedures”.
|

|
Defining the Effect of Cervical Manipulation on
Vertebral Artery Integrity:
Establishment of an Animal Model
J Manipulative Physiol Ther 2004 (Nov); 27 (9): 539–546 ~ FULL TEXT
Over the past 5 to 10 years, the issue of cerebrovascular accidents (CVAs) and spinal manipulation has become a debate of ever-increasing intensity. A copious number of studies have investigated spinal manipulation as a putatative causative factor of CVAs [1–5]; however, a common theme among these is the failure to consider that the majority of vertebrobasilar accidents (VBAs) may be spontaneous, cumulative, or caused by factors other than spinal manipulation. The problem is not served by the sometimes hysterical reactions apparent in the media over the past 2 years in reaction to the flawed investigations. [6–11] In light of these recent reports, the entire phenomenon of spontaneous cervical artery dissections should be revisited to put this matter into a better perspective.
|

|
Internal Forces Sustained by the Vertebral Artery
During Spinal Manipulative Therapy
J Manipulative Physiol Ther 2002 (Oct); 25 (8): 504–510 ~ FULL TEXT
SMT resulted in strains to the VA that were almost an order of magnitude lower than the strains required to mechanically disrupt it. We conclude that under normal circumstances, a single typical (high-velocity/low-amplitude) SMT thrust is very unlikely to mechanically disrupt the VA.
|

|
Vertebral Arteries and Cervical Rotation:
Modeling and Magnetic Resonance Angiography Studies
J Manipulative Physiol Ther 2002 (Jul); 25 (6): 370–383 ~ FULL TEXT
All 16 vertebral arteries from the 8 patients displayed no changes in their lumen dimensions with full cervical rotation, although curves in each of the arteries did change. The model and cadaveric vertebral arteries demonstrated localized compression or kinking of the vessel wall with atlanto-axial rotation contralaterally but revealed no evidence of major contribution of stretching to stenosis.
|

|
Stroke, Cerebral Artery Dissection, and
Cervical Spine Manipulation Therapy
Journal of Neurology 2002 (Jul); 249 (8): 1098–1104
Stroke represents an infrequent adverse reaction associated with cervical spine manipulation therapy. Attempts to identify the patient at risk and the type of manipulation most likely to result in these complications of manipulation have not been successful. A retrospective review of 64 medical legal cases of stroke temporally associated with cervical spine manipulation was performed to evaluate characteristics of the treatment rendered and the presenting complaints in patients reporting these complications. Ninety two percent of cases presented with a history of head and/or neck pain and 16 (25 %) cases presented with sudden onset of new and unusual headache and neck pain often associated with other neurological symptoms that may represent a dissection in progress. The strokes occurred at any point during the course of treatment. Certain patients reporting onset of symptoms immediately after first treatment while in others the dissection occurred after multiple manipulations. There was no apparent dose-response relationship to these complications.
|

|
Transcranial Sonography and Vertebrobasilar Insufficiency
J Manipulative Physiol Ther 2002 (Mar); 25 (3): 180–183 ~ FULL TEXT
This illustrates a case of extra-arterial mechanical compression of the vertebral arteries documented by transcranial Doppler sonography procedures. Brainstem symptoms were correlated with a documented perfusion deficit during cervical positional testing. This case also demonstrated that spinal manipulative therapy may be safely used on patients with vertebrobasilar insufficiency when the biomechanics and related flow studies are elucidated.
|

|
Arterial Dissections Following Cervical Manipulation:
The Chiropractic Experience
Canadian Medical Association Journal 2001 (Oct 2); 165 (7): 905–906 ~ FULL TEXT
Following approval by the Institutional Review Board of the Canadian Memorial Chiropractic College in Toronto, Ont., a review of malpractice data from the Canadian Chiropractic Protective Association (CCPA) was carried out to evaluate all claims of stroke following chiropractic care for the 10-year period between 1988 and 1997. There are over 4500 licensed chiropractors in Canada. The likelihood that a chiropractor will be made aware of an arterial dissection following cervical manipulation is approximately 1 in 8.06 million office visits, 1 in 5.85 million cervical manipulations, 1 in 1430 chiropractic practice years and 1 in 48 chiropractic practice careers.
|

|
Vertebral Artery Flow and Cervical Manipulation:
An Experimental Study
J Manipulative Physiol Ther 1999 (Sep); 22 (7): 431–435 ~ FULL TEXT
We present an experimental model for investigations of vertebral artery hemodynamics during biomechanical interventions. We found a modest and transient effect of cervical manipulation on vertebral artery volume flow. The model may have further applications in future biomechanical research, for example, to determine whether any of several spinal manipulative techniques imposes less strain on the vertebral artery, thereby reducing possible future cerebrovascular accidents after such treatment.
|

|
Vertebral Artery Volume Flow in Human Beings
J Manipulative Physiol Ther 1999 (Jul); 22 (6): 363–367 ~ FULL TEXT
This appears to be the first in vivo Doppler study on human vertebral artery volume blood flow. Our results indicate that in symptom-free subjects there is no change in vertebral artery perfusion during rotation in spite of significant changes in flow velocity.
|

|
Vertebral Artery Flow and Spinal Manipulation:
A Randomized, Controlled and Observer Blinded Study
J Manipulative Physiol Ther 1998 (Mar); 21 (3): 141–144
To the best of our knowledge, this is the first study comparing flow velocity in the vertebral artery before and after spinal manipulative therapy. We found no significant changes in otherwise healthy subjects with a biomechanical dysfunction of the cervical spine.
|
|